Abstract
This is a rare case of serpine gene polymorphism causing thrombophilia and recurrent implantation failure following intrauterine insemination. SERPINE1 gene encodes plasminogen activator inhibitor type 1 and inhibits fibrinolysis, or clot dissolution. The 4G variant results in increased expression of SERPINE1 and consequently higher inhibition of fibrinolysis, thus leading to thrombophilia. The patient had unexplained primary infertility for 9 years. Ovulation induction was done with gonadotropin releasing hormone (GnRH) agonist long protocol. Recombinant follicle stimulating hormone (FSH) with step down protocol was used. Ovulation trigger was given with recombinant human chorionic gonadotrophin (HCG). Ovum pick up was done after 40 h of trigger. A total of 13 eggs were collected. Patient was put on Cabergoline to prevent ovarian hyperstimulation syndrome (OHSS). Four frozen embryos were transferred on day 14 after Laser-assisted hatching. EmbryoGlue was used to prevent implantation failure. Luteal phase support was given. She was put on enoxaparin and pregnancy has now been confirmed. The patient was on strict monitoring as this gene is also associated with preeclampsia during pregnancy.
KEYWORDS: Embryo–endometrial interphase, placental bed, preeclampsia genetic basis, serpine gene polymorphism
INTRODUCTION
Serpine1 plasminogen activator inhibitor-1 (PAI-1, 4G/5G) member is the principal inhibitor of tissue plasminogen activator and urokinase, and hence is an inhibitor of fibrinolysis. Defects in this gene [Serpine1 (PAI-1, 4G/5G) variant] are the cause of PAI-1 excess, and high concentrations of this gene product inhibit fibrinolysis and cause thrombophilia. Alternatively, spliced transcript variants encoding different isoforms have been found for this gene. Defects in serpine1 are the main cause of PAI-1 excess, which is characterized by thrombophilia.[1] Plasminogen activator gets inhibited leading to decreased plasmin and less fibrin dissolution and impaired invasion of extracellular matrix and altered cell migration.[2]
This case is highlights the role of low molecular weight heparin in implantation failure. Laser-assisted hatching in frozen embryo transfer may help in patients of PAI excess due to serpine gene polymorphism. Embryo transfer Media containing hyaluronic acid may have a role in cases of genetic defects of defective extracellular matrix degradation.
CASE HISTORY
Mrs. R, aged 30, had primary infertility for 9 years with 6 intrauterine insemination (IUI) failures. Her anti mullerian hormone (AMH) was 4.94 ng/ml. Hysteroscopy study of endometrium was normal [Figure 1]. Thrombophilia gene panel was investigated.
Figure 1.

Hysteroscopy of uterine endometrium and cavity
Patient had SERPINE1-816 5G/4G heterozygous genotype with one normal allele and one variant allele. Ovulation induction was done with GnRh agonist long mini-dose protocol Buserelin 0.001 mg/kg (Suprefact Injection Solution, Sanofi-Aventis New Zealand Limited, Ellerslie Auckland, New Zealand) long protocol started from day 21. Buserelin dose was decreased to 0.005 mg/kg on day 1. Recombinant FSH 150 IU was started on day 1. FSH was stepped down to 112.5 IU after day 8 when follicles were 14 mm. Ovulation trigger was given with recombinant HCG 250 µg on day 12 when multiple follicles of 17 to 20 mm were seen. Ovum pick up was done after 40 h of trigger. Thirteen eggs were collected. Patient was put on Cabergolin orally 0.05 mg at bedtime for 8 days (Generic Dostinex, Caberlin by Sun Pharma, Mumbai, Maharashtra) to prevent OHSS.
In the next cycle, the endometrium was prepared with estrogens. Four frozen day 3 embryos at 8-cell stage (Grade 1) were transferred on day 17 of estrogen and day 3 of progesterone after Laser-assisted hatching [Figure 2]. EmbryoGlue (Vitrolife, Göteborg, Sweden) (containing hyaluronic acid) in embryo transfer media was used to prevent implantation failure. Luteal phase support was given. She was put on enoxaparin from the day of embryo transfer. The patient was on strict monitoring as this gene is also associated with preeclampsia during pregnancy. At 34 weeks, she developed gestational hypertension. There was no proteinuria. The blood pressure was controlled with rest and diet. She delivered a live healthy baby by cesarean section at term. Postpartum blood pressure was normal.
Figure 2.
