Abstract
Objective To compare the effects of a minimal intervention strategy aimed at assessment and modification of psychosocial prognostic factors and usual care for treatment of (sub)acute low back pain in general practice.
Design Cluster randomised clinical trial.
Setting 60 general practitioners in 41 general practices.
Participants 314 patients with non-specific low back pain of less than 12 weeks' duration, recruited by their general practitioner.
Interventions In the minimal intervention strategy group the general practitioner explored the presence of psychosocial prognostic factors, discussed these factors, set specific goals for reactivation, and provided an educational booklet. The consultation took about 20 minutes. Usual care was not standardised.
Main outcome measures Functional disability (Roland-Morris disability questionnaire), perceived recovery, and sick leave because of low back pain assessed at baseline and after 6, 13, 26, and 52 weeks.
Results The dropout rate was 8% in the minimal intervention strategy group and 9% in the usual care group. Multilevel analyses showed no significant differences between the groups on any outcome measure during 12 months of follow-up in the whole group or in relevant subgroups (patients with high scores on psychosocial measures at baseline or a history of frequent or prolonged low back pain).
Conclusion This study provides no evidence that (Dutch) general practitioners should adopt our new treatment strategy aimed at psychosocial prognostic factors in patients with (sub)acute low back pain. Further research should examine why our new strategy was not more effective than usual care.
Introduction
Non-specific low back pain is common; the 12 month prevalence in the general population has been estimated at 44%.1 Although many episodes of acute low back pain resolve rapidly,2 around a third result in persistent or recurrent disabling symptoms.3 Persistent disabling symptoms may be prevented by early identification and modification of psychosocial factors that have been shown to play an important role in the transition from acute to chronic low back pain.4
General practice may be an appropriate setting for an early intervention. Low back pain is common in general practice, ranking among the top five most common reasons for consultation in the Netherlands.5 The Dutch guideline on low back pain for general practitioners, however, lacks explicit guidance for assessing psychosocial factors.6 We therefore developed a minimal intervention strategy aimed at assessment and modification of psychosocial prognostic factors in patients with (sub)acute low back pain, which can be carried out by general practitioners.
Previous studies have evaluated booklets with biopsychosocial information provided by a general practitioner, but these did not have beneficial effects on disability or pain.7-9 Only one of these studies reported a significant effect in a subgroup of patients with initially strong fear-avoidance beliefs.8 We are not aware of (other) studies in which psychosocial interventions for low back pain were delivered by a general practitioner.
To compare the effects of a minimal intervention strategy with the effects of usual care, we did a cluster randomised trial. We hypothesised that patients in the minimal intervention strategy group would improve more on functional disability, perceived recovery, and sick leave due to low back pain than would patients receiving usual care. Assuming that patients with high scores on psychosocial measures or patients with prolonged or frequent low back pain would especially benefit from the minimal intervention strategy, we studied effect modification by baseline levels of fear-avoidance beliefs, catastrophising thoughts or distress, and history of low back pain (pre-planned subgroup analyses).
Methods
Randomisation and training sessions
Randomisation took place at the level of the general practice in blocks of four practices, according to a random numbers table prepared before recruitment of general practitioners. General practitioners were informed about their allocation after they had given final consent to participation. Twenty practices (28 general practitioners) were randomised to the minimal intervention strategy group and 21 practices (32 general practitioners) to the usual care group.
The general practitioners randomised to the minimal intervention strategy group received two training sessions of 2.5 hours each, which were given by a general practitioner (HEvdH) with extensive expertise in development of and training in psychosocial interventions. The training consisted of theory, role playing, and feedback on the practised skills. In addition, we provided a treatment manual.
