Abstract
Peripheral neuropathy (PN) is a common disorder and presents as diagnostic and therapeutic challenge to physicians and neurologists. In epidemiological studies from India from various regions the overall prevalence of PN varied from 5 to 2400 per 10,000 population in various community studies. India is composed of a multiethnic, multicultural population who are exposed to different adverse environmental factors such as arsenic and lead. Use of different chemotherapeutic agents with propensity to affect peripheral nerves, increasing methods of diagnosis of connective tissue disorders and use of immunomodulating drugs, growing aging population is expected to change the spectrum and burden of peripheral neuropathy in the community. The other important aspect of peripheral neuropathies is in terms of the geographical and occupational distribution especially of toxic neuropathies like arsenic which is common in eastern belt; lead, mercury and organo-phosphorous compounds where occupational exposures are major sources. Inflammatory neuropathies either due to vasculitis or G B Syndrome, chronic inflammatory polyradiculopathies are another major group of neuropathies which is increasing due to increase longevity of Indian subjects and immunological impairment, also adds to morbidity of the patients and are potentially treatable. Leprous neuropathy is common in India and although its frequency is significantly decreasing because of national control program yet pure neuritic form still remains a cause of concern and similar is the case with another infective cause like diptheric neurpathy. Thus this article is an attempt to cover major categories and also highlight the areas where further studies are needed.
Keywords: Diabetic neuropathy, epidemiology, Guillain–Barre Syndrome, Hansen neuropathy, India, toxic neuropathy
INTRODUCTION
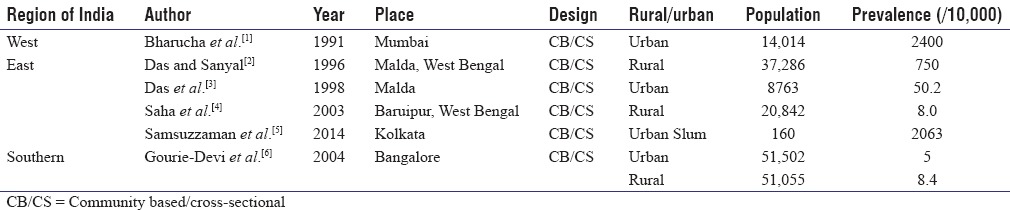
Peripheral neuropathy (PN) is a group of heterogeneous disorder with a wide etiological spectrum and presents to physicians and neurologists in the community frequently. Various epidemiological studies from India showed wide prevalence varying from 5 to 2400 per 10,000 population in different community studies [Table 1]. In a rural setting, it is less frequent and comparable with studies from eastern and southern regions. However, urban studies show higher rates. Exceptionally, high prevalence was noted among Parsis[1] and in urban slum.[5] The high rate in Parsis is probably related to aging population, and in urban slum, it may be due to nutritional and adverse environmental factors and needs further study.
Table 1.
Prevalence of peripheral neuropathy in various parts of India
In a hospital-based study from Eastern India[7] out of 225 patients of acute and chronic PN, Guillain–Barre Syndrome (GBS) was the most common (24.8%), followed by diabetes (11.1%), hereditary sensory motor neuropathy (7.55%), chronic inflammatory demyelinating neuropathy (7.55%), Hansen (4.8%), alcoholic/nutritional (3.55%), and entrapment neuropathy (3.55%). In 17.3% of patients, no etiology could be defined.
There are many papers on PN from India which are often case reports and small series, but no holistic compilation of data on epidemiology of PN was available. India is composed of a multiethnic, multicultural population who are exposed to different adverse environmental factors such as arsenic and lead. Further, use of different chemotherapeutic agents with propensity to affect peripheral nerves in different malignant diseases, increasing diagnosis of connective tissue disorders, and use of immunomodulating drugs, growing aging population is expected to change the spectrum and burden of PN in the community.
Hence, we plan to review the epidemiology of PN in the context of Indian scenario to highlight important peripheral neuropathies and also find deficiencies where further research is needed for planned epidemiological studies and possible direction to the occurrence of underlying etiology and risk factors for diagnostic and therapeutic targets.
Search strategy
We comprehensively searched the literature, using electronic medical databases (EMBASE, MEDLINE, Cochrane, PubMed Publisher, and Google Scholar), to identify published studies reporting the prevalence or incidence of polyneuropathy in the general population in India with keywords such as “PN - epidemiology” (n = 23,020). Furthermore, subtopics were searched with keywords such as “epidemiology of leprosy” (n = 23,300), “acute inflammatory demyelinating polyradiculoneuropathy (AIDP)/Landry–GBS Indian studies” (n = 820), and chronic inflammatory demyelinating polyneuropathy (CIDP) (n = 2490). Studies based on case series were included along with cross-sectional, retrospective, prospective studies, whereas case reports and Western data were found relevant. Hand search was also made from national journals such as Neurology India, Annals of Indian Academy of Neurology, and Journal of associated physician of India. Relevant articles and research papers in the past 35 years (1981–2016) were taken up.
NEUROPATHY RELATED TO DIABETES AND OTHER METABOLIC CAUSES
Diabetic neuropathy
Diabetes mellitus (DM) is a common cause of neuropathy worldwide. Prevalence of PN in diabetic patients ranges from around 10.5% to 32.2% in various studies across India [Table 2], and up to 50% patients will eventually develop neuropathy during the course of their disease according to Western literature.[20]
Table 2.
Epidemiology of diabetic neuropathy
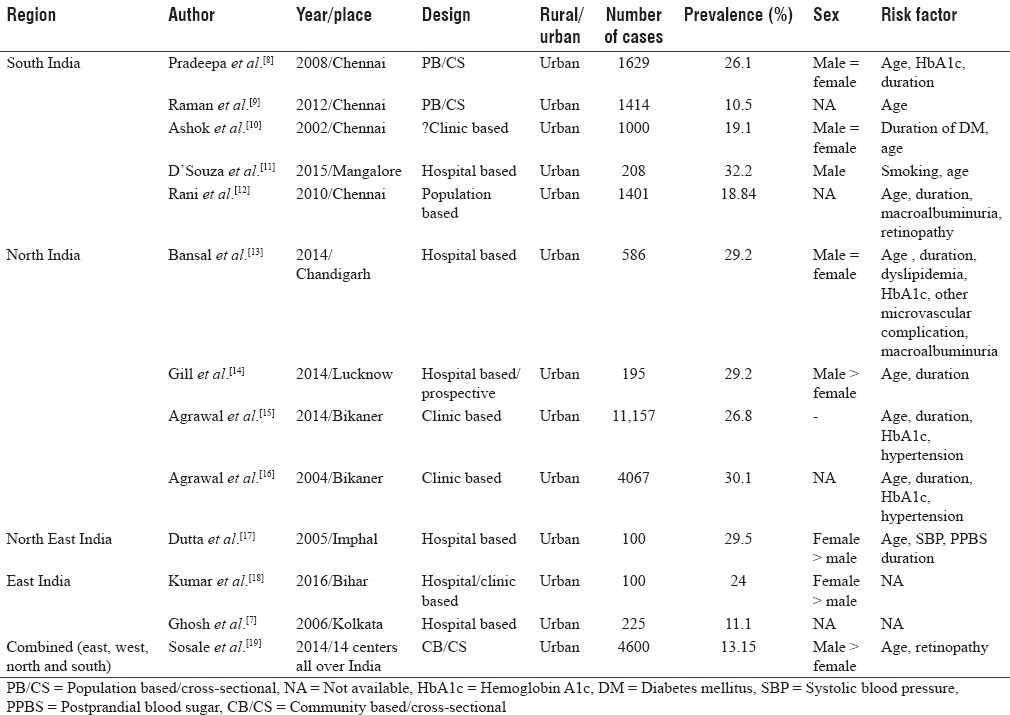
Most of the studies from five regions have been provided in Table 2 on diabetic PN. There is a higher prevalence of DM in India compared with the West.[21] However, most of the studies in India are either hospital or clinic based. Thus, the conclusions were often biased.
Above studies[7,8,9,10,11,12,13,14,15,16,17,18,19] showed that age, duration of diabetes, dyslipidemia, glycated hemoglobin, microvascular complications, macrovascular complications, and alcoholic status are risk factors for the development of PN.
