Abstract
Background:
Abnormal carotid intima-media thickness (IMT) is a marker of carotid atherosclerosis which is a risk factor for cerebrovascular and cardiovascular diseases. Recent studies have found an association of 25-hydroxyvitamin D deficiency with abnormal carotid IMT.
Purpose:
The purpose of the study was to investigate the association of serum 25-hydroxyvitamin D levels with carotid IMT in Indian participants.
Materials and Methods:
We prospectively recruited 300 participants at Yashoda Hospital, Hyderabad, during the study period between January 2012 and December 2014. All participants were assessed for fasting blood sugar, lipid profile, C-reactive protein (CRP), serum alkaline phosphatase, serum calcium, serum phosphorous, serum 25-hydroxyvitamin D levels, and carotid Doppler examination.
Results:
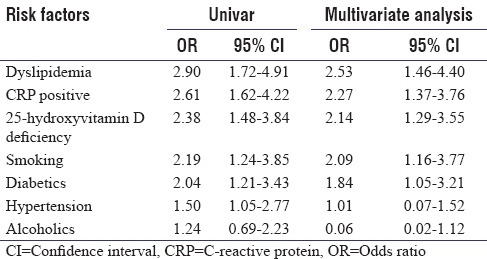
Among the 300 participants, men were 190 (63.3%) and mean age was 51.9 ± 7.7 years with a range from 35 to 64 years. On risk factors evaluation, 105 (35%) were hypertensive, 79 (26.3%) diabetics, 63 (21%) smokers, and 56 (18.6%) were alcoholics. On evaluation of biochemical parameters, 81 (27%) had dyslipidemia, 120 (40%) had elevated CRP levels, 119 (39.6%) had 25-hydroxyvitamin D deficiency, mean alkaline phosphatase was 93.9 ± 14.9 IU/L, serum calcium (mg/dL) was 9.2 ± 2.3, and serum phosphorous 4.4 ± 1.2 mg/dL. On carotid imaging, 121 (40.3%) had abnormal IMT. After multivariate analysis, 25-hydroxyvitamin D deficiency (odds ratio [OR]: 2.14; 95% confidence interval [CI]: 1.29–3.55), dyslipidemia (OR: 2.53; 95% CI: 1.46–4.40), elevated CRP (OR: 2.27; 95% CI: 1.37–3.76), smoking (OR: 2.09; 95% CI: 1.16–3.77), and diabetes (OR: 1.84; 95% CI: 1.05–3.21) were independently associated with abnormal IMT.
Conclusion:
In our study, we established 25-hydroxyvitamin D deficiency as an independently associated with abnormal IMT in Indian participants.
Keywords: Carotid atherosclerosis, intima-media thickness, Indian participants, serum 25-hydroxyvitamin D
INTRODUCTION
Atherosclerosis is a common disease, rapidly increasing in its prevalence worldwide, and is associated with high morbidity and mortality. Abnormal intima-media thickness (IMT) which can be detected on ultrasound, is a reliable marker of carotid atherosclerosis, and is a predictor for future risk of cardiovascular and cerebrovascular diseases.[1] Several researches have established an association of abnormal carotid IMT with vascular risk factors.[1]
Current studies have suggested a link between serum 25-hydroxyvitamin D deficiency and increased carotid IMT in general population.[2]
25-hydroxyvitamin D (cholecalciferol) is a fat-soluble vitamin belonging to the secosteroid group and is responsible for optimizing the intestinal absorption of calcium and phosphate and maintain the balance between the two.[3] Vitamin D deficiency exists in epidemic proportion throughout India, and population-based studies have shown a prevalence of 40%–45% in the general population.[3] We aim to investigate the effect of serum 25-hydroxyvitamin D levels on carotid IMT in Indian population as there are very few studies on this topic from the Indian subcontinent.
MATERIALS AND METHODS
This was a prospective cross-sectional study. We recruited 300 consecutive participants from Department of Neurology in Yashoda Hospital, Hyderabad, during the study period from January 2012 to December 2014 after taking written informed consent. Yashoda Hospital is a tertiary care medical center and a postgraduation teaching hospital in South India. This study was approved by the Institutional Ethics Committee.
