Abstract
Background
The purpose of this study is to assess the long-term follow-up of cementless total knee arthroplasty with the trabecular metal (TM) monoblock tibial component at an average 10-year follow-up. This report is an extension of our previously reported series of 108 TM tibias reported in 2011 (Unger and Duggan, 2011).
Methods
Fifty-eight of the original 108 knees were available for review. Each follow-up patient was evaluated by radiologic and clinical Knee Society Scores. The average follow-up was 10.2 years.
Results
Our results indicate excellent long-term survivorship (96.5%) with 2 confirmed tibia revisions, and 1 femoral revision for periprosthetic fracture and 1 patella open reduction internal fixation. X-ray evaluation demonstrated one patient with 1 mm medial polyethylene wear and a nonprogressive 1 mm of radiolucency on the medial side. All the other tibial components showed full bone apposition and incorporation. Knee Society Scores were excellent in all the patients seen on follow-up.
Conclusions
Long-term follow-up of TM monoblock tibia components confirm excellent survivorship and biologic implant fixation, with excellent outcomes and knee scores.
Keywords: Cementless knee arthroplasty, Trabecular metal, Porous tantalum, MIS knee arthroplasty, Uncemented knee arthroplasty
Introduction
The success of primary cemented total knee arthroplasty (TKA) is well established, with high survivorship and patient satisfaction [1]. Initial reports with cementless knees were unsatisfactory [2]. Newer implant design and materials, such as trabecular metal (TM), have been proposed to improve the results of cementless knees [3], [4].
TM has a high compressive strength and a low modulus of elasticity (3 GPa) that is comparable with trabecular bone (0.1-1.5 GPa) [5], [6]. It has a consistent, repeating, highly porous structure with mechanical properties similar to bone [5], [7]. The polyethylene bearing surface is direct compression molded to the TM. This unique design has been shown to eliminate backside wear and is mechanically resilient [8], [9]. These features may improve long-term survivorship in all populations receiving TKA.
Ghalayini and McLauchlan [10], in 2004, compared a consecutive series of TM tibia monoblock components with an older consecutive series of cemented components. Midterm results showed improved Knee Society Score (KSS) and only 1 revision at 27 months [11]. Minoda et al [12] reported on the bone mineral density in 28 knees receiving a TM tibial component vs a cemented component and found that there was a higher bone mineral density in the TM group, without a difference in KSS or migration.
Registry studies have reported excellent survivorship (100%) at 7 years for aseptic loosening as the primary end-point, and 97% survivorship with revision as the end-point for any reason [13]. In addition, Fernandez-Fairen et al's randomized controlled trial at 5-year follow-up, comparing one group that received a porous tantalum cementless tibial component with a cemented conventional tibial component, reported an increased KSS in the cementless TM group (90.4 ± 1.6 vs 86.5 ± 2.4) [14]. Favorable biomechanical characteristics of TM have shown excellent and rapid ingrowth, and a large prospective study at midterm follow-up showed 100% survivorship and ingrowth [15]. However, concerns do exist in regards to removing a well-fixed ingrown component. When removing any TM ingrown component, whether for instability, infection, or other mechanical etiologies, the goal is to preserve as much bone stock as possible, using the techniques as described by Klein et al [16]. There are case reports of early aseptic loosening of TM components. Tigani et al [17] noted painful aseptic loosening at 7 months postoperative from a primary TKA using TM tibial components. On revision, the authors noted complete lack of ingrowth of the TM tibia component. Etiologies proposed were the age of the patient and possible osteopenia providing a nonfavorable environment for ingrowth, a tibial cut that still showed evidence of sclerotic bone, thus not providing rich cancellous bone suitable for ingrowth, and lastly a type IV hypersensitivity reaction with an abundant lymphocyte response observed perhaps preventing ingrowth. The patient subsequently had a successful revision cemented TKA with relief of pain.
In 2011, the midterm results of a porous tantalum monoblock tibia component of 108 knees was reported, with good/excellent results in 105 knees, and improvement in average KSS from 36-89, with 2 revisions for loose components [18].
The purpose of this study is to analyze clinical and radiographic outcomes at a minimum follow-up of 10 years of the initial cohort of 108 knees that received a TM monoblock tibia component. The hypothesis is that this implant has excellent long-term survival while maintaining good/excellent scores.
