Abstract
Background:
Cryptococcal meningitis is an important and a fatal neuroinfection. Early diagnosis and treatment is of utmost importance in reducing morbidity and mortality.
Materials and Methods:
Data of patients with laboratory-confirmed cryptococcal meningitis seen in tertiary care hospital were reviewed. Details of demographic profile, clinical data, laboratory parameters, complications, and in-hospital mortality were studied.
Results:
Among 97 patients with cryptococcal meningitis (79 men, 18 women), 88 were HIV-positive, two were diabetic, and seven were sporadic. Their age ranged from 23 to 67 years (39.16 ± 9.49). Additional pathogens for meningitis were identified in 24 patients. Headache was the most common symptom (91%) followed by fever (66%), vomiting (51%), altered sensorium (31%), and seizures (20%). Neurological deficits included cranial nerve palsies (28), motor deficits (11), sphincter disturbances (5), and sensory involvement in four patients. Complications included renal dysfunction (20%), dyselectrolytemia (20%), seizures (16%), hypersensitivity (7%), and hepatic dysfunction (5%). Favorable outcome was seen in 72 patients, 13 remained unchanged, and 12 died. Rapid clinical progression, low cerebrospinal fluid (CSF) cell count and protein were associated with higher mortality. CSF cell count and protein were lower in patients who had isolated cryptococcal meningitis compared to those with additional pathogen. Mean sugar levels were higher and duration of illness was shorter in HIV-negative individuals.
Conclusion:
Cryptococcal meningitis is common in patients with AIDS. Effective and early antifungal treatment carries a good prognosis. On rapid evolution of the disease, decreased CSF cell count and protein heralds poor prognosis and warrants initiation of early specific treatment.
Keywords: Cryptococcal meningitis, HIV, immunocompromised patient, opportunistic infections
INTRODUCTION
The incidence of infections caused by the encapsulated yeast Cryptococcus neoformans has risen markedly over the past 25 years as a result of the HIV epidemic and increasing the use of immunosuppressive therapies.[1] Cryptococcal meningitis is a common and fatal opportunistic neuroinfection seen in immunosuppressed as well as few immunocompetent individuals. Clinical manifestations include acute or subacute fever, headache, vomiting, and focal neurological deficits. It is one of the AIDS-defining illnesses in up to 69% of patients with HIV infection.[2] Mortality from HIV-associated cryptococcal meningitis remains high (up to 30%) even in developed countries because of complications related to cryptococcal infection and relative lack of efficacy of the currently available drugs.[1,3] In developing countries, financial constraint is a major deterrent in the management of this infection.[4] Higher mortality up to 44% is reported in Sub-Saharan Africa.[1,5] Early diagnosis and treatment is of utmost importance in reducing morbidity and mortality. There is inadequate information about its incidence, prevalence, and also important prognostic factors that herald poor prognosis in developing countries. This retrospective study was undertaken to evaluate the clinical profile, laboratory parameters, outcome, and prognostic factors in patients with cryptococcal meningitis.
MATERIALS AND METHODS
Case records of patients with meningitis admitted under neurological services of the teaching university hospital in Southern India from 2001 to 2014 were retrieved from the medical records after obtaining the Institutional Ethical Clearance. Case records of patients with cryptococcal meningitis were selected for the study. Diagnosis of cryptococcal meningitis was established by detection of cryptococci by at least one of the following methods which included India Ink preparation, culture positivity, or antigen positivity. Patients’ demography, medical history, past illness, vital parameters, examination findings, laboratory parameters, and cerebral imaging data were documented. Information regarding HIV status, duration of illness, drug history, and treatment including highly active antiretroviral therapy (HAART) were obtained. Data were obtained regarding the presence of diabetes mellitus, immunosuppression, autoimmune disorders, internal malignancy, and radiation. Women in childbearing age were evaluated for pregnancy status. The level of consciousness was documented using Glasgow Coma Scale, and the functional outcome was measured using modified Rankin score (mRS).
The study group was divided into HIV-positive and HIV-negative groups, and further comparison was made between isolated cryptococcal meningitis and cryptococcal meningitis with additional pathogens. Statistical analysis was performed using Statistical analysis was performed using Statistical Package for the Social Sciences software (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc). Descriptive data were tabulated and mean, standard deviation, and median of the data were calculated. Chi-square test or Fisher's exact test was used to compare dichotomous variables and t-test was used for continuous variables as appropriate. The association of clinical and laboratory features with the outcome was analyzed, and their 95% confidence intervals were calculated. For all the tests, P ≤ 0.05 was considered statistically significant.