Participants
We invited general practitioners to participate through a leaflet and by telephone. A researcher (PJ) visited general practitioners who showed interest, informed them about the study's aim and procedures, and invited them to participate for a period of eight months. We asked participating general practitioners to select 10 consecutive patients who consulted them for low back pain. Inclusion criteria were age 18-65 years, non-specific low back pain of less than 12 weeks' duration or an exacerbation of persisting low back pain, and sufficient knowledge of the Dutch language. Exclusion criteria were low back pain caused by specific pathological conditions, low back pain currently treated by another healthcare professional, and pregnancy. Patients were kept unaware that two different interventions were studied.
Interventions
The minimal intervention strategy was aimed at identification and discussion of psychosocial prognostic factors. Main sources used during its development were a document on the assessment and management of angry and distressed patients with low back pain,10 a systematic review of psychological factors as predictors of chronicity or disability,4 the New Zealand guidelines for low back pain,11 and a document on education and counselling for patients with irritable bowel syndrome.12 When a patient showed interest in participation during the first consultation, the general practitioner did not immediately start the minimal intervention strategy but made an appointment for a second consultation. In between, a research assistant visited the patient to obtain informed consent and for baseline assessment. The actual minimal intervention strategy consultation took place within about five days, lasted about 20 minutes, and consisted of three phases: exploration, information, and self care. The box summarises the content of the three phases. We explicitly asked general practitioners in the minimal intervention strategy group not to refer to a physiotherapist in the first six weeks.
In the usual care group, the general practitioner provided care as usual and subsequently asked eligible patients to participate. Within about three days a research assistant visited the patient for informed consent and baseline assessment. We did not standardise the content and number of usual care consultations and assumed that general practitioners would follow the guideline for low back pain of the Dutch College of General Practitioners,6 the content of which is summarised in the box.
Outcome and psychosocial measures
We assessed outcomes by patient completed questionnaires at baseline and after 6, 13, 26, and 52 weeks. Primary outcome measures were functional disability, assessed by the 24 item Roland-Morris disability questionnaire (0-24)15; perceived recovery, scored by the patient on a seven point Likert-type scale (very much, much, slightly improved; no change; slightly, much, very much worse)16 (no recovery was defined as slightly improved; no change; slightly, much, very much worse); and sick leave because of low back pain since the previous questionnaire (yes/no), which was assessed only in patients who had a paid job at baseline. Secondary outcome measures were severity of pain during the day (0-10)17; severity of the main complaint (0-10)18; and perceived general health (1-5), measured using the first question of the subscale “general health perceptions” of the short form health survey (SF-36).19
We assessed the following psychosocial measures at baseline: fear-avoidance beliefs, measured using the four item physical activity subscale of the fear-avoidance beliefs questionnaire (0-24)20; catastrophising thoughts, measured with the six item subscale of the coping strategies questionnaire (0-36)21; and distress, measured by the 16 item subscale of the four dimensional symptom questionnaire (0-32).22
Power calculation
We based the calculation of study size on the ability to detect a standardised mean difference of 0.4 on the Roland-Morris disability questionnaire, which equals about 2.5 points (SD 6). A score of 2-3 points has been cited as the cut-off point for a minimal clinically important change.23 To detect this difference with a two sided significance level (α) of 0.05 and a power (1 - β) of 0.90, we needed a sample size of 260 patients. As we used four follow-up assessments, the sample size could be adjusted to 164 (estimated within patient correlation = 0.5). Next, given the clustered design, the required sample size was adjusted to 230 (intracluster correlation coefficient = 0.1024; estimated cluster size = five patients per general practitioner). Finally, taking into account a dropout rate of 20%, we estimated the required sample size at 290 patients.
