Abstract
Background:
Anesthesia induction is often accompanied by a period of hemodynamic instability, which could be deleterious in patients with coronary artery disease (CAD) and left ventricular dysfunction undergoing coronary artery bypass graft (CABG) surgery. The aim of this study was to compare the hemodynamic responses to propofol, etomidate, and diazepam following anesthesia induction, laryngoscopy and intubation in CABG surgery patients with low ejection fraction (EF).
Methods:
A double-blind randomized, clinical study was performed on 150 patients with CAD and left ventricular dysfunction (EF≤35%) scheduled for elective CABG surgery with Cardiopulmonary bypass (CPB). Patients were randomly allocated to three groups A, B, and C. These patients received propofol, etomidate or diazepam at induction of anesthesia, respectively. Hemodynamic variables (systolic and diastolic blood pressure [SBP, DBP], mean arterial pressure [MAP] and heart rate [HR]) were measured and recorded at baseline, immediately before laryngoscopy and tracheal intubation and one and three minutes after intubation.
Result:
One minute after induction and before laryngoscopy, there was a statistically significant decrease from the baseline in SBP, DBP and MAP in all three groups, but these variables in each hemodynamic parameters in diazepam group were less than other two groups (p<0.001). Moreover, the mean HR decreased in patients receiving propofol and etomidate one minute after induction and before laryngoscopy, but did not decreased in the diazepam group (p=0.005).
Conclusion:
The present study showed that in patients undergoing CABG surgery with low EF, diazepam is more favorable in terms of hemodynamic stability compared to propofol and etomidate and this drug can be used safely for induction of anesthesia in patients with impaired ventricular function.
Keywords: Diazepam, Etomidate, Hemodynamics, Propofol, Ventricular dysfunction, CABG
1. INTRODUCTION
Laryngoscopy and intubation is an integral part of general anesthesia (GA) for cardiac surgeries. Direct laryngoscopy and endotracheal intubation are detrimental stimuli which can produce negative responses in the cardiovascular, respiratory and other physiological systems (1). Patients with coronary artery disease (CAD) and left ventricular dysfunction undergoing coronary artery bypass graft (CABG) surgery are one of the most high-risk groups among patients undergoing cardiac surgery (1, 2). Hypertension, tachycardia and arrhythmia caused by endotracheal intubation can be deleterious in patients with low cardiovascular reserve. These hemodynamic changes may alter the balance between myocardial oxygen supply and demand and as a result, the incidence of ischemia in patients with CAD can be precipitated (3, 4).
Induction methods of anesthesia for cardiovascular surgeries are usually based on considerations such as hemodynamic stability, effects on myocardial oxygen supply and demand and also minimizing the stress response to intubation. Thus, in order to induction of anesthesia and preparation of patient for laryngoscopy and tracheal intubation, anesthetic drugs are administrated in higher dosage than doses for maintaining anesthesia during surgery (4). That is why researchers are always inspired the production of drugs and methods to minimize hemodynamic changes occur during induction of anesthesia and laryngoscopy in patients (5, 6).
Propofol and etomidate are known anesthetic agents which are normally used for induction of anesthesia in cardiac surgeries, with different clinical features (7). Etomidate, which is a hypnotic drug with unique properties, is the most commonly used anesthetic induction agent with minimal side effects on cardiovascular and respiratory functions (8). However, it has been shown that etomidate administration can inhibit adrenal gland function by blocking 11β-hydroxylase and 17α-hydroxylase enzymes. There is a relation between etomidate administration and adrenal insufficiency, which caused by reversible inhibition of cortisol synthesis (9). Reduced cortisol and aldosterone level following to adrenal suppression almost started in less than 30 minutes after a single dose of etomidate and can last up to 72 hours (10). On the other hand, it has been shown that relative adrenal insufficiency in septic patients may induce morbidity and mortality (9). Etomidate disadvantages include nausea and vomiting, pain on injection, myoclonic movement and hiccups (11).
