Abstract
Background
This study aims to explore the efficacy of tumor-infiltrating lymphocytes (TIL) along with interferon-α (IFN-α) to treat stage III malignant melanoma (MM) patients in China.
Methods
Between May 2010 and October 2014, 77 patients of stage III MM who underwent surgery were collected in this study. These patients were divided into two groups: patients who received TIL + IFN-α ± RetroNectin-activated cytokine-induced killer cells (R-CIK) in Arm 1 (n = 27) and IFN-α ± R-CIK in Arm 2 (n = 50) as adjuvant therapy. The primary endpoints were disease-free survival (DFS) time and DFS rates measured at time points of 1, 2, and 3 years. The secondary endpoints were overall survival (OS) rates measured at time points of 1, 2, 3, and 5 years as well as OS as evaluated by Kaplan-Meier.
Results
Our results indicated that the median DFS and OS in Arm 1 were significantly better than those in Arm 2. The data also demonstrated that DFS rate and OS rates in Arm 1 were significantly better than those in Arm 2 at all measured time points.
Conclusion
Patients who undergo surgical excision of stage III MM appear to enjoy prolonged DFS and OS when treated with TIL + IFN-α compared to IFN-α alone.
1. Introduction
The epidemiology data of the United States in 2014 indicated that an estimated 76,100 patients were diagnosed with melanoma and 9710 patients died from the disease [1]. Worse yet, incidence of this disease appeared to be rising rapidly. From 2002 to 2006, the incidence of melanoma increased by 33% among men and 23% among women [2]. Currently, definitive surgical excision is still the primary treatment for candidate malignant melanoma patients. However, the rate of relapse for stage III malignant melanoma patients remains very high even with the administration of adjuvant high-dose interferon-α (IFN-α) [3]. In numerous clinical trials, this IFN-α adjuvant therapy has been shown to improve DFS but not OS [4–6]. In cases of metastatic disease, prognosis is exceptionally poor with mOS of 6 to 8 months and a 5-year OS rate of approximately 6% [7, 8]. Recently, numbers of novel immunotherapies such as anticytotoxic T-lymphocyte-associated protein 4 (anti-CTLA-4) and programmed death 1 (anti-PD-1) antibodies have gained FDA approval. While, anti-PD-1 antibody, which has been associated with a 38% objective response rate (ORR), is only approved for advanced malignant melanoma [9]. Therefore, the identification of new postoperative therapies for malignant melanoma patients is of urgent importance.
For a long time, TIL therapy had already shown promise for advanced melanoma patients, with 51% to 72% ORR by Rosenberg et al. [10–14]. Then, more and more clinical trials applied TIL to treat advanced malignant melanoma patients; however, the data of applying TIL to treat postoperative malignant melanoma patients is still few. In 2002, Labarriere et al. reported that TIL treatment combined with interleukin-2 (IL-2) can prolong the DFS of stage III malignant melanoma patients, who emerged only one metastatic lymph node [15]. Unfortunately, in 2007, the 7 years' follow-up data from that same trial failed to show that TIL treatment combined with IL-2 prolonged RFS or OS overall. Intriguingly, however, in patients with only one positive lymph node, the estimated DFS and OS were significantly prolonged from the TIL + IL-2 therapy compared with IL-2 alone therapy [16]. In 2014, this same team of researchers updated their data and reported that TIL therapy can enhance the curative efficacy of patients with low tumor burden [17]. These data suggest that TIL treatment can be effective against malignant melanoma when applied in the right patient population. However, the efficacy of combining TIL therapy with administration of IFN-α to treat stage III malignant melanoma is unclear. The aim of our current study is to evaluate the efficacy of adjuvant TIL therapy with IFN-α for patients undergoing resection of stage III malignant melanoma.
2. Methods
2.1. Patients
From May 2010 to October 2014, 77 patients undergoing surgical resection of stage III malignant melanoma were collected in this study. Then, TIL + IFN-α ± R-CIK treatment was provided to 27 patients of Arm 1 and IFN-α ± R-CIK treatment was provided to 50 patients of Arm 2. This study was approved by the ethics committee at The Affiliated Cancer Hospital of Zhengzhou University, and an approved consent form was signed by all patients. The procedures were in accordance with the Helsinki Declaration of 1975 and Good Clinical Practice guidelines. Although the two groups have different sample sizes, the baselines of the two Arms were relatively well balanced. The detailed baseline of the 77 patients is listed in Table 1.
Table 1.