Content of interventions
Minimal intervention strategy
Exploration phase
The general practitioner explored the presence of psychosocial prognostic factors by asking standardised questions* that could be rephrased to fit the style of communication of the doctor and patient. The general practitioner started by asking a main question, which was usually an open question. When the patient's response gave the impression that this factor could be an obstacle to recovery, the doctor explored the problem further with additional questions. When the factor did not seem to be an obstacle to recovery, the doctor continued with the main question of the next factor. The following psychosocial prognostic factors were explored:
Patient's own ideas on the cause of the low back pain (for example, the idea that it is due to a defect of the spinal column)
Fear-avoidance beliefs (such as the idea that pain is harmful)
Worries about the pain (such as tenseness)
Catastrophising thoughts (for example, feeling that the pain will never stop)
Pain behaviour (such as avoidance behaviour)
Reactions from family or friends to the low back pain (for example, partner who ignores pain)
Physical and psychosocial factors at work (such as conflict at work)
Information phase
The general practitioner did not start the information phase before all the questions of the exploration phase had been asked. In the information phase the general practitioner provided general information on the cause, course, and (im)possibilities of treatment of low back pain and included the patient's cognitions, emotions, and behaviour. This should guarantee that the patient would understand the information better and would receive more reassurance than if told “you don't need to worry.” Specific attention was given to psychosocial factors identified in the exploration phase, and vicious circles between cognitions, emotions, behaviour, and pain were explained.
Self care phase
The general practitioner and patient set specific goals on resuming activities or work and discussed time contingent use of analgesic drugs, and the doctor gave the patient a booklet based on the Back Book.13,14 The content of the booklet reinforced that of the informational phase. If the general practitioner had identified many obstacles to recovery and suspected an increased risk of development of chronic complaints, he or she made an appointment for a follow-up visit.
Usual care
The guideline for low back pain of the Dutch College of General Practitioners advises a wait and see policy for acute low back pain, with analgesics and gradual uptake of activities, and provides general recommendations on reactivation and home exercises. For subacute low back pain (> 6 weeks), the guideline advises referral for exercise therapy, physiotherapy, or manual therapy in the case of persistent functional disability. Explicit guidance on psychosocial factors is lacking.
*These questions were adapted from Main and Watson (2001).10
Statistical analyses
Firstly, we studied baseline similarity. Secondly, we compared baseline characteristics of dropouts and completers by using logistic regression analysis. Thirdly, we used linear and logistic multilevel analyses to investigate the intervention effect (that is, the differences in outcome between the minimal intervention strategy and usual care over the total follow-up period), adjusting for possible clustering of observations (MlwiN version 1.1). The included levels were repeated measures (that is, time), patient, general practitioner, and practice. Although some scores at follow-up seemed to be skewed, parametric analyses were allowed as the analyses adjusted for baseline values yielded “change” scores that were normally distributed. We based analyses on intention to treat and set the level of significance at P < 0.05. Finally, we did three subgroup analyses for patients with elevated psychosocial scores at baseline (fear-avoidance beliefs score > 15,25 median split; coping strategies questionnaire score > 11, median split; four dimensional symptom score > 10,22 clinically validated for a general practice population) and one in patients with subacute or recurrent low back pain (duration ≥6 weeks or ≥3 episodes in the past year, current episode included).