Inclusion and exclusion criteria
All participants with no present or past history of cardiovascular or cerebrovascular disease were included in the study. Participants with osteomalacia, bone pains, muscle weakness, Vitamin D deficiency or Vitamin D or calcium supplementation, and any other bone disease were excluded from the study.
All participants’ data were collected through face-to-face interview and records of present and past medical history. All participants underwent testing for fasting blood sugar, lipid profile, serum calcium, serum alkaline phosphatase, serum phosphorous, C-reactive protein (CRP), serum 25-hydroxyvitamin D levels, and carotid Doppler assessment.
Hypertension was defined by Joint National Committee VI–VII guidelines, diabetes was diagnosed by criteria laid down by the World Health Organization, dyslipidemia as per the guidelines of the National Institutes of Health, USA, alcoholics were defined as those in whom the alcohol consumption was more than 50 g/day, and smokers were defined as those reporting daily smoking. Ex-smokers and occasional smokers were categorized as nonsmokers, and CRP positive ≥10 mg/L was considered positive.[1,4]
Estimation of 25-hydroxyvitamin D
We used chemiluminescent microparticle immunoassay with automated instrument for estimation of 25-hydroxyvitamin D, and this instrument sensitivity and specificity were 53% and 90.5%, respectively. According to laboratory manual and current literature, serum 25-hydroxyvitamin D values ≤20 ng/mL were considered deficient and more than 20 ng/mL as normal.[3,4,5]
Evaluation of carotid Doppler
The ultrasonographic examination was performed by qualified radiologists. The sonographic machine used in this study was a high-resolution duplex ultrasound system, Philips HD11XE duplex, and B-mode scan was performed with a probe at scanner frequency of 3–12 MHz. The examination was done over 2 cm of common carotid artery (CCA) and the carotid artery bulb. IMT on mid-CCA was measured in all participants. The thickness of IMT ≤0.07 cm was normal [Figure 1] and ≥0.08 cm was considered abnormal [Figure 2].[1,6]
Figure 1.
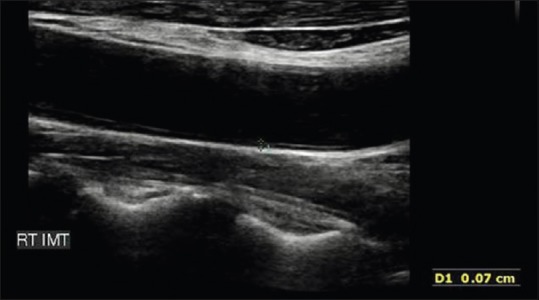
Normal carotid intima-media thickness
Figure 2.
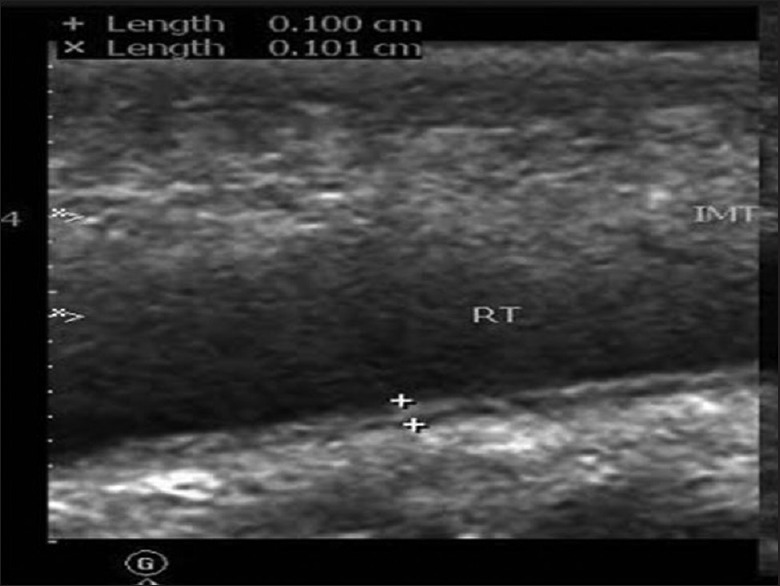
Abnormal carotid intima-media thickness
Statistical analysis
Statistical analysis was performed using SPSS Version 14.0 (Statistical Package for the Social Sciences (SPSS) SPSS Inc Chicago city Illinois state USA). Titers of mean ± standard deviations were used to describe continuous variable. Differences in continuous variables were assessed using Student's t-test and Chi-square test was used to evaluate the association in proportions. We calculated the odds ratio (OR) and the resulting 95% confidence interval (CI) for the effect of various risk factors on IMT. We performed multiple logistic regression analysis for association between carotid IMT and various risk factors (CRP, serum 25-hydroxyvitamin D, hypertension, diabetic, smoking, and alcoholics). All tests were two sided and P < 0.05 was considered statistically significant.
