Abstract
Introduction:
The association between lung tuberculosis and lung carcinoma is still controversial.
Objective:
to describe the characteristics of patients with associated lung tuberculosis (TB) and lung carcinoma (LC) in patients treated in Clinic for pulmonary diseases and TB “Podhrastovi”.
Material and Methods:
This is the retrospective study of patients with LC associated with TB treated in Clinic for pulmonary diseases and TB “Podhrastovi” in five-year period -from 2012 to 2016. We analyzed sex and age of patients, whether TB preceded LC or LC preceded TB, a time period between the developments of these two diseases, activity of TB, the histopathological type of LC, localization of LC in lungs (bronchial, peripheral, cavern) according to histopathological type.
Results:
In this period there were 2608 patients treated for LC. Among them there were 34 patients with diagnosed TB or 1.3%. All of them were smokers. No one had active TB. TB was the first diagnosis in all these patients. Each patient was previously treated for TB in hospital and had regular anti TB treatment. TB preceded LC in median time of 5 years (interquartile range 2 to 25 years). In 21 cases it was carcinoma of the drainage bronchus, in 11 cases it was peripheral lung carcinoma and 2 cases it was cavern carcinoma.
Conlusion:
patients with cured pulmonary tuberculosis represent a group at risk for developing lung carcinoma. Changes in the bronchial and alveolar mucosa which tuberculosis leaves behind in the lungs must be taken as a possible place of later malignant alteration. Patients with any form of pulmonary tuberculosis have to be controlled continuously.
Keywords: lung carcinoma tuberculosis
1. INTRODUCTION
Lung carcinoma (LC) is the leading cause of cancer-related death and represents one of the major public health problems worldwide (1). Tuberculosis (TB) is very important cause of morbidity and mortality despite good prevention, diagnosis and effective therapy, especially in the poor and developing countries (1, 2). The simultaneous or sequential occurrence of TB and LC in the same patient has been reported in various case series and case-control studies (1). Malignant tumors are characterized by an enormous proliferation of the cells with the tendencies of destruction and capture of normal tissue anarchically with the formation of metastases. Long term TB process, especially if it takes up larger portions of the lungs leads to metaplasia of the epithelium of bronchi and alveoli. Such metaplasia can be considered as a precancerous condition. The connection between lung tuberculosis and lung or bronchial carcinoma certainly exists, as it has been verified by many pathologists and clinical doctors. In the tuberculosis field cancer can develop or in cancer depleted patients tuberculosis develops secondary (3, 4).
Association between lung cancer and tuberculosis opens a series of questions about the relationship between these two diseases.
Tuberculosis and cancer can be found in the lungs in the following relationship:
a) Carcinoma occurs on the tuberculosis ground and reactivates the old focus of tuberculosis.
b) Carcinoma develops from the tuberculosis scars (scar carcinoma).
c) Carcinoma occurs by epithelium metaplasia of tuberculous cavities.
d) Both diseases are independent of each other and develop simultaneously or sequentially.
e) Metastatic carcinoma developing in an old TB lesion.
Lung cancer may arise as a consequence of chronic inflammatory changes that lead to metaplasia of epithelium in the caverns, in the calcified lymph nodes, in the old scars in the bronchi that are a consequence of the perforation of a tuberculosis changed lymph nodes (5). The three most common forms are: cavern carcinoma, carcinoma of the drainage bronchus and peripheral lung scar cancer (3, 4).
2. OBJECTIVE
Objective of the study is to describe the characteristics of patients with associated lung TB and lung carcinoma treated in Clinic for pulmonary diseases and TB “Podhrastovi “, Sarajevo.
3. MATERIAL AND METHODS
This is the retrospective study of patients with LC associated and TB treated in Clinic for pulmonary diseases and TB “Podhrastovi” in five-year period: from 2012 to 2016. We analyzed the histopathological type of carcinoma, whether tuberculosis preceded carcinoma or carcinoma preceded TB, a time period between the development of these two diseases, type - activity of tuberculous changes in lungs, sex and age of patients.