Results
Participants
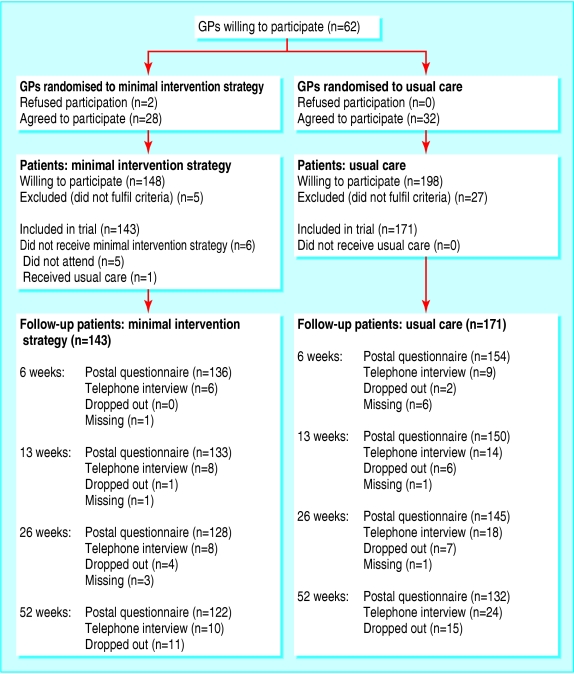
Between September 2001 and April 2003, 346 of the 405 patients asked by their general practitioner were willing to participate. We excluded 32 patients (figure). The main reasons for exclusion were “no low back pain any more” (n = 14), “too old” (n = 8), and “already treated for their low back pain by another healthcare professional” (n = 7). Of the 314 patients enrolled, three were enrolled incorrectly—two were too old and one had already been treated by another healthcare professional. Six patients did not receive the minimal intervention strategy consultation. During follow-up, 11 (8%) patients in the minimal intervention strategy group and 15 (9%) patients in the usual care group withdrew from the study. Reasons were “no time and no complaints any more” (minimal intervention strategy, n = 1; usual care, n = 4), “burden too high due to psychological problems” (usual care, n = 3), or unknown (minimal intervention strategy, n = 10; usual care, n = 8).
Figure 1.
Flow of general practitioners and patients through the trial. GP=general practitioner; dropped out=cumulative number of patients who did not return all following questionnaires; missing=number of patients who did not return that specific questionnaire
Table 1 shows that baseline characteristics of general practitioners and patients were largely similar for the two groups. We therefore adjusted our analyses only for baseline values of outcome measures and not for other prognostic variables. Dropouts were younger, less educated, and more distressed at baseline than completers.
Table 1.
Baseline characteristics of general practitioners and patients. Values are numbers (percentages) unless stated otherwise
| Characteristic | Minimal intervention strategy | Usual care |
|---|---|---|
| General practitioners | (n=28) | (n=32) |
| Mean (SD) age (years)* | 43.0 (7.2) | 45.7 (7.4) |
| Women | 6 (21) | 12 (38) |
| No of included patients/general practitioner: | ||
| 0 | 1 (4) | 5 (16) |
| 1-5 | 17 (61) | 14 (44) |
| >5 | 10 (36) | 13 (41) |
| Patients | (n=143) | (n=171) |
| Demographic characteristics: | ||
| Mean (SD) age (years) | 43.4 (11.1) | 42.0 (12.0) |
| Women | 68 (48) | 81 (47) |
| Dutch nationality | 139 (97) | 167 (98) |
| Public health insurance | 101 (71) | 116 (68) |
| Educational level and work status: | ||
| Education level* | ||
| primary or below | 50 (35) | 56 (33) |
| secondary | 66 (46) | 89 (53) |
| college, university | 27 (19) | 24 (14) |
| Paid job | 117 (82) | 139 (81) |
| Disability payment because of LBP | 3 (2) | 3 (2) |
| Characteristics of LBP: | ||
| Median (interquartile range) duration of current episode (days) | 11 (5-21) | 14 (7-21) |
| Frequency of LBP episodes in previous year: | ||
| 1-2 episodes | 83 (58) | 104 (61) |
| ≥3 episodes | 28 (20) | 32 (19) |
| exacerbation of persisting LBP | 32 (22) | 35 (21) |
| Pain radiating below knee* | 18 (13) | 25 (15) |
| Primary measures: | ||
| Mean (SD) functional disability score (RDQ, 0-24) | 11.7 (5.4) | 12.2 (5.0) |
| Sick leave because of LBP* (among the working population) | 40 (35) | 57 (41) |
| Secondary measures: | ||
| Mean (SD) pain severity during day (0-10)† | 4.9 (2.0) | 4.8 (2.0) |
| Mean (SD) severity of main complaint (0-10)* | 7.0 (1.9) | 6.8 (2.0) |
| Mean (SD) perceived general health (SF-36, 1-5)* | 2.7 (0.8) | 2.8 (0.8) |
| Psychosocial measures: | ||
| Mean (SD) fear-avoidance beliefs (FABQ, 0-24) | 14.3 (5.6) | 15.3 (5.2) |
| Mean (SD) catastrophising thoughts (CSQ, 0-36) | 10.3 (6.6) | 11.2 (6.9) |
| Mean (SD) distress (4DSQ, 0-32)† | 8.3 (7.0) | 9.5 (7.3) |
LBP=low back pain.
