Sir,
Dengue is a mosquito-borne viral disease caused by dengue virus that belongs to the genus Flavivirus, transmitted by two mosquito vectors, namely, Aedes aegypti and Aedes albopictus.[1] Dengue with or without warning signs, and severe dengue are the categories of disease under the WHO recent classification.[1] This recent clinical case definition had stated to consider all patients with neurological manifestations under severe dengue. Here, we describe the clinical presentation, neuroimaging findings, and management of a child with dengue encephalopathy manifesting with seizures and stroke. Neuroimaging had shown pontine bleed and watershed infarcts in this child.
A 29-month-old child was brought with high-grade fever of 6-day duration and multiple episodes of vomiting of 3-day duration. He had altered level of consciousness from the 5th day of illness and had developed multiple episodes of right focal motor seizures with secondary generalization without regaining consciousness. Seizures were controlled after the administration of benzodiazepines and phenytoin. Altered level of consciousness had persisted, and he was observed to have paucity of right-sided limb movements. There was an outbreak of dengue epidemic in their geographic area.
Length and weight of the child were <3rd centile for age. Temperature of 101°F, heart rate of 120/min, blood pressure of 95/41 mmHg, and respiratory rate of 38/min were documented on admission. Capillary refill time and oxygen saturation were normal. Glasgow coma score was 9/15. Tone was decreased in all four limbs and right hemiparesis was observed. Deep tendon reflexes were exaggerated and bilateral plantar responses were extensor.
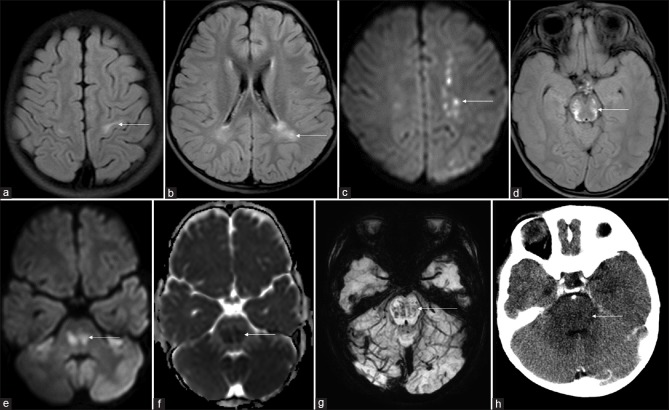
Clinical syndrome and laboratory parameters of this child [summarized in Table 1] were highly suggestive of severe dengue. Magnetic resonance imaging of the brain [Figure 1a–g] describes the radiological findings observed in our patient. Computerized tomography of the brain [Figure 1h] showed hypodensity and swelling of the pons.
Table 1.
Summary of laboratory parameters
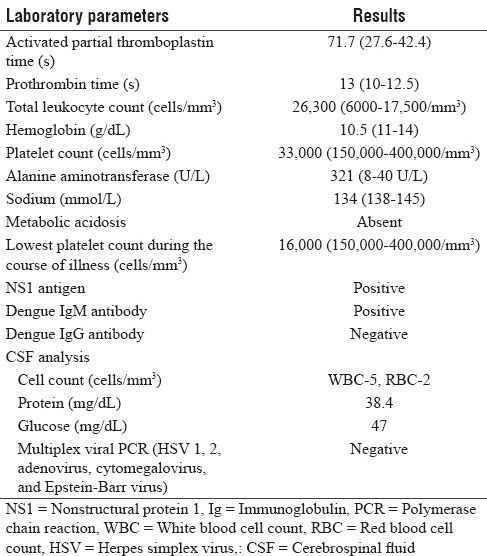
Figure 1.
