Abstract
Introduction:
Accidental murmurs occur in anatomically and physiologically normal heart. Accidental (innocent) murmurs have their own clearly defined clinical characteristics (asymptomatic, they require minimal follow-up care).
Aim:
To point out the significance of auscultation of the heart in the differentiation of heart murmurs and show clinical characteristics of accidental heart murmurs.
Material and methods:
Article presents review of literature which deals with the issue of accidental heart murmurs in the pediatric cardiology.
Results:
In the group of accidental murmurs we include classic vibratory parasternal-precordial Stills murmur, pulmonary ejection murmur, the systolic murmur of pulmonary flow in neonates, venous hum, carotid bruit, Potaine murmur, benign cephalic murmur and mammary souffle.
Conclusion:
Accidental heart murmurs are revealed by auscultation in over 50% of children and youth, with a peak occurrence between 3-6 years or 8-12 years of life. Reducing the frequency of murmurs in the later period can be related to poor conduction of the murmur, although the disappearance of murmur in principle is not expected. It is the most common reason of cardiac treatment of the child, and is a common cause of unreasonable concern of parents.
Keywords: heart murmurs, accidental heart murmurs, heart auscultation
1. INTRODUCTION
Heart murmurs can be organic (sign of heart disease) and inorganic (usually called innocent; basically divided into accidental and functional) (1). Accidental murmurs occur in anatomically and physiologically normal heart. Some authors may differ them from functional (murmurs occurring in diseases which secondarily affect the heart), but they are often involved in group of common innocent murmurs. With sufficient knowledge, it is possible to differentiate accidental and functional murmur, just by auscultation. The localisation of accidental murmurs is distributed in the precordium, most often with left edge of sternum. Accidental (innocent) murmurs have their own clearly defined clinical characteristics (asymptomatic, they require minimal follow-up care) (1). They occur in anatomically and physiologically normal heart. They are called innocent, harmless, physiological, irrelevant, evolving, benign, habitual, infantile, growth murmurs, accidental, non-pathological, non-organic, normal, false, meaningless, ‘’functional’’, supine position murmurs, nonsignificant, transitory, dynamic. Their place of origin may not be the same, but they are most commonly associated with aortic and pulmonary valve (trigonodation with systole) and turbulent bloodflow within cardiac and vascular structure. The pathologic substrate is a change from laminar to turbulent flow. Incomplete opening of the aortic valve during systole gives a triangular appearance of the aortic valve lumen and tension of the valve, and thus converting laminar blood flow to turbulent flow with the vibration of valves and surrounding wall structures (1, 2). The transfer of valve vibrations in the wall caused by tribulation, probably represents the physical background for etiology of these murmurs. This change is not only developed because of trigonidation (inconsistency or volatility) of the valve, but also because of the flow of the blood through large vessels, which vary in size and diameter. Insufficient elasticity of valves leads to the incomplete opening of the pulmonic or aortic valve, with a so-called triangular form of valve opening, which leads to turbulence outside the normal laminar flow and flickering/trembling of the valve, which produces the murmur. When they appear on semilunar valves (pulmonary and aortic valve), for the development of murmur the tendon fibers of atrioventricular valves are primarily responsible (3, 4). The common background for development of accidental murmurs presents interaction of turbulency, vibrations of valves and limited dimensions of wall structures. Today it is possible with echocardiographical aproach to visualise the symmetry within the structure of pulmonary and aortic valve (bicuspid, instead of tricuspid semilunar valves). Probably the most common places for development of accidental murmurs are tendinious fibers (chorde tendinae) of atrioventricular valves, so-called atypical or accessory tendinious fibers. Finally, there are also tendinious fibers (chorde tendinae) which are completely atypical and are present in the left ventricle, and they do not communicate with atrioventricular valve.
When that kind of atypical chordae is placed in a position with normal blood flow, it produces a murmur similar to harp, which has a high frequency and produces a very typical musical murmur, around the lower left edge of sternum (so-called Still’s murmur) (5).