RDQ= Roland-Morris disability questionnaire; SF-36=short form 36; FABQ=fear-avoidance beliefs questionnaire; CSQ=coping strategies questionnaire; 4DSQ=four dimensional symptom questionnaire (higher scores mean more functional disability, worse health, more fear-avoidance, more catastrophising, or more distress).
n=2 missing.
n=1 missing.
Effect of intervention
Multilevel analyses showed that all analyses needed to be adjusted for the correlation of repeated measures within patients, but not for clustering of effects within general practitioners or practices, except for functional disability (Roland-Morris disability questionnaire). Tables 2 and 3 present the scores for primary and secondary outcomes and differences in the course of these outcomes estimated with multilevel analysis.
Table 2.
Primary outcomes at baseline and follow-up and difference over time between groups
|
Median (interquartile range) or proportion (%)
|
|||
|---|---|---|---|
| Measurement | Minimal intervention strategy | Usual care | Mean difference*or odds ratio†(95% CI) |
|
Functional disability (RDQ, 0-24)
|
|
|
|
| Baseline
|
13 (7-16) (n=143)
|
13 (8-16) (n=171)
|
Mean difference 0.25 (−0.77 to 1.28) |
| 6 weeks
|
4 (1-9) (n=142)
|
4 (1-10) (n=163)
|
|
| 13 weeks
|
2 (0-6) (n=140)
|
2 (0-5) (n=163)
|
|
| 26 weeks
|
1 (0-4) (n=134)
|
1 (0-3) (n=163)
|
|
| 52 weeks | 1 (0-4) (n=132) | 1 (0-4) (n=154) | |
| No recovery‡ | |||
| Baseline
|
-
|
-
|
Odds ratio 1.16 (0.63 to 2.17) |
| 6 weeks
|
56/142 (39)
|
60/163 (38)
|
|
| 13 weeks
|
47/141 (33)
|
53/164 (32)
|
|
| 26 weeks
|
44/136 (32)
|
50/163 (31)
|
|
| 52 weeks | 42/132 (32) | 43/156 (28) | |
|
Sick leave because of low back pain§
|
|
|
|
| Baseline
|
40/115 (35)
|
57/139 (41)
|
Odds ratio 0.69 (0.43 to 1.13) |
| 6 weeks
|
19/116 (16)
|
26/132 (20)
|
|
| 13 weeks
|
5/114 (4)
|
17/134 (13)
|
|
| 26 weeks
|
3/110 (3)
|
11/134 (8)
|
|
| 52 weeks | 8/107 (8) | 9/128 (7) | |
RDQ=Roland-Morris disability questionnaire (higher scores mean more functional disability).
Minimum intervention strategy (MIS) minus usual care (UC), adjusted for baseline values and estimated with multilevel analysis. Mean difference >0 means that over 12 months MIS group had higher mean score on functional disability than UC group.
MIS versus UC, estimated with multilevel analysis. For sick leave, adjusted for baseline values. An odds ratio >1 means that over 12 months more patients in MIS group than in the UC group reported sick leave or no recovery.
Yes=slightly improved + no change + slightly worse + much worse + very much worse.
Proportion of patients on sick leave because of low back pain among working population.
Table 3.