Clinical characteristics of 77 patients in this study.
| Arm 1 (n = 27) | Arm 2 (n = 50) | P value | |
|---|---|---|---|
| Sex | |||
| Male | 12 | 29 | 0.255 |
| Female | 15 | 21 | |
| Age (year) | |||
| >60 | 11 | 21 | 0.915 |
| ≤60 | 16 | 29 | |
| KPS | |||
| ≥80 | 22 | 45 | 0.289 |
| <80 | 5 | 5 | |
| Primary tumor site | |||
| Mucosa type∗ | 4 | 15 | 0.140 |
| No-mucosa type∗ | 23 | 35 | |
| R-CIK | |||
| Yes | 22 | 45 | 0.289 |
| No | 5 | 5 | |
| Treatment after metastasis | |||
| Surgical | 8 | 10 | — |
| Immunotherapy | 27 | 45 | — |
| Chemotherapy | 5 | 10 | — |
| Radiotherapy | 3 | 6 | — |
| Any 2 or more | 16 | 35 | — |
| Any 3 or more | 3 | 8 | 0.912 |
∗In Arm 1, mucosa type patients include 3 patients with nasal cavity mucosa melanoma and one patient with mouth cavity melanoma. No-mucosa type patients include 12 patients with acral lentiginous melanoma, 7 patients with nodular melanoma, and 4 patients with superficial spreading melanoma. In Arm 2, mucosa type patients include 5 patients with rectal mucosa melanoma, 6 patients with nasal cavity mucosa melanoma, 2 patients with mouth cavity melanoma, one patient with penis mucosa melanoma, and one patient with vaginal mucosa melanoma. No-mucosa type patients include 14 patients with acral lentiginous melanoma, 11 patients with nodular melanoma, and 10 patients with superficial spreading melanoma.
2.2. Retrospective Analysis and Follow-Up
The primary endpoint was DFS, with DFS rates measured at time points of 1, 2, and 3 years. The secondary endpoints were 1-, 2-, 3-, and 5-year OS rates as well as OS as evaluated by Kaplan-Meier analysis, and potential prognostic factors were also analyzed by univariate analysis and multivariate analysis. Following surgery, patients were seen for follow-up every 3 months for a two-year period. During postoperative years 2 to 5, patients were reevaluated every 6 months. Beyond the 5-year mark, follow-up evaluation occurred annually. The follow-up deadline was December 8, 2016. When follow-up evaluation revealed metastatic disease, other therapies were employed, including surgery, immunotherapy, chemotherapy, and radiotherapy (Table 1).
2.3. Preparation of TIL
Following surgery, fresh excised tumor tissues were used to culture TILs. Firstly, the excised tumor tissues were sliced into pieces of approximately 2 to 3 mm3 in size using a scalpel. Secondly, collagenase, DNase I type IV, and hyaluronidase type V (Sigma-Aldrich, St. Louis, MO, United States) were used to perform enzymatic digestion of these tissues for 2 to 3 hours at room temperature to obtain single-cell suspension. Thirdly, the single-cell suspension was filtered, washed twice with phosphate-buffered saline (PBS), and then incubated in a 12-well plate at a concentration of 1.0 × 106 TIL/ml in X-VIVO medium (Muenchensteinerstrasse 38 CH-4002 Basel, Switzerland) with 7000 IU/ml recombinant human interleukin-2 (rhIL-2). The next day, the cell suspension was removed and further purified via Ficoll gradient. The purified bulk TIL culture was maintained at a concentration of 1-2 × 106 cells/ml in X-VIVO medium with 7000 IU/ml rhIL-2 until all melanoma cells were eliminated and a cell number of at least 5 × 107 TIL cells were achieved. This culture process required approximately 10 to 14 d. Finally, the cultured TIL cells were immediately used with anti-CD3 antibody (GE Healthcare Biosciences, Pittsburgh, PA, USA; 5 μg/ml) and 1000 IU/ml rhIL-2 for large-scale expansion. By this process, cultures were expanded to 5 × 109 TIL cells and were harvested. Finally, these cells were infused back into patients.
2.4. Preparation of R-CIK
Peripheral blood mononuclear cells (PBMCs) of the patients were used to culture R-CIK. The detailed process of R-CIK preparation is the same to our published data [18]. Then, at the transfusion day, the dose of R-CIKs is about 5 × 109 cells.
