Abstract
Objectives:
To identify and compare the stressors in the work environment experienced by employees in primary health care and secondary health care, amongphysiciansand nurses.
Patients and methods:
The survey was conducted to identify types of stressors by assessing health care workers employed in the primary and secondary health care services of the Public Institution, the Health Centre of the Sarajevo Canton, using a questionnaire about stress in the workplace.
Results:
Among all study participants stressors connected to the organization of work, finance and communication were found to affect their mental health most strongly. The results show a significant difference between primary and secondary health care in experience of stressors related to the organization of work, communication, and stressors related to the emotional and physical risks. Primary health care physicians report a significantly higher experience of stress and impact on mental health compared with other physicians related to emotional difficulties when working in the field of palliative care. Our results also indicate a significant difference between primary and secondary health providers in experiencing stressors related to the organization of work, such as: on-call duty shifts, an inadequate working environment and in the assessment of administrative work overload.
Conclusion:
The survey identified the most intense stressors for doctors and nurses at primary and secondary levels of health care services. The results of the study indicate that doctors and nurses have a different hierarchy of stressors, as well as subjects at Primary and Secondary Health Care. The results of the study indicate that subjects et Primary Health Care perceive more stressful organizational, emotional and communicational problems.
Keywords: stress at work, primary health care, secondary health care
1. INTRODUCTION
Stress is a response of the organism to various stimuli, positive or negative, real or perceived. These stimuli can be short-term, long-term or recurring, and regardless of their nature, they cause changes in the body. The short-term effects of stressors have certain benefits, but long-term exposure to stress results in an increase in blood pressure, consequent heart failure or suppression of the immune system (1, 2). Different types of stressors, the length of exposure to stress and personality characteristics are the elements that influence the response of the hypothalamic-pituitary-adrenal axis, which is considered responsible for the development of various conditions caused by the effects of chronic stress (3). High stress levels can contribute to development of health-related impairments, including mental and behavioral disorders, as well as other physical impairments,. Stress caused by work environment factors falls into the category of daily stress, and because of its consequences, requires special attention and evaluation, and calls for the definition of adequate preventive measures. According to its most common definition, stress at work results from the imbalance between demands and the ability to satisfy those demands. It can be a significant cause of illness, high levels of absenteeism due to illness, professional issues or constant changes of personnel within an institution. Karasek’s demand-control model of occupational stress presents the two dimensions in which the stress level increases with the increasing demands of the workplace while reducing the level of decision-making (4). The factors that cause occupational stress are divided into general and specific stressors. General stressors include those that are present in all or at least most working environments. In some professions, along with the general stressors, there are also specific stressors that are typical of the environment and the specific profession (5). Occupational stress has become a growing problem in health care workers in recent years, and given this trend, a number of different tools have been developed to identify the main causes of stress (6).
2. AIM
The aim of this study was to identify the types and intensity of stressors in the workplace for health care providers at primary and secondary levels of health care, to compare them in relation to physicians and nurses and health care providers at different levels of the health care system.
3. PATIENTS AND METHODS
The study was cross-sectional, epidemiological and observational, performed as an anonymous survey of health care workers in primary health care services, and in specialist-consultative services in secondary health care, at the Public Institution the Health Centre of the Sarajevo Canton, in the period between April 2014 and September 2014. The study involved a total of 489 participants, 418 (85%) from Primary Health Care (PHC) and 71 (14%) from Secondary Health Care (SHC).
The questionnaire used in this study was created and designed as part of the project “Occupational health and a healthy environment” (6). After obtaining the permission of the author, the questionnaire was adapted into the Bosnian language, and a panel of experts validated its content. The panel was organized as a focus group formed of five members. The questionnaire adoption was done using the principles adapted from Geisinger (1994) and Van de Vijver & Hambleton (1996) for cross-cultural researchers to ensure satisfactory reliability and validity of the cross-cultural study. After the internal validation, the questionnaire contained 31 questions assessed using a Likert scale, from 1 (not at all stressful) to 5 (very stressful), with the possibility of the respondent entering three additional stressors that were not listed in the questionnaire.
Retaining the five point Likert scale in analysis makes interpretation difficult, because of that we put it up into three point scale. The groups “stressful’ and “very stressful”, as well as „not at all stressful” and “slightly stressful”, have been clubbed together.
The questionnaire contained an introductory part:
Socio-demographic data: Age, sex, marital status, occupation, academic degree.
Workplace data: Service and level of health care, shift work, type of employment contract.
The questions in the Questionnaire about occupational stress for health care workers were grouped into three categories:
Stressors related to organization of work (14 questions).