Neuropathy with impaired glucose tolerance
Many studies have noted that in idiopathic PN patients, glucose tolerance test results are abnormal. In a study of 107 patients of idiopathic neuropathy who were tested with glucose tolerance test, 13 had DM, and 36 had impaired glucose tolerance (IGT), which they note is almost 3 times the prevalence among previously published control patients.[22] In another study from South India, IGT group exhibited a significantly lower mean nerve conduction velocity (NCV) when compared with normal participants and warrants early screening.[23]
Uremic polyneuropathy
Chronic kidney disease (CKD) affects all levels of the nervous system. In a cross-sectional study from Andhra Pradesh,[24] out of 74 patients of CKD, 65% of the study population was suffering from peripheral nerve dysfunction. It was more prevalent in elderly (>65 years), patients with longer duration of CKD, males, and patients with creatinine clearance <15 ml/min. CKD may also be present with entrapment neuropathies, autonomic neuropathies, and cranial neuropathies. In a study to evaluate the involvement of inner ear and eighth nerve in CKD patients, out of 46 patients with normal hearing included in the study, there was a statistically significant difference in the mean absolute latency of wave I, III, and V and mean inter-peak latency I–III, III–V, and I–V suggestive of subclinical involvement of auditory end organs and auditory nerve and it worsened with duration of disease, blood urea levels (>200 mg%), and advancement of stage of CKD.[25]
NEUROPATHY DUE TO INFLAMMATION AND INFECTIOUS ETIOLOGY
Guillain–Barre syndrome
GBS affects between 1 and 4/100,000 of population annually throughout the world,[26] with complications such as respiratory failure requiring ventilation in approximately 25%,[27] persistent disability in approximately 20%,[28] persistent fatigue in 67%,[29] and death in 4%–15%.[27]
After the first decade of life, there is an escalating increase of 20% with each passing decade of life. Male and female gender ratio has been observed to be 1.78:1.[30] Nearly two-thirds of cases are preceded by symptoms of upper respiratory tract infection or diarrhea and rarely vaccination.[31]
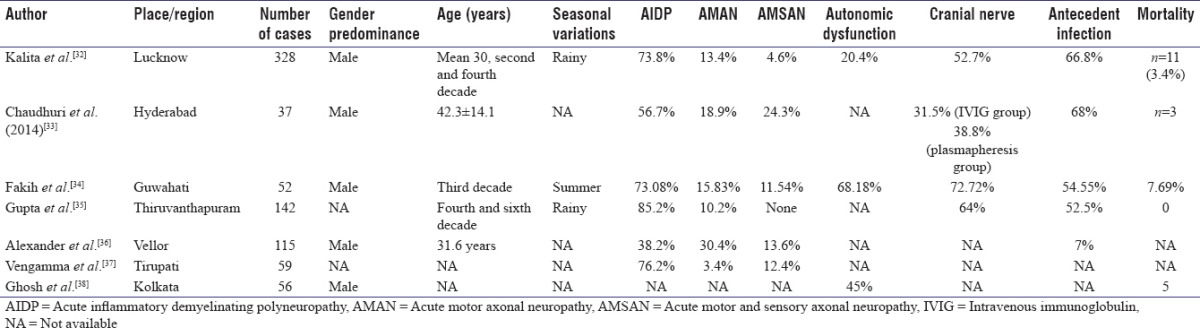
Studies have shown cross-reactivity between infectious and neural epitopes, especially for Campylobacter jejuni and certain forms, for example, motor axonal forms of GBS.[28,29] Among the electrophysiological subtypes, axonal types are common in Asian countries as compared to demyelinating in Western countries.[30,31] However, studies from India have yielded varying results showing AIDP or demyelinating type being more common [Table 3]. However, one study from Vellore in Southern India has almost comparable proportion of demyelinating and axonal variety [Table 3]. Most of the Indian studies have shown also male dominance, and median age of occurrence is about third decades. Cranial nerve involvement is common and varied from 52.7% to 72.72% of cases from two studies. Antecedent infection was documented in 54.55%–68% of cases except the study from Vellore, Southern India, showing a rate of 7% only.
Table 3.
Profile of Guillain-Barre Syndrome patients in India
Chronic dysimmune neuropathy
The chronic dysimmune neuropathies are a clinically heterogeneous group of polyneuropathies united by their presumed immune-mediated etiology. The subdivision is based on a combination of clinical, electrophysiological, pathological, and immunological features.
Chronic inflammatory demyelinating polyneuropathy
CIDP is a chronic PN with progressive phase beyond 8 weeks. The distinction between AIDP and CIDP may be artificial as the distribution of onset phases is unimodal not bimodal[38] and intermediate or subacute forms occur.[39] The reported prevalence of CIDP varies greatly from 1.9 to 7.7 per 100,000 along with sparse reports of incidence ranging from 0.15 to 0.48 per 100,000 per year.[40,41]
A study from North India[42] on 65 patients aged between 17 and 72 years, 25 patients had secondary CIDP due to DM (n = 16), polyneuropathy, organomegaly, endocrinopathy, M protein, skin changes (n = 4), monoclonal gammopathy of undetermined significance (n = 2), myeloma (n = 1), lymphoma (n = 1), and malignancy (n = 1). Secondary CIDP patients were older (48.35 vs. 41.0 years), had less relapsing-remitting course, and more frequent dysautonomia (7 vs. 1). Demyelinating features were more marked in primary CIDP patients with a better outcome. Hence, primary or idiopathic CIDP is common and indicative of primary immunological disturbance against large diameter nerve fibers.
Vasculitic neuropathies
Vasculitic neuropathy usually presents with painful mononeuropathies or asymmetric polyneuropathy of acute or subacute onset. The disorder may be classified as being systemic or nonsystemic. The systemic vasculitides are divided into primary systemic disorders, for which there is no known cause, and secondary systemic disorders, for which a virus, drug, or connective-tissue disease causes inflammation of the vessel wall.[43]
In a study on vasculitic neuropathy,[44] twenty patients with vasculitic neuropathy were analyzed. Sixteen of the twenty presented with classic mononeuritis multiplex but four had distal, symmetrical, sensorimotor polyneuropathy. Only 13 patients had definitive collagen vascular disease. A large proportion (7/20) had vasculitic neuropathy as the only clinical feature. A study on rheumatoid arthritis in Indian cohorts of 74 participants has shown PN in 39.19% on NCV study, and significant association has been noticed with disease duration and rheumatoid factor.[45] In another study on sixty systemic lupus erythematosus patients, only two patients (3.3%) had PN.[46]
Human immunodeficiency virus-associated neuropathy
PN is one of many neurological complications of human immunodeficiency virus (HIV). Clinically, there are at least six patterns of HIV-associated PN.[47] Distal sensory PN, which is the most common out of all HIV-associated neuropathies,[47] can exist as two major types: primary HIV-associated distal sensory polyneuropathy (HIV-DSP) and antiretroviral toxic neuropathy.[48]
In an Indian study on 75 patients, 40% had clinical HIV-associated sensory neuropathy (HIV-SN).[49] HIV-SN considerably affects their quality of life. Symptomatic relief therapy is usually not satisfactory.[50] Furthermore, antiretroviral therapy is still composed of some first-line drugs that have been demonstrated to increase the risk of PN.[51]
Although after introduction of highly active antiretroviral therapy, the incidence of HIV-associated dementia and central nervous system (CNS) opportunistic infections have fallen,[52] but rates of HIV-associated DSP increased with reported prevalence rates exceeding 50%.[53] HIV-SN is more common among middle-aged participants similar to other studies.[54] According to a Western study, two-thirds of HIV-SN is subclinical,[55] which was less common (around 16%) in Indian study.[49]
Leprous or Hansen neuropathy
Leprosy is the most common treatable cause of neuropathy.[56] Multidrug treatment and WHO surveillance programs are having a major impact on disease occurrence. Between 1990 and 1994, there was a 55% fall in the worldwide prevalence.[57] Leprosy has been eliminated globally, as the number of cases has decreased from 5.4 million in 1985 to 0.24 million in 2013, and the prevalence rate has come down to 0.37 cases per 10,000.[58] South-East Asia region currently has highest prevalence with 72% of the global leprosy burden and India accounted for 58.85%.[59] A total of 86,000 cases were on record as on April 1, 2014, giving a prevalence rate of 0.68 per 10,000 population.[60] Clinical case series estimate that 4%–8% of all leprosy is limited to only peripheral nerves producing diagnostic challenge.[61,62]
According to Indian studies, pure neuritic leprosy constitutes about 2.17%–5.3% of leprosy patients [Table 4]. At present, the endemic and hyperendemic areas of India are in the North and East. Pure neuritic leprosy is more common in men. The disease has been reported from 5 years to 69 years and it is most common in the 15–30 age group [Table 4].
Table 4.
Epidemiology of neuropathy in leprosy
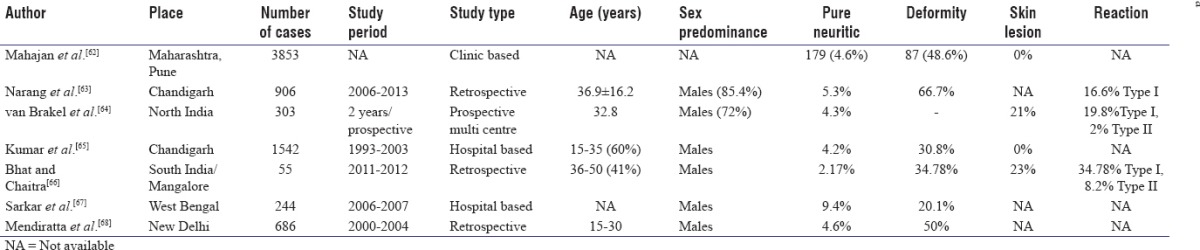
The most common pattern of involvement in leprosy is mononeuritis multiplex. However, mononeuropathy, cranial neuropathies, or polyneuropathy also occur. In a study on cranial neuropathies in leprosy, greater auricular nerve conduction study (NCS) was found abnormal in 10 of the 12 patients, thus emphasizing the usefulness of the procedure in diagnosis.[69] Deformity was observed in about one-third of cases. Associated skin lesion was documented between 21% and 49% of cases. Type 1 reaction is more common than type 2 reaction [Table 4].
