Abstract
Introduction:
Orthostatic hypotension is defined as a sustained decrease in systolic blood pressure of 20 mm Hg or a decrease in diastolic blood pressure of 10 mm Hg within three minutes of standing compared with blood pressure from the sitting or supine position or by head-up tilt-table testing (1). When sustained blood pressure (BP) drop is after three minutes of upright posture it is called delayed orthostatic hypotension (delayed OH) (2).
Aim of the Study:
To detect the incidence of delayed orthostatic hypotension in patients referred to our autonomic lab.
Materials and Method:
BP was measured noninvasively at 1-minute intervals with an automated cuff sphygmomanometer over the right brachial artery for 45 minutes. The onset and duration of falls in blood pressure either systolic or diastolic or both were documented, and any associated symptoms were recorded. Only patients with sustained falls in BP were included. Drugs causing OH was stopped 48 hours before testing as per protocol followed in lab. We also looked into other autonomic function test abnormalities in patients with delayed OH.
Inclusion criteria:
Patients above age of 18 years referred for evaluation of autonomic function tests.
Exclusion criteria:
Patients with severe cardiac failure and cardiac arrhythmias were excluded and patients with rapid fall in BP and bradycardia (Neurally mediated syncope) were excluded.
Results:
Total 170 patients underwent tilt table testing. Orthostatic hypotension was seen within 3 minutes in seventy patients, fifty patients had delayed OH (BP fall after 3 minutes). There were twenty seven males and twenty three females in this group. Twenty nine of the 50 patients with delayed orthostatic hypotension, had symptoms during the tilt table procedure. Asymptomatic OH was more common in patients who developed OH after 10 minutes.
Conclusion:
This is a pilot study, first in India where we looked into the incidence of delayed orthostatic hypotension in patients undergoing tilt table testing in our autonomic lab. We found that fifty patients had delayed orthostatic hypotension which could have been missed on clinical evaluation. High clinical suspicion is needed to detect this disorder and tilt table testing should be done in suspicious cases since orthostatic hypotension is cause of high morbidity.
Keywords: Autonomic function tests, blood pressure, delayed orthostatic hypotension, morbidity
INTRODUCTION
Orthostatic hypotension (OH) is defined as a sustained decrease in systolic blood pressure (BP) of 20 mmHg or a decrease in diastolic BP of 10 mmHg within 3 min of standing compared with BP from the sitting or supine position or by head-up tilt-table testing.[1] When sustained BP drop is after 3 min of upright posture, it is called delayed OH.[2] Streeten and Andersonin 1992 have shown the significance of prolonged monitoring of BP to detect delayed fall in BP.[3] OH can be asymptomatic and detected only on testing.[4] The symptoms include dizziness, lightheadedness, blurred vision, weakness, fatigue, nausea, palpitations, headache syncope, dyspnea, chest pain, and neck and shoulder pain.[5,6] The cause of OH can be secondary to peripheral or central nervous system disorder, cardiac disease, drugs, anemia, and old age.
We conducted this retrospective study to detect the incidence of delayed OH in patients referred to our autonomic laboratory.
MATERIALS AND METHODS
The autonomic function tests done in our laboratory include tilt-table testing, valsalva maneuver, sympathetic skin response, and expiratory: inspiratory ratio for evaluation of autonomic nervous system. We reviewed the records of patients who had undergone autonomic function tests over the last 1 year (2014 June–2015 June). Patients with delayed OH, BP fall after 3 min of upright posture were included in the study.
To begin the test, the patient is monitored in the supine position 10 min to obtain baseline heart rate and BP measurements. The patient is instructed to remain as calm and relaxed as possible and to report any symptoms that may develop. The patient is then positioned in a head-up tilt position at a tilt angle 70°. BP was measured noninvasively at 1-min intervals with an automated cuff sphygmomanometer over the right brachial artery for 45 min. The onset and duration of falls in BP either systolic or diastolic or both were documented, and any associated symptoms were recorded.