Propofol is an intravenous hypnotic agent, which commonly used for anesthesia induction due to rapid onset, short duration of action, anti-nausea and vomiting effect and feeling comfortable after surgery (9). The most prominent effect of propofol is a decrease in arterial blood pressure during induction of anesthesia and is associated with a decrease in cardiac output, stroke volume, and systemic vascular resistance (3, 9). Furthermore, propofol induces severe vasodilation while the effects of myocardial depression are not exactly clear. Vasodilation occurs in both venous and arterial circulation, which leads to reduced preload and afterload (12). After induction dose of propofol, heart rate (HR) does not change significantly because propofol can inhibit baroreflex response, so tachycardia response to hypotension is reducing. Drop in blood pressure after administration of propofol can be due to the effects of vasodilator and reduced sympathetic activity (13).
Diazepam is one of the drugs that have been used since half a century ago. It induces anesthesia with minimal cardiovascular effects like etomidate. Increase coronary blood flow and myocardial function, reduce myocardial oxygen consumption and blood pressure stability have been observed in cardiovascular patients following administration of diazepam (9).
Considering the importance and influence of hemodynamic changes on the outcome of surgery and related mortalities and conflicting results of previous studies related to propofol and diazepam hemodynamic responses (14-16), this study was conducted to compare the hemodynamic responses of three sedatives for anesthetic induction with minimal hemodynamic changes in CABG surgery patients with low ejection fraction (EF).
2. METHODS
A double-blind randomized, clinical study was performed on 150 patients with CAD and left ventricular dysfunction (EF≤35%) scheduled for elective CABG surgery with Cardiopulmonary bypass (CPB). The study was done from February 2014 to April 2015 in the cardiac surgery unit and the open heart intensive care unit (ICU) of a teaching hospital affiliated with Mazandaran University of Medical Sciences, Sari, Iran. Preliminary selection of patients was based on non-randomly and due to be eligible to enter the study units. Approval from the Mazandaran University of Medical Sciences ethics committee, as well as informed consents from patients was obtained.
Inclusion criteria of this clinical study included non-emergency CABG surgery, and having stable hemodynamic (systolic blood pressure ≥90 mm Hg, the absence of dangerous dysrhythmias and HR between 60-100 beats in minutes). Patients with a history of chronic inflammatory diseases, endocarditis, adrenal insufficiency, sepsis, history of steroid use in the preceding six months, prolonged and difficult intubation (more than 30 seconds or more than 3 times), and combined cardiac valve surgery with CABG and Bentall surgery were excluded from this study. Patients who meet the inclusion criteria were randomly allocated to three groups A, B, and C (50 patients in each group) by the sealed envelope technique. Patient allocation was performed by a nurse who was unaware of the study groups, according to numbers generated by the computer-generated list for 150 patients.
In the operating room, Ringer lactate (5cc/kg) was infused via an intravenous line for all patients before induction of anesthesia and all patients underwent monitoring (temperature, invasive blood pressure (IBP) (left radial artery), central venous pressure (CVP), pulse oximetry, capnography and monitoring heart rhythm). Also, electrocardiogram, invasive arterial blood pressure, and pulse oximeter were applied for all patients and baseline systolic and diastolic blood pressure (SBP, DBP), mean arterial pressure (MAP) and HR were measured and recorded for all of them.
All patients received midazolam (0.03 mg/kg) and fentanyl (2µg/kg) intravenously as premedication. One minute later, patients in group A were induced with propofol (1.5 mg/kg), Group B was induced with etomidate (0.2 mg/kg) and Group C was induced with diazepam (0.3 mg/kg). All drugs were administered at the same speed and within 60-90 seconds. Drugs already were prepared in equal volumes separately by anesthetist who was not involved in this study and all syringes were covered with masking tape to conceal any details of the product. Loss of eyelash reflex was considered as the endpoint of anesthesia induction and also bispectral index (BIS) score between 40 and 60 was considered adequate to ensure adequate anesthesia depth. Then all patients received succinylcholine 1.5mg/kg for muscle relaxation and to facilitate intubation. Tracheal intubation performed one minute after succinylcholine administration.