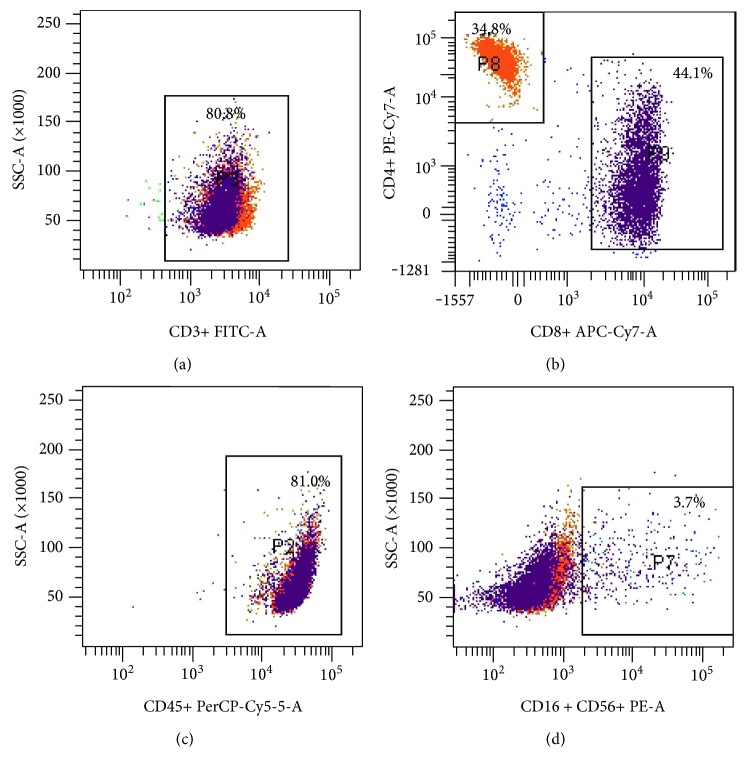
2.5. Phenotype Detection
In order to analyze the cell population of TILs before transfusion, they were stained with antibodies against CD3-FITC, CD4-PE-Cy7-A, CD8-APC-Cy7-A, and CD16/CD56-PE (BD Bioscience, San Jose, CA, USA) and flow cytometry was performed using a BD FACSCanto cell sorter (BD Bioscience, San Jose, CA, USA). Finally, the proportion of CD3+CD4+ and CD3+CD8+ cells of TILs was analyzed by gating the CD3+ population, and the percentage of CD3-CD16+ CD56+ cells of TILs was analyzed by CD45+ gating.
2.6. Statistical Analysis
Spss17.0 software was used to perform the statistical analysis. The Kaplan-Meier method was used to analyze the DFS and OS. Univariate and multivariable analyses also were used to analyze the prognostic factors. P < 0.05 was considered to demonstrate a statistically significant difference.
3. Results
3.1. Phenotype Analysis
Before transfusion of TIL cells to patients, we used flow cytometry to detect the proportion of CD3+, CD3+CD4+, CD3+CD8+, and CD3-CD16+CD56+ cells (Figures 1(a), 1(b), 1(c), and 1(d)). When the proportion of CD3+, CD3+CD4+, CD3+CD8+, and CD3-CD16+CD56+ cells reached appropriate levels, then we transfused the TIL back to patients. At the time of delivery of cultured TIL back to patients, the composition of the transfused cells was as follows: CD3+ 80.8% ± 3.23%, CD3+CD4+ 34.8% ± 2.14%, CD3+CD8+ 44.1% ± 2.56%, and CD3-CD16+CD56+ 3.7% ± 0.34%.
Figure 1.
(a) The proportion of CD3+ T cells among TIL cells. (b) The proportion of CD3+CD4+ and CD3+CD8+ T cells among TIL cells. (c) The proportion of CD45+ T cells among TIL cells. (d) The proportion of CD3−CD16+CD56+ T cells among TIL cells.
3.2. Treatment Outcomes
Our data demonstrated that the mDFS and mOS of Arm 1 versus Arm 2 were 23.66 months versus 9.78 months (χ2 = 11.559, P ≤ 0.001, Figure 2) and 43.75 months versus 21.86 months (χ2 = 15.03, P ≤ 0.001, Figure 3), respectively. Then, we also analyzed the 1-year DFS rates and OS rates, 2-year DFS rates and OS rates, 3-year DFS rates and OS rates, and 5-year OS rates. The data indicated that DFS rate and OS rates in Arm 1 were significantly better than those in Arm 2 at all measured time points. The detailed data was listed in Table 2. Thus, it appears that stage III malignant melanoma patients can benefit from TIL + IFN-α treatment.
Figure 2.