Diphtheritic neuropathy
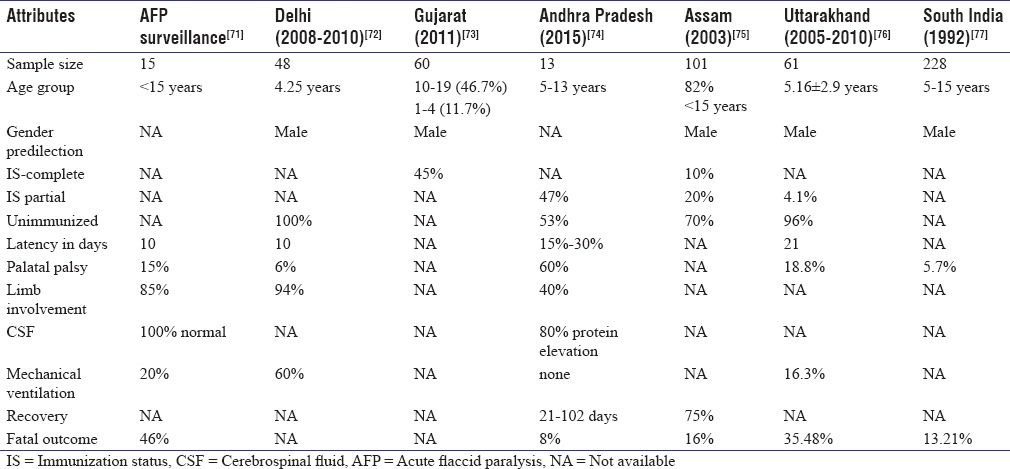
Diphtheria is caused by toxin-producing strains of Corynebacterium diphtheriae spread by human-to-human contact. Diphtheritic polyneuropathy (DP) is recognized as one of the most severe complications of diphtheria. Among 20,000 cases of diphtheria reported by the WHO during 2007–2011, 17,926 (89.6%) cases were from India alone.[70] Most persons with diphtheria in India are either partially immunized or unimmunized. Profile of DP in various studies is described in Table 5. Diphtheritic neuropathy has been reported from all zones of India. It is more common among males and more common in unimmunized and partially immunized person. Even among those with background of complete immunization, 10%–45% of patients from different series have been affected. Latency of disease is variable. In unimmunized person, limb involvement is common.
Table 5.
Profile of diphtheritic polyneuropathy in various studies in India
TOXIN-INDUCED NEUROPATHIES
Toxins may be environmental, occupational, recreational, or iatrogenic. In India, Ayurveda, Homeopathy, and Arabic medicine are potential sources of toxicity. In a survey, 14 of the seventy herbal medical products available commercially were found to contain lead in 13 (median concentration 40 mg/g; range, 5–37,000), mercury in 6 (median concentration, 20,225 mg/g; range, 28–104,000), and arsenic in 6 (median concentration 430 mg/g; range, 37–8130).[78] One should be cautious when evaluating a case of PN about possible toxic causes. In early stage, it is reversible, but in advanced stage, it becomes progressive and irreversible.
Arsenic
Arsenic exposure may be occupational (smelting, mining, tanning, and numerous manufacturing processes),[79] environmental (groundwater contamination, combustion fumes of contaminated fossil fuels and arsenate-treated wood, and contact with arsenic-containing pesticides and herbicides),[80] and iatrogenic medicinal exposure including folk and herbal medicines.[78] Arsenic is also a homicidal or suicidal agent.[80,81]
In some parts of the world like Bangladesh (79.9 million), India, including the state of West Bengal (42.7 million), subacute onset or chronic arsenic neuropathy commonly reflects exposure to drinking water contamination from geologic, mining, or other industrial sources or ingestion of arsenic-containing homeopathic medicines.[80,82,83] Chronic arsenic intoxication occurs either adulteration of opium or country liquor (common in North India) and contaminated ground water (Common in West Bengal and Bangladesh). Occurrence of PN has been observed in 11%–41% of cases, common in subacute exposure (87%) than chronic (37.3%).[80,83]
Acute arsenic neuropathy usually follows a single massive exposure, after which neuropathy appears within 5–10 days. Initial symptoms include paresthesias and burning pain, distal numbness and tingling, muscle aches, and distal weakness. The neuropathy progresses over weeks despite no additional exposure (coasting).[84]
Some cases, the neuropathy results in flaccid paralysis resembling GBS.[85]
Lead poisoning
Lead is a nonferrous toxic metal that is absorbed across respiratory and gastrointestinal membranes.[86] Exposure may result from consumption of illicit whiskey made in lead-lined stills,[87] lead-containing candy, powdered food coloring, herbal medications, food contaminated by glaze pigments in ceramic dishes,[88] and occupational (smelting reprocessing of lead-containing products, demolition of lead-painted structures, manufacturing paint pigments, and repair of automobile radiators).[89]
In a survey on fifty petrol pump workers and garage attendants in Orissa, blood lead levels ranged between 20 and 80 ng/dl and complained of fatigue (50%), abdominal pain (20%), sleep disturbance (20%), and tremors (14%). NCS revealed subclinical motor neuropathy in four participants.[90] Radial neuropathy in five patients aged 30–37 years was reported in battery factory or battery shop workers (wrist drop in four and finger drop in one). All patients had elevated blood lead level (37.8–107.8 mg/dL)[91] with subtle changes in the form of reduced compound motor action potential (CMAP) on NCS.[91]
Elemental mercury
Mercury is used in the chlor-alkali industry, metal plating, tanning processes, thermometers, electromechanical switches, a component of dental amalgams, and antiseptic and purgative medication.[92]
Acute exposure to high-level mercury vapor produces erosive bronchitis, interstitial pneumonitis with pulmonary edema, and renal insufficiency.[93] Signs of chronic intoxication include behavioral changes, postural tremor, and neuropathy.[94,95]
Chronic exposure is characterized by insidious onset of stocking-distribution sensory loss, Romberg sign, absent ankle reflexes, and postural tremor with mild motor involvement[93] and generally resolve after removal from exposure although there may be a residual tremor.[96]
Evidence of mild neuropathy has been identified among chlor-alkali workers exposed to elemental mercury with 28% of workers showing clinical evidence of neuropathy having markedly elevated urinary mercury excretion levels above 850 μg/L.[93,96]
In one study, one-fifth of both US-manufactured and Indian-manufactured Ayurvedic medicines purchased through the internet contain detectable lead, mercury, or arsenic.[97]
Kodaikanal, India, suffered mercury contamination due to emissions and waste from a thermometer factory. Results from a study on mercury in Kodai Lake waters showed that pollution of the lake has taken place due to mercury emissions by the factory.[98]
Organophosphorus poisoning
Acute organophosphate (OP) poisoning is a significant cause of morbidity and mortality in developing countries including India. Although no exact estimates are available, hospital-based studies suggest that it is the most common poisoning in India with nearly half of the admissions to the “emergency” with poisoning being due to these compounds.[99,100,101,102]
According to the WHO, one million serious accidental and two million suicidal poisonings due to insecticides occur worldwide every year, of which 200,000 die and most of these deaths occur in developing countries.[103]
In a report on 200 cases of OP poisoning for suicidal ingestion, the clinical manifestations included miosis in all, impaired consciousness (10%), fasciculations (27%), convulsions (11%), delirium (50%), and paralysis (26%). The paralytic signs were divided into type I and type II (intermediate syndrome). Type I paralysis manifested with impaired consciousness and bipyramidal signs due to excessive cholinergic stimulation of muscarinic receptors and responded to atropine. Type II paralysis manifested from 24 to 96 h with wasting and weakness of proximal muscle, areflexia, and cranial nerve palsy not responding to atropine and usually lasts for 5–6 days.[104] Type III symptoms or delayed neurotoxicity of OPs occur after 8–12 days with severe distal weakness due to axonal neuropathy.