RESULTS
Out of 372 participants screened, 300 participants were included in the study [Figure 3]. Among 300 participants, 190 (63.3%) were men and mean age was 51.9 ± 7.7 years (age range 35–64 years). Among the risk factors, participants with hypertension were 105 (35%), diabetes 79 (26.3%), smoking 63 (21%), alcoholism 56 (18.6%), obesity 20 (6.6%), and dyslipidemia 81 (27%).
Figure 3.
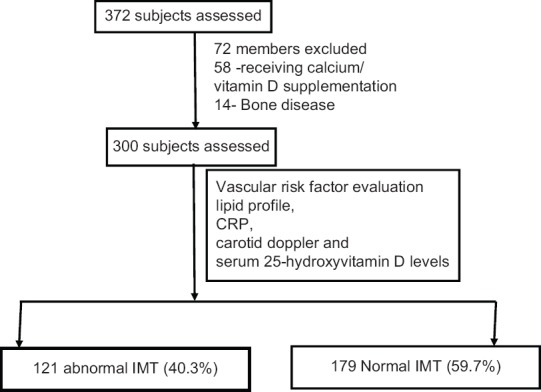
Flowchart
Abnormal carotid IMT was noted in 121 (40.3%) and serum 25-hydroxyvitamin D deficiency in 119 (39.6%) participants. CRP was positive in 120 (40%), mean serum calcium, phosphorus, and alkaline phosphatase were 9.2 ± 2.3 mg/dl, 4.4 ± 1.2 mg/dl, and 93.9 ± 14.9 IU/L, respectively.
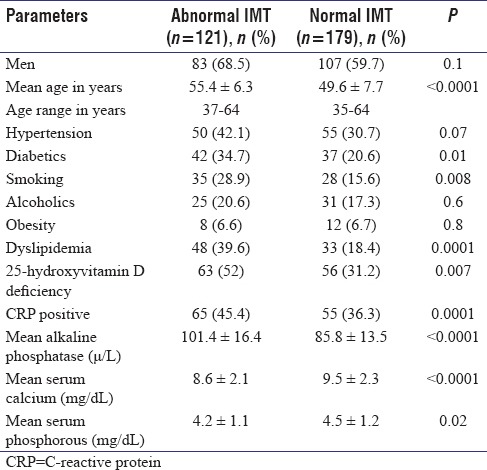
We dichotomized the study population into abnormal IMT and normal IMT.
On comparing the two groups, older age (mean 55.4 ± 6.3 [P < 0.0001]), higher prevalence of diabetes 42 (34.7%) (P = 0.01), smoking 35 (28.9%) (P = 0.008), dyslipidemia 48 (39.6%) (P = 0.0001), serum 25-hydroxyvitamin D deficiency 63 (52%) (P = 0.007), and CRP positivity 65 (45.4%) (P = 0.0001) along with elevated mean alkaline phosphatase (101.4 ± 16.4 μ/L [P < 0.0001]), lower mean serum calcium (8.6 ± 2.1 mg/dL [P < 0.0001]), and lower mean serum phosphorous levels (4.2 ± 1.1 mg/dL [P = 0.02]) were found in abnormal IMT group compared to normal IMT group and were statistically significant [Table 1].
Table 1.