Only patients with sustained falls (persistent BP fall throughout the recording) in BP were included in the study. Drugs causing OH was stopped 48 h before testing as per protocol followed in laboratory. We also looked into other autonomic function test abnormalities in patients with delayed OH.
Valsalva maneuver
The patient lies supine with head slightly elevated to about 30°. The patient strains for 15 s against 40 mmHg by blowing into a mouthpiece attached to a sphygmomanometer. Following cessation of the valsalva strain, the patient relaxes and breathes at a normal comfortable rate. The electrocardiogram is monitored during the strain and 30–45 s following its release. The ratio of minimum to maximum heart rate is calculated. The procedure is repeated three times after a brief rest and average is taken.
Expiratory: Inspiratory ratio
The patient is made supine with the head elevated to 30° and breathing deeply at a rate of 6/min, allowing 5 s each for inspiration and expiration. The maximum and minimum heart rate with each respiratory cycle is noted. The expiratory (E) to inspiratory (I) ratio or index is determined as the sum of 6 longest R-R intervals, divided by the sum of 6 shortest R-R intervals.
Sympathetic skin response
The recordings are obtained from the hand and feet. The active electrodes are placed on the palm or sole and reference over the dorsum of the respective body part after cleaning the skin, and the response is noted.
The beat—to-beat BP recording permits determination of role played by sympathetic nervous system. It detects the baroreflex sensitivity. It accurately reflects the arterial BP.
Inclusion criteria
Patients above age of 18 years referred for the evaluation of autonomic function tests.
Exclusion criteria
Patients with severe cardiac failure and cardiac arrhythmias were excluded, and patients with rapid fall in BP and bradycardia (neurally mediated syncope) were excluded from the study.
RESULTS
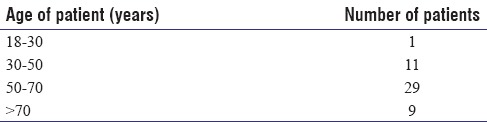
Totally, 170 patients underwent tilt-table testing. OH was seen within 3 min in 70 patients, 50 patients had delayed OH (BP fall after 3 min), and 50 patients had normal tilt-table test. Of 50 patients with delayed OH, BP fall was seen in 3–10 min in 20 patients, 23 patients had OH in 10–25 min, and 7 patients had OH in 25–45 min. Age-wise distribution of patients is shown in Table 1. There were 27 male and 23 female in this group. Twenty-nine of the 50 patients with delayed OH had symptoms during the tilt-table procedure. Sixteen patients had blurring of vision, while ten patients had giddiness or light headedness, and three patients had fatigue with sweating and cold periphery. Asymptomatic OH was more common in patients who developed OH after 10 min.
Table 1.
Age-wise distribution of patients with orthostatic hypotension
The mean systolic BP drop was 32 mm of Hg, and diastolic BP drop was 20 mm of Hg. Systolic BP mean ± standard deviation (SD) = 34.12 ± 11.05 and diastolic BP mean ± SD = 19.75 ± 2.60. Isolated systolic BP drop was more common. Both systolic BP and diastolic BP drop was seen in 21 patients with delayed OH. Isolated diastolic BP drop was not seen in any patients.
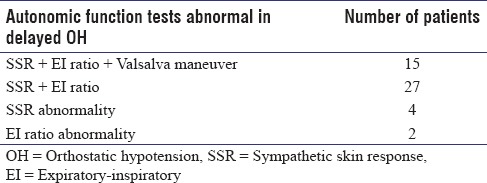
In 50 patients with delayed OH, valsalva maneuver was done only in 17 patients as majority of patients were not cooperative or did not do the procedure in proper technique. The abnormalities in autonomic function tests are given in Table 2. Two patients had delayed OH only with other autonomic function tests being normal.
Table 2.
Autonomic function tests abnormal in delayed OH
Neurological disorders seen in these patients where diabetic peripheral neuropathy in 20 patients, 12 patients with atypical PD, 11 patients with typical PD, 5 patients with neuropathy due to causes other than diabetic (liver disease and vasculitic neuropathy), and 2 patients had no definite neurological diagnosis.