There is no dependency between localisation of accessory chordae and maximal point of earshot of that murmur.
2. AIM
To point out the significance of auscultation of the heart in the differentiation of heart murmurs and show clinical characteristics of accidental heart murmurs.
3. MATERIAL AND METHODS
Article presents review of literature which deals with the issue of accidental heart murmurs in the pediatric cardiology.
4. RESULTS
Classic vibratory parasternal–precordial Stills murmur (described by Still in 1918) is a systolic ejection murmur which constitutes over 50% of all accidental murmurs, best heard in area between ictus and lower left edge of sternum (maximal puncture is most commonly between 3rd and 4th intercostal space, on the left), usual intensity is between 2nd and 3rd degree based on Levine’s scale low-freqency, with duration in the first half or first two thirds of systole, by the quality it can be musical, vibratory, buzzing, pinking, blubbering/sobbing (6). Sometimes the murmur may radiate towards exile. Most frequently it is seen in children of preschool age, between the age of 3 to 7, it is increased with states of tachycardia, overload states, and is more audible/perceptible in lying position. It correlates with presence of aberrant chordae in depth of left ventricle (36%). It is the most common of all accidental murmurs. McKusic considers that the cause of these murmurs is trigonization/inconsistency of pulmonary cusps in systole. Some studies show that parasternal-precordial murmurs may be third, or even fourth degree, based on intensity, when is also possible to register a following thrill.
Pulmonary ejection murmur (physiological systolic) is the second most common innocent murmur, often heard at the base of the heart, to the left. In its character it is blowing to the third degree of loudness/volume. It is more harsh than Still’s murmur, increased with tachycardia and it is the loudest in lying position. It is common in kids with deformities of thorax, pectus excavatum, kyphoscoliosis, flat back syndrome, with obese children and abnormal heart positions (7, 8). It is seen in school-aged kids, and puberty and probably developed due to normal turbulency of blood to the pulmonary valve. It is less common than Still’s murmur, best heard in second and third intercostal space on the left, in lying position, probably due to increased stroke volume and ejection of blood. This murmur shows a significant increase of incidence, in deference to Still murmur, in cases of increased cardiac output, but we should keep in mind that both types of murmurs are increasing the frequency. It is briefly transmitted parasternaly and toward heart apex. Pulmonary components of 2nd heart sound are normal. It is frequently seen in adolescents and it is the most common accidental murmur in this age. Based on duration, it is included in the first part of systole, when the speed of systole ejection is at its maximum. Fast flow through an exit tract of the right ventricle, which is relatively superficial leads to trgonization/inconsistency of pulmonary cusps. Usually, the murmur is louder, when the patient is in a lying position, and after laying stress/overload, because of an increase in venous flow and stroke volume of the right ventricle. It is possible that murmur develops due to compression of pulmonary artery with following increase of cardiac phase and cardiac ejection.
The systolic murmur of pulmonary flow in neonates (physiological murmur of pulmonary stenosis in neonates) most commonly is lost on end of the second month of life (present in premature babies and neonates). It is ejection type, 1st or 2nd degree by Levine, and heard on both sides on the bases of heart with propagation to exile and the back. Short, usually developed due to turbulence of blood on bifurcation of the pulmonary artery. This is the weakest, by intensity, systolic murmur and best audible on the base of the heart, in exile, under armpits and in the back, on both sides.
Venous hum (cervical venous hum, spindle murmur) represents continuous murmur which may appear like profound silent and soft humming, with maximal audibility in systole. It is auscultated with fast blood flow, from the jugular vein into superior vena cavae, within the right edge of the manubrium of the sternum, although it can be auscultated on the left in second intercostal space (9).