Comparison between abnormal intima-media thickness and normal intima-media thickness with various risk factors
After multivariate analysis using multiple logistic regression analysis, serum 25-hydroxyvitamin D deficiency (OR: 2.14; 95% CI: 1.29–3.55), diabetes (OR: 1.84; 95% CI: 1.05–3.21), smoking (OR: 2.09; 95% CI: 1.16–3.77), dyslipidemia (OR: 2.53; 95% CI: 1.46–4.40), and CRP positivity (OR: 2.27; 95% CI: 1.37–3.76) were independently associated with abnormal IMT [Table 2].
Table 2.
Univariate and multivariate analysis
DISCUSSION
In the present study on India population, we found a significant association of serum 25-hydroxyvitamin D deficiency with abnormal IMT, and similar findings were advocated by studies from various countries,[2,7,8,9,10,11,12,13,14] Carrelli et al.[2] and Reis et al.[7] from America, Richart et al. from Belgium,[8] Pacific et al. from Italy (children and adolescents),[9] Lim et al. from Korea,[10] Zang et al.[11] and Ma[12] et al. from China, Oz et al. from Turkey,[13] and Sypniewska et al. from Poland.[14]
The mechanism by which deficiency of Vitamin D is associated with atherosclerosis is not fully understood. Vitamin D receptors are not exclusively detected in the bone and mineral pathway but are ubiquitous and have a wide tissue distribution including vascular smooth muscle cells and vascular endothelial cells. The diverse physiological actions of Vitamin D on the vascular wall include reduction of smooth muscle cell proliferation, reduction of macrophage secretion of pro-inflammatory cytokines interleukin (IL)-6 and tumor necrosis factor-a, and increased secretion of the anti-inflammatory cytokine IL-10 and thus reduces the state of vascular inflammation.[15] In addition, peripheral lymphocytes also express receptors for Vitamin D and convert circulating 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D which further reduces the proliferation of lymphocytes. This anti-inflammatory effect may have a protective role as there is increasing evidence that systemic inflammation leads to atherosclerosis.[3]
Li et al.[16] observed an effect of Vitamin D on blood pressure regulation caused by suppressing the renin-angiotensin system. Aihara et al.[17] demonstrated that Vitamin D inhibited thrombosis and reduced arterial calcification. Juonala et al. observed that presence of low levels of 25-hydroxyvitamin D in childhood translated to a high risk of developing abnormal carotid IMT in adulthood even after adjustment for several potential confounding factors.[18]
Our study establishes an independent association of deficiency of 25-hydroxyvitamin D abnormal carotid IMT (OR: 2.14; 95% CI: 1.29–3.55) as advocated by others.[12] However, some studies have found no association between carotid IMT and serum 25-hydroxyvitamin D deficiency.[19,20]
In the present study, prevalence of hypertension was higher among participants with abnormal IMT (50 [42.1%]) compared to normal IMT (55 [30.7%]) with a trend toward significance (P = 0.07). Hypertension is a risk factor for atherosclerosis, and recent studies have found independent association of hypertension with abnormal IMT.[1] In our study, however, on multivariate analysis, we did not find a statistically significant association of hypertension with abnormal IMT (OR: 1.01; 95% CI: 0.07–1.52). This may be due to the fact that duration of hypertension, early detection, and adequacy of treatment of hypertension, the antihypertensive drug used can modify its effect on atherosclerosis.[21]
Diabetes is a major risk factor for atherosclerosis.[22] In our study, we found diabetes to be significantly associated with abnormal IMT (prevalence of 42 [34.7%] in abnormal IMT group compared to 37 [20.6%] in participants with normal IMT), and these findings were supported by others.[1]
Diabetes may accelerate atherosclerosis by a myriad of pathways. Hyperglycemia can cause a reduction in nitric oxide by increasing its consumption by an increase in reactive oxygen species. Reduction in nitric oxide can cause endothelial dysfunction. Advanced glycation end products can cause activation of pro-inflammatory cytokines and promote atherogenesis. Low-density lipoprotein (LDL) is prone to glycation which may induce antibodies which are proinflammatory. The role of infections may be emphasized by diabetes. Further, both diabetes and atherosclerosis may have a common inflammatory pathway.[23]
In our study, we established diabetes as an independent risk factor associated with abnormal IMT (OR: 1.84; 95% CI: 1.05–3.21). Similar findings were described recently by Kaul et al.[1]
Several epidemiological studies have noted a strong relationship between cigarette smoking and atherosclerosis.[24] We also observed a significantly higher percentage of smokers among the abnormal IMT group (35 [28.9%]) compared to normal IMT (28 [15.6%]); these findings were supported by others.[24,25] Howard et al. noted that even past smokers had increased atherosclerosis compared to nonsmokers.[26] Schott et al. found in his study that smoking was associated with increased IMT in carotid bulb only.[27] Johnson et al. observed a higher risk of atherosclerosis among female smokers compared to male smokers.[24] In our study, none of the women smoked.
