Abstract
Aim:
To compare the findings and diagnostic accuracy of Hysterosalpingography (HSG) and hysteroscopy in infertile women.
Setting and Design:
Prospective comparative study in a tertiary care Centre.
Material and Methods:
108 women with primary or secondary infertility were recruited. In all women after basic infertility workup, both HSG and hysteroscopy were performed.
Results:
Out of 108 women, in 3 women HSG couldn’t be done and in one woman there was uterine perforation on hysteroscopy. HSG showed normal uterine cavity in 77.8% (81/105) women and abnormal in 22.85% (24/105). Hysteroscopy findings were normal in 70.09% (75/107) and abnormal in 29.91% (32/107). Hysteroscopy detected incidental findings in 15.38% (16/104) cases. HSG showed irregular uterine cavity in 14.15% (15/105) women but on hysteroscopy; normal cavity was present in 6 (40%) women and abnormality was detected in 9 (60%) women. The sensitivity, specificity, positive predictive and negative predictive value of HSG in evaluating uterine cavity abnormalities were 44.83% (95% confidence interval (CI); 0.26–0.64), 86.67% (95% CI; 0.76–0.93), 56.52% (95% CI; 0.34–0.76) and 80.25% (95%CI; 0.69–0.88). Positive likelihood ratio and negative likelihood ratio of HSG in detecting uterine cavity abnormality was 3.36 and 0.64 respectively. The agreement between HSG and hysteroscopy was 75%. This was statistically significant (P value = 0.001) with fair strength of agreement between HSG and hysteroscopy. (k value= 0.336).
Conclusion:
Hysteroscopy should be performed in all infertile patients as it can detect significant number of incidental findings missed by HSG.
KEYWORDS: Hysterosalpingography, hysteroscopy, infertility
INTRODUCTION
Infertility is defined as failure of a couple to conceive for at least 1 year after regular and unprotected intercourse. Infertility can be primary and secondary. There are many causes of infertility among which tuboperitoneal pathology is responsible for infertility in 30 to 40% of the cases, whereas uterine pathology accounts for 15% of cases. Other factors include ovulatory dysfunction (20–40%). In 20 to 40% cases, infertility is due to male factor.[1] Hysterosalpingography (HSG) plays an important diagnostic role in finding the cause of infertility and in deciding the line of management. HSG is a simple, safe, and minimally invasive radiologic procedure to visualize uterine cavity and tubes after contrast enhancement. This is employed to study the causes of infertility like uterine anomalies, tubal patency, uterine synechiae, and uterine polyps. HSG provides us permanent record and shows the exact site of tubal blockage. In some cases, where blockage is due to mucus plug, dye dislodges it and maintains the tubal patency. Though pelvic sonography and HSG are good enough for excluding gross intrauterine pathology, subtle changes in the form of small polyps, adhesions, and subendometrial fibroid seedling, which influences fertility, can be missed. These subtle changes are better picked up on magnification with hysteroscopy. Hysteroscopy involves inspection of uterine cavity and the cornual ends of the fallopian tube with an endoscope inserted through the cervix.
Debate still continues on the role of HSG and hysteroscopy in diagnosing the causes of infertility. This study is designed to compare the diagnostic value of HSG with hysteroscopy in the assessment of cause of infertility. This study is based on the hypothesis that hysteroscopy is superior than HSG in detecting the uterine cavity abnormalities.
AIMS AND OBJECTIVES
The primary objective was to evaluate the diagnostic value of hysterosalpingography and hysteroscopy in infertile women and to correlate the findings of hysterosalpingography with findings of hysteroscopy in infertile women. The secondary objective was to study complications of hysterosalpingography and hysteroscopy in infertile women.
MATERIALS AND METHODS
The present study was a prospective comparative study conducted at infertility clinic of obstetrics and gynecology, in a tertiary care center. The study was carried out from November 2013 to February 2015. Ethical clearance and informed consent was taken. The purpose of the study was to compare the diagnostic value of HSG and hysteroscopy in infertile women and to evaluate their role in diagnosis and management of infertility. The inclusion criteria are all women attending infertility clinic for treatment (primary and secondary) in the age 20 to 40 years and the exclusion criteria was known case of pelvic inflammatory disease, women with acute vaginal and cervical infection, pregnancy, and women allergic to dye used in hysterosalpingography.