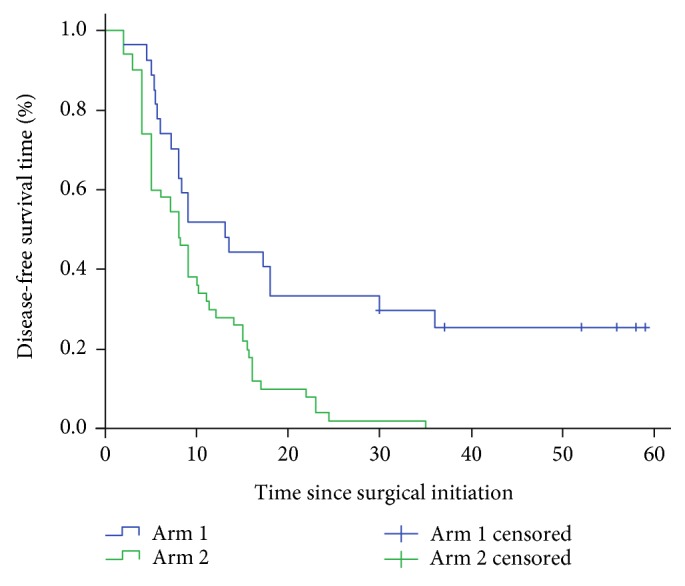
Disease-free survival time of Arm 1 versus Arm 2 was calculated in 27 patients in Arm 1 compared with 50 patients in Arm 2.
Figure 3.
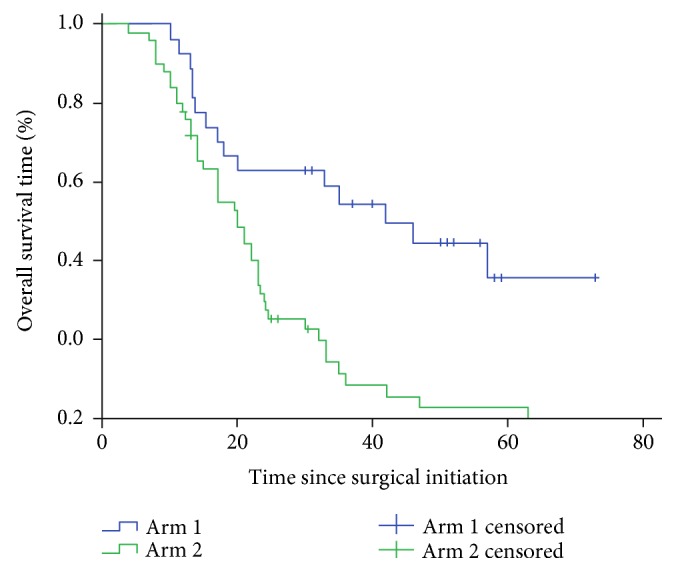
Overall survival time of Arm 1 versus Arm 2 was calculated using 27 patients in Arm 1 compared with 50 patients in Arm 2.
Table 2.
Treatment group outcomes.
| Treatment group | DFS | OS | ||||
|---|---|---|---|---|---|---|
| Arm 1 | Arm 2 | P | Arm 1 | Arm 2 | P | |
| 1-year DFS or OS rates | 48.21% (95% CI 29.76–64.46%) | 28.00% (95% CI 16.45–40.75%) | 0.04 | 92.59% (95% CI 73.50–98.09%) | 78.00% (95% CI 63.81–87.16%) | 0.03 |
| 2-year DFS or OS rates | 33.38% (95% CI 17.80–49.78%) | 2.00% (95% CI 0.16–9.23%) | 0.00 | 62.96% (95% CI 42.12–78.07%) | 32.00% (95% CI 19.70–44.97%) | 0.00 |
| 3-year DFS or OS rates | 25.96% (95% CI 12.47–41.75%) | 0% (95% CI 0-0%) | 0.00 | 55.56% (95% CI 35.22–71.81%) | 16.00% (95% CI 7.50–27.37%) | 0.00 |
| 5-year DFS or OS rates | — | — | — | 48.14% (95% CI 28.69–65.19%) | 12.00% (95% CI 4.88–22.60%) | 0.00 |
3.3. Prognostic Factors of TIL + IFN-α ± R-CIK Treatment in Arm 1
The DFS and OS of Arm 1 patients achieved greater improvement compared with those of Arm 2 patients. In order to observe potential prognostic factors in the Arm 1 treatment group, then we analyzed many factors such as sex, age, KPS scores, cell numbers for transfusion, number of culture days, and use of R-CIK therapy. Although univariate analyses indicated that KPS scores, transfused cell numbers, and increased duration of culture were potential predictive factors (Table 3), there were no significant differences by multivariate analysis based on these predictive factors (Tables 4 and 5).
Table 3.