Stressors related to communication (9 questions).
Occupational stressors related to emotional and physical risks (8 questions).
Ethics statement
The study was conducted under the principles of the applicable revision of the Declaration of Helsinki, after approval had been given by the Ethics Committee of the Medical Faculty of the University of Sarajevo (7). The data were collected in accordance with bioethical standards, ensuring the privacy of the subjects involved in the research, and protection of data confidentiality.
Statistical analyses
Statistical analysis of the collected data was performed by the descriptive biostatistics method, using statistical software program SPSS ® version 22.0 for Windows, and calculating the descriptive measures: count, percentage, minimum, maximum, arithmetic mean, median and standard deviation and appropriate statistical tests such as χ2-test.
Cronbach’s alpha reliability coefficient was used for for three scales (groups of questions for measuring workplace stressors) divided on the basis of three main factors. In this paper the software package Microsoft Excel 2010 was used. The hypothesis was tested by the correlation method. The difference between samples was considered significant if p<0.05.
4. RESULTS
During the study, n= 600 questionnaires were distributed, 512 were returned (response rate 85.3%). Out of 512 questionnaires, 489 (95.5%) were fully useful for the analysis. Most subjects were employed in General Primary Health Care - Family Medicine, n=279 (57.1%), and in other services belonging to primary health care, n=139 (28.5%). Most subjects were employed in the Primary Health care n=418 (85.5%), and there were Secondary Health Care subjects 71 (14.5%), seeing that the Secondary Health Care is a numerically smaller branch in an organizational sense.
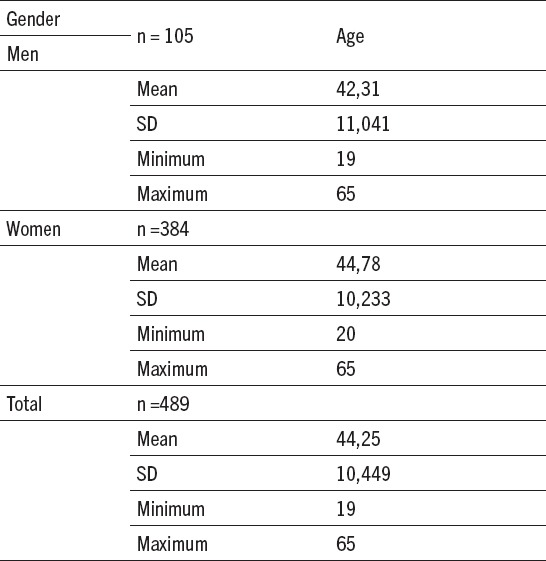
According to occupation breakdown, among the subjects there were n=174 (37.7%) physicians, n=305 (62.3%) nurses. The average age of male gender was M = 42.31 years (SD = 11.04). For female respondents average age was M = 44.78 years (SD = 10.23) (Table 1).
Table 1.
Sociodemografic data of stressors in our sample
The most intense stressors in PHC, SHC and among physicians and nurses are presented by tables (Table 2, Table 3). The main stressors for the study groups employees in PHC: Unrealistic expectations of patients and family members, Wrong media information about health profession, Negative public attitude towards health profession, Overload of administrative work, Insufficient number of workers/staff, Daily unforeseen and unplanned-for situations, inadequate personal income, Work overload, Limited time to examine patients.
Table 2.
Most intensive stressors related to the organization of work, communication, emotional and physical risks
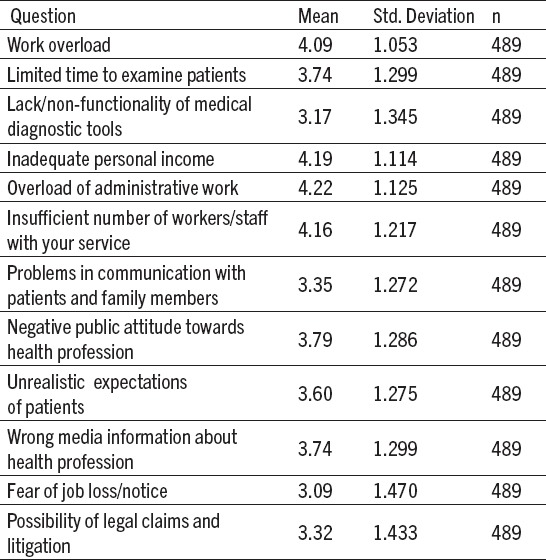
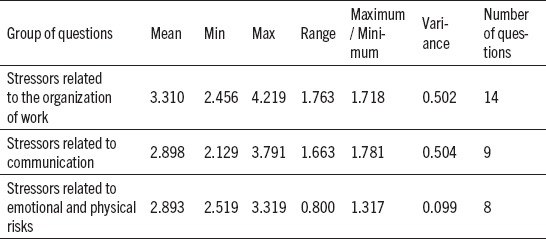
Table 3.