Hysterosalpingography was done as an outpatient procedure. Patients were given injection Biscotas (Hyoscine butylbromide, Biscotas, Intas, India) intramuscular before the procedure. The cervix was exposed and held with tenaculum forceps. The Leech Wilkinson cannula was inserted gently through the cervical canal into the uterine cavity beyond the internal cervical os. Sims speculum was removed. Ultravist 300/370 [Iopromide injection, ultravist Zydus (G. Rem)], a water soluble, nonirritating, nephrotropic, low-osmolar, and radio-opaque contrast media of about 10 ml, was slowly injected by attaching the loaded syringe to the cannula. After that X-rays were taken under fluoroscopic screening and the uterine cavity and fallopian tubes were visualized. The instruments were withdrawn. Women were observed for some time. Further plan of management was decided according to the normal or abnormal HSG. The criteria taken for normal HSG were normal uterine cavity with no evidence of tubal occlusion, normal fallopian tube contour, and free bilateral spillage of contrast.
Total 112 women with primary or secondary infertility were enrolled in the study. HSG was performed in all women under aseptic conditions. In infertile women with normal HSG findings, hysteroscopy was performed only if patient failed to conceive after three ovulation induction and intrauterine insemination (IUI) cycles, and in patients with abnormal HSG findings, hysteroscopy was performed in the immediate post menstrual phase.
All HSGs were performed by one individual and hysteroscopy was performed by different consultant so that decreases the chances of interobserver bias.
Four women got pregnant after HSG and hence were excluded from the study. A total of 26 women who failed to conceive and 82 women with abnormal HSG were taken up for diagnostic/operative hysteroscopy and the findings were compared.
Hysteroscopy was performed in operation theater under anesthesia. Hysteroscopy was performed in lithotomy position. Size and position of the uterus was confirmed by bimanual examination. The hysteroscope was connected to the source of distending medium and introduced into endocervical canal and uterine cavity after ensuring that there were no air bubbles in the distending fluid. Saline was used as distending media for diagnostic procedure. The endocervical and uterine lining was studied and both uterine ostia were identified. The criteria taken for normal hysteroscopy were normal uterine cavity (regular in shape and contour, no fibroid/mass/polyp), normal endometrium, and normal bilateral ostium.
Any abnormality of uterine cavity, endometrium, and uterine ostia were noted and corrective measures were taken accordingly. Complication were noted and treated.
Statistical analysis
Categorical variables were presented in number and percentage (%).
Statistical tests were applied as follows:
Qualitative variables were compared using Chi-square test/Fisher’s exact test.
Inter-rate kappa agreement was used to find strength of agreement between two methods.
McNemar’s test was used to find out the significance of difference in prediction of two methods.
Diagnostic test was used to find out sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of HSG in respect to hysteroscopy and laproscopy.
P value of <0.05 was considered statistically significant.
The data were entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0 (IBM).
RESULTS
Total 108 women were analyzed in the study. A majority of 73.14% had primary infertility (79/108) and 26.85% had secondary infertility (29/108). Mean age of women in our study was 27.56 ± 2.80 years. Maximum women were in age group 26 to 28 years 39.8% (43/108) followed by women in age group 23 to 25 years 27.8% (30/108) and 29 to 31 years 23.1% (25/108). Mean infertility period was 5.65 ± 2.54 years. HSG was normal in 24.07% (26/108) and abnormal in 75.93% (82/108) women. Women with secondary infertility had more abnormal HSG findings 79.31% (23/99) than women with primary infertility 74.68% (59/79). This difference in findings was not statistically significant (P value = 0.807). Out of 108 women, in three women, HSG could not be performed because of cervical stenosis, and in one woman, hysteroscopy couldn’t be done due to uterine perforation. Hysteroscopic findings were normal in 64.49% (69/107) women and abnormal in 35.51% (38/107) women. Abnormal hysteroscopic findings were detected in 35.44% (28/79) women with primary infertility and in 35.71% (10/28) women with secondary infertility. The difference between two groups was not statistically significant (P value = 0.839).