Various epidemiological studies as well as animal experiments have shown that both active smoking and passive exposure to smoke can cause vasomotor dysfunction, atherogenesis, and vascular thrombosis.[1] Even though a complete pathophysiological pathway remains elusive, the effect of smoking on atherosclerosis seems to be through free radical-mediated oxidative stress.[28] These free radicals may be generated directly from cigarette smoke and indirectly from endogenous sources as well.[29]
In our study, we found smoking as an independent risk factor for increasing IMT (OR: 2.09; 95% CI: 1.16–3.77), and our findings are advocated by others.[1,30]
In the current study, we found no relationship between alcohol consumption and abnormal carotid IMT in men, our finding advocated by others.[1,31] However, some studies have found an association between consumption of alcohol and abnormal carotid IMT in healthy participants.[32]
In the present study, dyslipidemia was significantly higher in participants with abnormal IMT compared to normal IMT (P < 0.0001), our findings were accounted by other studies.[33] Dyslipidemia is probably the most important risk factor predisposing to atherosclerosis. Elevated levels of LDL, triglycerides, and free fatty acids as well as reduced high-density lipoprotein can tip the balance toward endothelial dysfunction by increasing oxidative stress and stimulating inflammation and thrombosis.[23] In our study, we established dyslipidemia to be independently associated with abnormal IMT (OR: 2.53; 95% CI: 1.46–4.40), similar to other studies.[1]
In the present study, we found a significant association between CRP positivity and abnormal carotid IMT, as advocated by others.[34] Suh et al. established in his study a gender predisposition and found that elevated CRP was significantly associated with abnormal carotid IMT levels in women but not in men.[35]
CRP, a marker of inflammation, is associated with atherosclerosis.[33] However, it is still not very clear how CRP contributes to the genesis of cardiovascular and cerebrovascular diseases. CRP may exacerbate atherogenesis by its interactions with immunological and inflammatory factors, for example, the complement system and may also have a direct effect on the cells associated with atherosclerotic lesions.[35]
In the present study, we established positive CRP as an independent risk factor for abnormal carotid IMT (OR: 2.27; 95% CI: 1.37–3.76) and our finding was advocated by previous studies.[36] However, some studies have found no relationship between positive CRP and carotid IMT.[37]
There is a growing evidence that 25-hydroxyitamin D deficiency is associated with other risk factors predisposing to atherosclerosis such as diabetes, dyslipidemia, and inflammation.[4,5,8] In this study, we have demonstrated an independent association of Vitamin D deficiency on atherosclerosis. Thus, the impact of Vitamin D deficiency on atherosclerosis is a compound activity of its independent association as well as its effect on various risk factors making it a formidable risk factor.
Strengths and limitations
In this study, we recruited 300 participants from a single center have used a single laboratory for analysis of serum 25-hydroxyvitamin D levels, and the Doppler evaluation of carotid arteries in all participants were done by one qualified radiologist – thus effectively preventing bias from inter-rater variability. The age range was wide and included participants from 35 to 62 years. However, the main drawbacks of the study were that we did not further analyze the carotid plaque measurements and characteristics including carotid stiffness markers, and we did not assess the impact of seasonal variations, medications, socioeconomic status or the diet, and their effect on serum-25-hydroxyvitamin D levels. We used chemiluminescent microparticle immunoassay for Vitamin D estimation, and reports have suggested that it may underestimate levels in comparison to high-pressure liquid chromatography–tandem mass spectrometry which is not feasible in our setup.