DISCUSSION
OH (postural) is a frequent cause of syncope and may contribute to morbidity, disability, and even death.[7] The Classical definition of OH is BP fall at 3 min. This is usually done as bedside evaluation. An entity of delayed OH exists where the BP fall is after 3 min of upright posture. This can be under diagnosed if BP monitoring is not done for more than 3 min in upright posture. Here, we were looking into the incidence of delayed OH in patients who were evaluated in our laboratory.
Of 170 patients who underwent tilt-table testing, 120 patients showed OH. Seventy patients showed OH in 3 min of testing while fifty patients showed OH after 3 min confirming the diagnosis of delayed OH.[2] We have divided delayed OH into three categories based on time at which BP fall was seen, 3–10 min, 10–25 min, and 25–45 min. There were 20 patients, 23 patients, and 7 patients, respectively, in these groups.
Gibbons and Freeman[3] reported that among 108 patients with OH on tilt-table testing, 46% had OH occurring within 3 min of tilt-table testing, 15% occurring between 3 and 10 min, and 39% occurring after 10 min. In our study, delayed OH was 42% and incidence of OH after 10 min was 66%. This shows the incidence of OH after 10 min is high; hence, patients should have tilt-table testing done to detect this phenomenon.
When we stand up, the blood pools up in venous system below the diaphragm. This fluid shift produces a decrease in venous return, ventricular filling, cardiac output, and BP. This gravity-induced drop in BP, detected by arterial baroreceptors in the aortic arch and carotid sinus, triggers a compensatory reflex tachycardia and vasoconstriction that restores normotension in the upright posture.[8] OH is the result of baroreflex failure (autonomic failure), end organ dysfunction, or volume depletion.
The symptom associated with delayed OH was fatigue on exertion, unsteadiness of gait, neck pain on prolonged standing, and recurrent falls.[6] The symptoms are due to hypoperfusion secondary to fall in BP in upright posture. Visual blurring is due to retinal or occipital-lobe ischemia,[6] and neck pain which is seen in OH is seen in suboccipital, posterior cervical, and shoulder region (called the coat-hanger headache), is due to ischemia in the trapezius and neck muscles. Patients may report orthostatic dyspnea due to ventilation–perfusion mismatch or angina due to impaired myocardial perfusion even in patients with normal coronary arteries.[9] One or more of symptoms may be the presenting symptom of OH.
We have looked into abnormality in other autonomic function tests in our series and found that in patients with delayed OH, other autonomic function tests abnormality was found in 48 patients. Hence, delayed OH should be considered as sign of autonomic nervous system involvement.
Causes of neurogenic OH can be central and peripheral autonomic nervous system disorders. The primary autonomic degenerative disorders are multiple-system atrophy (the Shy–Drager syndrome), Parkinson's disease, dementia with lewy bodies, and pure autonomic failure.[7,10] Association of OH with small-fiber peripheral neuropathy, due to diabetes, amyloidosis, immune-mediated neuropathies, hereditary sensory and autonomic neuropathies, and inflammatory neuropathies has been reported previously.[7,11] Nonneurological causes can be dehydration, anemia, drugs, cardiovascular, and endocrine causes.[11,12] The most common neurological disorder seen in association with delayed OH in our series where diabetic neuropathy followed by atypical Parkinson's disease. Two patients had delayed OH without neurological disorders, and all these patients were above 65-year-old; this has been seen in the previous reports were delayed OH was seen in elderly without other causes.[12]
Tilt-table testing is useful in the assessment of elderly patients with recurrent, unexplained falls, convulsive syncope, OH,[13] and postural orthostatic tachycardia syndrome. The tilt-table testing is useful in diagnosing OH even if clinical BP monitoring within 3 min is normal[14] and should be done in patients with suspicion of OH even if 3 min clinical BP monitoring is normal. We used the New castle protocol except for isoproterenol infusion in our study. Our study shows that the incidence of delayed OH is high and can be missed if tilt-table testing is not done. A 10 years follow-up study by Gibbons and Freeman have shown that delayed OH frequently progress to OH with a high associated mortality.[15]
CONCLUSION
This is a pilot study first in India, where we looked into the incidence of delayed OH in patients undergoing tilt-table testing in our autonomic laboratory. We found that fifty patients had delayed OH which could have been missed on clinical evaluation. The symptoms can be varying but high clinical suspicion is needed to detect this disorder, and tilt-table testing should be done in suspicious cases since OH is cause of morbidity.