Material and methods
Our initial cohort of 95 patients (108 knees) underwent minimally invasive surgery (MIS) TKA from March 2003-2006 with an uncemented porous tantalum monoblock tibia component. The primary indication for surgery was degenerative joint disease with significant pain and disability not responsive to conservative treatment [18]. All patients had a preoperative flexion of at least 115° with minimal deformity (valgus/varus <10°). Body mass index was not an exclusion criterion and all patients enrolled had intact posterior cruciate ligaments by clinical examination. Patients with more deformity (>10° varus/valgus), radiographic osteopenia, previous surgery, and bone loss underwent a standard cemented TKA with a posterior-stabilized implant and were excluded from this study. All procedures were performed with the MIS technique by a single surgeon using a standard medial parapatellar approach [18] with a mechanical axis referencing technique. The primary surgeon had completed 50 total knees with TM tibia components before study initiation.
At an average 10-year follow-up (range 8.4-12.2 years), 11 men (23%) and 36 women (77%), 58 knees were available for evaluation. Ten patients included underwent simultaneous bilateral TKA. The mean age was 71.1 ± 9.95 years (range 35-89 years). The average body mass index was 30.2 kg/m2 (range 18.3-49.9 kg/m2), average weight was 173 lbs (range 130-210 lbs), and preoperative knee range of motion was 127° (118°-139°) (Table 1). Of the initial 108 cohorts, 28 patients were lost to follow-up, 11 patients were contacted by phone but unable to return to clinic, 6 patients reported outcome scores by phone and sent in recent x-rays for evaluation, and 5 patients were deceased (Table 2). These patients are categorized as “unconfirmed” from the inability to examine the patient in the office and/or obtain radiographs or operative reports.
Table 1.
Patient demographics and complications.
| Original | 11-y follow-up | |
|---|---|---|
| Total knees | 108 | 58 |
| Total patients | 95 | 47 |
| Avg F/U | 4.5 | 10.2 |
| Avg age | 65 | 71.1 |
| Avg BMI | 30.2 | |
| KSS score diff | 36-->89 | 36.45-->99.2 |
| Excellent/good rating | 105 | 58 |
| Poor rating | 3 | 0 |
| Patellar revision loose component | 2 | 2 |
| Patellar revision misalignment | 1 | 1 |
| Patellar ORIF | 1 | 1 |
| Femoral revision | 1 | 2 |
| Tibial revision | 0 | 2 |
| Unknown revision | 0 | 4 |
BMI, body mass index; KSS, Knee Society Score; F/U, follow up; ORIF, open reduction internal fixation.
Table 2.
Patient follow-up and revisions.
| Original Cohort (=n) | 11 Year Follow up (=n) | |
|---|---|---|
| Total follow-upa | 6 | 58 |
| Revision total | 5 | 7 |
| Revision nontibial loosening unconfirmed | X | 2 |
| Revision tibial loosening unconfirmed | X | 3 |
| Revision tibial loosening confirmed | X | 2 |
| Phone call only | 4 | 11 |
| Phone call + x-ray | 3 | 6 |
| Deceased | 2 | 5 |
| Lost to follow-up | 1 | 28 |
1 patient 1 mm medial polyethylene wear + 1 mm tibial radiolucency.
Surgical technique
All TKAs were performed as previously described through a minimally invasive midvastus approach [18]. An uncemented TM monoblock tibial component and a cruciate-retaining, uncemented, high flex femoral component was used in all patients. Every patient had a well-padded tourniquet placed. In each case, the quadriceps tendon remained intact and the patella was translated laterally. Intramedullary referencing was used for the femur, with extramedullary guides for the tibia cuts, and a freehand cut for the patella. All flexion and extension gaps were symmetric before implant insertion of the uncemented TM monoblock tibial component system (Fig. 1). All cases received an uncemented cruciate-retaining high flex femoral component and the patella was resurfaced in all cases. Every knee had a single deep drain placed and the arthrotomy was closed with absorbable sutures.
Figure 1.