Univariate analysis.
| DFS (months) | P | mOS (months) | P | |
|---|---|---|---|---|
| Age (years) | ||||
| >60 | 25.69 | 0.637 | 42.79 | 0.814 |
| ≤60 | 21.27 | 38.82 | ||
| Sex | ||||
| Male | 20.47 | 0.560 | 37.33 | 0.861 |
| Female | 28.17 | 44.10 | ||
| KPS scores | ||||
| ≥80 | 26.69 | 0.032 | 49.33 | 0.020 |
| <80 | 13.27 | 21.50 | ||
| Cell numbers for transfusion | ||||
| <8 × 109 | 6.91 | 0.000 | 16.94 | 0.000 |
| ≥8 × 109 | 30.97 | 53.46 | ||
| Culture days | ||||
| <30 | 30.77 | 0.014 | 55.78 | 0.001 |
| ≥30 | 13.79 | 24.43 | ||
| R-CIK | ||||
| Yes | 29.22 | 0.578 | 44.29 | 0.791 |
| No | 22.35 | 35.28 | ||
Table 4.
Multivariate analysis (DFS).
| Parameters | Hazard ratio | 95% confidence interval | P value |
|---|---|---|---|
| KPS (≥80 scores versus <80 scores) | 0.948 | (0.889–1.011) | 0.104 |
| Cell numbers for transfusion (≥8 × 109 versus <8 × 109) | 0.912 | (0.782–1.064) | 0.276 |
| Culture days (<30 days versus ≥30 days) | 1.038 | (0.976–1.105) | 0.268 |
Table 5.
Multivariate analysis (OS).
| Parameters | Hazard ratio | 95% confidence interval | P value |
|---|---|---|---|
| KPS (≥80 scores versus <80 scores) | 0.944 | (0.878–1.015) | 0.119 |
| Cell numbers of transfusion (≥8 × 109 versus <8 × 109) | 0.794 | (0.586–1.075) | 0.136 |
| Culture days (<30 days versus ≥30 days) | 1.064 | (0.981–1.153) | 0.134 |
3.4. Prognostic Factors of IFN-α ± R-CIK Treatment in Arm 2
In Arm 1, our data indicated that adding R-CIK might not improve the DFS and OS of stage III malignant melanoma patients. To investigate whether adding R-CIK can improve the DFS or/and OS of the patients of Arm 2, we also used univariate analysis. Unfortunately, our data demonstrated that there were no significant differences whether with R-CIK therapy or not by univariate analysis (DFS: 9.94 months versus 8.40 months, P = 0.707; OS: 21.66 months versus 23.83 months, P = 0.770). Thus, it appears that stage III malignant melanoma patients cannot benefit from R-CIK based on IFN-α therapy.
3.5. Adverse Events
In this retrospective analysis, all patients completed our immunotherapy. There were no severe adverse effects (grade 3 or grade 4) associated with TIL, IFN-α, or R-CIK therapy. The primary side effects of immunotherapy (grade 1 or grade 2) were fever, arthralgia, nausea, leucopenia, liver dysfunction, anemia, and vitiligo (Table 6).
Table 6.
Distribution of adverse events.
| Side effects | Arm 1 | Arm 2 | ||
|---|---|---|---|---|
| Grade 1/2 | Grade 3/4 | Grade 1/2 | Grade 3/4 | |
| Fever | 13 | 0 | 20 | 0 |
| Arthralgia | 5 | 0 | 13 | 0 |
| Nausea | 3 | 0 | 12 | 0 |
| Leukopenia | 4 | 0 | 8 | 0 |
| Liver dysfunction | 2 | 0 | 9 | 0 |
| Anemia | 3 | 0 | 10 | 0 |
| Vitiligo | 2 | 0 | 1 | 0 |
4. Discussion
Clearly, surgery is still the appropriate primary treatment for candidate malignant melanoma. However, in high-dose IFN-α as a current adjuvant therapy, the rate of relapse for stage III malignant melanoma patients remains very high [3]. The treatment of stage III malignant melanoma patients with TIL in combination with IL-2 has previously demonstrated promising results [15–17]. Unfortunately, this combination appears to prolong DFS and OS only among those patients with a single-positive lymph node.