HSG showed normal uterine cavity in 77.8% (81/105) women and abnormality was found in 22.85% (24/105) women.[1] Most common abnormality found on HSG was filling defects in 15 (14.28%) women. HSG showed congenital uterine anomaly in five (4.6%) women, bicornuate uterus in four, and arcuate uterus in one woman [Fig. 1].
Figure 1.
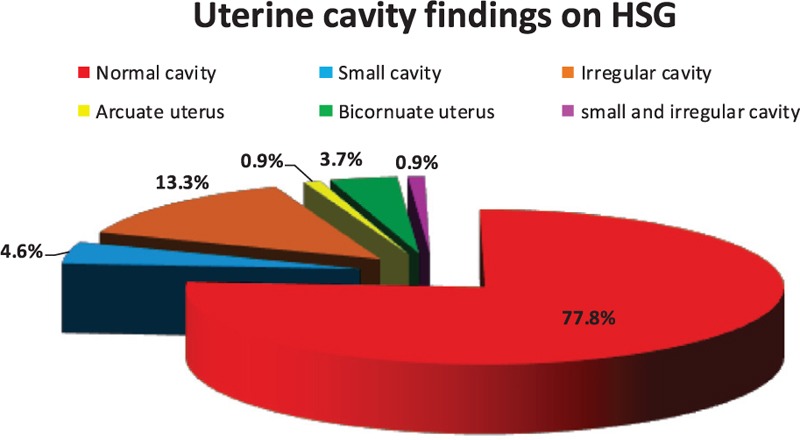
Uterine cavity findings on HSG
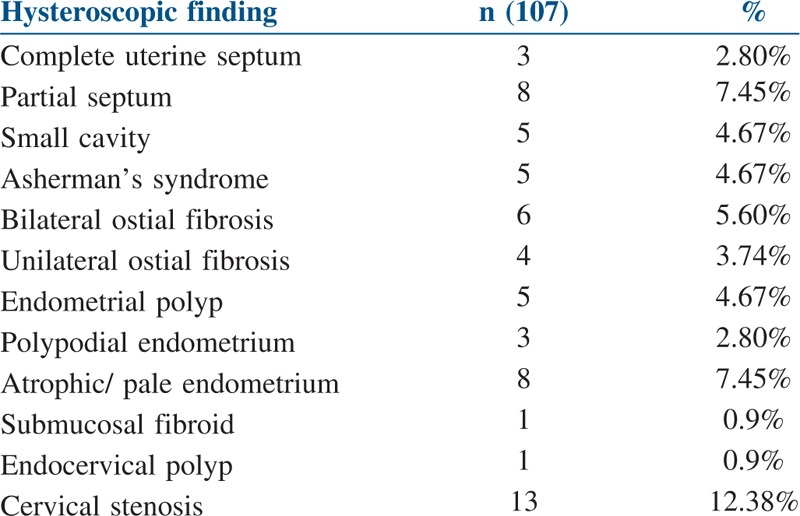
On hysteroscopy, uterine cavity was normal in 70.09% (75/107) and abnormal in 29.91% (32/107). The most common uterine cavity finding on hysteroscopy was uterine septum in 11 (10.25%) followed by ostial fibrosis in 10 (9.34%), pale or atrophic endometrium 8 (7.45%), endometrial polyp 5 (4.67%), and Asherman’s syndrome in 5 (4.67%) women [Table 1].
Table 1.