Electrophysiological studies by Indian investigators during such paralysis showed normal distal latency and NCV even in severely paralyzed patients with reduced CMAP amplitude more severely affected cases. Low rate repetitive nerve stimulation (RNS) did not reveal any decrement, but significant decrement was observed at high rate (30 Hz) RNS even in the absence of paralysis.[105]
Delayed OP neurotoxicity, especially in relation to triorthocresyl phosphate (TOCP), has been reported following outbreaks in Mumbai, in which 58 patients were affected.[106] Four outbreaks have been reported from Bengal due to imported flour contaminated with TOCP[107] and adulteration of rapeseed oil.[108] In a report on 592 patients, 50% patients had diarrhea and vomiting initially. After an interval of 1–3 weeks, paralytic phase developed ranging from quadriplegia to foot drop and wrist drop. Proximal lower limb muscles were affected in 40% patients, rare upper limb involvement and ankle reflexes were absent in all with evidence of axonal degeneration and reinnervation on electrodiagnostic study. Later, myelopathic features appeared in up to 65% cases. After 2 years, 25% patients recovered completely and about 65% patients returned to occupation.[109]
Alcoholic neuropathy
Polyneuropathy has been reported to be present in 13%–66% of chronic alcoholics.[110] The relative risk of polyneuropathy in chronic alcoholics is estimated at 3.9 times.[111] The pathophysiology of alcoholic polyneuropathy combines the toxic effect of alcohol with nutritional deficiency.[112] Both alcoholic neuropathy and thiamine-deficiency neuropathy are mainly of axonal type and are usually characterized by painful sensory disturbance and weakness in the distal lower extremities. Autonomic dysfunction often occurs. Pure alcoholic neuropathy without accompanying thiamine deficiency mainly affects small fibers, whereas thiamine-deficiency neuropathy predominantly affects large fibers polyneuropathy with predominantly motor symptoms.[112]
In a study on 33 patients with liver cirrhosis, sensory motor axonal neuropathy was present in 7 (21%) and nerve conductions were abnormal in 24 (73%) which was present in both alcohol and nonalcohol-related cirrhosis. Neuropathy was subclinical in majority of patients with cirrhosis (73%) and was not related to alcohol.[113]
In another study by Bajaj et al.,[114] 16 out of twenty patients with cirrhosis of liver had autonomic neuropathy, and the frequency was comparable between alcoholic and nonalcoholics. The severity of autonomic neuropathy increased with severity of liver damage suggesting liver damage was primarily responsible for autonomic neuropathy.
In a study carried out on thirty patients admitted at a tertiary hospital in Southern India with a history suggestive of alcohol dependence syndrome, the prevalence of neuropathy was 63.3%.[115]
Drug-induced toxic neuropathies
There are many drugs that cause polyneuropathy as an adverse effect. An Indian study estimated the incidence of polyneuropathy from medications or toxins to be 2%–4%.[116] However, there are no epidemiological data but mostly anecdotal reports.
NUTRITIONAL NEUROPATHY
Malnutrition affects both peripheral and CNS. PN may coexist with myelopathy (myeloneuropathy) can be seen with nutritional neuropathies.
They most commonly affect neuron itself and myelin sheath in peripheral nervous system resulting in either clinical or subclinical neuropathy. In a study on 67 children, nerve conduction velocities were found to be markedly decreased in protein energy malnutrition (PEM) Grades 3 and 4 as compared to the controls. Nerve conduction velocities were lower in children when the age of onset of malnutrition was <12 months.[117] In another study on 43 children, abnormality of motor nerve conduction was directly related to the severity of PCM and presence of hypotonia and/or hyporeflexia. Nerve dysfunction was not only entirely due to PEM but also contributed by many nutrient deficiencies.[118] Large myelinated fibers and sensory fibers are more affected than small myelinated and motor fibers.[119]
Vitamin B12, B6, niacin, and thiamine deficiencies result in PN of predominantly axonal distal symmetrical sensory-motor type. However, well-designed studies on these are lacking.
Tropical ataxic neuropathy
Tropical myeloneuropathies are classified into two clinical syndromes that can have overlapping features – tropical ataxic neuropathy (TAN) and tropical spastic paraparesis TAN are predominantly a SN seen in malnourished populations who consume large quantities of cassava. In a study of clinical and laboratory profile of forty TAN cases diagnosed in a tertiary referral center in Kerala, demographic characteristics included female preponderance, peak age at onset in the thirties, rural residence, and poor socioeconomic status. In addition to SN, 90% had decreased hearing, 50% decreased vision, and 25% had spasticity of lower extremities. Serum, urine, and sural nerve thiocyanate levels were significantly elevated in the patients and cessation of cassava intake, and better nutrition caused improvement in the neurological disability.[120]
CRITICAL ILLNESS POLYNEUROPATHY
Critical illness polyneuropathy is a condition occurring in critically ill patients who have been on mechanical ventilation for more than 1 week and usually identified by failure to wean the patient from ventilator. Based on clinical evaluation alone, an incidence of 25%–36% has been shown in prospective studies.[121,122] Electrophysiologic testing revealed that neuropathy and/or myopathy is present in 52%–57% of patients in Intensive Care Unit for 7 days or more.[123] In a cohort of 100 patients with sepsis, 37 patients had features of neuropathy, 81% of which developed it in the first 14 days, Acute Physiology and Chronic Health Evaluation II score ≥15, and use of neuromuscular blocking agents were significant risk factors.[124] In another study[125] to characterize the prevalence, time of onset, and cause of neuromuscular dysfunction in patients with severe sepsis, abnormal NCS was present in 31 out 48 patients (63%). Development of acquired neuromuscular dysfunction could be predicted by NCS done on day 7. Presence of abnormal baseline NCS was predictive of hospital mortality (55% vs. 0% for patients with normal baseline NCS; P < 0.001).
PARANEOPLASTIC NEUROPATHY
In up to 50% of patients with carcinoma, PN can be due to treatment toxicity, tumorous infiltration, metabolic disturbances, or terminal cachexia.[126] Neuropathy is defined as paraneoplastic when none of the above causes are detected or when cancer-related immunological mechanisms are involved. About 15% of patients with cancer develop a paraneoplastic sensorimotor neuropathy, which is usually mild and develops during the terminal stage of the disease.[127] There is another group that may precede the diagnosis of the tumor. The majority of paraneoplastic neuropathies develop rapidly in a matter of weeks and subsequently stabilizes or continues to progress until the patient's death.[128] In patient in remission, development of paraneoplastic neuropathy may signify tumor recurrence.[129]
In a study on paraneoplastic vasculitic neuropathy (PVN), out of 14 cases of paraneoplastic neuropathies, four had PVN with age of onset more than 50 years. Pain was seen in three patients. Two patients were previously treated for a thymoma and two were diagnosed with a colonic carcinoma and lung carcinoma, respectively.[130]
HEREDITARY NEUROPATHIES
The inherited neuropathies can broadly be classified into two groups: Those in which neuropathy is primary (e.g. Charcot–Marie–Tooth disease, CMT) and those in which neuropathy is part of generalized neurological or multisystem disorder.
CMT is a common form of inherited PN and estimated prevalence is 40–82 per 100,000 people.[131,132] In Indian hospital-based study, the frequency was found to be 4.8%.[7]
In a series of twenty patients of CMT type 1, the inheritance pattern was autosomal recessive (AR) in four families and five sporadic cases were present.[133] Males were commonly affected, and predominant pattern was axonal type.
Amyloid neuropathy is another hereditary neuropathy due to deposition of transthyretin or less commonly other proteins, in peripheral nerves. It may be an acquired disorder secondary to B-cell dyscrasia and immunoglobulin light chain deposition. In a report from North-West India, six members of a family spanning two generations were affected with polyneuropathy, autonomic neuropathy, vitreous, and cardiac involvement.[134]
In hereditary neuropathy associated with systemic degeneration, most cases in India have been described in association with patients of spinocerebellar ataxia by Wadia et al.[135] having sensory axonal neuropathy and AR hereditary SN with spastic paraplegia described by Thomas et al.[136] in five patients, four of whom were from India.
Limitation
Although it has been an effort to put into perspective the major studies in India on PN and its subtypes, there remains many untouched portions such as entrapment neuropathies, cranial neuropathies, porphyria-associated neuropathies due to drugs and toxins apart from the mentioned, plant and animal toxins-induced neuropathies, and traumatic neuropathies.