Based upon these encouraging results, efforts to improve the treatment method will be an urgent significance. In our study, administration of cultured autologous TIL combined with IFN-α therapy was employed as an adjuvant treatment strategy for stage III malignant melanoma patients. This was compared to the use of IFN-α alone. Our data indicates that TIL combined with IFN-α therapy can improve the DFS and OS of stage III malignant melanoma patients. From 1991 to present, CIK cell therapy has been applied as an immunotherapy for cancer patients in many clinical trials, including in patients with hepatocellular carcinoma (HCC), non-small-cell lung cancer (NSCLC), and renal cell carcinoma (RCC) [19–26]. And in our Immunotherapy Center of The Affiliated Cancer Hospital of Zhengzhou University, we also did some work to demonstrate that R-CIK (or CIK) combined with chemotherapy or not can prolong the mOS of HCC, RCC, pancreatic cancer, and so on [18, 27–31]. Therefore, R-CIK therapy was often employed in both Arm 1 and Arm 2 patients in order to increase the treatment efficacy. However, in our analysis of Arm 1 and Arm 2 data, there was no difference in DFS and OS with or without R-CIK. Up to now, many experiments indicate that CIK or R-CIK is considered to a nonspecific immunotherapy, which has major histocompatibility- (MHC-) unrestricted cytotoxic effect [26, 32]. Therefore, R-CIK and IL-2 are all nonspecific immunotherapy methods. It appears that combined two nonspecific immunotherapies (R-CIK and IL-2) may not improve the prognosis of stage III malignant melanoma patients.
As we all have known, Rosenberg et al. had done many experiments for metastatic melanoma by applying TIL combined with nonmyeloablative chemotherapy with or without 1200 cGy total body irradiation. The objective response rate can achieve more than 50% [33–35]. In our study, we applied TIL combined with IFN-α to treat stage III malignant melanoma as an adjuvant therapy, which indicated that this therapy can prolong the DFS and OS of these patients. Therefore, we conclude that patients diagnosed with stage III malignant melanoma can benefit from TIL + IFN-α treatment after surgery.
To explore the prognostic factors governing the efficacy of TIL + IFN-α treatment in Arm 1, we analyzed individual results in Arm 1 and correlated them to sex, age, KPS scores, cell numbers at time of transfusion, duration of culture, and presence or absence of R-CIK therapy. Although univariate analyses identified KPS scores, cell numbers for transfusion, and number of culture days as potential predictive factors, there were no significant differences based on these potential predictive factors by multivariate analysis. This leads us to conclude that adjuvant TIL therapy combined with administration of IFN-α can prolong DFS and OS in stage III malignant melanoma patients generally. However, adding R-CIK cannot improve the DFS and OS of stage III malignant melanoma patients further. In addition, in our study of all the patients, there were no treatment-related mortalities, and the toxic effects were comparable with previous TIL studies and IFN-α studies. While TIL cultures and transfusions require high laboratory expertise, the quality of cultured TIL is the key problem in clinical use. Most of all, our study demonstrated that TIL combined with IFN-α might be a good method for stage III malignant melanoma patients. In the future, a multicenter randomized phage study will become a better way to reveal the true clinical contribution of TIL combined with IFN-α for the treatment of stage III malignant melanoma.
5. Conclusions
In summary, adjuvant adoptive TIL therapy combined with IFN-α therapy can prolong the DFS and OS of stage III malignant melanoma patients who undergo surgical excision. Toxicity and side effects were quite manageable. In the future, more studies should be performed to provide additional data regarding the efficacy of adjuvant TIL combined with IFN-α therapy in the management of stage III malignant melanoma.
Acknowledgments
This study was supported by the International Cooperation Foundation of Henan Science and Technology Research (172102410021). The authors are grateful for the collaboration received from the participating college and its staff. The authors thank Qiqing Cai, Songtao Gao, and Weitao Yao (from the Department of Bone and Tissue, Henan Cancer Hospital), who served as the surgeons and collected the specimens for TIL cell culture. The authors are also grateful to Dr. Yan Zhao from the Department of Radiology, Henan Cancer Hospital, China, for the statistical analysis.
Abbreviations
- IFN-α:
Interferon-α
- DFS:
Disease-free survival time
- OS:
Overall survival time
- TIL:
Tumor-infiltrating lymphocytes
- R-CIK:
RetroNectin-activated cytokine-induced killer cells
- ORR:
Overall response rate
- ACT:
Adoptive cell transfer
- PBMC:
Peripheral blood mononuclear cells.
Conflicts of Interest
The authors declare that they have no competing interests.
Authors' Contributions
Wei Li, Quanli Gao, and Linping Xu designed the study. Wei Li and Yaomei Wang analyzed the data and wrote the paper. Lingdi Zhao and Daniel B. Kellner read and edited the manuscript. All authors read and provided comments on the report. All authors read and approved the final manuscript. Wei Li, Linping Xu, and Yaomei Wang share co-first authorship.