Uterine and cervical findings on hysteroscopy
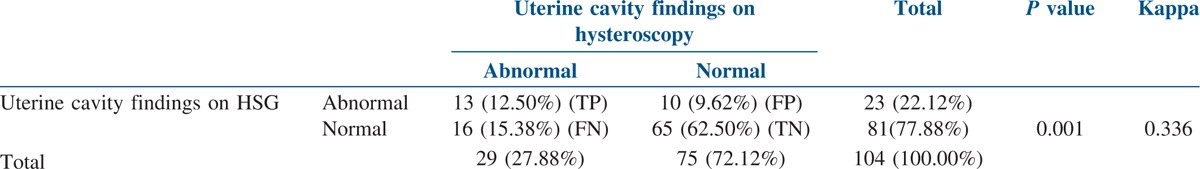
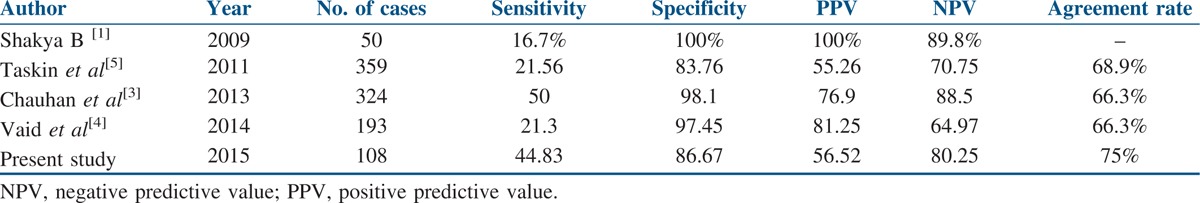
Comparison of uterine cavity findings on HSG and hysteroscopy is shown in Table 2. The sensitivity, specificity, positive predictive, and negative predictive value of HSG in evaluating uterine cavity abnormalities were 44.83 (95% confidence interval (CI); 0.26–0.64), 86.67 (95% CI; 0.76–0.93), 56.52 (95% CI; 0.34–0.76), and 80.25% (95% CI; 0.69–0.88). Positive and negative likelihood ratios of HSG in detecting uterine cavity abnormality were 3.36 and 0.64, respectively. The agreement between HSG and hysteroscopy was 75%. This was statistically significant (P value = 0.001) with fair strength of agreement between HSG and hysteroscopy (k value = 0.336).
Table 2.
Comparison of uterine cavity finding on HSG and hysteroscopy
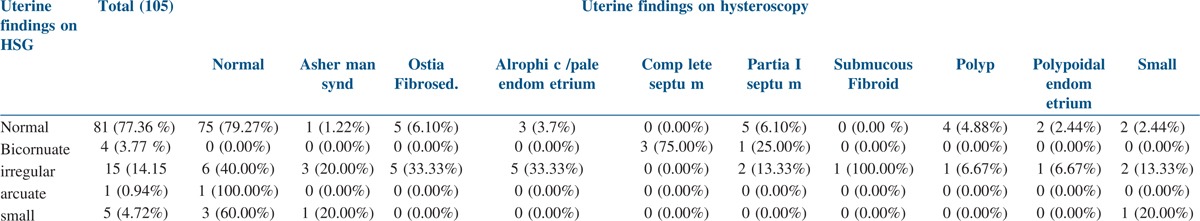
On comparing the findings of HSG with hysteroscopy, the incidental findings were detected in 15.38% (16/104) cases on hysteroscopy. These findings were partial septum 3.8% (4/104), endometrial polyp 3.8% (4/104), Asherman’s syndrome in one, small cavity with atrophic/pale endometrium with bilateral ostia fibrosis in two, polypoidal endometrium in two, and ostia fibrosis in three women. HSG showed irregular uterine cavity in 14.15% (15/105) women but on hysteroscopy; normal cavity was present in six (40%) women and abnormality was detected in nine (60%) women, including which was Asherman’s syndrome in three, partial septum in two, submucosal fibroid in one, endometrial polyp with small cavity in one, and small cavity in one. HSG was suggestive of bicornuate uterus in four women (3.74%), which was found to be complete septum in three and partial septum in one woman on hysteroscopy. In one women, HSG showed arcuate uterus which was found to be normal on hysteroscopy. Out of 10 cases of ostial fibrosis on hysteroscopy, HSG findings were normal in five and cavity was irregular in five cases, which may be because of pre-existing pelvic pathology [Table 3].
Table 3.
Comparison of findings of HSG and hysteroscopy (subgroups)
Hysteroscopic intervention was done in 28.73% (30/107) in same sitting. Cervical dilatation was the most common procedure done in 13% (14/108), out of which, perforation occurred in one woman [Fig. 2].
Figure 2.