The diagnoses of LC and tuberculosis were classified as follows: simultaneous - when the diagnoses of tuberculosis and LC occurred simultaneously or when the time between the two diagnoses was < 6 months; sequential (LC first) - when tuberculosis was diagnosed ≥ 6 after LC diagnosis and within 12 months of completion of LC treatment; sequential (TB first) - when LC is diagnosed ≥ 6 months after tuberculosis diagnosis, or two illnesses developed independently (2, 6, 7).
4. RESULTS
There were 2608 patients treated for LC in five-year period: from 2012 to 2016. in Clinic for Pulmonary Diseases and Tuberculosis “Podhrastovi” of University Clinical Center in Sarajevo. Among them there were 34 patients with diagnosed TB or 1.3%. All of these patients were smokers. No one had active TB i.e. no one had sputum positive for Mycobacterium tuberculosis and none had histopathological evidence of active tuberculosis. Bronchoscopy with lung biopsy was done in each patient and the obtained material was examined histopathologically. TB was the first diagnosis in all these patients. Each patient was treated for TB in hospital and had had regular anti TB treatment. TB preceded LC in median time of 5 years (interquartile range- 2 to 25 years). The most common h histopathological type was the planocellular carcinoma - 13 cases, following with squamous cell carcinoma - 8, adenocarcinoma - 7 and small cell carcinoma - 6 cases. In 21 cases it was carcinoma of the drainage bronchus, in 11 cases it was peripheral lung carcinoma and in 2 cases it was cavern carcinoma (not active TB cavern but open-negative syndrome - unclosed old tuberculous cavern, but without the positivity for Mycobacterium tuberculosis).
Results are shown on Figures 1, 2 and 3.
Figure 1.
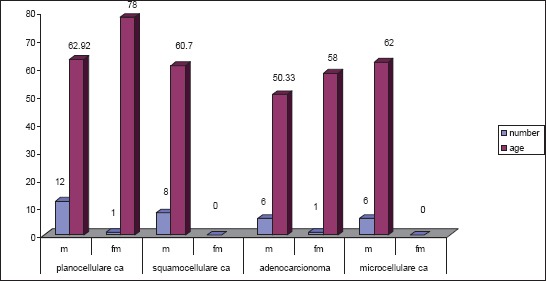
Age, sex and histopathological type of LC in patients with associated LC and TB
Figure 2.
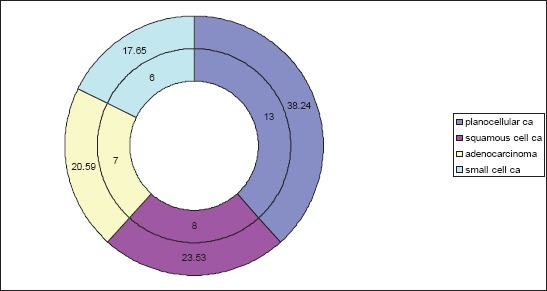
The ratio between different histopathological types of LC in patients with associated LC and TB
Figure 3.
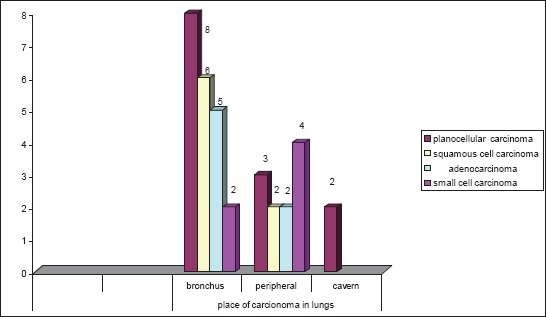
The localization of LC in lungs according to histopathological type in patients with associated LC and TB
There were 34 patients with LC and TB: 12 males middle-aged 62,2 and 1 female aged 78 with planocellular carcinoma; 8 males middle-aged 60,7 with squamous cell carcinoma, 6 males middle-aged 50,33 and 1female aged 58 with adenocarcinoma, 6 males middle-aged 62 with small cell lung carcinoma. Men are significantly more represented than women (p<0,001) (Figure 1).