Comparison of the three groups of questions (Central tendency and dispersion measures)
The most intensive stressors in SHC were almost the same except stressors related to communication.
In the study group of nurses there were identified the similar stressors as most intensive and in addition of these also possibility of being infected from the patients, possibility of injury by a sharp object/needle and possible physical attack by a patient.
Among physicians the main identified stressors were the same as well as in other study groups but in addition there were a stressors Possibility of legal claims and litigation, Fear of loss of license and Fear of job loss/notice.
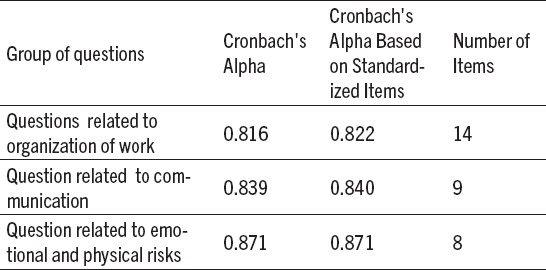
Deletion any ofquestions will not increase Cronbach alpha in the group of questions related to the organization of work (Table 3).
In the group of questions related to communication, deletion of only one question - “problems in communication with patient or family member” would slightly increase Cronbach alpha value for only 0.1. Because of that, we did not delete it and were counted Cronbach alpha value with this question.
Deletion any of questions will not increase Cronbach alpha in the group of questions related to emotional and physical risks (Table 4).
Table 4.
Cronbach’s alpha reliability coefficient forthree scales/ groups of questions
5. DISCUSSION
The results of this study indicate the exposure of health care workers to a wide range of occupational stressors. Among all study participants stressors connected to the organization of work, finance and communication were found to affect their mental health most strongly.
The results seem to identify some common stressors which will help in recommending a set of interventions for all health care workers and some stressors more common in study groups which will lead to another set of measures which are more in line with the level of care and hierarchy. Primary health care physicians report a significantly higher experience of stress and impact on mental health compared with other physicians related to emotional difficulties when working in the field of palliative care. The same results were shown in a study in the United Kingdom (9).
Our results also indicate a significant difference between primary and secondary health providers in experiencing stressors related to the organization of work, such as: on-call duty shifts, an inadequate working environment and in the assessment of administrative work overload. Similar results were found in research in Saudi Arabia among health providers at primary and secondary levels of health care (10), where the level among nurses was 45.5%, or 43.1% and 46.2% in primary and secondary care, respectively. Our results show that organizational and funding issues have a high position among stress factors, which is supported by the literature data. Poor organization of work is a stressor mentioned by health care workers in developed countries, but also in health care systems such as, for example in Croatia (11). In studies in Taiwan (12) and Australia (13) it was noted that specialist physicians, general practitioners/family physicians and registered nurses had a statistically elevated likelihood of work stress relative to other health care providers, similar to what we noted in our research. Financial constraints are typical for countries in transition, as well as in physicians in developed countries who work in public institutions with limited financial, material and spatial resources, which results in the development of stress. Considering the fact that significant economic and political reforms took place in the countries of South Eastern Europe over the past two decades and, as a result, the reform of the health care system is still ongoing in all countries in the region, including Bosnia and Herzegovina, it is to be expected that there is a somewhat different hierarchy regarding the most important stressors related to the working place here, compared to developed countries (15).
Considering the fact that Bosnia and Herzegovina is a country in transition and these changes in the organization of the health system and education of professionals occurred in the 1990-ies, it is expected for us to witness new occupational stressors and their obvious connection with these changes. The importance of organization at the level of institutions is not negligible, as it can be a source of stress for employees. In the field of the organization of the work of an institution, the usual prominent stressors are the insufficient number of workers/staff, poor communication with superiors or colleagues, work overload, overload of administrative work or little possibility of promotion at work (15), and all of these stressors were also identified and assessed as stressful or very stressful in our research.