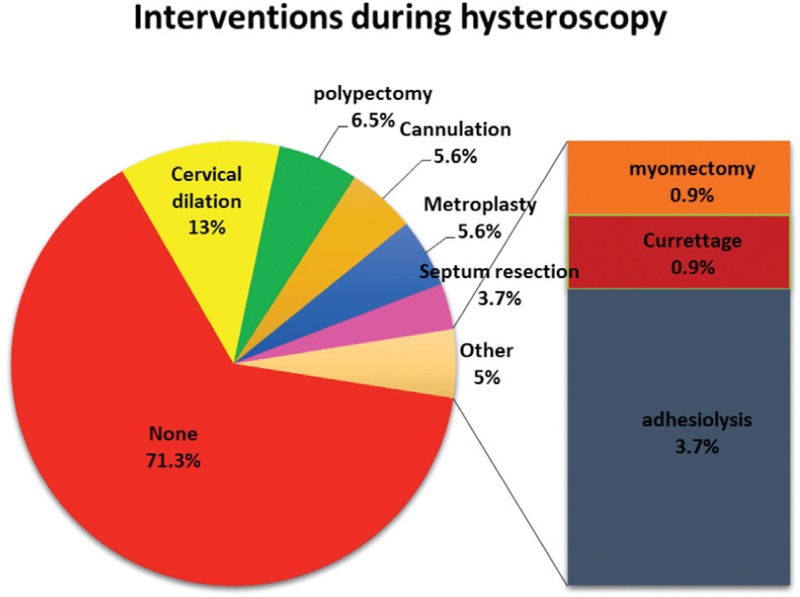
Interventions done during hysteroscopy
DISCUSSION
The study demonstrated that around one-third of the women, 74.07% had primary infertility and 25.93% had secondary infertility. The proportion of women with primary or secondary infertility was found to be comparable with other studies.
Normal HSG findings were seen in 24.07% (n = 26) and abnormal findings in 75.92% (n = 82). The abnormal HSG findings were 79.31% in women with secondary infertility and 74.68% with primary infertility. Although the abnormal findings were more in women with secondary infertility, the difference was not statistically significant (P value = 0.201). Ibinaiye et al.[2] also didn’t find significant difference between the two groups (P value = 0.077).
Considering uterine cavity and tubal factors separately on HSG, normal uterine cavity was found in 77.8% (81/105) women and abnormal cavity in 22.85% (24/105) women. Similar results were reported by Ibinaiye et al.[2] as normal uterine cavity on HSG in 75.9% and abnormal cavity in 24.1% women. Chauhan et al.[3] have reported normal uterine cavity on HSG in 87% and abnormal cavity in 13%. Vaid et al.[4] reported normal cavity on HSG in 91.7% and abnormal cavity in 8.29% women.
The most common abnormal uterine cavity finding on HSG in our study was filling defects or irregular uterine cavity in 14.28% (15/105). Vaid et al.[4] have reported filling defects and irregular cavity separately in 3.1 and 1.55%, respectively. Ibinaiye et al.[2] reported uterine cavity adhesions to be the most common finding in 11.3% on HSG; they didn’t mention about irregular cavity or filling defects.
Hysteroscopy was performed in 107 women; normal findings were detected in 64.49% (69/107) and abnormal findings 35.51% (38/107) women. Chauhan et al.[3] reported normal hysteroscopic findings in 80% and abnormal findings in 20%.
Hysteroscopic findings between women with primary and secondary infertility were compared; abnormal hysteroscopic findings were detected in 35.44% (28/79) women with primary infertility and in 35.71% (10/28) women with secondary infertility. The difference was not statistically significant in our study (P value = 0.839). On hysteroscopy, uterine cavity was normal in 70.09% (75/107) and abnormal in 29.91% (32/107) women. Other findings associated with normal uterine cavity on hysteroscopy were ostia fibrosis in five women and pale/atrophic endometrium in three women. Vaid et al.[4] reported normal uterine cavity in 61.1% and abnormal cavity in 38.96% women on hysteroscopy.