Among 34 patients with LC and TB there were 38,24% patients with planocellular carcinoma, 23,53% with squamous cell carcinoma, 20,59% with adenocarcinoma and 17,65 % with small cell carcinoma. Number of patients with NSCLC (Non-small-cell lung carcinoma) was significantly bigger (p<0,001) than small cell lung carcinoma (Figure 2).
There were 21 bronchial carcinoma: 8 planocellular, 6 squamous cell, 5 adenocarcinoma and 2 small cell carcinoma; 11 peripheral carcinoma: 3 planocellular, 2 squamous cell, 2 adenocarcinoma and 4 small cell carcinoma ; and 2 planocellular cavern carcinoma (Figure 3).
5. DISCUSSION
Clinicians sometimes encounter patients with co-existent lung carcinoma and pulmonary TB. The co-existence of TB and LC has remained controversial (5). These patients may be the patients with LC developing active pulmonary TB or carcinoma develops in patients earlier treated for TB. Chronic inflammation due to TB is thought to be responsible for the genesis of cancer (1). Co-existence of cancer and TB may cause a delay in the diagnosis. Patients with cancer are vulnerable to develop active TB because of immunosuppression due to the use of intensive treatment modalities, such as aggressive chemotherapy, radiotherapy or to malnutrition (7).
Cancer is a global health problem causing more than 7 million deaths accounting to nearly 13% of all deaths worldwide (7). The burden of cancer is increasing globally, with an expected 20 million new cases per year in 2020, half of which will be in the low-and middle-income countries (8). TB is one of the major causes of death amongst infectious diseases and it is estimated that one-third of the human population is infected with Mycobacterium tuberculosis. In 2010, there were an estimated 8.8 million incident cases of TB (range 8.5 - 9.2 millions) and 1.1 million deaths (range 0.9 - 1.2 millions) among human immunodeficiency virus (HIV)-negative cases of TB and an additional 0.35 million deaths (range, 0.32 - 0.39 million) among people who were HIV-positive (20/100 000 population) (9).
There are various reasons for association between lung TB and LC by different authors. One hypothesis would be that inflammation associated with infections can contribute to carcinogenesis (7). Reactive oxygen or nitrogen species produced by activated neutrophils can bind to the DNA, inducing genetic damage and neoplastic transformation (10). In fact, it has been shown that alterations of the fragile histidine triad gene might be involved in lung carcinogenesis in patients with chronic pulmonary tuberculosis (11-13). In addition, during tissue repair, there is increased cell proliferation and angiogenesis, and the epithelium is more prone to metaplasia (12, 13). Furthermore, carcinogens concentrate preferentially in hyperactive areas to induce neoplastic changes (14).
In our study in 2608 patients with LC in only 34 of them or in 1, 3% we found the association between TB and LC. In all of them TB preceded LC in median time of 5 years (interquartile range 2 to 25 years). In one study median time was also 5 years with interquartile range 1-30 years (1). In none of our cases LC was diagnosed before TB. In a retrospective case-control study (15, 16) involving 36 patients with LC, 10 patients (27.8%) were diagnosed with tuberculosis and cancer concomitantly, whereas 26 (72.2%) were diagnosed with tuberculosis after being diagnosed with cancer.
In our study the most common histopathological type of LC was planocellular carcinoma i.e. 38, 24%. In other studies adenocarcinoma was the most common histopathological type (1, 10, 14, 15). According to localization, in our study the most common was the bronchial carcinoma.