SBP, DBP, MAP and HR were measured and recorded immediately before laryngoscopy and tracheal intubation and one and three minutes after intubation. Laryngoscopy and anesthesia administration were done by an anesthesiologist who was blinded to the study groups. The duration of laryngoscopy and intubation were recorded for each patient.
If the blood pressure decreased to less than 20% of a patient’s baseline, ephedrine (10 mg) was administered and and it was recorded in data collection sheet. In addition, demographic variables such as age and sex, Body Mass Index (BMI), history of drugs and disease (diabetes and hypertension) were recorded. This study registered in the Iranian Registry of Clinical Trials Database (IRCT2015082921669N2).
Statistical analysis
We used the Kolmogorov-Smirnov test to determine whether data were normally distributed. Statistical analysis of the data was performed by using the software 17 SPSS. Quantitative variables were analyzed by repeated measure analysis of variance (ANOVA), and Bonferroni test. A P value of 0.05 or less was considered statistically significant.
3. RESULTS
During the study, 164 patients were initially evaluated. Of these, 9 patients did not meet the inclusion criteria and 5 patients declined to participate in the study. All 150 patients completed the present study and data from all these patients were analyzed (Figure 1).
Figure 1.
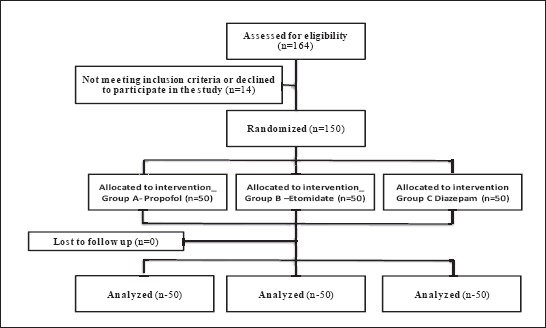
Flow chart of the study
The mean age of patients was 59.05 years with a standard deviation (SD) of 7.9 and minimum and maximum ages of 35 and 80 years respectively. In addition, 98 patients (65.3%) were male. The mean EF of patients in the three groups was 32.4% with a SD of 2.5 and duration of laryngoscopy was 22.5 seconds with SD of 9.6.
Kolmogorov-Smirnov test results showed that heart rate, mean arterial pressure, diastolic blood pressure, systolic blood pressure, age and EF had a normal distribution and using of the parametric test was permitted. According to the two-way ANOVA test, there was no difference between the interactions of gender with two groups on EF.
Table 1 shows that there were no statistically significant changes in HR, MAP, SBP, DBP and EF before intervention in three groups. In addition, there were no significant differences in laryngoscopy duration, age average and interaction of gender between three groups (Table 1).
Table 1.
Comparison of baseline hemodynamic variables between three groups before induction of anesthesia HR: heart rate; MAP: mean arterial pressure; SBP: systolic blood pressure; DBP: diastolic blood pressure; EF: ejection fraction

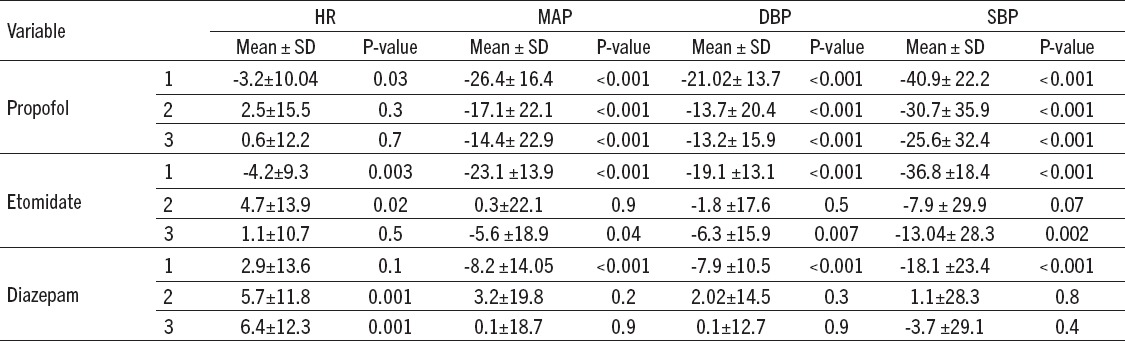
Table 2 shows the mean and SD of HR, MAP, SBP and DBP in all three groups of study before the intervention, one minute after hypnotic administration and prior to laryngoscopy and intubation, one and three minutes after laryngoscopy and intubation.