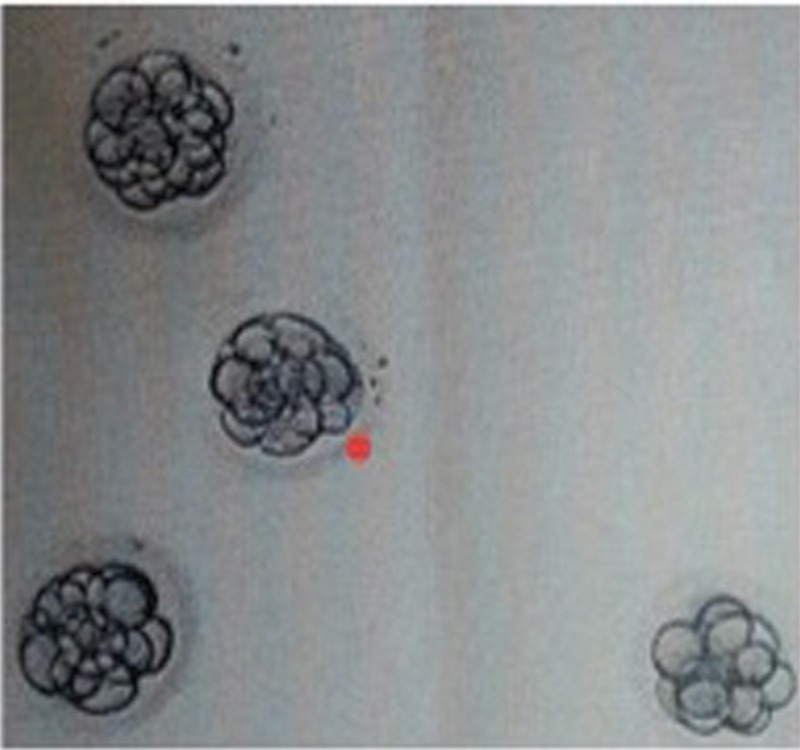
Laser assisted hatching helps in implantation as the freeze all protocol may lead to Zona Hardening
DISCUSSION
The polymerase chain reaction (PCR) test categorizes individuals for risk of thrombophilia by genotyping Factor V (Leiden, 1691G>A), Factor II prothrombin (20210G>A), and SERPINE1 (PAI-1, 4G/5G) variations using allele-specific real-time PCR. The method has almost 100% analytical accuracy and sensitivity. Variants or genes other than the ones mentioned are not tested. Very rarely the test may give inconclusive, clinical false positive, or false negative results. (BSH 2011, Clinical guideline in British Journal of Haematology; ASRM 2012, Committee Opinion in Fertility and Sterility; RCOG 2011, Green-top Guideline 17)
Thrombophilia, or hypercoagulability, refers to the increased tendency of blood to clot. Among the frequent causes of inherited thrombophilia are mutations in Factor V, Factor II prothrombin, and SERPINE1.[3,4] Pregnancy is by itself a thrombophilia condition. The presence of these mutations increases clotting events, which may lead to recurrent pregnancy loss (early and/or late), preeclampsia (high blood pressure), intrauterine growth restriction, and stillbirth. About 15 to 60% of infertile women were found to have one or more mutations predisposing to thrombophilia. Other contributors to thrombophilia include protein C, protein S, antithrombin, and antiphospholipid antibodies, which may be tested by protein-based assays. Close monitoring and thromboprophylaxis in these women may be beneficial during pregnancy.
This polymorphism is also associated with preeclampsia. Meta-analysis of 11 studies involving 1297 preeclampsia cases and 1791 controls found a significant association between the SERPINE1-675 4G/5G polymorphism and preeclampsia for the recessive genetic model [odds ratio (OR) = 1.36, 95% confidence interval (CI): 1.13–1.64, P = 0.001], a robust finding according to sensitivity analysis.[5,6,7]
Thrombophilia gene profile (including serpine1) is a cost effective method to be included in patients diagnosed to have recurrent clinical and subclinical pregnancy losses. Plasmin has a role in fibrin degradation, extracellular matrix remodeling, and cell migration. Genetic factors cannot be modified but adding adjuvants to improve the microenvironment of embryo–endometrial interphase can help. Recurrent implantation failure and placental bed disorders, resulting in preeclampsia, may have a common genetic basis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors thank Dr. Sooraj Swagene Lab, Chennai, for testing the female genetic infertility thrombophilia panel.
REFERENCES
- 1.Chen H, Nie S, Lu M. Association between plasminogen activator inhibitor-1 gene polymorphisms and recurrent pregnancy loss: a systematic review and meta-analysis. Am J Reprod Immunol. 2015;73:292–300. doi: 10.1111/aji.12321. [DOI] [PubMed] [Google Scholar]
- 2.Dossenbach-Glaninger A, Van Trotsenburg M, Schneider B, Oberkanins C, Hopmeier P. ACE I/D polymorphism and recurrent first trimester pregnancy loss: interaction with SERPINE1 4G/5G and F13 Val34Leu polymorphisms. Br J Haematol. 2008;141:269–71. doi: 10.1111/j.1365-2141.2008.07058.x. doi:10.1111/j.1365-2141.2008.07058.x. [DOI] [PubMed] [Google Scholar]
- 3.Goodman CS, Coulam CB, Jeyendran RS, Acosta VA, Roussev R. Which thrombophilic gene mutations are risk factors for recurrent pregnancy loss? Am J Reprod Immunol. 2006;56:230–6. doi: 10.1111/j.1600-0897.2006.00419.x. doi:10.1111/j.1600-0897.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 4.Magdoud K, Herbepin VG, Touraine R, Almawi WY, Mahjoub T. Plasminogen activatorinhibitor 1 4G/5G and 844G A variants inidiopathic recurrent pregnancy loss. Am J Reprod Immunol. 2013;70:246–52. doi: 10.1111/aji.12116. [DOI] [PubMed] [Google Scholar]
- 5.Khosravi F, Zarei S, Ahmadvand N, et al. Association between plasminogen activator inhibitor 1 gene mutation and different subgroups of recurrent miscarriage and implantation failure. J Assist Reprod Genet. 2014;31:121–4. doi: 10.1007/s10815-013-0125-8. doi:10.1007/s10815-013-0125-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buurma AJ, Turner RJ, Driessen JH, Mooyaart AL, Schoones JW, Bruijn JA, et al. Genetic variants in pre-eclampsia: a meta-analysis. Hum Reprod Update. 2013;19:289–303. doi: 10.1093/humupd/dms060. doi:10.1093/humupd/dms060. Epub 2013 Jan 8. PubMed PMID: 23300202. [DOI] [PubMed] [Google Scholar]
- 7.Morgan JA, Bombell S, McGuire W. Association of plasminogen activator inhibitor-type 1 (-675 4G/5G) polymorphism with pre-eclampsia: systematic review. PLoS One. 2013;8:e56907. doi: 10.1371/journal.pone.0056907. doi:10.1371/journal.pone.0056907. [DOI] [PMC free article] [PubMed] [Google Scholar]