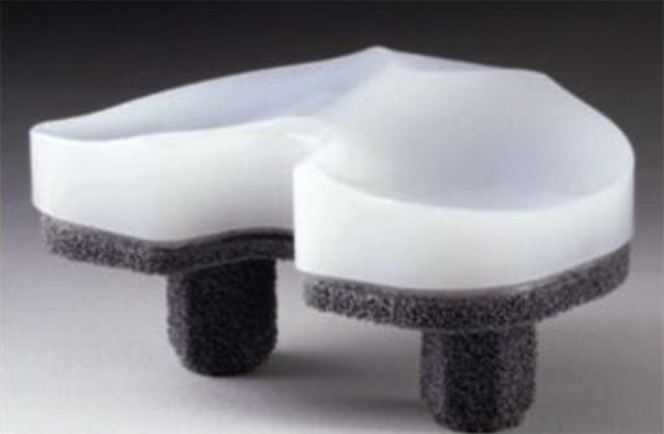
Uncemented TM tibia monoblock.
The postoperative protocol included low-molecular weight heparin or warfarin for 4 weeks as was customary. The drains were all removed postoperative day 1 and physical therapy was begun postoperative day 1. Patients were discharged to either a rehabilitation unit or home with therapy using a team discharge approach (protocol) with nursing, physical therapy, and occupational therapy.
Our long-term follow-up was an average of 10.2 years. In all cases, the operative surgeon completed a follow-up Knee Society Score and repeat x-rays of the operative knee were obtained and scrutinized for subsidence, interval changes, and/or radiolucencies using the Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System [19]. Our postoperative protocol has been previously described with radiographs at 6 weeks, 6 and 12 months, then at 12 months intervals thereafter.
The end-point for survival was defined as revision of the tibia component. Kaplan-Meir survival analysis was performed for all revisions, revisions for confirmed tibial loosening/failure, revisions for extensor mechanism failure, and revisions for unconfirmed revision. Given our age population and the characteristics of a long-term follow-up study, there were 5 patients who stated they underwent total knee revision, but we were unable to confirm the cause or reason for revision without radiographs or operative reports. Two patients underwent tibial revision for loosening confirmed by radiographs or operative reports.
Results
The KSS evaluation
Pre- and postoperative KSS were calculated in all patients at final follow-up. The mean preoperative objective score from the initial cohort was 36 and the mean preoperative functional score was 46. At final follow-up 10.2 years (range 8.4-12.2 years), the mean postoperative KSS was 99.2 ± 2.97 and the mean KSS function score was 97.4 ± 12.9. The total average KSS was 98.3 ± 7.0. The KSS at final follow-up rated all 58 knees as good and/or excellent.
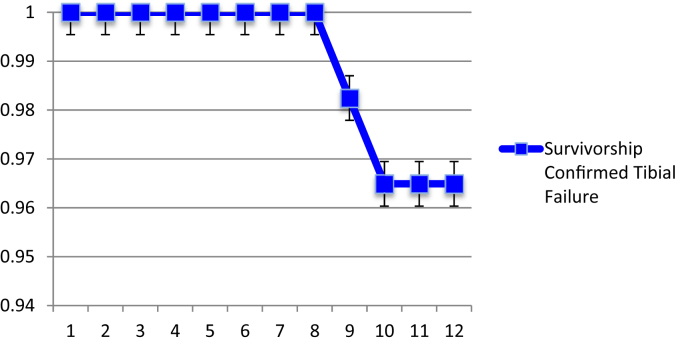
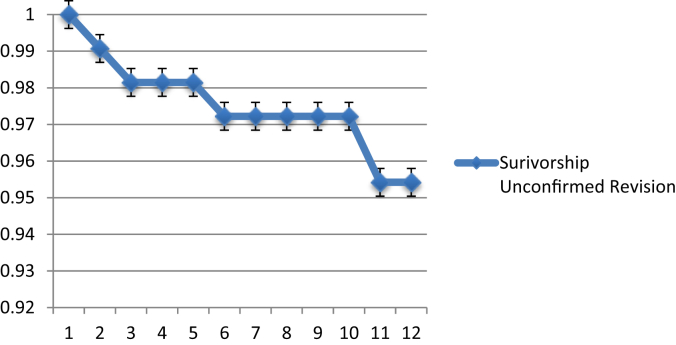
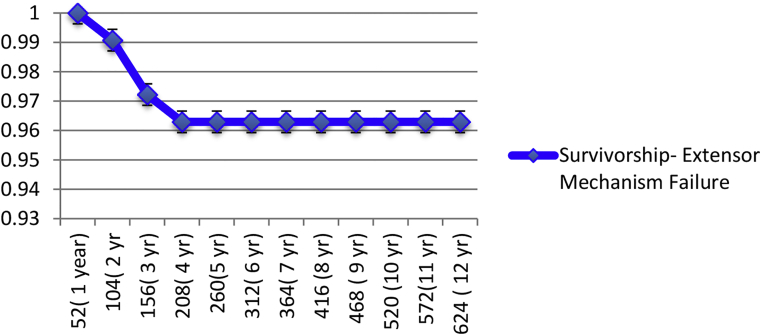
Clinical evaluation/survivorship
Fifty-eight knees were available for follow-up in 47 patients. The average postoperative flexion from the KSS was “maximum” (between 121° and 125°) for all 58 knees. Using Kaplan–Meir Curve analysis, survivorship for confirmed tibia failure necessitating revision was 100%, 100%, and 96.5% at 1, 5, and 10 years, respectively (Fig. 2). The survivorship for all revisions including the unconfirmed patients was 95% at 10 years (Fig. 3). Kaplan-Meir survivorship with extensor mechanism failure as an end-point was 100%, 96%, and 96% at 1, 5, and 10 years, respectively (Fig. 4).