RESULTS
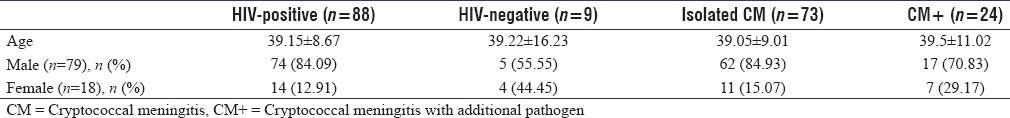
During the study period, 10,247 patients were admitted under neurological services among which 277 had neuro-AIDS. There were 97 patients with cryptococcal meningitis with 79 men and 18 women [Table 1]. Among these, 88 patients were HIV-positive (31.77% of neuro-AIDS patients). Among HIV-negative patients, two had diabetes and seven patients had no identifiable cause. Twenty-four patients had additional pathogen identified which included tuberculosis in 19, bacterial meningitis in four, and progressive multifocal leukoencephalopathy in one patient. Fifty-six patients were HIV seropositive from 15 days to 15 years (median 2 years) at presentation of whom 17 were on HAART. HIV infection was detected at presentation in 32 patients. Duration of the symptoms in HIV-negative patients was shorter (median 8 days) in comparison with HIV-positive patients (median 15 days).
Table 1.
The demographic data of the patients in relation to the HIV-positivity and presence of additional pathogens in the cerebrospinal fluid
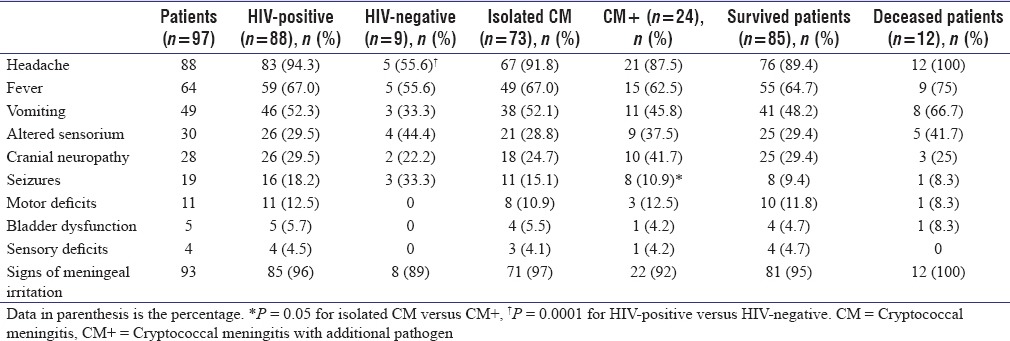
Headache was the most common symptom (91%) followed by fever (66%), vomiting (51%), altered sensorium (31%), and seizures (20%). Headache was significantly more frequent in HIV-positive patients. Seizures were significantly more in patients with isolated cryptococcal meningitis [Table 2]. The clinical features of the patients in relation to HIV status and presence of additional pathogen are shown in Table 2. Headache, fever, vomiting, and altered sensorium were more frequent in patients who died. Neurological deficits consisting of quadriparesis (five patients), hemiparesis (three patients), paraparesis (two patients), monoparesis (one patient), sensory abnormalities (four patients), and sphincter dysfunction (five patients) were seen only in HIV-positive patients. Nine patients had facial palsy, five had abducent palsy, seven had papilledema, two had optic atrophy, one had oculomotor, and one each had chorioretinitis and HIV retinopathy. Two had sensorineural deafness and seven patients had limb ataxia.
Table 2.
The clinical features of the patients with cryptococcal meningitis
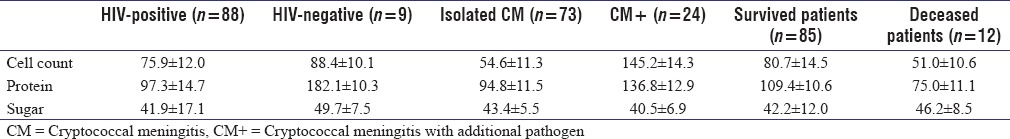
Anemia was present in 76 patients. Leukopenia was seen selectively in HIV-positive patients (five patients) whereas among the HIV-negative patients, six had leukocytosis. Mean sugar levels were higher in non-HIV patients (148.77 mg/dl) as compared to HIV-positive patients (119.03 mg/dl). Fourteen patients had hyponatremia (12 HIV-positive, two HIV-negative) and one had hypernatremia. Sodium levels were lower in patients who had additional pathogens as compared to those with isolated cryptococcal meningitis (132.83 ± 5.45 mEq/L vs. 135.9 ± 4.62 mEq/L; P = 0.02). Nine patients had hypokalemia (eight HIV-positive, one HIV-negative). Cerebrospinal fluid (CSF) analysis revealed higher protein level in HIV-negative patients. Patients with isolated cryptococcal meningitis and those who succumbed had lower CSF protein and cellularity [Table 3]. Cranial imaging data were available in 83 patients which revealed infarction in seven patients, atrophy in five patients, granuloma in two patients, cortical and brainstem hyperintensities in two patients, features of progressive multifocal leukoencephalopathy in one patient, and hydrocephalus in one patient.