Magnetic resonance imaging fluid-attenuated inversion recovery axial images (a and b) bilateral white matter hyperintensities in the precentral gyrus and posterior periventricular region. Diffusion-weighted image (c) multiple foci of restriction in the left centrum semiovale. Fluid-attenuated inversion recovery axial image (d) symmetric midbrain hyperintensity. Diffusion-weighted image and apparent diffusion coefficient image at pontine level (e and f) restricted diffusion. Susceptibility-weighted image (g) hypointense foci in pons suggestive of bleed. Computerized tomography brain (h) hypodensity and swelling of the pons
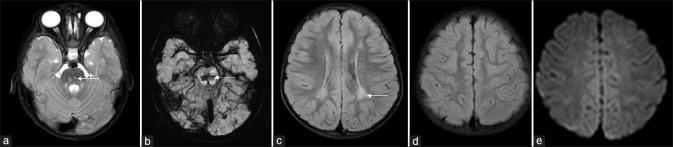
The child was managed with intravenous fluids as per the WHO protocol and maintenance doses of anticonvulsants. During the hospital stay, blood culture had grown nonfermenting Gram-negative Bacillus which was treated appropriately. His sensorium had gradually improved over next 2 weeks. At discharge, central hypotonia persisted but right hemiparesis had improved. Bilateral alternate convergent squint was observed. Follow-up assessment after 3 months had shown an alert and active child with normal speech and language. Bilateral alternate convergent squint persisted. Follow-up MRI brain findings are depicted [Figure 2a–e].
Figure 2.
Follow-up magnetic resonance imaging T2 axial image (a) small persistent hyperintense foci in the pons. Susceptibility-weighted image (b) persisting hypointensity suggestive of hemosiderin deposits. Minimal persistent posterior periventricular hyperintensity is seen on fluid-attenuated inversion recovery axial image (c). Fluid-attenuated inversion recovery axial image and diffusion-weighted image at a higher level (d and e) complete resolution of findings
“Dengue central nervous system (CNS) involvement refers to the presence of any one of the symptoms such as impaired consciousness, neck stiffness, focal neurological signs, or seizures with laboratory evidence.”[2] Neurological complications reported in association with dengue are Guillain–Barre syndrome, rhabdomyolysis, and neuro-ophthalmic.[2] Criteria for severe dengue include plasma leakage resulting in shock, fluid accumulation, clinical evidence of severe bleeding or severe organ involvement such as elevated liver enzymes, CNS involvement, and heart or other organ involvement.[1]
Diagnosis of dengue encephalopathy in our case was based on the presence of clinical evidence of CNS involvement such as altered consciousness, seizures, focal neurological deficit, and laboratory evidence such as positivity for nonstructural protein 1 antigen and presence of dengue immunoglobulin (Ig) M antibody. Our patient also had documentation of elevated liver enzymes, intracranial bleed, and normal cerebrospinal fluid findings. Postulated mechanisms to explain the various CNS presentations in dengue are direct virus invasion, metabolic disturbances, capillary leak, shock, and immune mediated.[3]
Incidence of stroke in dengue has been reported as 0.26%, and reports of both ischemic stroke and hemorrhagic stroke exist.[4,5] Imaging findings described in patients with dengue are hyperintensity involving thalami, corpus callosum, centrum semiovale, cortex, basal ganglia, cerebral edema, hypoxic brain injury, focal lesions, meningeal enhancement, multiple hemorrhagic foci, watershed infarcts, cerebellar haemorrhage, and obstructive hydrocephalus.[5,6,7,8] Pontine hemorrhage, subdural hematoma, subarachnoid bleed, and hemorrhage into pituitary adenoma have also been reported.[3,9,10,11]
Stroke in children is extremely rare. Watershed infarcts and pontine hemorrhage could possibly explain the neurological deficit in our case. This is the earliest reported age of presentation of dengue with stroke with a near complete neurological recovery. Ischemic stroke in dengue has been previously reported in elderly adults.[4,12,13] Ischemic stroke due to dengue-associated vasculopathy has also been reported in an 8-year-old child.[14]
Treatment in dengue encephalopathy is usually supportive. Intravenous methylprednisolone or immunoglobulins may be considered for immune-mediated encephalomyelitis and dengue-associated vasculopathy. Our patient was managed conservatively with adequate hydration, nutrition, anticonvulsants, and neurorehabilitation.