References
- 1.Siegel R., Ma J., Zou Z., Jemal A. Cancer statistics, 2014. CA: A Cancer Journal for Clinicians. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A., Saraiya M., Patel P., et al. Recent trends in cutaneous melanoma incidence and death rates in the United States, 1992-2006. Journal of the American Academy of Dermatology. 2011;65(5) Supplement 1:S17–S25. doi: 10.1016/j.jaad.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 3.Davar D., Kirkwood J. M. Adjuvant therapy of melanoma. Cancer Treatment and Research. 2016;167:181–208. doi: 10.1007/978-3-319-22539-5_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirkwood J. M., Strawderman M. H., Ernstoff M. S., Smith T. J., Borden E. C., Blum R. H. Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. Journal of Clinical Oncology. 1996;14(1):7–17. doi: 10.1200/JCO.1996.14.1.7. [DOI] [PubMed] [Google Scholar]
- 5.Kirkwood J. M., Ibrahim J. G., Sondak V. K., et al. High- and low-dose interferon alfa-2b in high-risk melanoma: first analysis of intergroup trial E1690/S9111/C9190. Journal of Clinical Oncology. 2000;18(12):2444–2458. doi: 10.1200/JCO.2000.18.12.2444. [DOI] [PubMed] [Google Scholar]
- 6.Eggermont A. M., Suciu S., Santinami M., et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet. 2008;372(9633):117–126. doi: 10.1016/S0140-6736(08)61033-8. [DOI] [PubMed] [Google Scholar]
- 7.Balch C. M., Soong S. J., Gershenwald J. E., et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. Journal of Clinical Oncology. 2001;19(16):3622–3634. doi: 10.1200/JCO.2001.19.16.3622. [DOI] [PubMed] [Google Scholar]
- 8.Barth A., Wanek L. A., Morton D. L. Prognostic factors in 1,521 melanoma patients with distant metastases. Journal of the American College of Surgeons. 1995;181(3):193–201. [PubMed] [Google Scholar]
- 9.Hamid O., Robert C., Daud A., et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. The New England Journal of Medicine. 2013;369(2):134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenberg S. A., Dudley M. E. Adoptive cell therapy for the treatment of patients with metastatic melanoma. Current Opinion in Immunology. 2009;21(2):233–240. doi: 10.1016/j.coi.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenberg S. A., Restifo N. P., Yang J. C., Morgan R. A., Dudley M. E. Adoptive cell transfer: a clinical path to effective cancer immunotherapy. Nature Reviews Cancer. 2008;8(4):299–308. doi: 10.1038/nrc2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dudley M. E., Rosenberg S. A. Adoptive cell transfer therapy. Seminars in Oncology. 2007;34(6):524–531. doi: 10.1053/j.seminoncol.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dudley M. E., Wunderlich J. R., Yang J. C., et al. Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. Journal of Clinical Oncology. 2005;23(10):2346–2357. doi: 10.1200/JCO.2005.00.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dudley M. E., Yang J. C., Sherry R., et al. Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. Journal of Clinical Oncology. 2008;26(32):5233–5239. doi: 10.1200/JCO.2008.16.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Labarriere N., Pandolfino M. C., Gervois N., et al. Therapeutic efficacy of melanoma-reactive TIL injected in stage III melanoma patients. Cancer Immunology, Immunotherapy. 2002;51(10):532–538. doi: 10.1007/s00262-002-0313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khammari A., Nguyen J. M., Pandolfino M. C., et al. Long-term follow-up of patients treated by adoptive transfer of melanoma tumor-infiltrating lymphocytes as adjuvant therapy for stage III melanoma. Cancer Immunology, Immunotherapy. 2007;56(11):1853–1860. doi: 10.1007/s00262-007-0340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khammari A., Knol A. C., Nguyen J. M., et al. Adoptive TIL transfer in the adjuvant setting for melanoma: long-term patient survival. Journal of Immunology Research. 2014;2014:10. doi: 10.1155/2014/186212.186212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li W., Wang Y., Zhao L., et al. Efficacy of RetroNectin-activated cytokine-induced killer cell therapy in metastatic brain tumor patients. Oncology Research and Treatment. 2015;38(4):160–165. doi: 10.1159/000380890. [DOI] [PubMed] [Google Scholar]
- 19.Liu L., Zhang W., Qi X., et al. Randomized study of autologous cytokine-induced killer cell immunotherapy in metastatic renal carcinoma. Clinical Cancer Research. 2012;18(6):1751–1759. doi: 10.1158/1078-0432.CCR-11-2442. [DOI] [PubMed] [Google Scholar]