CONCLUSION
In the present study, we established an independent association of deficiency of 25-hydroxyvitamin D with abnormal IMT in Indian population. Our findings suggest that individuals with deficiency of 25-hydroxyvitamin D have a risk of developing cardiovascular and cerebrovascular disease. Although this study does not address the impact of treatment, there is a possibility that improving Vitamin D status might be a potential public health strategy to reduce atherosclerosis. Further large-scale, multicentric studies are required to confirm these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Dr. G.S Rao, Managing Director of Yashoda group of hospitals and Dr. Lingaih A, DMS, for their immense support, which made it possible for us to conduct this study at Yashoda Hospital, Hyderabad, Telangana, India.
REFERENCES
- 1.Kaul S, Alladi S, Mridula RK, Bandaru SV, Boddu DB, Anjanikumar D, et al. Prevalence and risk factors of carotid intima-media thickness in asymptomatic individual subjects in a tertiary care center in India. Ann Indian Acad Neurol. 2015;18:430–4. doi: 10.4103/0972-2327.165481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carrelli AL, Walker MD, Lowe H, McMahon DJ, Rundek T, Sacco RL, et al. Vitamin D deficiency is associated with subclinical carotid atherosclerosis: The Northern Manhattan study. Stroke. 2011;42:2240–5. doi: 10.1161/STROKEAHA.110.608539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaudhuri JR, Mridula KR, Alladi S, Anamika A, Umamahesh M, Balaraju B, et al. Serum 25-hydroxyvitamin D deficiency in ischemic stroke and subtypes in Indian patients. J Stroke. 2014;16:44–50. doi: 10.5853/jos.2014.16.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhuri JR, Mridula KR, Anamika A, Boddu DB, Misra PK, Lingaiah A, et al. Deficiency of 25-hydroxyvitamin D and dyslipidemia in Indian subjects. J Lipids 2013. 2013 doi: 10.1155/2013/623420. 623420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhuri JR, Mridula KR, Lingaiah A, Balaraju B, Bandaru VC. Low serum levels of 25-hydroxyvitamin D in association with type 2 diabetes in Indian patients. Iran J Diabetes Obes. 2014;6:47–55. [Google Scholar]
- 6.Bandaru VC, Kaul S, Laxmi V, Neeraja M, Mahesh MU, Alladi S, et al. Antibodies to Chlamydia pneumoniae are associated with increased intima media thickness in asymptomatic Indian individuals. J Stroke Cerebrovasc Dis. 2009;18:190–4. doi: 10.1016/j.jstrokecerebrovasdis.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Reis JP, von Mühlen D, Michos ED, Miller ER, 3rd, Appel LJ, Araneta MR, et al. Serum Vitamin D, parathyroid hormone levels, and carotid atherosclerosis. Atherosclerosis. 2009;207:585–90. doi: 10.1016/j.atherosclerosis.2009.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richart T, Thijs L, Nawrot T, Yu J, Kuznetsova T, Balkestein EJ, et al. The metabolic syndrome and carotid intima-media thickness in relation to the parathyroid hormone to 25-OH-D (3) ratio in a general population. Am J Hypertens. 2011;24:102–9. doi: 10.1038/ajh.2010.124. [DOI] [PubMed] [Google Scholar]
- 9.Pacifico L, Anania C, Osborn JF, Ferraro F, Bonci E, Olivero E, et al. Low 25(OH) D3 levels are associated with total adiposity, metabolic syndrome, and hypertension in Caucasian children and adolescents. Eur J Endocrinol. 2011;165:603–11. doi: 10.1530/EJE-11-0545. [DOI] [PubMed] [Google Scholar]