Figure 2.
Survivorship-confirmed tibia revision (n = 2).
Figure 3.
Survivorship-unconfirmed revision (n = 4).
Figure 4.
Survivorship extensor mechanism failure (n = 4).
Radiographic assessments
All patients underwent routine AP and lateral knee radiographs at follow-up. The postoperative radiographs were reviewed by the primary surgeon for new radiolucencies or progression of previously noted radiolucencies or subsidence. All the TM tibia components that previously demonstrated stability continued to demonstrate healthy osseous integration into the TM interface (Fig. 5), without evidence of metallic debris. One knee showed 1 mm of radiolucency under the medial flange, as well as 1 mm of medial polyethylene wear. This radiolucency was nonprogressive. We previously reported that one of the components had a progressive settling of 8 mm at 3-year follow up, but had been stable on last follow-up. Unfortunately, that patient was lost to follow-up.
Figure 5.

Implanted TM tibia component.
Discussion
TM tibia components are durable with excellent bone ingrowth [20], higher knee scores [21], and long-term survivorship [22]. Historically, cementless fixation has had a high rate of failure for TKA, with only 50% survival at 5 years in early designs [23]. Screw holes in tibia baseplates may contribute to osteolysis and porous surfaces that do not have enhanced ingrowth characteristics may have contributed to early failure. Our surgical technique used tibia and femoral components that were uncemented. The original FDA approval for the TM monoblock tray called for a partial cementing technique, where the TM monoblock tibia was fixed with cement under the tibial tray while the hexagonal tibial pegs were left uncemented [24]. It was the primary authors decision from the original study to challenge the survivorship and fixation strength of TM, and thus cement was not used.
Recently, long-term studies have shown success with cementless fixation. Ritter and Meneghini reported 98.6% survivorship at 20 years [25], and Schroder et al reported 97% survivorship for cementless porous-coated TKA at 10 years [26].
Highly porous metallic surfaces such as TM provide promising clinical outcomes compared with standard cemented TKA. Henricson et al [27] reported that TM components, measured by radiostereographic analysis, migrated during the first 3 months, but stabilized. Wilson et al [20], using radiostereometric analysis (RSA) comparing TM with cemented components, showed that the displacement with TM component was nonprogressive and all patients had bony ingrowth.