CONCLUSION
Thus, PN is a group of neurological disorder with varied etiologies caused by hereditary, metabolic, toxic, and environmental causes. In India, because of varied ethnicity and environmental causes, PN due to diabetes, GBS, leprosy, toxin-like arsenic, and TOCP poisoning are common. Yet, there are other such as vasculitic neuropathies, drug-induced neuropathies, and hereditary neuropathies where well-designed studies are lacking. However, many of our series are hospital based or clinic based which had got inherent bias, we need more community-based studies to search for the real scenario in different parts of India. The studies also highlight the regional differences which are important to know to arrive at appropriate pattern of PN and undertaking proper preventive measures. Yet, many a times, even after intensive investigation, one may not arrive at an etiological diagnosis warranting long-term follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bharucha NE, Bharucha AE, Bharucha EP. Prevalence of peripheral neuropathy in the Parsi community of Bombay. Neurology. 1991;41:1315–7. doi: 10.1212/wnl.41.8.1315. [DOI] [PubMed] [Google Scholar]
- 2.Das SK, Sanyal K. Neuroepidemiology of major neurological disorders in rural Bengal. Neurol India. 1996;44:47–58. [PubMed] [Google Scholar]
- 3.Das S, Sanyal K, Moitra A. A pilot study on neuroepidemiology in urban Bengal. Indian J Public Health. 1998;42:34–6. 41. [PubMed] [Google Scholar]
- 4.Saha SP, Bhattacharya S, Das SK, Maity B, Roy T, Raut DK. Epidemiological study of neurological disorders in a rural population of Eastern India. J Indian Med Assoc. 2003;101:299–300. 302-4. [PubMed] [Google Scholar]
- 5.Samsuzzaman MD, Bhattacharyya PK, Manna N, Das S. A comparative study on socio-demographic profile, working environment and morbidity profile among shoemakers and non shoemakers in a slum area of Kolkata. IOSR J Dent Med Sci. 2014;13:38–41. [Google Scholar]
- 6.Gourie-Devi M, Gururaj G, Satishchandra P, Subbakrishna DK. Prevalence of neurological disorders in Bangalore, India: A community-based study with a comparison between urban and rural areas. Neuroepidemiology. 2004;23:261–8. doi: 10.1159/000080090. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh B, Sengupta S, Bhattacharjee R, Pal S, Saha SP, Ganguly G, et al. Spectrum of peripheral neuropathy in Eastern India. J Indian Med Assoc. 2006;104:168–170. 3. [PubMed] [Google Scholar]
- 8.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban South Indian population: The Chennai Urban Rural Epidemiology Study (CURES-55) Diabet Med. 2008;25:407–12. doi: 10.1111/j.1464-5491.2008.02397.x. [DOI] [PubMed] [Google Scholar]
- 9.Raman R, Gupta A, Krishna S, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic microvascular complications in newly diagnosed type II diabetes mellitus. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS, report 27) J Diabetes Complications. 2012;26:123–8. doi: 10.1016/j.jdiacomp.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Ashok S, Ramu M, Deepa R, Mohan V. Prevalence of neuropathy in type 2 diabetic patients attending a diabetes centre in South India. J Assoc Physicians India. 2002;50:546–50. [PubMed] [Google Scholar]
- 11.D’Souza M, Kulkarni V, Bhaskaran U, Ahmed H, Naimish H, Prakash A, et al. Diabetic peripheral neuropathy and its determinants among patients attending a tertiary health care centre in Mangalore, India. J Public Health Res. 2015;4:450. doi: 10.4081/jphr.2015.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rani PK, Raman R, Rachapalli SR, Pal SS, Kulothungan V, Sharma T. Prevalence and risk factors for severity of diabetic neuropathy in type 2 diabetes mellitus. Indian J Med Sci. 2010;64:51–7. [PubMed] [Google Scholar]
- 13.Bansal D, Gudala K, Muthyala H, Esam HP, Nayakallu R, Bhansali A. Prevalence and risk factors of development of peripheral diabetic neuropathy in type 2 diabetes mellitus in a tertiary care setting. J Diabetes Investig. 2014;5:714–21. doi: 10.1111/jdi.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill HK, Yadav SB, Ramesh V, Bhatia E. A prospective study of prevalence and association of peripheral neuropathy in Indian patients with newly diagnosed type 2 diabetes mellitus. J Postgrad Med. 2014;60:270–5. doi: 10.4103/0022-3859.138750. [DOI] [PubMed] [Google Scholar]
- 15.Agrawal RP, Ola V, Bishnoi P, Gothwal S, Sirohi P, Agrawal R. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. J Assoc Physicians India. 2014;62:504–8. [PubMed] [Google Scholar]
- 16.Agrawal RP, Beniwal R, Sharma S, Purohit VP, Kochar DK, Kothari RP. Prevalence of micro and macro vascular complications in type 2 diabetes and their risk factors. Int J Diabetes Dev Ctries. 2004;24:11–6. [Google Scholar]
- 17.Dutta A, Naorem S, Singh TP, Wangjam K. Prevalence of peripheral neuropathy in newly diagnosed type 2 diabetics mellitus. Int J Diabetes Dev Ctries. 2005;25:30–3. [Google Scholar]
- 18.Kumar A, Alam MI, Reza TA, Sonal S, Sinha KK, Bhargav K, Alam W. An observational study of lipid profile and prevalence of microvascular complication in type 2 diabetes mellitus patients: A hospital based study. J Evid Based Med Healthc. 2016;3:2655–61. [Google Scholar]
- 19.Sosale A, Prasanna Kumar KM, Sadikot SM, Nigam A, Bajaj S, Zargar AH, et al. Chronic complications in newly diagnosed patients with type 2 diabetes mellitus in India. Indian J Endocrinol Metab. 2014;18:355–60. doi: 10.4103/2230-8210.131184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maser RE, Steenkiste AR, Dorman JS, Nielsen VK, Bass EB, Manjoo Q, et al. Epidemiological correlates of diabetic neuropathy. Report from Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes. 1989;38:1456–61. doi: 10.2337/diab.38.11.1456. [DOI] [PubMed] [Google Scholar]
- 21.Pickup J, Wilham G. Epidemiology of diabetes. In: Guikshank K, editor. Textbook of Diabetes. New York: Blackwell Science; 1991. [Google Scholar]
- 22.Singleton JR, Smith AG, Bromberg MB. Increased prevalence of impaired glucose tolerance in patients with painful sensory neuropathy. Diabetes Care. 2001;24:1448–53. doi: 10.2337/diacare.24.8.1448. [DOI] [PubMed] [Google Scholar]
- 23.Viswanathan V, Seena R, Nair MB, Snehalatha C, Bhoopathy RM, Ramachandran A. Nerve conduction abnormalities in different stages of glucose intolerance. Neurol India. 2004;52:466–9. [PubMed] [Google Scholar]
- 24.Babu MM, Kiran MR, Ravindra K, Srinivas V, Kandregula P, Vardhan RV, et al. Clinical manifestation and prevalence of peripheral neuropathy and nerve dysfunction in patients with chronic kidney disease. Int J Res Med Sci. 2015;3:451–5. [Google Scholar]
- 25.Sharma R, Gautam P, Gaur S, Kumar S, Taneja V. Evaluation of central neuropathy in patients of chronic renal failure with normal hearing. Indian J Otol. 2012;18:76–81. [Google Scholar]
- 26.Hughes RA, Rees JH. Clinical and epidemiologic features of Guillain-Barré syndrome. J Infect Dis. 1997;176(Suppl 2):S92–8. doi: 10.1086/513793. [DOI] [PubMed] [Google Scholar]
- 27.Van Koningsveld R, Van Doorn PA, Schmitz PI, Ang CW, Van der Meché FG. Mild forms of Guillain-Barré syndrome in an epidemiologic survey in the Netherlands. Neurology. 2000;54:620–5. doi: 10.1212/wnl.54.3.620. [DOI] [PubMed] [Google Scholar]
- 28.Randomised trial of plasma exchange, intravenous immunoglobulin, and combined treatments in Guillain-Barré syndrome. Plasma Exchange/Sandoglobulin Guillain-Barré Syndrome Trial Group. Lancet. 1997;349:225–30. [PubMed] [Google Scholar]
- 29.Merkies IS, Schmitz PI, Samijn JP, van der Meché FG, van Doorn PA. Fatigue in immune-mediated polyneuropathies. European Inflammatory Neuropathy Cause and Treatment (INCAT) Group. Neurology. 1999;53:1648–54. doi: 10.1212/wnl.53.8.1648. [DOI] [PubMed] [Google Scholar]
- 30.Yuki N, Hartung HP. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294–304. doi: 10.1056/NEJMra1114525. [DOI] [PubMed] [Google Scholar]
- 31.Talukder RK, Sutradhar SR, Rahman KM, Uddin MJ, Akhter H. Guillian-Barre syndrome. Mymensingh Med J. 2011;20:748–56. [PubMed] [Google Scholar]
- 32.Kalita J, Misra UK, Goyal G, Das M. Guillain-Barré syndrome: Subtypes and predictors of outcome from India. J Peripher Nerv Syst. 2014;19:36–43. doi: 10.1111/jns5.12050. [DOI] [PubMed] [Google Scholar]
- 33.Chaudhuri JR, Alladi S, Kandadai RM, Bandaru VS. Clinical outcome of Guillain-Barré syndrome with various treatment methods and cost effectiveness: A study from tertiary care center in South India: Yashoda GBS Registry. Neurol Asia. 2014;19:263–70. [Google Scholar]