- 10.Lim S, Shin H, Kim MJ, Ahn HY, Kang SM, Yoon JW, et al. Vitamin D inadequacy is associated with significant coronary artery stenosis in a community-based elderly cohort: The Korean longitudinal study on health and aging. J Clin Endocrinol Metab. 2012;97:169–78. doi: 10.1210/jc.2011-1580. [DOI] [PubMed] [Google Scholar]
- 11.Zang L, Fu P, Huang YQ, Wu M, Li L, Zang J, et al. Vitamin D deficiency and carotid artery intima-media thickness and coronary calcification in patients with diabetic nephropathy. Sichuan Da Xue Xue Bao Yi Xue Ban. 2012;43:420–4. 450. [PubMed] [Google Scholar]
- 12.Ma H, Lin H, Hu Y, Li X, He W, Jin X, et al. Serum 25-hydroxyvitamin D levels are associated with carotid atherosclerosis in normotensive and euglycemic Chinese postmenopausal women: The Shanghai Changfeng study. BMC Cardiovasc Disord. 2014;14:197. doi: 10.1186/1471-2261-14-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oz F, Cizgici AY, Oflaz H, Elitok A, Karaayvaz EB, Mercanoglu F, et al. Impact of Vitamin D insufficiency on the epicardial coronary flow velocity and endothelial function. Coron Artery Dis. 2013;24:392–7. doi: 10.1097/MCA.0b013e328362b2c8. [DOI] [PubMed] [Google Scholar]
- 14.Sypniewska G, Pollak J, Strozecki P, Camil F, Kretowicz M, Janikowski G, et al. 25-hydroxyvitamin D, biomarkers of endothelial dysfunction and subclinical organ damage in adults with hypertension. Am J Hypertens. 2014;27:114–21. doi: 10.1093/ajh/hpt174. [DOI] [PubMed] [Google Scholar]
- 15.van de Luijtgaarden KM, Voûte MT, Hoeks SE, Bakker EJ, Chonchol M, Stolker RJ, et al. Vitamin D deficiency may be an independent risk factor for arterial disease. Eur J Vasc Endovasc Surg. 2012;44:301–6. doi: 10.1016/j.ejvs.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 16.Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP. 1,25-dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110:229–38. doi: 10.1172/JCI15219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aihara K, Azuma H, Akaike M, Ikeda Y, Yamashita M, Sudo T, et al. Disruption of nuclear Vitamin D receptor gene causes enhanced thrombogenicity in mice. J Biol Chem. 2004;279:35798–802. doi: 10.1074/jbc.M404865200. [DOI] [PubMed] [Google Scholar]
- 18.Juonala M, Voipio A, Pahkala K, Viikari JS, Mikkilä V, Kähönen M, et al. Childhood 25-OH Vitamin D levels and carotid intima-media thickness in adulthood: The cardiovascular risk in young Finns study. J Clin Endocrinol Metab. 2015;100:1469–76. doi: 10.1210/jc.2014-3944. [DOI] [PubMed] [Google Scholar]
- 19.Giri R, Rai R, Verma S, Verma RK. Correlation between Vitamin D and carotid artery intima media thickness in patients with ischemic stroke. Int J Adv Med. 2016;3:398–401. [Google Scholar]
- 20.Winckler K, Tarnow L, Lundby-Christensen L, Almdal TP, Wiinberg N, Eiken P, et al. Vitamin D, carotid intima-media thickness and bone structure in patients with type 2 diabetes. Endocr Connect. 2015;4:128–35. doi: 10.1530/EC-15-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mizuno Y, Jacob RF, Mason RP. Effects of calcium channel and renin-angiotensin system blockade on intravascular and neurohormonal mechanisms of hypertensive vascular disease. Am J Hypertens. 2008;21:1076–85. doi: 10.1038/ajh.2008.258. [DOI] [PubMed] [Google Scholar]
- 22. [Last accessed on 2016 Apr 20]. Available from: http://www.news.medical.net/health/Risk-Factors-for-Atherosclerosis.aspx .