The mechanical properties of TM allow for rapid bony ingrowth and stable fixation at long-term [13], [15]. However, there are concerns of early migration, with a possible increased risk of aseptic loosening due to migration. Early postoperative migration of TM components has been demonstrated, with subsequent stabilization of the components over time without increased risk of aseptic loosening [27], [28], [29]. Dunbar et al [30] reported in their prospective randomized trial comparing cemented total knee implants with uncemented TM components, using RSA analysis, that nearly 32% of the subjects in the TM group did show evidence of migration >1 mm. However, all components had stabilized at final follow-up, and none, compared with the cemented group, were at risk for aseptic loosening [30]. We demonstrated in one patient rapid settling and migration of the implant in the early postoperative period, but the implant had stabilized at 3-year follow-up. Unfortunately, this patient was lost to long-term follow-up. Our long-term results are similar, in that only 1 patient showed 1 mm of medial lucency, and no tibias showed progression of subsidence or radiolucencies. Other reports using RSA for early migration and demonstrating subsequent stabilization has been shown. In the studies by Henricson et al [28], [29], they compared a cohort of uncemented TM tibial components with standard cemented TKA. They reported that although both groups showed evidence of migration within the first 3 months, all had stabilized and were nonprogressive at 5 years and 10 years. Further Pulido et al [24] demonstrated that highly porous TM tibia components provided durable fixation and pain relief with restoration of function compared with cemented modular tibia in TKA.
One well published concern with porous tantalum, as seen in glenoid components for reverse total shoulder arthroplasty is shedding of metallic debris over time. Recent studies evaluating porous tantalum glenoid components for reverse total shoulder arthroplasty continue to report high shedding of metallic debris, with an increased incidence and severity over time at short and midterm follow-up [31]. Our data and follow-up radiographs did not note any metallic debris in any patient at long-term follow-up.
The directed molded polyethylene on porous TM tibias theoretically eliminates the potential for backside wear. Given the biomechanical benefits of having an implant similar to that of trabecular bone, TM is an ideal implant choice for longevity and an implant material with an expected prolonged survivorship. The unique characteristics of TM may prevent bone loss over time, decrease subsidence, as has been shown in this study, and provide improved bone surface area for the revision surgeon.
Outcomes on registry analyses performed also demonstrate excellent survivorship of TM knees at mid and long-term follow-up. Neimelainen et al [13] showed that an uncemented porous TM tibial component had excellent midterm survivorship at 7 years. In their cohort of 1143 patients with TM components, only 1 knee was revised due to aseptic loosening of the tibial components, and other revisions (n = 20) were due to tibiofemoral instability with or without malposition (n = 12), then prosthetic joint infection (n = 7). Their survivorship using component loosening as an end-point was 100% at 1, 5, and 7 years. When comparing cemented vs TM tibia components, Dunbar et al [30] in their prospective randomized study, using radioisometric analysis, found no risk of progressive subsidence or loosening at 24 months, compared with 0.2% risk in the cemented cohort. Kwong et al reported at a mean follow-up of 7 years (2-11 years) a 95.7% survival of TM tibias, with no radiographic evidence of loosening and no osteolysis [32].
This study reports the radiographic and clinical assessment data on a cohort of 58 knees that were previously reported for short-medium term follow-up of TM tibia components implanted in an MIS technique [18]. Our data indicate that patients have good-excellent long-term outcomes based on fixation, improved KSS, and long-term survivorship at 1, 5, and 10 years is possible. A recent long-term follow-up study by De Martino et al [22] using TM tibia monoblock components, with similar cohorts, also confirms excellent long-term survivorship: Revision for any reason 96.9%, with no tibias revised for aseptic loosening requiring revision at a minimum of 10 years. In our original cohort of 108 TM tibias, there were no deep infections and 1 superficial infection. At final follow-up, there were no revisions for infection in the cohort of 58 knees. TM does not change the incidence of infection in TKA.
The limitations that exist in this study are its retrospective nature and a small cohort of patients. As a long-term follow-up study, a large number of patients were lost to follow-up (n = 28). Five were deceased from the initial cohort. Secondly, continued follow-up is difficult in our geographic area that is very transient, and many patients now live out of state and were unable to return. However, most patients who relocated and were contacted on the phone reported no complaints, with 5 patients reporting revision surgery. We recommend continued use of TM for TKA, as evidence shows that long-term durability is possible.