Table 3.
The cerebrospinal fluid analysis findings in patients with cryptococcal meningitis
Seventy-eight patients were treated with amphotericin among whom 62 tolerated the drug and 28 had adverse effects including renal dysfunction (19), dyselectrolytemia (16), hypersensitivity (7), and hepatic dysfunction.(5). Three patients who had renal dysfunction with amphotericin B were shifted to liposomal amphotericin. Among the remaining patients with azotemia, some patients could be restarted on conventional amphotericin after renal functions stabilized. None of the patients received intrathecal amphotericin. Fifteen patients had seizures during treatment. Patients not tolerating or not affording amphotericin were treated with fluconazole or voriconazole. Mean duration of amphotericin therapy was 12 days. Patients at discharge were put on fluconazole. Favorable outcome defined as change in mRS at discharge from baseline by two grades was seen in 72 patients, 13 remained unchanged, and 12 patients died. Among the 12 patients who died, five had seizures during treatment (41.7%) as against ten patients (11.7%) who survived. There was no significant association between Glasgow coma score at admission and outcome. Similarly, prior use of HAART did not alter the outcome.
DISCUSSION
Epidemiological studies have revealed increasing incidence of cryptococcal meningitis. From the documented global incidence of cryptococcal meningitis of about 500 patients in the 1950s, there has been tremendous increase in the incidence of cryptococcal meningitis with the epidemic of AIDS and the use of multiple immunomodulatory drugs.[2] Cryptococcal meningitis is one of the most common opportunistic infections in patients with AIDS. Before the introduction of HAART, 5%–10% of patients with AIDS developed cryptococcal meningitis. Although the numbers have fallen, this disease remains a major concern in Asia and Africa.[6,7]
Patients with cryptococcal meningitis have various causes of immunodeficiency. Malignancies, drug-induced immunosuppression, and primary immunodeficiency states were the most common predisposing causes for cryptococcal meningitis before the AIDS epidemic. However, from the 1980s, HIV infection and AIDS are the most common predisposing factors for the occurrence of cryptococcal meningitis. A study from India documented HIV infection in 43.9% of the 60 patients included from 1978 to 1995 with cryptococcal meningitis.[8] Recent studies have demonstrated a higher incidence of AIDS-related cryptococcal meningitis in 88.7% which is comparable with our data.[9] A study from the United States showed a higher occurrence of cryptococcal meningitis in non-HIV patients as compared to the present study which is probably due to higher use of immunomodulation in developed countries.[5] Cryptococcal meningitis was an AIDS-defining illness in 31.77% of our patients which is far less than the study from Zimbabwe.[10]
Majority of the studies have documented male predominance which is similar to the present study.[9,11,12] However, few studies have demonstrated female predominance.[13] Duration of the symptoms before diagnosis of cryptococcal meningitis in majority of HIV-positive patients was reported to be longer compared with HIV-negative patients as seen in our study.[11] In addition, the duration of symptoms was shorter in patients who died or had no improvement which could be due to increased severity of meningitis.
It is interesting to see that motor deficits, sphincter involvement, and sensory disturbances were seen only in HIV-positive patients. Headache was significantly more among the HIV-positive patients, which needs further correlation with CSF pressure studies and cerebral imaging. Seizures and altered sensorium were seen more in non-HIV patients which differ from data published in a recent study.[9] The presence of altered sensorium, fever, and features of raised intracranial pressure was reported to be more frequent in the patients who died similar to the observations in our patients.[14] Patients who had seizures during the treatment had higher mortality in our study.
Magnitude of CSF pleocytosis among patients without HIV infection was documented to be higher compared to patients with HIV infection.[15] Although we have a smaller HIV-negative group, similar findings were seen in our patients. An important observation in our patients was the lower degree of CSF pleocytosis and lower protein levels among the patients who succumbed probably reflecting the poor immunological status. Our study showed that 73% of the patients tolerated amphotericin while others had complications, azotemia being the most common which limited the use of the drug.
Prior use of HAART among HIV patients with cryptococcal meningitis has been documented to be associated with better outcome.[16] However, in our patients, the outcome was not modified by HAART status which is probably explained by inadequate details about drug compliance. Mortality among our patients was higher in HIV-positive patients in contrast with earlier reports documenting higher mortality in HIV-negative patients.[12] This may be due to smaller number of HIV-negative patients. Long-term follow-up would be required to ascertain the true mortality rate. We also found that the mortality was higher when patients had additional pathogen along with Cryptococcus highlighting the importance of searching and treating the coexisting opportunistic infections. Factors that determined poor outcome were shorter duration of illness, seizures while on treatment, low CSF cellularity, and protein level. Retrospective nature of the study along with unavailability of CD4 counts, viral load data, and unequal comparative groups was the limitations of this study. Prospective long-term studies would be helpful in assessing the outcome in these patients.