- 34.Fakih Z, Khanikar D, Baruah C, Das M. A clinical study of prognostic factors of Guillain Barré syndrome in a tertiary care hospital of North-East India. Int J Med Res Prof. 2016;2:170–6. [Google Scholar]
- 35.Gupta D, Nair M, Baheti NN, Sarma PS, Kuruvilla A Diplomate-American Board. Electrodiagnostic and clinical aspects of Guillain-Barré syndrome: An analysis of 142 cases. J Clin Neuromuscul Dis. 2008;10:42–51. doi: 10.1097/CND.0b013e31818e9510. [DOI] [PubMed] [Google Scholar]
- 36.Alexander M, Prabhakar AT, Aaron S, Thomas M, Mathew V, Patil AK. Utility of neurophysiological criteria in Guillain Barreé syndrome: Subtype spectrum from a tertiary referral hospital in India. Neurol India. 2011;59:722–6. doi: 10.4103/0028-3886.86548. [DOI] [PubMed] [Google Scholar]
- 37.Vengamma B. Managing critically ill patients with AIDP: Relevance of international guideline to Indian scenario. Jaypee Publication, Medicine update. 2013 [Google Scholar]
- 38.Gibbels E, Giebisch U. Natural course of acute and chronic monophasic inflammatory demyelinating polyneuropathies (IDP). A retrospective analysis of 266 cases. Acta Neurol Scand. 1992;85:282–91. doi: 10.1111/j.1600-0404.1992.tb04045.x. [DOI] [PubMed] [Google Scholar]
- 39.Hughes R, Sanders E, Hall S, Atkinson P, Colchester A, Payan P. Subacute idiopathic demyelinating polyradiculoneuropathy. Arch Neurol. 1992;49:612–6. doi: 10.1001/archneur.1992.00530300044009. [DOI] [PubMed] [Google Scholar]
- 40.Chiò A, Cocito D, Bottacchi E, Buffa C, Leone M, Plano F, et al. Idiopathic chronic inflammatory demyelinating polyneuropathy: An epidemiological study in Italy. J Neurol Neurosurg Psychiatry. 2007;78:1349–53. doi: 10.1136/jnnp.2007.114868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iijima M, Koike H, Hattori N, Tamakoshi A, Katsuno M, Tanaka F, et al. Prevalence and incidence rates of chronic inflammatory demyelinating polyneuropathy in the Japanese population. J Neurol Neurosurg Psychiatry. 2008;79:1040–3. doi: 10.1136/jnnp.2007.128132. [DOI] [PubMed] [Google Scholar]
- 42.Wadwekar V, Kalita J, Misra UK. Does the chronic inflammatory demyelinating polyradiculoneuropathy due to secondary cause differ from primary? Neurol India. 2011;59:664–8. doi: 10.4103/0028-3886.86537. [DOI] [PubMed] [Google Scholar]
- 43.Moore PM, Richardson B. Neurology of the vasculitides and connective tissue diseases. J Neurol Neurosurg Psychiatry. 1998;65:10–22. doi: 10.1136/jnnp.65.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singhal BS, Khadilkar SV, Gursahani RD, Surya N. Vasculitic neuropathy: Profile of twenty patients. J Assoc Physicians India. 1995;43:459–61. [PubMed] [Google Scholar]
- 45.Biswas M, Chatterjee A, Ghosh SK, Dasgupta S, Ghosh K, Ganguly PK. Prevalence, types, clinical associations, and determinants of peripheral neuropathy in rheumatoid patients. Ann Indian Acad Neurol. 2011;14:194–7. doi: 10.4103/0972-2327.85893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saigal R, Bhargav R, Goyal L, Agrawal A, Mital P, Wadhwani D. Peripheral neuropathy in systemic lupus erythematosus: Clinical and electrophysiological properties and their association with disease activity parameters. J Assoc Physicians India. 2015;63:15–9. [PubMed] [Google Scholar]
- 47.Morgello S, Estanislao L, Simpson D, Geraci A, DiRocco A, Gerits P, et al. HIV-associated distal sensory polyneuropathy in the era of highly active antiretroviral therapy: The Manhattan HIV Brain Bank. Arch Neurol. 2004;61:546–51. doi: 10.1001/archneur.61.4.546. [DOI] [PubMed] [Google Scholar]
- 48.Simpson DM, Tagliati M. Nucleoside analogue-associated peripheral neuropathy in human immunodeficiency virus infection. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;9:153–61. [PubMed] [Google Scholar]
- 49.Dubey TN, Raghuvanshi SS, Sharma H, Saxena R. HIV neuropathy in pre-HAART patients and it's correlation with risk factors in Central India. Neurol India. 2013;61:478–80. doi: 10.4103/0028-3886.121912. [DOI] [PubMed] [Google Scholar]
- 50.Ellis RJ, Rosario D, Clifford DB, McArthur JC, Simpson D, Alexander T, et al. Continued high prevalence and adverse clinical impact of human immunodeficiency virus-associated sensory neuropathy in the era of combination antiretroviral therapy: The CHARTER Study. Arch Neurol. 2010;67:552–8. doi: 10.1001/archneurol.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shikuma C, Gerschenson M, Ananworanich J, Valcour V, Teeratakulpisarn N, Jadwattanakul T, et al. Determinants of epidermal nerve fibre density in antiretroviral-naïve HIV-infected individuals. HIV Med. 2012;13:602–8. doi: 10.1111/j.1468-1293.2012.01024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sacktor N, Lyles RH, Skolasky R, Kleeberger C, Selnes OA, Miller EN, et al. HIV-associated neurologic disease incidence changes: Multicenter AIDS Cohort Study, 1990-1998. Neurology. 2001;56:257–60. doi: 10.1212/wnl.56.2.257. [DOI] [PubMed] [Google Scholar]
- 53.Watters MR, Poff PW, Shiramizu BT, Holck PS, Fast KM, Shikuma CM, et al. Symptomatic distal sensory polyneuropathy in HIV after age 50. Neurology. 2004;62:1378–83. doi: 10.1212/01.wnl.0000120622.91018.ea. [DOI] [PubMed] [Google Scholar]
- 54.Luma HN, Tchaleu BC, Doualla MS, Temfack E, Sopouassi VN, Mapoure YN, et al. HIV-associated sensory neuropathy in HIV-1 infected patients at the Douala General Hospital in Cameroon: A cross-sectional study. AIDS Res Ther. 2012;9:35. doi: 10.1186/1742-6405-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Skopelitis EE, Kokotis PI, Kontos AN, Panayiotakopoulos GD, Konstantinou K, Kordossis T, et al. Distal sensory polyneuropathy in HIV-positive patients in the HAART era: An entity underestimated by clinical examination. Int J STD AIDS. 2006;17:467–72. doi: 10.1258/095646206777689062. [DOI] [PubMed] [Google Scholar]
- 56.Nations SP, Katz JS, Lyde CB, Barohn RJ. Leprous neuropathy: An American perspective. Semin Neurol. 1998;18:113–24. doi: 10.1055/s-2008-1040867. [DOI] [PubMed] [Google Scholar]
- 57.World Health Organization. Progress towards eliminating leprosy as a public health problem. Wkly Epidemiol Rec. 1994;20:145–51. [PubMed] [Google Scholar]
- 58.Global leprosy: Update on the 2012 situation. Wkly Epidemiol Rec. 2013;88:365–79. [PubMed] [Google Scholar]
- 59.Global leprosy update, 2013; reducing disease burden. Wkly Epidemiol Rec. 2014;89:389–400. [PubMed] [Google Scholar]
- 60.National Leprosy Eradication Programme (NLEP) – Progress Report for the Year 2013-14. [Last accessed on 2016 Sep 29]. Available from: http://www.nlep.nic.in/pdf/Progress%20report%2031st%20March%202013.14 .
- 61.Suneetha S, Arunthathi S, Chandi S, Kurian N, Chacko CJ. Histological studies in primary neuritic leprosy: Changes in the apparently normal skin. Lepr Rev. 1998;69:351–7. doi: 10.5935/0305-7518.19980035. [DOI] [PubMed] [Google Scholar]
- 62.Mahajan PM, Jogaikar DG, Mehta JM. A study of pure neuritic leprosy: Clinical experience. Indian J Lepr. 1996;68:137–41. [PubMed] [Google Scholar]
- 63.Narang T, Vinay K, Kumar S, Dogra S. A critical appraisal on pure neuritic leprosy from India after achieving WHO global target of leprosy elimination. Lepr Rev. 2016;87:456–63. [PubMed] [Google Scholar]
- 64.van Brakel WH, Nicholls PG, Das L, Barkataki P, Suneetha SK, Jadhav RS, et al. The INFIR Cohort Study: Investigating prediction, detection and pathogenesis of neuropathy and reactions in leprosy. Methods and baseline results of a cohort of multibacillary leprosy patients in North India. Lepr Rev. 2005;76:14–34. [PubMed] [Google Scholar]
- 65.Kumar B, Kaur I, Dogra S, Kumaran MS. Pure neuritic leprosy in India: An appraisal. Int J Lepr Other Mycobact Dis. 2004;72:284–90. doi: 10.1489/0020-7349(2004)72<284:PNLIIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 66.Bhat RM, Chaitra P. Profile of new leprosy cases attending a South Indian referral hospital in 2011-2012. ISRN Trop Med. 2013;2013:4. [Google Scholar]
- 67.Sarkar J, Dasgupta A, Dutt D. Disability among new leprosy patients, an issue of concern: An institution based study in an endemic district for leprosy in the state of West Bengal, India. Indian J Dermatol Venereol Leprol. 2012;78:328–34. doi: 10.4103/0378-6323.95449. [DOI] [PubMed] [Google Scholar]
- 68.Mendiratta V, Khan A, Jain A. Primary neuritic leprosy: A reappraisal at a tertiary care hospital. Indian J Lepr. 2006;78:261–7. [PubMed] [Google Scholar]
- 69.Gourie-Devi M. Greater auricular nerve conduction in leprosy. Indian J Lepr. 1984;56:182–90. [PubMed] [Google Scholar]
- 70.World Health Organization. Diphtheria: Immunization Surveillance, Assessment, and Monitoring. [Last cited on 2013 Mar 05]. Available from: http://www.who.int/immunization_monitoring/diseases/diphteria/en/index.html .