Conclusions
Our long-term follow-up study of TM monoblock tibia components demonstrate excellent survivorship of biologic implant fixation. TM components may be a viable alternative to traditional cemented tibia components for survivorship, and display a very low aseptic loosening rate. We report an aseptic loosening rate of 1.7% in our cohort of TKA patients receiving TM implants. Additional local and systemic complications were rare, with no infections, 1 femur revision due to fracture, and 4 extensor mechanism disruptions leading to reoperations, all within the first 5 years. Given recent literature supporting TM use and its longevity, with excellent biologic ingrowth and fixation, TM components can improve survivorship and outcomes in TKA patients.
Acknowledgments
The research team and Dr. Unger would like to thank Dr. R. Pandarinath for his contribution to this manuscript.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2017.02.004.
This study was funded by The Alma and Joseph Gildenhorn Orthopaedic Fund.
Appendix A. Supplementary data
References
- 1.NIH Consensus Panel NIH Consensus Statement on Total Knee Replacement. December 8-10, 2003. J Bone Joint Surg Am. 2004;86-A:1328. doi: 10.2106/00004623-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 2.Berger R.A., Lyon J.H., Jacobs J.J. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res. 2001;(392):196. doi: 10.1097/00003086-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Naudie D.R., Ammeen D.J., Engh G.A. Wear and osteolysis and total knee arthroplasty. J Am Acad Orthop Surg. 2007;15:53. doi: 10.5435/00124635-200701000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Thiele K., Perka C., Matziolis G., Mary H. Current failure mechanisms after knee arthroplasty have changed. Polyethylene wear is less common in revision surgery. JBJS. 2015;97(9):715. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 5.Bobyn J.D., Stackpool G.J., Hacking S.A. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907. doi: 10.1302/0301-620x.81b5.9283. [DOI] [PubMed] [Google Scholar]
- 6.Balla V.K., Bose S., Davies N.M., Bandyopadhyay A. Tantalum - a bioactive metal for implants. JOM. 2010;62(7):61. [Google Scholar]
- 7.Minoda Y., Kobayashi A., Ikebuchi M. Porous tantalum tibial component prevents periprosthetic loss of bone mineral density after total knee arthroplasty for five years - a matched cohort study. J Arthroplasty. 2013;28(10):1760. doi: 10.1016/j.arth.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 8.Poggie RA, Cohen RC, Averill RG. Characterization of a porous metal, direct compression molded UHMWPE junction. Presented at the annual meeting of the ORS, New Orleans, LA, March; 1998.
- 9.Florio CS, Poggie RA, Sidebotham C, et al. Stability characteristics of a cementless monoblock porous tantalum tibial implant without ancillary fixation. Presented at the annual meeting of the ORS, San Francisco, CA, March; 2004.
- 10.Ghalayini S., McLauchlan G.J. Early results of a trabecular metal tibial component in total knee replacement. J Bone Joint Surg Br. 2015;87-B(Supp II):145. [Google Scholar]
- 11.Ghalayini S.R., Helm A.T., McLauchlan G.J. Minimum 6-year results of an uncemented trabecular metal tibial component in total knee arthroplasty. Knee. 2012;19:872. doi: 10.1016/j.knee.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Minoda Y., Kobayashia A., Iwaki H. Comparison of bone mineral density between porous tantalum and cemented tibia total knee arthroplasty components. J Bone Joint Surg Am. 2010;92(3):700. doi: 10.2106/JBJS.H.01349. [DOI] [PubMed] [Google Scholar]
- 13.Niemelainen M., Skytta E.T., Remes V., Makela K., Eskelinen A. Total knee arthroplasty with an uncemented trabecular metal tibial component: a registry-based analysis. J Arthroplasty. 2014;29:57. doi: 10.1016/j.arth.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez-Fairen M., Hernandez-Vaquero D., Murcia A., Torres A., Llopis R. Trabecular metal in total knee arthroplasty associated with higher knee scores: a randomized controlled trial. Clin Orthop Relat Res. 2013;471:3543. doi: 10.1007/s11999-013-3183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okeefe T., Winter S., Lewallen D., Robertson D., Poggie R. Clinical and radiographic evaluation of a monoblock tibial component. J Arthroplasty. 2010;25(5):785. doi: 10.1016/j.arth.2009.05.029. [DOI] [PubMed] [Google Scholar]