In conclusion, dengue-associated stroke is extremely rare in children. Stroke in dengue patients may be hemorrhagic or ischemic. Dengue should be enlisted as a cause of stroke in children from tropical countries with febrile encephalopathy and focal neurological deficits. Treatment is supportive and prognosis may be variable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.WHO. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 2.Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12:906–19. doi: 10.1016/S1474-4422(13)70150-9. [DOI] [PubMed] [Google Scholar]
- 3.de Souza LJ, Martins AL, Paravidini PC, Nogueira RM, Gicovate Neto C, Bastos DA, et al. Hemorrhagic encephalopathy in dengue shock syndrome: A case report. Braz J Infect Dis. 2005;9:257–61. doi: 10.1590/s1413-86702005000300009. [DOI] [PubMed] [Google Scholar]
- 4.Liou LM, Lan SH, Lai CL. Dengue fever with ischemic stroke: A case report. Neurologist. 2008;14:40–2. doi: 10.1097/NRL.0b013e3180d0a391. [DOI] [PubMed] [Google Scholar]
- 5.Mathew S, Pandian JD. Stroke in patients with dengue. J Stroke Cerebrovasc Dis. 2010;19:253–6. doi: 10.1016/j.jstrokecerebrovasdis.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Bhoi SK, Naik S, Kumar S, Phadke RV, Kalita J, Misra UK. Cranial imaging findings in dengue virus infection. J Neurol Sci. 2014;342:36–41. doi: 10.1016/j.jns.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Koshy JM, Joseph DM, John M, Mani A, Malhotra N, Abraham GM, et al. Spectrum of neurological manifestations in dengue virus infection in Northwest India. Trop Doct. 2012;42:191–4. doi: 10.1258/td.2012.120286. [DOI] [PubMed] [Google Scholar]
- 8.Cam BV, Fonsmark L, Hue NB, Phuong NT, Poulsen A, Heegaard ED. Prospective case-control study of encephalopathy in children with dengue hemorrhagic fever. Am J Trop Med Hyg. 2001;65:848–51. doi: 10.4269/ajtmh.2001.65.848. [DOI] [PubMed] [Google Scholar]
- 9.Dey AB, Chaudhury D, Mohapatra AK, Nagarkar KM, Malhotra OP. Fever, mucocutaneous haemorrhage, and severe headache during an epidemic of haemorrhagic fever. Postgrad Med J. 1998;74:433–5. doi: 10.1136/pgmj.74.873.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar V, Kataria R, Mehta VS. Dengue hemorrhagic fever: A rare cause of pituitary tumor hemorrhage and reversible vision loss. Indian J Ophthalmol. 2011;59:311–2. doi: 10.4103/0301-4738.82002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patey O, Ollivaud L, Breuil J, Lafaix C. Unusual neurologic manifestations occurring during dengue fever infection. Am J Trop Med Hyg. 1993;48:793–802. doi: 10.4269/ajtmh.1993.48.793. [DOI] [PubMed] [Google Scholar]
- 12.Verma R, Sahu R, Singh AS, Atam V. Dengue infection presenting as ischemic stroke: An uncommon neurological manifestation. Neurol India. 2013;61:317–8. doi: 10.4103/0028-3886.115083. [DOI] [PubMed] [Google Scholar]
- 13.Seet RC, Lim EC. Dysarthria-clumsy hand syndrome associated with dengue type-2 infection. J Neurol. 2007;254:1129–30. doi: 10.1007/s00415-006-0458-7. [DOI] [PubMed] [Google Scholar]
- 14.Nanda SK, Jayalakshmi S, Mohandas S. Pediatric ischemic stroke due to dengue vasculitis. Pediatr Neurol. 2014;51:570–2. doi: 10.1016/j.pediatrneurol.2014.06.019. [DOI] [PubMed] [Google Scholar]