- 71.Mateen FJ, Bahl S, Khera A, Sutter RW. Detection of diphtheritic polyneuropathy by acute flaccid paralysis surveillance, India. Emerg Infect Dis. 2013;19:1368–73. doi: 10.3201/eid1909.130117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kanwal SK, Yadav D, Chhapola V, Kumar V. Post-diphtheritic neuropathy: A clinical study in paediatric Intensive Care Unit of a developing country. Trop Doct. 2012;42:195–7. doi: 10.1258/td.2012.120293. [DOI] [PubMed] [Google Scholar]
- 73.Talsania N, Chauhan J, Nayak H, Shaha C, Modi K, Devaliya J. Investigation of an outbreak of diphtheria in Dabela village of Amirgagh taluka and CHC, Banaskantha, Gujarat (current scenario) Natl J Community Med. 2011;2:196–200. [Google Scholar]
- 74.Manikyamba D, Satyavani A, Deepa P. Diphtheritic polyneuropathy in the wake of resurgence of diphtheria. J Pediatr Neurosci. 2015;10:331–4. doi: 10.4103/1817-1745.174441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nandi R, De M, Browning S, Purkayastha P, Bhattacharjee AK. Diphtheria: The patch remains. J Laryngol Otol. 2003;117:807–10. doi: 10.1258/002221503770716250. [DOI] [PubMed] [Google Scholar]
- 76.Singh N, Singh A, Gaur S. A study of diphtheria menace in Kumaun region of Uttarakhand state in India. Journal Of Drug Delivery and Therapeutics. 2013;3:105–7. [Google Scholar]
- 77.Havaldar PV. Diphtheria in the eighties: Experience in a South Indian district hospital. J Indian Med Assoc. 1992;90:155–6. [PubMed] [Google Scholar]
- 78.Saper RB, Kales SN, Paquin J, Burns MJ, Eisenberg DM, Davis RB, et al. Heavy metal content of Ayurvedic herbal medicine products. JAMA. 2004;292:2868–73. doi: 10.1001/jama.292.23.2868. [DOI] [PubMed] [Google Scholar]
- 79.Feldman RG, Niles CA, Kelly-Hayes M, Sax DS, Dixon WJ, Thompson DJ, et al. Peripheral neuropathy in arsenic smelter workers. Neurology. 1979;29:939–44. doi: 10.1212/wnl.29.7.939. [DOI] [PubMed] [Google Scholar]
- 80.Mukherjee SC, Rahman MM, Chowdhury UK, Sengupta MK, Lodh D, Chanda CR, et al. Neuropathy in arsenic toxicity from groundwater arsenic contamination in West Bengal, India. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2003;38:165–83. doi: 10.1081/ese-120016887. [DOI] [PubMed] [Google Scholar]
- 81.Chhuttani PN, Chawla LS, Sharma TD. Arsenical neuropathy. Neurology. 1967;17:269–74. doi: 10.1212/wnl.17.3.269. [DOI] [PubMed] [Google Scholar]
- 82.Chakraborti D, Mukherjee SC, Saha KC, Chowdhury UK, Rahman MM, Sengupta MK. Arsenic toxicity from homeopathic treatment. J Toxicol Clin Toxicol. 2003;41:963–7. doi: 10.1081/clt-120026518. [DOI] [PubMed] [Google Scholar]
- 83.Rahman MM, Chowdhury UK, Mukherjee SC, Mondal BK, Paul K, Lodh D, et al. Chronic arsenic toxicity in Bangladesh and West Bengal, India – A review and commentary. J Toxicol Clin Toxicol. 2001;39:683–700. doi: 10.1081/clt-100108509. [DOI] [PubMed] [Google Scholar]
- 84.Albers JW, Garabrant DH. Arsenic poisoning. In: Lynn DJ, Newton HB, editors. The 5-Minute Neurology Consult. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. pp. 70–1. [Google Scholar]
- 85.Donofrio PD, Wilbourn AJ, Albers JW, Rogers L, Salanga V, Greenberg HS. Acute arsenic intoxication presenting as Guillain-Barré-like syndrome. Muscle Nerve. 1987;10:114–20. doi: 10.1002/mus.880100203. [DOI] [PubMed] [Google Scholar]
- 86.Fischbein A. Environmental and occupational lead exposure. Environ Occup Med. 1983;57:433–47. [Google Scholar]
- 87.Ellis T, Lacy R. Illicit alcohol (moonshine) consumption in West Alabama revisited. South Med J. 1998;91:858–60. doi: 10.1097/00007611-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 88.Ibrahim AS, Latif AH. Adult lead poisoning from a herbal medicine. Saudi Med J. 2002;23:591–3. [PubMed] [Google Scholar]
- 89.Conradi S, Ronnevi LO, Norris FH. Motor neuron disease and toxic metals. Adv Neurol. 1982;36:201–31. [PubMed] [Google Scholar]
- 90.Mohapatra BN, Panda KN, Dash P. Lead toxicity in garage and petrol pump workers in Orissa. J Assoc Physicians India. 1998;46:97. [Google Scholar]
- 91.Shobha N, Taly AB, Sinha S, Venkatesh T. Radial neuropathy due to occupational lead exposure: Phenotypic and electrophysiological characteristics of five patients. Ann Indian Acad Neurol. 2009;12:111–5. doi: 10.4103/0972-2327.53080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clarkson TW, Friberg L, Nordberg GF, Sager PR. Mercury. Biological Monitoring of Toxic Metals. New York: Plenum Press; 1988. pp. 199–246. [Google Scholar]
- 93.Feldman RG. Neurological manifestations of mercury intoxication. Acta Neurol Scand Suppl. 1982;92:201–9. [PubMed] [Google Scholar]
- 94.Hänninen H. Behavioral effects of occupational exposure to mercury and lead. Acta Neurol Scand Suppl. 1982;92:167–75. [PubMed] [Google Scholar]
- 95.Bromberg MB. Peripheral neurotoxic disorders. Neurol Clin. 2000;18:681–94. doi: 10.1016/s0733-8619(05)70218-8. [DOI] [PubMed] [Google Scholar]
- 96.Albers JW, Kallenbach LR, Fine LJ, Langolf GD, Wolfe RA, Donofrio PD, et al. Neurological abnormalities associated with remote occupational elemental mercury exposure. Ann Neurol. 1988;24:651–9. doi: 10.1002/ana.410240510. [DOI] [PubMed] [Google Scholar]
- 97.Saper RB, Phillips RS, Sehgal A, Khouri N, Davis RB, Paquin J, et al. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. JAMA. 2008;300:915–23. doi: 10.1001/jama.300.8.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Karunasagar D, Balarama Krishna MV, Anjaneyulu Y, Arunachalam J. Studies of mercury pollution in a lake due to a thermometer factory situated in a tourist resort: Kodaikanal, India. Environ Pollut. 2006;143:153–8. doi: 10.1016/j.envpol.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 99.Singh S, Wig N, Chaudhary D, Sood NK, Sharma BK. Changing pattern of acute poisoning in adults: Experience of a large North West Indian hospital (1970-1989) J Assoc Physicians India. 1997;45:194–7. [Google Scholar]
- 100.Lall SB, Peshin SS, Seth SD. Acute poisoning: A ten years retrospective study. Ann Natl Acad Med Sci. 1994;30:35–44. [Google Scholar]
- 101.Malik GM, Mubarik M, Romshoo GJ. Organophosphorus poisoning in the Kashmir Valley, 1994 to 1997. N Engl J Med. 1998;338:1078. doi: 10.1056/NEJM199804093381520. [DOI] [PubMed] [Google Scholar]
- 102.Siwach SB, Gupta A. The profile of acute poisonings in Harayana-Rohtak Study. J Assoc Physicians India. 1995;43:756–9. [PubMed] [Google Scholar]
- 103.Jeyaratnam J. Acute pesticide poisoning: A major global health problem. World Health Stat Q. 1990;43:139–44. [PubMed] [Google Scholar]