- 23.Frostegård J. Immune mechanisms in atherosclerosis, especially in diabetes type 2. Front Endocrinol (Lausanne) 2013;4:162. doi: 10.3389/fendo.2013.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson HM, Piper ME, Jorenby DE, Fiore MC, Baker TB, Stein JH. Risk factors for subclinical carotid atherosclerosis among current smokers. Prev Cardiol. 2010;13:166–71. doi: 10.1111/j.1751-7141.2010.00068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tzou WS, Douglas PS, Srinivasan SR, Bond MG, Tang R, Li S, et al. Distribution and predictors of carotid artery intima-media thickness in young adults: The Bogalusa Heart Study. Prev Cardiol. 2007;10:181–9. doi: 10.1111/j.1520-037x.2007.06450.x. [DOI] [PubMed] [Google Scholar]
- 26.Howard G, Wagenknecht LE, Burke GL, Diez-Roux A, Evans GW, McGovern P, et al. Cigarette smoking and progression of atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) study. JAMA. 1998;279:119–24. doi: 10.1001/jama.279.2.119. [DOI] [PubMed] [Google Scholar]
- 27.Schott LL, Wildman RP, Brockwell S, Simkin-Silverman LR, Kuller LH, Sutton-Tyrrell K. Segment-specific effects of cardiovascular risk factors on carotid artery intima-medial thickness in women at midlife. Arterioscler Thromb Vasc Biol. 2004;24:1951–6. doi: 10.1161/01.ATV.0000141119.02205.6b. [DOI] [PubMed] [Google Scholar]
- 28.Nakou ES, Liberopoulos EN, Milionis HJ, Elisaf MS. The role of C-reactive protein in atherosclerotic cardiovascular disease: An overview. Curr Vasc Pharmacol. 2008;6:258–70. doi: 10.2174/157016108785909733. [DOI] [PubMed] [Google Scholar]
- 29.Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: An update. J Am Coll Cardiol. 2004;43:1731–7. doi: 10.1016/j.jacc.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 30.Rosvall M, Persson M, Östling G, Nilsson PM, Melander O, Hedblad B, et al. Risk factors for the progression of carotid intima-media thickness over a 16-year follow-up period: The Malmö Diet and Cancer Study. Atherosclerosis. 2015;239:615–21. doi: 10.1016/j.atherosclerosis.2015.01.030. [DOI] [PubMed] [Google Scholar]
- 31.Lee YH, Shin MH, Kweon SS, Choi SW, Kim HY, Ryu SY, et al. Alcohol consumption and carotid artery structure in Korean adults aged 50 years and older. BMC Public Health. 2009;9:358. doi: 10.1186/1471-2458-9-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie X, Ma YT, Yang YN, Fu ZY, Ma X, Huang D, et al. Alcohol consumption and carotid atherosclerosis in China: The Cardiovascular Risk Survey. Eur J Prev Cardiol. 2012;19:314–21. doi: 10.1177/1741826711404501. [DOI] [PubMed] [Google Scholar]
- 33.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: The Rotterdam Study. Circulation. 1997;96:1432–7. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 34.Schulze Horn C, Ilg R, Sander K, Bickel H, Briesenick C, Hemmer B, et al. High-sensitivity C-reactive protein at different stages of atherosclerosis: Results of the INVADE study. J Neurol. 2009;256:783–91. doi: 10.1007/s00415-009-5017-6. [DOI] [PubMed] [Google Scholar]
- 35.Suh M, Lee JY, Ahn SV, Kim HC, Suh I. C-reactive protein and carotid intima-media thickness in a population of middle-aged Koreans. J Prev Med Public Health. 2009;42:29–34. doi: 10.3961/jpmph.2009.42.1.29. [DOI] [PubMed] [Google Scholar]
- 36.Trindade M, Martucci RB, Burlá AK, Oigman W, Neves MF, Araújo DV. Evaluation of clinical variables associated with increased carotid intima-media thickness in middle-aged hypertensive women. Int J Hypertens 2012. 2012 doi: 10.1155/2012/257501. 257501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grufman H, Gonçalves I, Edsfeldt A, Nitulescu M, Persson A, Nilsson M, et al. Plasma levels of high-sensitive C-reactive protein do not correlate with inflammatory activity in carotid atherosclerotic plaques. J Intern Med. 2014;275:127–33. doi: 10.1111/joim.12133. [DOI] [PubMed] [Google Scholar]