Secondary outcomes at baseline and follow-up and mean difference over time between groups
|
Minimum intervention strategy
|
Usual care
|
||||
|---|---|---|---|---|---|
| Measurement | Median (IQR) or mean (SD) | No | Median (IQR) or mean (SD) | No | Mean difference*(95% CI) |
| Pain severity during day (0-10) | |||||
| Baseline
|
5 (3-7)
|
142
|
5 (3-6)
|
171
|
0.015 (−0.41 to 0.44) |
| 6 weeks
|
2 (0-4)
|
141
|
2 (0-4)
|
162
|
|
| 13 weeks
|
0 (0-3)
|
140
|
1 (0-3)
|
164
|
|
| 26 weeks
|
0 (0-3)
|
135
|
0 (0-2)
|
163
|
|
| 52 weeks | 0 (0-3) | 132 | 0 (0-2) | 155 | |
| Severity of main complaint (0-10) | |||||
| Baseline
|
7 (5-8)
|
142
|
7 (5-8)
|
170
|
0.021 (−0.45 to 0.49) |
| 6 weeks
|
2 (0-5)
|
142
|
2 (0.5-4)
|
161
|
|
| 13 weeks
|
1 (0-3.25)
|
138
|
1 (0-3)
|
164
|
|
| 26 weeks
|
1 (0-4)
|
135
|
1 (0-3)
|
160
|
|
| 52 weeks | 1 (0-3) | 132 | 1 (0-3) | 153 | |
| Perceived general health (SF-36, 1-5) | |||||
| Baseline
|
2.7 (0.8)
|
143
|
2.8 (0.8)
|
169
|
0.056 (−0.07 to 0.17) |
| 6 weeks
|
-
|
|
-
|
|
|
| 13 weeks
|
2.6 (0.8)
|
136
|
2.6 (0.8)
|
154
|
|
| 26 weeks
|
2.6 (0.7)
|
132
|
2.6 (0.8)
|
154
|
|
| 52 weeks | 2.7 (0.9) | 131 | 2.7 (0.8) | 153 | |
IQR=interquartile range; SF-36=short form 36 (higher scores mean worse health; not assessed after six weeks' follow-up).
Minimal intervention strategy (MIS) minus usual care (UC), adjusted for baseline values and estimated with multilevel analysis. Mean difference >0 means that over 12 months MIS group had higher mean score on that outcome measure than UC group (that is, more pain, greater severity of main complaint, and worse health).
Over 12 months' follow-up, the adjusted mean difference on functional disability (Roland-Morris disability questionnaire) was 0.25 points (95% confidence interval -0.77 to 1.28), slightly favouring usual care, and the odds ratio for sick leave due to low back pain was 0.69 (0.43 to 1.13), slightly favouring the minimal intervention strategy. However, these differences, like the other differences in tables 2 and 3, were small and not statistically significant. Table 4 shows that in subgroups of patients with high baseline scores on psychosocial measures or with subacute or recurrent low back pain, the differences between the two groups were also small and not statistically significant.
Table 4.
Subgroup analyses: difference over time between intervention groups
| Measurement | Functional disability (RDQ): mean difference*(95% CI) | No recovery: odds ratio†(95% CI) |
|---|---|---|
| Psychosocial measures | ||
| Fear-avoidance (0-24): | ||
| FABQ>15 (n=150) | −0.35 (−1.65 to 1.30) | 0.89 (0.36 to 2.18) |
| FABQ≤15 (n=164) | 0.80 (−0.58 to 1.38) | 1.50 (0.64 to 3.53) |
| Catastrophising (0-36): | ||
| CSQ>11 (n=140) | 0.20 (−1.19 to 1.59) | 0.72 (0.29 to 1.80) |
| CSQ≤11 (n=174) | 0.37 (−0.78 to 1.52) | 1.84 (0.80 to 4.22) |
| Distress (0-32): | ||
| 4DSQ>10 (n=107) | 0.35 (−1.55 to 2.26) | 1.35 (0.51 to 3.60) |
| 4DSQ≤10 (n=206) | 0.35 (−0.54 to 1.23) | 1.16 (0.52 to 2.56) |
| Episodes of low back pain | ||
| ≥6 weeks or ≥3 episodes in past year (n=145) | −0.24 (−1.85 to 1.37) | 1.37 (0.58 to 3.22) |
| <6 weeks and <3 episodes in past year (n=169) | 0.54 (−0.27 to 1.34) | 0.88 (0.38 to 2.08) |
RDQ=Roland-Morris disability questionnaire; FABQ=fear-avoidance beliefs questionnaire; CSQ=coping strategies questionnaire; 4DSQ=four dimensional symptom questionnaire (higher scores mean more functional disability, more fear-avoidance, more catastrophising thoughts, and more distress).