- 104.Wadia RS, Sadagopan C, Amin RB, Sardesai HV. Neurological manifestations of organophosphorus insecticide poisoning. J Neurol Neurosurg Psychiatry. 1974;37:841–7. doi: 10.1136/jnnp.37.7.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wadia RS, Chitra S, Amin RB, Kiwalkar RS, Sardesai HV. Electrophysiological studies in acute organophosphate poisoning. J Neurol Neurosurg Psychiatry. 1987;50:1442–8. doi: 10.1136/jnnp.50.11.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vora DD, Dastur DK, Braganca BM, Parihar LM, Iyer CG, Fondekar RB, et al. Toxic polyneuritis in Bombay due to ortho-cresyl-phosphate poisoning. J Neurol Neurosurg Psychiatry. 1962;25:234–42. doi: 10.1136/jnnp.25.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chakraborty A, Mukherjee S, Chaterjee S. TOCP neuropathy: The Indian scene. Med Update. 1992;2:3483–55. [Google Scholar]
- 108.Chaudhuri RN. Recent outbreak of a paralytic disease in Malda, West Bengal. Bull Calcutta Sch Trop Med. 1962;10:141–52. [PubMed] [Google Scholar]
- 109.Sarangi NN, Das SK. TOCP neuropathy. Rev Neurol. 1995;2:191–201. [Google Scholar]
- 110.Koike H, Sobue G. Alcoholic neuropathy. Curr Opin Neurol. 2006;19:481–6. doi: 10.1097/01.wco.0000245371.89941.eb. [DOI] [PubMed] [Google Scholar]
- 111.Beghi E, Monticelli ML. Chronic symmetric symptomatic polyneuropathy in the elderly: A field screening investigation of risk factors for polyneuropathy in two Italian communities. Italian General Practitioner Study Group (IGPST) J Clin Epidemiol. 1998;51:697–702. doi: 10.1016/s0895-4356(98)00039-0. [DOI] [PubMed] [Google Scholar]
- 112.Koike H, Iijima M, Sugiura M, Mori K, Hattori N, Ito H, et al. Alcoholic neuropathy is clinicopathologically distinct from thiamine-deficiency neuropathy. Ann Neurol. 2003;54:19–29. doi: 10.1002/ana.10550. [DOI] [PubMed] [Google Scholar]
- 113.Kharbanda PS, Prabhakar S, Chawla YK, Das CP, Syal P. Peripheral neuropathy in liver cirrhosis. J Gastroenterol Hepatol. 2003;18:922–6. doi: 10.1046/j.1440-1746.2003.03023.x. [DOI] [PubMed] [Google Scholar]
- 114.Bajaj BK, Agarwal MP, Ram BK. Autonomic neuropathy in patients with hepatic cirrhosis. Postgrad Med J. 2003;79:408–11. doi: 10.1136/pmj.79.933.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rebecca J, Peter G, Kavina F. Pattern of peripheral neuropathy among patients with alcohol dependence syndrome. IOSR J Dent Med. 2016;15:5–8. [Google Scholar]
- 116.Jain KK, editor. Drug-Induced Neurological Disorders. 2nd ed. Seattle: Hogrefe & Huber; 2001. Drug-induced peripheral neuropathies; pp. 263–94. [Google Scholar]
- 117.Ghosh S, Vaid K, Mohan M, Maheshwari MC. Effect of degree and duration of protein energy malnutrition on peripheral nerves in children. J Neurol Neurosurg Psychiatry. 1979;42:760–3. doi: 10.1136/jnnp.42.8.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chopra JS, Dhand UK, Mehta S, Bakshi V, Rana S, Mehta J. Effect of protein calorie malnutrition on peripheral nerves. A clinical, electrophysiological and histopathological study. Brain. 1986;109(Pt 2):307–23. doi: 10.1093/brain/109.2.307. [DOI] [PubMed] [Google Scholar]
- 119.Singh N, Kumar A, Ghai OP. Conduction velocity of motor nerves in children suffering from protein-calorie malnutrition and marasmus. Electromyogr Clin Neurophysiol. 1976;16:381–92. [PubMed] [Google Scholar]
- 120.Madhusudanan M, Menon MK, Ummer K, Radhakrishnanan K. Clinical and etiological profile of tropical ataxic neuropathy in Kerala, South India. Eur Neurol. 2008;60:21–6. doi: 10.1159/000127975. [DOI] [PubMed] [Google Scholar]
- 121.de Letter MA, Schmitz PI, Visser LH, Verheul FA, Schellens RL, Op de Coul DA, et al. Risk factors for the development of polyneuropathy and myopathy in critically ill patients. Crit Care Med. 2001;29:2281–6. doi: 10.1097/00003246-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 122.De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, et al. Paresis acquired in the Intensive Care Unit: A prospective multicenter study. JAMA. 2002;288:2859–67. doi: 10.1001/jama.288.22.2859. [DOI] [PubMed] [Google Scholar]
- 123.Leijten FS, Harinck-de Weerd JE, Poortvliet DC, de Weerd AW. The role of polyneuropathy in motor convalescence after prolonged mechanical ventilation. JAMA. 1995;274:1221–5. [PubMed] [Google Scholar]
- 124.Gupta S, Mishra M. Acute physiology and chronic health evaluation II score of ≥15: A risk factor for sepsis-induced critical illness polyneuropathy. Neurol India. 2016;64:640–5. doi: 10.4103/0028-3886.185356. [DOI] [PubMed] [Google Scholar]
- 125.Khan J, Harrison TB, Rich MM, Moss M. Early development of critical illness myopathy and neuropathy in patients with severe sepsis. Neurology. 2006;67:1421–5. doi: 10.1212/01.wnl.0000239826.63523.8e. [DOI] [PubMed] [Google Scholar]
- 126.Antoine JC, Mosnier JF, Absi L, Convers P, Honnorat J, Michel D. Carcinoma associated paraneoplastic peripheral neuropathies in patients with and without anti-onconeural antibodies. J Neurol Neurosurg Psychiatry. 1999;67:7–14. doi: 10.1136/jnnp.67.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Croft PB, Wilkinson M. The incidence of carcinomatous neuromyopathy in patients with various types of carcinoma. Brain. 1965;88:427–34. doi: 10.1093/brain/88.3.427. [DOI] [PubMed] [Google Scholar]
- 128.Rosenfeld MR, Dalmau J. Paraneoplastic syndromes of the Nervous system. In: Schiff D, Kesari S, Wen PY, editors. Cancer Neurology in Clinical Practice. 2nd ed. Totowa, NJ: Humana Press; 2008. pp. 237–55. [Google Scholar]
- 129.Sillevis Smitt P, Grefkens J, de Leeuw B, van den Bent M, van Putten W, Hooijkaas H, et al. Survival and outcome in 73 anti-Hu positive patients with paraneoplastic encephalomyelitis/sensory neuronopathy. J Neurol. 2002;249:745–53. doi: 10.1007/s00415-002-0706-4. [DOI] [PubMed] [Google Scholar]
- 130.Kannan MA, Challa S, Kandadai RM, Uppin MS, Jabeen SA, Borgohain R. Series of paraneoplastic vasculitic neuropathy: A rare, potentially treatable neuropathy. Neurol India. 2015;63:30–4. doi: 10.4103/0028-3886.152629. [DOI] [PubMed] [Google Scholar]
- 131.Pareyson D, Marchesi C. Diagnosis, natural history, and management of Charcot-Marie-Tooth disease. Lancet Neurol. 2009;8:654–67. doi: 10.1016/S1474-4422(09)70110-3. [DOI] [PubMed] [Google Scholar]
- 132.Braathen GJ. Genetic epidemiology of Charcot–Marie–Tooth disease. Acta Neurol Scand. 2012;126(Suppl. 193):iv–22. doi: 10.1111/ane.12013. doi: 10.1111/ane.12013. [DOI] [PubMed] [Google Scholar]
- 133.Nair KR. Acrodytrophic neuropathy. Neurol India. 1978;26:247–52. [Google Scholar]
- 134.Jain RS, Jain R, Mathur T, Raghavendra BS, Handa R, Jain A, et al. Hereditary amyloid polyneuropathy in a family from North West India: Phenotypic, MRI and pathologic study. J Assoc Physicians India. 2014;62:538–41. [PubMed] [Google Scholar]
- 135.Wadia NH, Irani PF, Mehta LN, et al. Evidence of peripheral neuropathy in a variety of heredofamilial olivopontocerebellar degeneration frequently seen in India. In: Sobue I, editor. Proceedings of the Internation Symposium on Spinocerebellar Degenerations. Tokyo: University of Tokyo Press; 1980. pp. 239–50. [Google Scholar]
- 136.Thomas PK, Misra VP, King RH, Muddle JR, Wroe S, Bhatia KP, et al. Autosomal recessive hereditary sensory neuropathy with spastic paraplegia. Brain. 1994;117:651–9. doi: 10.1093/brain/117.4.651. [DOI] [PubMed] [Google Scholar]