It is also heard on the right with the neck, and on the front part of the thorax (above and below the clavicle). Maximal pointer is sometimes located just below right clavicle. These murmurs are usually seen in anemic patients, and are most prominent in sitting position and loosing on intensity, and nearly stoping in lying position. They are completely absent during the compression of jugular veins in the neck. Sometimes it is enough just to compress the vein with your thumb, in order to change or too loose, previously found systolic-diastolic murmur. After turning the head in the opposite position, it enhances. Murmurs are, by quality, the closest to deep silence, and soft humming /(differential diagnosis with murmur PDA). In extremely rare cases it can give the thrill. Most commonly it appears in preschool age, with the greatest prevalence in kids between age 3 to 8.
Carotid bruit (arterial supraclavicular vascular murmur, arterial murmur of neck blood vessels) is presented either above or below the clavicle on the right side, and it is transmitted to the bases (9). In overload states it gets louder, and a change in body position or respirations do not affect it. It is seen in proto or meso systole. Usually is short, commonly quiet, but it can be louder up to 4th degree of Levins scale, occasionally is palpable the thrill over carotid. Gets softer or lost with Hyperextension of the shoulders or compression of carotid on that side. Probably caused by turbulent blood flow in the exit parts of the great blood vessels in the aortic arch, thus when blood from the aorta in systole is re-directed to brachycephalic trunk and into the left carotid artery. Usually audible over clavicles, more presented on the right side. Can present the problem with differential diagnosing towards murmur of aortic stenosis.
Cardiopulmonary murmurs (Potaine) develops on parts of lungs close to the heart, from which air is expelled with contractions. This is the way the high-frequency high-pitched murmur occurs, which is mainly audible over pericardium on heart to lung border, almost always just in one particular place, and its loudness is changed with respirations. It is superficial, audible only in inspiring, and best heard at heart apex. These murmurs are almost always systolic and may vary in intensity, in dependance with respirations. Probably develops because of friction between heart and lung tissue. The murmur is not synchronised with heartbeats, and commonly heard in the middle of systole, from first tone. Starts abruptly, with narrow localisation and heard as chanting.
Benign cephalic murmur is presented during the first ten years of life, with low frequency, continuity, but in the least number of cases may be systolic. By localisation, in form with upper part of thorax and neck.
Mammary souffle is murmured with continuity, audible around mammary blood vessels, presented by adolescent persons.
5. DISCUSSION
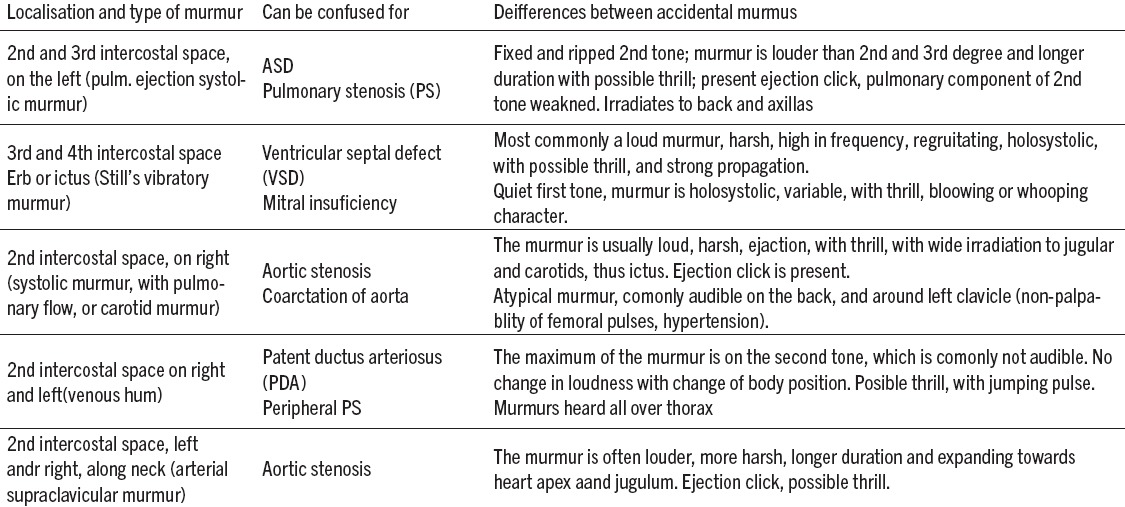