Limitation
We have evaluated only BP in this study, the relation of heart rate and BP variation was not looked into. The response to treatment and follow-up were not analyzed. Ongoing study is being done in our laboratory looking into all these factors and comparing the variables between OH and delayed OH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology. 1996;46:1470. doi: 10.1212/wnl.46.5.1470. [DOI] [PubMed] [Google Scholar]
- 2.Streeten DH, Anderson GH., Jr Delayed orthostatic intolerance. Arch Intern Med. 1992;152:1066–72. [PubMed] [Google Scholar]
- 3.Gibbons CH, Freeman R. Delayed orthostatic hypotension: A frequent cause of orthostatic intolerance. Neurology. 2006;67:28–32. doi: 10.1212/01.wnl.0000223828.28215.0b. [DOI] [PubMed] [Google Scholar]
- 4.Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension. 1992;19(6 Pt 1):508–19. doi: 10.1161/01.hyp.19.6.508. [DOI] [PubMed] [Google Scholar]
- 5.Lahrmann H, Cortelli P, Hilz M, Mathias CJ, Struhal W, Tassinari M. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur J Neurol. 2006;13:930–6. doi: 10.1111/j.1468-1331.2006.01512.x. [DOI] [PubMed] [Google Scholar]
- 6.Freeman R. Clinical practice. Neurogenic orthostatic hypotension. N Engl J Med. 2008;358:615–24. doi: 10.1056/NEJMcp074189. [DOI] [PubMed] [Google Scholar]
- 7.Mathias CJ. Autonomic diseases: Clinical features and laboratory evaluation. J Neurol Neurosurg Psychiatry. 2003;74(Suppl 3):iii31–41. doi: 10.1136/jnnp.74.suppl_3.iii31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sjostrand T. The regulation of the blood distribution in man. Acta Physiol Scand. 1952;26:312–27. doi: 10.1111/j.1748-1716.1952.tb00912.x. [DOI] [PubMed] [Google Scholar]
- 9.Gibbons CH, Freeman R. Orthostatic dyspnea: A neglected symptom of orthostatic hypotension. Clin Auton Res. 2005;15:40–4. doi: 10.1007/s10286-005-0227-1. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann H, Biaggioni I. Autonomic failure in neurodegenerative disorders. Semin Neurol. 2003;23:351–63. doi: 10.1055/s-2004-817719. [DOI] [PubMed] [Google Scholar]
- 11.Bradley JG, Davis KA. Orthostatic hypotension. Am Fam Physician. 2003;68:2393–8. [PubMed] [Google Scholar]
- 12.Lanier JB, Mote MB, Clay EC. Evaluation and management of orthostatic hypotension. Am Fam Physician. 2011;84:527–36. [PubMed] [Google Scholar]
- 13.Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Neurol Sci. 1996;144:218–9. [PubMed] [Google Scholar]
- 14.Faraji F, Kinsella LJ, Rutledge JC, Mikulec AA. The comparative usefulness of orthostatic testing and tilt table testing in the evaluation of autonomic-associated dizziness. Otol Neurotol. 2011;32:654–9. doi: 10.1097/MAO.0b013e3182117769. [DOI] [PubMed] [Google Scholar]
- 15.Gibbons CH, Freeman R. Clinical implications of delayed orthostatic hypotension: A 10-year follow-up study. Neurology. 2015;85:1362–7. doi: 10.1212/WNL.0000000000002030. [DOI] [PMC free article] [PubMed] [Google Scholar]