Table 2.
Change trends of hemodynamic parameters in the two groups during follow-up T1: Before the intervention; T2: one minute after hypnotic administration and prior to laryngoscopy and intubation; T3: one minute after laryngoscopy and intubation; T4: three minutes after laryngoscopy and intubation
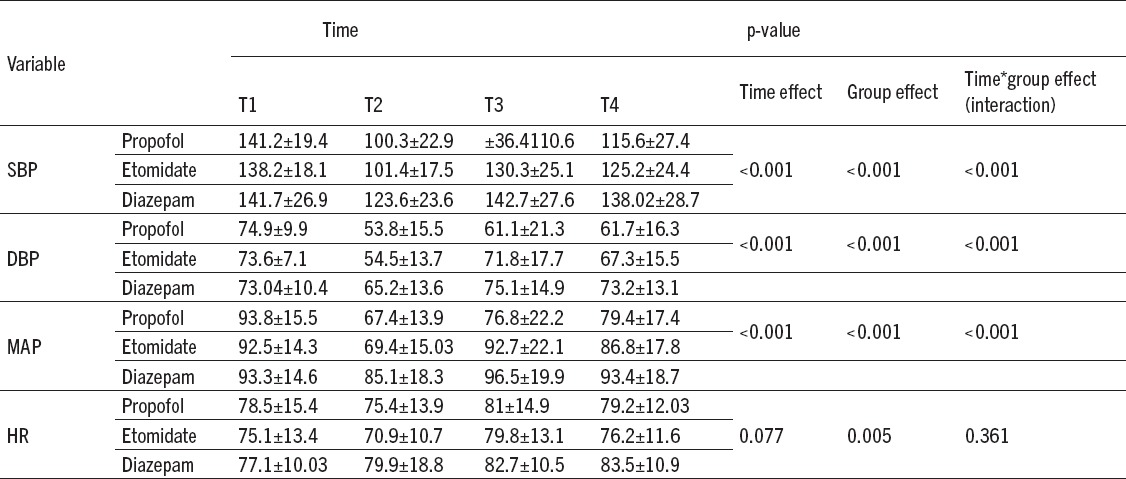
As shown in Table and Figure 2, there were a statistically significant time effect (within-subject effect) (P<0.001) for SBP, DBP and MAP in all three groups, indicating that when the three groups were combined, the average SBP, DBP, and MAP at baseline were higher than the average after induction times. There was a significant decrease from the baseline in MAP, SBP and DBP in one minute after administration of hypnotic and before laryngoscopy and intubation, in all three groups of the patient but these variables in each hemodynamic parameter in diazepam group were less than other two groups. Moreover, the mean HR decreased in patients receiving propofol and etomidate one minute after hypnotic administration and before laryngoscopy and intubation, but HR did not reduce in the diazepam group.
Figure 2.
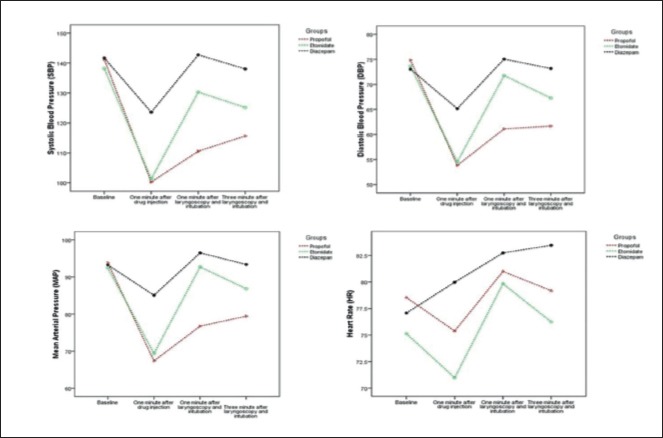
Change trends of hemodynamic parameters in the two groups during follow-up period
As depicted in Table and Figure 2, there were statistically significant difference between groups (between-subject differences or group effect) (p<0.001) for SBP, DBP, MAP, and HR. Moreover, a significant group-by-time interaction effect were also present for SBP, DBP and MAP (P=0.007), indicating that the magnitude of the differences between the 3 groups was not constant over time.