Differentially - diagnostically analyzed (Table 1) accidental murmurs of vibratory and pulmonary systolic - ejection character may be replaced with murmurs of organic origin in aortic stenosis, pulmonary stenosis, atrial septal defect (ASD). Supraclavicular or carotidic murmur can often be replaced with the murmur of aortic stenosis, coarctation, carotid stenosis, stenosis of the subclavian artery. Venous hum can often imitate the sound of murmur of persistent ductus arteriosus or arterio-venous fistulae. If you have enough experience, it is possible to differentiate accidental and functional murmur by auscultation. Still’s murmur may be replaced with murmur of mitral insufficiency, accidental murmur over the pulmonary artery with defect of the interatrial septum or partial anomalous pulmonary vein or vein, but in these cases doubts may be avoided if it is known that the aforementioned cardiac anomalies are characterized by accentuated and fixedly agitated other tone. Assistance in differential diagnosis can certainly provide an electrocardiogram, X-ray examination and ultrasound scan. The characteristics of these murmurs are that they are purely systolic, maximally affecting up to 60% of the systole, usually occur in early systole, are separated from both tons, with relatively shorter duration, with poor propagation (where they occur and die), and are mainly of ejection (extrusion) type. Most often in intensity they are between the first and second degree, and very rare of third. They can be best heard on the left sternal edge of the patient in the lying position. By shape they are ascending-descending (crescendo-decrescendo).. They are variable and change during respiration and body position change (4). They are amplified after loading or inhaling amyl nitrate, and are rarely encountered in the newborn and younger infants. They are not associated with other clinical signs of heart disease (10, 11, 18, 19). They are more gentle in the inspiration when the patient is sitting or standing. Murmurs are most often musical, soft with a frequency of oscillation of about 200 hertz. The amplitude maximum is in the early systole, and form of murmur is spindle-shaped. They are best audible in the supine position. Intensity is reduced with Valsalva maneuver. They are not associated with ejection clicks or abnormalities of other heart rate neither with cardiovascular abnormalities (12,13).
Table 1.
6. CONCLUSION
The characteristics of accidental murmurs are that they are purely systolic, maximally affecting up to 60% of the systole, usually occur in early systole, are separated from both tons, with relatively shorter duration, with poor propagation (where they occur and die), and are mainly of ejection (extrusion) type. Accidental heart murmurs are revealed by auscultation in over 50% of children and youth, with a peak occurrence between 3-6 years or 8-12 years of life. Reducing the frequency of murmurs in the later period can be related to poor conduction of the murmur, although the disappearance of murmur in principle is not expected. It is the most common reason of cardiac treatment of the child, and is a common cause of unreasonable concern of parents.
Footnotes
• Conflict of Interest: none declared.
• Author’s Contribution: E.B. made substantial contribution to conception and design (acquisition of data, analysis and interpretation of data). Z.B. revised it critically and gave final approval of the version to be submitted.