- 20.Hontscha C., Borck Y., Zhou H., Messmer D., Schmidt-Wolf I. G. Clinical trials on CIK cells: first report of the international registry on CIK cells (IRCC) Journal of Cancer Research and Clinical Oncology. 2011;137(2):305–310. doi: 10.1007/s00432-010-0887-7. [DOI] [PubMed] [Google Scholar]
- 21.Yu X., Zhao H., Liu L., et al. A randomized phase II study of autologous cytokine-induced killer cells in treatment of hepatocellular carcinoma. Journal of Clinical Immunology. 2014;34(2):194–203. doi: 10.1007/s10875-013-9976-0. [DOI] [PubMed] [Google Scholar]
- 22.Hui D., Qiang L., Jian W., Ti Z., Da-Lu K. A randomized, controlled trial of postoperative adjuvant cytokine-induced killer cells immunotherapy after radical resection of hepatocellular carcinoma. Digestive and Liver Disease. 2009;41(1):36–41. doi: 10.1016/j.dld.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Zhao H., Wang Y., Yu J., et al. Autologous cytokine-induced killer cells improves overall survival of metastatic colorectal cancer patients: results from a phase II clinical trial. Clinical Colorectal Cancer. 2016;15(3):228–235. doi: 10.1016/j.clcc.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Lee J. H., Lee J. H., Lim Y. S., et al. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148(7):1383–1391. doi: 10.1053/j.gastro.2015.02.055. [DOI] [PubMed] [Google Scholar]
- 25.Li R., Wang C., Liu L., et al. Autologous cytokine-induced killer cell immunotherapy in lung cancer: a phase II clinical study. Cancer Immunology, Immunotherapy. 2012;61(11):2125–2133. doi: 10.1007/s00262-012-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kong D. S., Nam D. H., Kang S. H., et al. Phase III randomized trial of autologous cytokine-induced killer cell immunotherapy for newly diagnosed glioblastoma in Korea. Oncotarget. 2016;8(4):7003–7013. doi: 10.18632/oncotarget.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li W., Wang Y., Kellner D. B., Zhao L., Xu L., Gao Q. Efficacy of RetroNectin-activated cytokine-induced killer cell therapy in the treatment of advanced hepatocelluar carcinoma. Oncology Letters. 2016;12(1):707–714. doi: 10.3892/ol.2016.4629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Z., Zhang Y., Liu Y., et al. Association of myeloid-derived suppressor cells and efficacy of cytokine-induced killer cell immunotherapy in metastatic renal cell carcinoma patients. Journal of Immunotherapy. 2014;37(1):43–50. doi: 10.1097/CJI.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 29.Wang Z., Liu Y., Li R., et al. Autologous cytokine-induced killer cell transfusion increases overall survival in advanced pancreatic cancer. Journal of Hematology & Oncology. 2016;9(1):p. 6. doi: 10.1186/s13045-016-0237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Z., Liu Y., Zhang Y., Shang Y., Gao Q. MDSC-decreasing chemotherapy increases the efficacy of cytokine-induced killer cell immunotherapy in metastatic renal cell carcinoma and pancreatic cancer. Oncotarget. 2016;7(4):4760–4769. doi: 10.18632/oncotarget.6734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li W., Wang Y., Kellner D. B., Xu L., Mai L. Efficacy of cytokine-induced killer cells in the treatment of elderly patients with metastatic pancreatic adenocarcinoma. Central-European Journal of Immunology. 2015;40(2):188–193. doi: 10.5114/ceji.2015.52833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim J. S., Kim Y. G., Park E. J., et al. Cell-based immunotherapy for colorectal cancer with cytokine-induced killer cells. Immune Network. 2016;16(2):99–108. doi: 10.4110/in.2016.16.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goff S. L., Dudley M. E., Citrin D. E., et al. Randomized, prospective evaluation comparing intensity of lymphodepletion before adoptive transfer of tumor-infiltrating lymphocytes for patients with metastatic melanoma. Journal of Clinical Oncology. 2016;34(20):2389–2397. doi: 10.1200/JCO.2016.66.7220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alvarez-Downing M. M., Inchauste S. M., Dudley M. E., et al. Minimally invasive liver resection to obtain tumor-infiltrating lymphocytes for adoptive cell therapy in patients with metastatic melanoma. World Journal of Surgical Oncology. 2012;10(1):p. 113. doi: 10.1186/1477-7819-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rosenberg S. A., Yang J. C., Sherry R. M., et al. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clinical Cancer Research. 2011;17(13):4550–4557. doi: 10.1158/1078-0432.CCR-11-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]