According to the results of ANOVA, significant differences in Heart rate were seen in all three groups, one minute after hypnotic administration and before laryngoscopy and intubation, and three minutes after laryngoscopy and intubation. Also, in all three groups, there was a significant difference following hypnotic administration and one and three minutes after laryngoscopy and intubation in MAP, SBP, and DBP (Table 3).
Table 3.
Adjusted mean HR, SBP, DBP and MAP in four measurements in the three groups (SD)
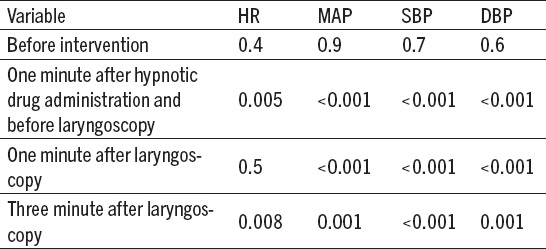
Mean HR, MAP, SBP and DBP variables one minute after hypnotic administration and before laryngoscopy and one and three minutes after laryngoscopy and intubation compared to before intervention and hypnotic administration are shown in Table 4.
Table 4.
Comparison the mean change of HR, MAP, DBP and SBP before intervention in each group (Paired T test)
Our study has revealed that 14(28%), 2(4%), and 1 (2%) of the patients that have received propofol, etomidate and diazepam required administration of the ephedrine because of the hemodynamic variations. This differences were statistically difference (P<0.001).
4. DISCUSSION
The prevalence of patients with compromised left ventricular function undergoing CABG is increasing. It is believed that CABG is a safe and effective treatment for patients with severe compromised left ventricular function with CAD (17). Cardiovascular stability is a crucial prerequisite for any anesthetic agent used for induction of anesthesia for patients undergoing CABG surgery, specifically for patients with poor cardiovascular reserve (18, 19). Several studies investigate the effects of a wide variety of induction agents in the patients CAD. We compared the hemodynamic responses to diazepam, propofol, and etomidate for anesthetic induction in these patients. The results of the present study showed more hemodynamic stability during anesthesia induction and intubation with using diazepam compared to propofol and etomidate.
In a study by Samuelson et al. aiming to examining the hemodynamic response to anesthesia induction by midazolam (0.2 mg/kg) or diazepam (0.5 mg/kg) in patients with ischemic heart disease. In patients who received midazolam, a significant but slight reduction was observed in systemic and pulmonary artery blood pressure, pulmonary hypertension, stroke index, and right and left ventricle stroke work index. While in patients receiving diazepam, only a significant decrease was observed in systemic blood pressure and a significant difference was seen between the two groups 5 minutes after drug administration. Following midazolam injection, HR increased but SBP and left ventricle stroke work index decreased. Both groups responded to the tracheal intubation through a temporary increase in BP, HR and systemic vascular resistance (SVR) and hemodynamic parameters turned to their normal states in 2 to 5 minutes. This study suggests that, despite some differences, midazolam may be as appropriate as diazepam for rapid induction and maintaining stable hemodynamic status in patients with ischemic heart disease (19), which is in line with the results of our study. The only difference is that in our study maintaining hemodynamic parameters in diazepam group was more significant than others.