CONCLUSION
Cryptococcal meningitis remains a common and potentially lethal opportunistic infection in AIDS and other immunodeficient states. Cryptococcal meningitis can coexist with other pathogens, which needs to be diligently searched and treated. Low CSF cellularity and the phenotype of illness with seizures could predict poor outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull. 2005;72:99–118. doi: 10.1093/bmb/ldh043. [DOI] [PubMed] [Google Scholar]
- 2.Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997-2009. PLoS One. 2013;8:e56269. doi: 10.1371/journal.pone.0056269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robinson PA, Bauer M, Leal MA, Evans SG, Holtom PD, Diamond DA, et al. Early mycological treatment failure in AIDS-associated cryptococcal meningitis. Clin Infect Dis. 1999;28:82–92. doi: 10.1086/515074. [DOI] [PubMed] [Google Scholar]
- 4.Sloan DJ, Dedicoat MJ, Lalloo DG. Treatment of cryptococcal meningitis in resource limited settings. Curr Opin Infect Dis. 2009;22:455–63. doi: 10.1097/QCO.0b013e32832fa214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.French N, Gray K, Watera C, Nakiyingi J, Lugada E, Moore M, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS. 2002;16:1031–8. doi: 10.1097/00002030-200205030-00009. [DOI] [PubMed] [Google Scholar]
- 6.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–30. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 7.Okongo M, Morgan D, Mayanja B, Ross A, Whitworth J. Causes of death in a rural, population-based human immunodeficiency virus type 1 (HIV-1) natural history cohort in Uganda. Int J Epidemiol. 1998;27:698–702. doi: 10.1093/ije/27.4.698. [DOI] [PubMed] [Google Scholar]
- 8.Khanna N, Chandramuki A, Desai A, Ravi V. Cryptococcal infections of the central nervous system: An analysis of predisposing factors, laboratory findings and outcome in patients from South India with special reference to HIV infection. J Med Microbiol. 1996;45:376–9. doi: 10.1099/00222615-45-5-376. [DOI] [PubMed] [Google Scholar]
- 9.Abhilash KP, Mitra S, Arul JJ, Raj PM, Balaji V, Kannangai R, et al. Changing paradigm of cryptococcal meningitis: An eight-year experience from a tertiary hospital in South India. Indian J Med Microbiol. 2015;33:25–9. doi: 10.4103/0255-0857.148372. [DOI] [PubMed] [Google Scholar]
- 10.Heyderman RS, Gangaidzo IT, Hakim JG, Mielke J, Taziwa A, Musvaire P, et al. Cryptococcal meningitis in human immunodeficiency virus-infected patients in Harare, Zimbabwe. Clin Infect Dis. 1998;26:284–9. doi: 10.1086/516298. [DOI] [PubMed] [Google Scholar]
- 11.van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337:15–21. doi: 10.1056/NEJM199707033370103. [DOI] [PubMed] [Google Scholar]
- 12.Prasad KN, Agarwal J, Nag VL, Verma AK, Dixit AK, Ayyagari A. Cryptococcal infection in patients with clinically diagnosed meningitis in a tertiary care center. Neurol India. 2003;51:364–6. [PubMed] [Google Scholar]
- 13.Boaz MM, Kalluvya S, Downs JA, Mpondo BC, Mshana SE. Pattern, clinical characteristics, and outcome of meningitis among HIV-infected adults admitted in a tertiary hospital in North Western Tanzania: A cross-sectional study. J Trop Med 2016. 2016 doi: 10.1155/2016/6573672. 6573672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar S, Wanchu A, Chakrabarti A, Sharma A, Bambery P, Singh S. Cryptococcal meningitis in HIV infected: Experience from a North Indian tertiary center. Neurol India. 2008;56:444–9. [PubMed] [Google Scholar]
- 15.Patel AK, Patel KK, Ranjan R, Shah S, Patel JK. Management of cryptococcal meningitis in HIV-infected patients: Experience from Western India. Indian J Sex Transm Dis. 2010;31:22–6. doi: 10.4103/2589-0557.68996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Antinori S, Ridolfo A, Fasan M, Magni C, Galimberti L, Milazzo L, et al. AIDS-associated cryptococcosis: A comparison of epidemiology, clinical features and outcome in the pre- and post-HAART eras. Experience of a single centre in Italy. HIV Med. 2009;10:6–11. doi: 10.1111/j.1468-1293.2008.00645.x. [DOI] [PubMed] [Google Scholar]