6. CONCLUSIONS
The results of this research identify specific stressors related to the working environment. There is a significant difference in the assessment of the intensity of stressors between the PHC and SHC employees. PHC employees experience stressors more intensely in the field of organization of work, such as: work overload, overload of administrative work, on-call duty shifts, daily unforeseen and unplanned for situations, lack of adequate continuous education, and inadequate working space. Primary health care is also characterized by more intense emotional stressors, such as: emotional difficulties in the field of palliative care, the inability to separate private and professional life, inaccurate media information about the health care profession, unrealistic expectations of patients and their families, and the fear of a physical attack by a patient. Secondary health care employees assess little possibility of promotion at work as a more intense stressor. From the results of the research it may be concluded that physicians and nurses/technicians have a different hierarchy of stressors. Physicians strongly perceive stressors in the field of organization of work, such as work overload and limited time for examination of the patient, the lack of adequate continuous medical education, lack of literature, public criticism and the possibility of legal claims.
Footnotes
• Authors’ contributions: Conception and design: NT and ADžK; Acquisition, analysis and interpretation of data: ZJ; Drafting the article: NT, ADžK and ZJ; Revising it critically for important intellectual content: ZJ and ADžK; Approved final version of the manuscript: NT, ADžK and ZJ.
• Conflict of interest: none declared
REFERENCES
- 1.Dantzer R, Kelley KW. Stress and Immunity: An Integrated View of Relationships between the Brain and the Immune System. Life Sci. 1998;44(26):1995–2008. doi: 10.1016/0024-3205(89)90345-7. [DOI] [PubMed] [Google Scholar]
- 2.Dhabhar HYPERLINK “https://www.ncbi.nlm.nih.gov/pubmed/?term=Dhabhar%20FS%5BAuthor%5D&cauthor=true&cauthor_uid=11268419. ” FS. Acute stress enhances while chronic stress suppresses skin immunity. The role of stress hormones and leukocyte trafficking.AnnHYPERLINK “https://www.ncbi.nlm.nih.gov/pubmed/11268419. ” N Y HYPERLINK “https://www.ncbi.nlm.nih.gov/pubmed/11268419. ”AcadHYPERLINK “https://www.ncbi.nlm.nih.gov/pubmed/11268419” Sci. 2000;917:876-93. [DOI] [PubMed]
- 3.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Chronic stress experience in young physicians: impact of person and workplace related factors. Int Arch Occup Environ Health. 2010 Apr 83;(4):373–9. doi: 10.1007/s00420-009-0467-9. [DOI] [PubMed] [Google Scholar]
- 4.Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. AdmSci Q. 1979;24:285. [Google Scholar]
- 5.Tuthill JI, Ahmed MS, Mathew G, Bolton AC, Molokhia AA. University Hospital Lewisham, London, UK. Work-related stress amongst doctors in intensive care, anesthetics, accident and emergency and general medicine Crit Care. 2013;17(Suppl 2):508. [Google Scholar]
- 6.Milosević M. Validation of the questionnaire on workplace stressors for hospital workers. [dissertation] University of Zagreb. 2010 [Google Scholar]
- 7.Geisinger KF. Cross-cultural normative assessment: Translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychological Assessment. 1994;6(4):304–12. [Google Scholar]
- 8.Van de Vijver F, Hambleton RK. Translating tests: Some practical guidelines. European Psychologist. 1996;1(2):89–99. [Google Scholar]
- 9.World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 10.Al-Makhaita MH, Sabra A, Hafez HA. Predictors of work-related stress among nurses working in primary and secondary health care levels in Dammam Eastern, Saudi Arabia. J Family Community Med. 2014;21(2):79–84. doi: 10.4103/2230-8229.134762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knezevic B. Stress at work and work ability health care workers in hospitals [dissertation] University of Zagreb. 2010 [Google Scholar]
- 12.Lee WL, Tsai SH, Tsai CW, Lee CY. A Study on Work Stress, Stress Coping Strategies and Health Promoting Lifestyle among District Hospital Nurses in Taiwan. J Occup Health. 2011;53(5):377–83. doi: 10.1539/joh.11-0054-fs. [DOI] [PubMed] [Google Scholar]
- 13.Lim J, Bogossian F, Ahern K. Stress and coping in Australian nurses: a systematic review. Int Nurs Rev. 2010;57(1):22–31. doi: 10.1111/j.1466-7657.2009.00765.x. [DOI] [PubMed] [Google Scholar]
- 14.Salavecz G, Chandola T, Pikhart H, Dragano N, Siegrist J, Jöckel KH, et al. Work stress and health in Western European and post-communist countries: an East-West comparison study. J Epidemiol Community Health. 2010;64(1):57–62. doi: 10.1136/jech.2008.075978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pranjic N, Males-Bilic L, Beganlic A, Mustajbegovic J. Mobbing, Stress and Work Ability Index among Physicians in Bosnia and Herzegovina: Survey Study. Croat Med J. 2006;47(5):750–8. [PMC free article] [PubMed] [Google Scholar]