In a study by Reza et al. to compare the effect of diazepam and midazolam on patients with CAD, 45 patients who were candidate for cardiac catheterization received 0.2 mg/kg midazolam and 30 patients received 0.4mg/kg diazepam intravenously. It has been shown that the decrease in SVR, DBP and left ventricular stroke work index was more significant in the midazolam group, but both groups expressed same changes in HR, pulmonary artery pressure, SBP and DBP, cardiac output, cardiac index, stroke volume index, pulmonary artery resistance and right ventricular stroke work index. Both drugs were, ultimately, described as “safe” for use in patients with CAD (16).
Findings of a study by Habibi et al. aiming to compare hemodynamic changes in patients under CABG with low EF during induction with etomidate or a combination of ketamine and thiopental, indicated no difference in MAP, DBP, SBP, and HR of patients before and immediately after (1, 2 and 3 minutes after) laryngoscopy among the two groups (18). In the present study, a reduction was observed in SBP, DBP, and MAP in all three studied groups of subjects after administration of hypnotic drugs, 1 minute before laryngoscopy as compared to before intervention. Blood pressure decreases following propofol administration may result from a reduction of SVR and cardiac output and effect of the drug on the sympathetic drive of heart; since propofol is a vasodilator drug degrading sympathetic activity (9). Decreasing in blood pressure after intimidate administration, may originate from the effect of the drug on gamma-Aminobutyric acid (GABA) receptors which results from a lack of impact on sympathetic system and activity of baroreceptors (with minimum influence on cardiovascular activity) (20). Diazepam can cause decrease MAP and SVR due to maintaining homeostatic reflexive mechanisms and these effects are resulted from suppression of sympathetic tonicity associated with GABA and nitric oxide (9).
The HR of patients receiving propofol and etomidate was lower than that of those induced with diazepam and this could be the result of lack of control on the sympathetic system by diazepam as compared to other two drugs. Meanwhile, benzodiazepines maintain HR, left ventricular filling pressure, and cardiac output after anesthesia induction (3, 6, 11). Moreover, diazepam has a nitroglycerine-like effect (preload reduction and increase of HR) and this is usually associated with filling pressure reduction and enhancement of cardiac output (9). MAP, SBP, and DBP in all studied groups increased 1 and 3 minutes after laryngoscopy and intubation and this may be considered as a consequence of pain and sympathetic stimulation resulting from laryngoscopy. So thatthe diazepam and propofol groups expressed the highest and the lowest amount of increase, respectively. In all groups, blood pressure decreased one minute after induction dose injection but this decrease in diazepam group was lower than others. While blood pressure in diazepam group went back to its initial value faster compared to other groups. After drug injection in diazepam group, HR increased one and three minutes after laryngoscopy and intubation, unlike other groups that initially HR dropped and then returned to initial values.
The reason for the return of BP, HR to baseline values may be due to pain and sympathetic stimulation caused by laryngoscopy and intubation. Furthermore, propofol led to the most significant increase in studied variables among 3 considered groups. In a study on examining the effect of etomidate and propofol on hemodynamic and endocrine responses in 60 candidate patients of CABG, Kaushal et al. showed that etomidate creates the better hemodynamic stability than propofol (6). This is consistent with results of our study in two groups (receiving propofol and etomidate).
In another clinical trial, evaluating hemodynamic effects of propofol and etomidate during rapid sequence tracheal intubation in non-surgery patients, it has been shown that changes in SBP, DBP, and HR in five minutes after tracheal intubation are lesser in etomidate group than propofol one and this is consistent with results of the present research (13). Findings of another study on patients undergoing elective surgeries showed that patients, who receive the propofol-etomidate combinations during anesthesia induction, had more hemodynamic stability compared to patients who received propofol-ketamine combination (21). This is while the present study proved diazepam is more successful than other drugs in maintaining hemodynamic stability.
A limitation of this study was that even though two groups were given the same premedication with midazolam (0.03 mg/kg) and fentanyl (2µg/kg), the dosages per kilogram body weight may be unequally distributed between groups, and thus the dosing of these premedication drugs may be a confounding variable.
5. CONCLUSION
The present study showed that in patients undergoing CABG surgery with low EF, diazepam is more favorable in terms of hemodynamic stability compared to propofol and etomidate and this drug can be used safely for induction of anesthesia in patients with impaired ventricular function in these patients.