- 16.Klein G.R., Levine H.B., Hartzband M.A. Removal of a well fixed trabecular metal monoblock tibial component. J Arthroplasty. 2008;23(4):619. doi: 10.1016/j.arth.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Tigani D., Sabbioni G., Raimondi A. Early aseptic loosening of a porous tantalum knee prosthesis. Musculoskelet Surg. 2009;93:187. doi: 10.1007/s12306-009-0047-x. [DOI] [PubMed] [Google Scholar]
- 18.Unger A.S., Duggan J.P. Midterm results of a porous tantalum monoblock tibia component clinical and radiographic results of 108 knees. J Arthroplasty. 2011;26(6):855. doi: 10.1016/j.arth.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 19.Ewald F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;(248):9. [PubMed] [Google Scholar]
- 20.Wilson D.A., Richardson G., Hennigar A.W. Continued stabilization of trabecular metal tibial monoblock total knee arthroplasty components at 5 years-measured with radiostereometric analysis. Acta Orthop. 2012;83(1):36. doi: 10.3109/17453674.2011.645196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lachiewicz P.F. Cement versus cementless total knee replacement: is there a place for cementless fixation in 2001? Curr Opin Orthop. 2001;12:33. [Google Scholar]
- 22.De Martino I., D'Apolito R., Sculco P.K. Total knee arthroplasty using cementless porous tantalum monoblock tibial component: a minimum 10-year follow up. J Arthroplasty. 2016;31(10):2193. doi: 10.1016/j.arth.2016.03.057. [DOI] [PubMed] [Google Scholar]
- 23.Dorr L.D. Fixation for the millennium—the knee journal. J Bone Joint Surg Br. 2002;84-B:172. [Google Scholar]
- 24.Pulido M.P., Lewallen D.G., Stuart M.J. The Mark Coventry Award: trabecular metal tibial components were durable and reliable in primary total knee arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2015;473(1):34. doi: 10.1007/s11999-014-3585-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ritter M., Meneghini R. Twenty-year survivorship of cementless anatomic graduated component total knee arthroplasty. J Arthroplasty. 2010;25(4):507. doi: 10.1016/j.arth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 26.Schroder H., Berthelsen A., Hassani G., Hansen E., Solgaard S. Cementless porous-coated total knee arthroplasty: 10-year results in a consecutive series. J Arthroplasty. 2001;16(5):559. doi: 10.1054/arth.2001.23565. [DOI] [PubMed] [Google Scholar]
- 27.Henricson A., Linder L., Nilsson K.G. A trabecular metal tibial component in total knee replacement in patients younger than 60 years: a two-year radiostereophotogrammetric analysis. J Bone Joint Surg Br. 2008;90(12):1585. doi: 10.1302/0301-620X.90B12.20797. [DOI] [PubMed] [Google Scholar]
- 28.Henricson A., Nilsson K.G. Trabecular metal tibial knee component still stable at 10 years: an RSA study of 33 patients less than 60 years of age. Acta Orthop. 2016;87(5):504. doi: 10.1080/17453674.2016.1205169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henricson A., Rösmark D., Nilsson K.G. Trabecular metal tibia still stable at 5 years: an RSA study of 36 patients ages less than 60 years. Acta Orthop. 2013;84(4):398. doi: 10.3109/17453674.2013.799418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dunbar M.J., Wilson D.A., Hennigar A.W. Fixation of a trabecular metal knee arthroplasty component. A prospective randomized study. J Bone Joint Surg Am. 2009;91:1578. doi: 10.2106/JBJS.H.00282. [DOI] [PubMed] [Google Scholar]
- 31.Endrizzi D.P., Mackenzie J.A., Henry P.D. Early debris formation with a porous tantalum glenoid component: radiographic analysis with 2-year minimum follow-up. J Bone Joint Surg Am. 2016;98(12):1023. doi: 10.2106/JBJS.15.00410. [DOI] [PubMed] [Google Scholar]
- 32.Kwong L.M., Nielsen E.S.N., Ruiz D.R. Cementless total knee replacement fixation: a contemporary durable solution-affirms. Bone Joint J. 2014;96-B(11 Suppl A):87. doi: 10.1302/0301-620X.96B11.34327. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.