The most common finding on hysteroscopy was uterine septum in 11 (10.25%) followed by ostial fibrosis in 10 (9.34%), pale or atrophic endometrium 8 (7.45%), endometrial polyp five (4.67%), and Asherman’s syndrome in five (4.67%) women. Taskin et al.[5] also found uterine septum or subseptum (9.54%) as most common finding in their study followed by endometrial polyp (6.89%). They found Asherman’s syndrome in relatively less women (0.1%) than our study, which may be because most of their cases were of male factor infertility. Chauhan et al.[3] found submucous fibroids and congenital malformations each in 6% of the women as the most common uterine abnormalities detected in their study on hysteroscopy. Vaid et al.[4] found ostia fibrosis in 15.02% as most common finding followed by intrauterine adhesions followed by polyp/myoma 11.91 and 6.21%, respectively, on hysteroscopy. In our study, uterine adhesions were associated with Asherman’s syndrome in 4.67% women. Hysteroscopic intervention was performed in 28.73% (30/107) of women. Most common procedure performed was hysteroscopy guided cervical dilation in 14 (13%) followed by polypectomy in seven (6.5%), metroplasty in six (5.6%) cases, cannulation for ostia fibrosis in six (5.6%) women, septum resection in four (3.7%), and adhesiolysis in four (3.7%) cases. In the study of Vaid et al.,[4] adhesiolysis as the most common intervention was performed in 22% women. Studies done by Taskin et al.[5] and Chauhan et al.[3] have not commented on intervention performed during hysteroscopy.
In the present study, HSG showed abnormal uterine cavity in 22.85% (24/105), and 29.91% (32/107) women had abnormal hysteroscopy. The agreement between two procedures was 75%. On comparing, the difference in findings between HSG and hysteroscopy was statistically significant (P value = 0.001) with fair degree of agreement between two procedures (k value = 0.336).
HSG detected false-negative in 9.62% (10/104) and false-positive in 15.38% (16/104), whereas Chauhan et al.[3] reported that HSG detected false-negative in 10% of women and false-positive in 3%. This difference in findings could be because they performed HSG and hysteroscopy on same day; though they didn’t find the difference to be statistically significant (Chi-square value: 1.77, P value >0.05). Taskin et al.[5] reported false-positive and false-negative rates of HSG as 16.23 and 78.43%, respectively. The reason for high false-negative rate in the study could be because standardization of the procedure was not possible in their centre due to large patient population whereas in our study HSG were performed by one of the investigator so there is less discrepancy in results.
In the present study, hysteroscopy detected incidental findings (false-negative findings) in 15.38% (16/104) cases. Most common incidental findings were partial septum in 3.8% (4/104) followed by endometrial polyp 3.8% in (4/104) women. This figure reported by other authors is 29.2% by Taskin et al.,[5] 32.12% by Vaid et al.,[4] and 13% by Chauhan et al.[3]
In the present study, HSG showed uterine anomaly in five women. Bicornuate uterus in four women was found to be complete uterine septum in three women and partial septum in one, and in one woman with arcuate uterus, hysteroscopy detected normal uterine cavity. HSG is good for screening purpose but not reliable in making a correct diagnosis of uterine anomaly. Chauhan et al.[3] also mentioned in their study that the diagnosis of double uterus is generally made from HSG, but it cannot differentiate between septate and bicornuate uterus. Clever et al.[6] detected intrauterine adhesions as the most common finding on HSG in their study and mentioned that both HSG and hysteroscopy are effective in evaluating endometrial adhesion with no difference in accuracy.
Study by Vahdat et al.[7] has reported the diagnostic accuracy of HSG as 84.8% in diagnosis of uterine malformations. In their study, HSG with hysteroscopy as the gold standard had a sensitivity of 95.6%, specificity of 60%, PPV of 84.62%, and NPV of 85.71% for evaluating Müllerian anomalies.