REFERENCES
- 1.Smith KM. The innocent heart murmur in children. J Pediatr Health Care. 1997 Sep-Oct;11(5):207–14. doi: 10.1016/s0891-5245(97)90103-6. [DOI] [PubMed] [Google Scholar]
- 2.Wiles HB, Saul JP. Pediatric cardiac auscultation. J S C Med Assoc. 1999 Oct;95(10):375–8. [PubMed] [Google Scholar]
- 3.Begic Z, Dinarevic SM, Pesto S, Begic E, Dobraca A, Masic I. Evaluation of Diagnostic Methods in the Differentiation of Heart Murmurs in Children. Acta Inform Med. 2016;24(2):94–8. doi: 10.5455/aim.2016.24.94-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvares S, Ferreira M, Mota CR. Intial assessment of heart murmurs in children: role of complementary diagnostic tests. Rev Port Cardiol. 1997 Jul-Aug;16(7-8):621–24. [PubMed] [Google Scholar]
- 5.Constant J. How to Differentiate Ejection Murmurs from Systolic Regurgitant Murmurs. Keio J Med. 1995;44(3):85–7. doi: 10.2302/kjm.44.85. [DOI] [PubMed] [Google Scholar]
- 6.Alpert MA. Systolic Murmurs. Clinical Methods: The History, Physical, and Laboratory Examinations. In: Walker HK, Hall WD, Hurst JW, editors. 3rd edition. Chapter 26. Boston: Butterworths; 1990. Available from: https://www.ncbi.nlm.nih.gov/books/NBK345/ [PubMed] [Google Scholar]
- 7.Van Oort A. The Vibratory Innocent Heart Murmor in Schoolchildren: Difference in Auscultatory Findings Between School Medical Officers and a Pediatric Cardiologist. Pediatric Cardiol. 1994;5:282–7. doi: 10.1007/BF00798121. [DOI] [PubMed] [Google Scholar]
- 8.Van Oort A. The Vibratory Innocent Heart Murmur in Schoolchildren: A Case-Control Doppler Echocardiographic Study. Pediatric Cardiol. 1994;15:275–81. doi: 10.1007/BF00798120. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz KJ. In: Bruits and Hums of the Head and Neck. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Chapter 18. Walker HK, Hall WD, Hurst JW, editors. Boston: Butterworths; 1990. Available from: https://www.ncbi.nlm.nih.gov/books/NBK289/ [PubMed] [Google Scholar]
- 10.Gressner IH. What makes a heart murmur innocent? Pediatr Ann. 1997 Feb;26(2):82–4. doi: 10.3928/0090-4481-19970201-05. 87-8, 90-1. [DOI] [PubMed] [Google Scholar]
- 11.Shaver JA. Cardiac auscultation: A cost-effective diagnostic skill. Curr Probl Cardiol. 1995;20:441. [PubMed] [Google Scholar]
- 12.Klewer SE, Donnerstein RL, Goldberg SJ. Still's like innocent murmur can be produced by increasing aortic velocity to a threshold value. Am J Cardiol. 1991;68:810–12. doi: 10.1016/0002-9149(91)90664-7. [DOI] [PubMed] [Google Scholar]
- 13.Danford DA, Nasir A, Gumbiner Cost assessement of the evaluation of the heart murmurs in children. Pediatrics. 1993;91:65–368. [PubMed] [Google Scholar]
- 14.Keck EW. Pedijatrijska kardiologija. Školska knjiga, Zagreb. 1995:1–15. [Google Scholar]
- 15.McCrindle WB, Shaffer MK, Kan SJ, Zahka GK, Rowe AS, Kidd L. Cardinal Clinical Signs in the Differentiation of Heart Murmurs in Children. Arch Pediatr Adolesc Med. 1996;150:169–74. doi: 10.1001/archpedi.1996.02170270051007. [DOI] [PubMed] [Google Scholar]
- 16.Wiles HB, Saul JP. Pediatric cardiac auscultation. J S C Med Assoc. 1999 Oct;95(10):375–8. [PubMed] [Google Scholar]
- 17.Asprey DP. Evaluation of children with heart murmurs. Lippincotts Prim Care Pract. 1998 Sep-Oct;2(5):505–13. [PubMed] [Google Scholar]
- 18.Marinović B. Anamneza i klinički pregled djeteta, Školska knjiga, Zagreb. 1994:19–35. 68-74. [Google Scholar]
- 19.Begic Z, Begic E, Begic N. Differential Diagnosis of Innocent Heart Murmurs In Children. American Journal of Cardiology. 2015;115:S30. doi: http://dx.doi.org/10.1016/j.amjcard.2015.01.114. [Google Scholar]