6. CONCLUSION
Patients with cured pulmonary tuberculosis represent a group at risk for developing lung cancer. Metaplastic and proliferative changes in the bronchial and alveolar mucosa which tuberculosis leaves behind, can not be ignored and must be taken as a possible place of later malignant alteration. Therefore, patients with any form of pulmonary tuberculosis have to be controlled continuously.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Silva DR, Valentini DF, Jr, Müller AM, de Almeida CP, Dalcin Pde T. Pulmonary tuberculosis and lung cancer: simultaneous and sequential occurrence. J Bras Pneumol. 2013;39(4):484–9. doi: 10.1590/S1806-37132013000400013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang HY, Li XL, Yu XS, Guan P, Yin ZH, He QC, et al. Facts and fiction of the relationship between preexisting tuberculosis and lung cancer risk: a systematic review. Int J Cancer. 2009;125(12):2936–44. doi: 10.1002/ijc.24636. [DOI] [PubMed] [Google Scholar]
- 3.Teventiyanon T, Ratanaharathorn V, Leoparait J. Mucoepidermoid carcinoma of the lung presenting as cavitary lesion. J Med Assoc Thai. 2004;87(8):988–91. [PubMed] [Google Scholar]
- 4.Yilmaz A, Gungor S, Damadoglu E, Axoy F, Aibatly A. Coexisting bronchial carcinod tumor and pulmonary tuberculosis in the same lobe: a case report. Tuberk. Toraks. 2004;52(4):369–72. [PubMed] [Google Scholar]
- 5.Lubarsch O. Ueber den primaren Krebs des ileum, nebst bemerhunge uber das gleichzeitge vorkommen von krebs und tuberculose. Virchows Arch. 1888;111:280–317. [Google Scholar]
- 6.Cha SI, Shin KM, Lee JW, Lee SY, Kim CH, Park JY. The clinical course of respiratory tuberculosis in lung cancer patients. Int J Tuberc Lung Dis. 2009;13(8):1002–7. [PubMed] [Google Scholar]
- 7.Harikrishna J, Sukaveni V, Kumar DP, Mohan A. Cancer and tuberculosis. JIACM. 2012;13(2):142–4. [Google Scholar]
- 8.Sharma V, Kerr SH, Kawar Z, Kerr DJ. Challenges of cancer control in developing countries: current status and future perspective. Future Oncol. 2011;7:1213–22. doi: 10.2217/fon.11.101. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Global tuberculosis control 2011. Geneva: 2011. [Google Scholar]
- 10.Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117(5):1175–83. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nalbandian A, Yan BS, Pichugin A, Bronson RT, Kramnik I. Lung carcinogenesis induced by chronic tuberculosis infection: the experimental model and genetic control. Oncogene. 2009;28(17):1928–38. doi: 10.1038/onc.2009.32. [DOI] [PubMed] [Google Scholar]
- 12.Song L, Yan W, Deng M, Song S, Zhang J, Zhao T. Aberrations in the fragile histidine triad (FHIT) gene may be involved in lung carcinogenesis in patients with chronic pulmonary tuberculosis. Tumour Biol. 2004;25(6):270–5. doi: 10.1159/000081391. [DOI] [PubMed] [Google Scholar]
- 13.Song L, Yan W, Zhao T, Deng M, Song S, Zhang J, et al. Mycobacterium tuberculosis infection and FHIT gene alterations in lung cancer. Cancer Lett. 2005;219(2):155–62. doi: 10.1016/j.canlet.2004.06.036. [DOI] [PubMed] [Google Scholar]
- 14.Dheda K, Booth H, Huggett JF, Johnson MA, Zumla A, Rook GA. Lung remodeling in pulmonary tuberculosis. J Infect Dis. 2005;192(7):1201–9. doi: 10.1086/444545. [DOI] [PubMed] [Google Scholar]
- 15.Dacosta NA, Kinare SG. Association of lung carcinoma and tuberculosis. J Postgrad Med. 1991;37(4):185–9. [PubMed] [Google Scholar]
- 16.Watanabe A, Tokue Y, Takahashi H, Sato K, Nukiwa T, Honda Y. Management of mycobacteriosis in general hospital without isolation ward for tuberculosis patients. Clinical study on pulmonary tuberculosis associated with lung cancer patients, Kekkaku. 1999;74(2):157–62. [PubMed] [Google Scholar]