The sensitivity and specificity of HSG in detecting uterine cavity abnormalities differ in various studies[7,8,9] ranging between 21 to 81 and 70 to 98%, respectively. In study of Taskin et al.,[5] reason for low sensitivity could be that most of the couples visiting their clinic had male factor infertility. In study by Nigam et al.,[10] the positive predictive value of HSG for detecting the intrauterine abnormalities was 70% with a false-negative rate of 12.96%. Shakya,[11] in his study on investigating the accuracy of HSG in comparison to hysteroscopy in the detection of intrauterine pathology in infertility, found that HSG in the detection of intrauterine pathology had a sensitivity of 16.7%, specificity 100%, PPV 100%, NPV 89.8%, false-positive rate close to zero, false-negative rate 83.3%, and accuracy rate 90%. This difference in results from the present study could be because both HSG and hysteroscopy were done in same menstrual cycles and sample size was also less.
The other reasons for variation between the results of different studies [Table 4] could be because of different techniques used for performing HSG, different reporting methods, and performing HSG in different length of menstrual cycle.
Table 4.
HSG vs hysteroscopy in detecting uterine cavity abnormalities
CONCLUSION
From our study, we concluded that HSG can detect uterine abnormalities, but findings have to be confirmed by hysteroscopy or other modality. Hysteroscopy should be performed in all infertile women with abnormal HSG and those who fail to conceive after normal HSG findings as incidental lesions can be missed on HSG.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Berek JS. Berek and Novak’s Gynaecology. 15th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. Chapter 32: Infertility and assisted reproductive technology; pp. 1133–34. [Google Scholar]
- 2.Ibinaiye PO, Lawan RO, Avidime S. Comparative evaluation of pattern of abnormalities in hysterosalpingography, diagnostic laparoscopy and hysteroscopy among women with infertility in Zaria, Nigeria. Int J Med Med Sci. 2015;7:26–35. [Google Scholar]
- 3.Chauhan MB, Lakra P, Nanda S, Malik R, Malhotra V. Hysterosalpingography vs hysteroscopy: role in assessment of uterine factor during infertility workup. J S Asian Fed Obstet Gynaecol. 2013;5:116–9. [Google Scholar]
- 4.Vaid K, Mehra S, Verma M, Jain S, Sharma A, Bhaskaran S. Pan endoscopic approach “hysterolaparoscopy” as an initial procedure in selected infertile women. J Clin Diagn Res. 2014;8:95–8. doi: 10.7860/JCDR/2014/7271.4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taskin EA, Berker B, Ozmen B, Sönmezer M, Atabekoğlu C. Comparison of hysterosalpingography and hysteroscopy in the evaluation of the uterine cavity in patients undergoing assisted reproductive techniques. Fertil Steril. 2011;96:349–52. doi: 10.1016/j.fertnstert.2011.05.080. [DOI] [PubMed] [Google Scholar]
- 6.Clever O, Esther A, Ebuka O, Anthony M. Relative assessment of abnormalities patterns in hysterosalpingography, diagnostic laparoscopy and hysteroscopy with infertility cases in women in Nigeria. Int J Obstet Gynecol. 2015;3:081–9. [Google Scholar]
- 7.Vahdat M, Sariri E, Kashanian M, Najmi Z, Mobasseri A, Marashi M, et al. Can combination of hysterosalpingography and ultrasound replace hysteroscopy in diagnosis of uterine malformations in infertile women.? Med J Islam Repub Iran. 2016;30:352. [PMC free article] [PubMed] [Google Scholar]
- 8.Nayak PK, Mahapatra PC, Mallick JJ, Swain S, Mitra S, Sahoo J. Role of diagnostic hystero-laparoscopy in the evaluation of infertility: a retrospective study of 300 patients. J Hum Reprod Sci. 2013;6:32–4. doi: 10.4103/0974-1208.112378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahu L, Tempe A, Gupta S. Hysteroscopic evaluation in infertile patients: a prospective study. Int J Reprod Contracept Obstet Gynecol. 2012;1:37–41. [Google Scholar]
- 10.Nigam A, Saxena P, Mishra A. Comparison of hysterosalpingography and combined laparohysteroscopy for the evaluation of primary infertility. Kathmandu Univ Med J (KUMJ) 2015;13:281–5. doi: 10.3126/kumj.v13i4.16824. [DOI] [PubMed] [Google Scholar]
- 11.Shakya B. Hysterosalpingography vs hysteroscopy in the detection of intrauterine pathology in infertility. J Nepal Health Res Counc. 2009;7:6–9. [Google Scholar]