Footnotes
• Conflict of interest: All authors declare no conflict of interest; no conflict of interest exists for any of the authors associated with the manuscript. The funding organization had no role in the design and conduct of the study, or in the collection, analysis, and interpretation of the data.
•Author’s contributions: Study conception and design: AS, NH, MRH, FHK, MK and AEZ. Acquisition of data: AS, NH, MRH, FHK, FBS. Statistical analysis and interpretation of data: AS, MK. Drafting of the manuscript: AS, NH, MRH, FHK, MK, AEZ, and FBS. Critical revision of the manuscript for important intellectual content: AS, NH, AEZ, MRH, and FHK.
•Clinical trial registration number: IRCT2015082921669N2.
REFERENCES
- 1.Gavrilovska-Brzanov A, Jarallah MA, Cogliati A, Mojsova-Mijovska M, Mijuskovic D, Slaveski D. Evaluation of the Hemodynamic Response to Endotracheal Intubation Comparing the Airtraq(®) with Macintosh Laryngoscopes in Cardiac Surgical Patients. Acta Inform Med. 2015;23(5):280–4. doi: 10.5455/aim.2015.23.280-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shapira OM, Hunter CT, Anter E, Bao Y, DeAndrade K, Lazar HL, Shemin RJ. Coronary artery bypass grafting in patients with severe left ventricular dysfunction - early and mid-term outcomes. J Card Surg. 2006;21(3):225–32. doi: 10.1111/j.1540-8191.2006.00221.x. [DOI] [PubMed] [Google Scholar]
- 3.Gholipour Baradari A, Alipour A, Habibi MR, Rashidaei S, Emami Zeydi A. A randomized clinical trial comparing hemodynamic responses to ketamine-propofol combination (ketofol) versus etomidate during anesthesia induction in patients with left ventricular dysfunction undergoing coronary artery bypass graft surgery. Arch Med Sci. [Access: March 09 2017]. doi:10.5114/aoms.2016.63193]. Available from: http://www.termedia.pl/A-randomized-clinical-trial-comparing-hemodynamic-responses-to-ketamine-propofol-combination-ketofol-versus-etomidate-during-anesthesia-induction-in-patients-with-left-ventricular-dysfunction-undergoi,19,28604,1,1.html . [DOI] [PMC free article] [PubMed]
- 4.Basagan-Mogo E, Goren S, Korfali G, Turker G, Kaya FN. Induction of anesthesia in coronary artery bypass graft surgery: the hemodynamic and analgesic effects of ketamine. Clinics. 2010;65(2):133–8. doi: 10.1590/S1807-59322010000200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siddiqui N, Katznelson R, Friedman Z. Heart rate/blood pressure response and airway morbidity following tracheal intubation with direct laryngoscopy, GlideScope and Trachlight: a randomized control trial. Eur J Anaesthesiol. 2009;26(9):740–5. doi: 10.1097/EJA.0b013e32832b138d. [DOI] [PubMed] [Google Scholar]
- 6.Kaushal RP, Vatal A, Pathak R. Effect of etomidate and propofol induction on hemodynamic and endocrine response in patients undergoing coronary artery bypass grafting/mitral valve and aortic valve replacement surgery on cardiopulmonary bypass. Ann Card Anaesth. 2015;18(2):172–8. doi: 10.4103/0971-9784.154470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iribarren JL, Jiménez JJ, Hernández D, Lorenzo L, Brouard M, Milena A, et al. Relative adrenal insufficiency and hemodynamic status in cardiopulmonary bypass surgery patients. A prospective cohort study. J Cardiothorac Surg. 2010;5:26. doi: 10.1186/1749-8090-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gooding JM, Weng JT, Smith RA, Berninger GT, Kirby RR. Cardiovascular and pulmonary responses following etomidate induction of anesthesia in patients with demonstrated cardiac disease. Anesth Analg. 1979;58(1):40–1. doi: 10.1213/00000539-197901000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Legrand M, Plaud B. Etomidate and general anesthesia: the butterfly effect? Anesth Analg. 2013;117(6):1267–9. doi: 10.1213/ANE.0000000000000003. [DOI] [PubMed] [Google Scholar]
- 10.Cherfan AJ, Arabi YM, Al-Dorzi HM, Kenny LP. Advantages and disadvantages of etomidate use for intubation of patients with sepsis. Pharmacotherapy. 2012;32(5):475–82. doi: 10.1002/j.1875-9114.2012.01027.x. [DOI] [PubMed] [Google Scholar]
- 11.Komatsu R, You J, Mascha EJ, Sessler DI, Kasuya Y, Turan A. Anesthetic induction with etomidate, rather than propofol, is associated with increased 30-day mortality and cardiovascular morbidity after noncardiac surgery. Anesth Analg. 2013;117(6):1329–37. doi: 10.1213/ANE.0b013e318299a516. [DOI] [PubMed] [Google Scholar]
- 12.Habibi MR, Hasanzadeh Kiabi F, Soleimani A, Emami Zeydi A. Sedation and analgesia during bone marrow aspiration in children: Is ketamine and propofol combination (Ketofol) an appropriate agent? Indian J Med Paediatr Oncol. 2013;34(4):337–9. doi: 10.4103/0971-5851.125268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aggarwal S, Goyal VK, Chaturvedi SK, Mathur V, Baj B, Kumar A. A comparative study between propofol and etomidate in patients under general anesthesia. Braz J Anesthesiol. 2016;66(3):237–41. doi: 10.1016/j.bjane.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 14.McClish A. Diazepam as an intravenous induction agent for general anaesthesia. Can Anaesth Soc J. 1966;13(6):562–75. doi: 10.1007/BF03002226. [DOI] [PubMed] [Google Scholar]
- 15.Singh R, Choudhury M, Kapoor PM, Kiran U. A randomized trial of anesthetic induction agents in patients with coronary artery disease and left ventricular dysfunction. Ann Card Anaesth. 2010;13:217–23. doi: 10.4103/0971-9784.69057. [DOI] [PubMed] [Google Scholar]
- 16.Raza SM, Masters RW, Zsigmond EK. Comparison of the hemodynamic effects of midazolam and diazepam in patients with coronary occlusion. Int J Clin Pharmacol Ther Toxicol. 1989;27(1):1–6. [PubMed] [Google Scholar]
- 17.Aghdaii N, Ziyaeifard M, Faritus SZ, Azarfarin R. Hemodynamic Responses to Two Different Anesthesia Regimens in Compromised Left Ventricular Function Patients Undergoing Coronary Artery Bypass Graft Surgery: Etomidate-Midazolam Versus Propofol-Ketamine. Anesth Pain Med. 2015;5(3):e27966. doi: 10.5812/aapm.27966v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Habibi MR, Baradari AG, Soleimani A, Emami Zeydi A, Nia HS, Habibi A, et al. Hemodynamic responses to etomidate versus ketamine-thiopental sodium combination for anesthetic induction in coronary artery bypass graft surgery patients with low ejection fraction: a double-blind, randomized, clinical trial. J Clin Diagn Res. 2014;8(10):GC01–5. doi: 10.7860/JCDR/2014/10237.5006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samuelson PN, Reves JG, Kouchoukos NT, Smith LR, Dole KM. Hemodynamic responses to anesthetic induction with midazolam or diazepam in patients with ischemic heart disease. Anesth Analg. 1981;60(11):802–9. [PubMed] [Google Scholar]
- 20.De Jong A, Jaber S. Etomidate for anesthesia induction: friends or foe in major cardiac surgery? Crit Care. 2014;18(5):560. doi: 10.1186/s13054-014-0560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moosavi Tekye SM, Pashang SM. Comparison of the hemodynamic effects of Etomidate versus propofol, Rapid Sequence Intubation, on none surgical patients. Med J Mashad Univ Med Sci. 2014;57(4):602–8. [Google Scholar]