Minimal intervention strategy (MIS) minus usual care (UC), adjusted for baseline values and estimated with multilevel analysis. Mean difference >0 means that over 12 months minimum intervention strategy (MIS) group had higher mean score on functional disability than usual care (UC) group.
MIS versus UC, estimated with multilevel analysis. Odds ratio >1 means that over 12 months more patients in MIS group than in UC group reported no recovery.
Treatment received
In the first six weeks, more patients in the minimal intervention strategy group than in the usual care group visited their general practitioner (96% v 24%). In the minimal intervention strategy group, 103 (72%) visited their general practitioner for one consultation, 30 (21%) for two consultations, and 4 (3%) for three consultations. Between six and 52 weeks, the proportion of patients visiting their general practitioner was comparable in the two groups (29% v 28%).
In the first six weeks, more patients in the usual care group than in the minimal intervention strategy group visited a physiotherapist, exercise therapist, or manual therapist (39% v 18%). These figures decreased to 28% and 16% between six and 13 weeks. Between 13 and 52 weeks, the referral rate was comparable in the two groups (14% v 17%).
Discussion
Our new treatment strategy aimed at psychosocial factors and delivered by general practitioners showed no clinically relevant or statistically significant effects compared with usual care in patients with (sub)acute low back pain. Although our study was not powered to firmly establish subgroup effects, subgroup analyses also yielded effect sizes that were not clinically relevant. Findings of (in)effectiveness may result from the interaction between the intervention itself, the care provider, and the patient, and may be influenced by methodological characteristics of the study.
Intervention
As regards the intervention, one might argue that the minimal intervention strategy lacked sufficient intensity, frequency, or duration to establish a change in outcomes. For instance, 72% of the patients in the minimal intervention strategy group had only one 20 minute consultation in which psychosocial issues were assessed and discussed. We are not aware of trials that have studied more intensive psychosocial interventions for treatment of (sub)acute low back pain delivered by general practitioners. However, even if a more intensive psychosocial intervention seemed to be effective, one might wonder if that intervention would ever become “usual care” as the general practitioner's available time is limited.
Care provider
In our study the care providers were general practitioners who were interested in the study objectives and willing to participate. General practitioners in the usual care group might also have paid attention to psychosocial factors. General practitioners who decided to participate may have been especially interested in the role of psychosocial issues in low back pain. Furthermore, general practitioners are assumed to consider not solely physical factors in patients with non-specific complaints. Therapists to whom some of the patients in the usual care group were referred may also have considered psychosocial factors. This may have resulted in a diminished contrast between the treatment groups. However, participating general practitioners indicated before-hand that they felt unsure about which psychosocial factors to consider and how to discuss these factors.
Another explanation for the fact that we found no effect may be that general practitioners did not deliver the minimal intervention strategy adequately. It is difficult to check the actual quality of the minimal intervention strategy. We asked general practitioners to record the content of their consultations on standardised forms and to record one of their consultations on audiotape. According to the forms, general practitioners mostly carried out the minimal intervention strategy intervention as intended; however, 18% of the patients in this group reported referral to a therapist even though we explicitly asked general practitioners in this group not to refer in the first six weeks. Unfortunately, too few audio recordings were made to enable a proper analysis of the quality of the consultations. Therefore, we cannot rule out that the fact that we found no effect was (partly) caused by an insufficient quality of the minimal intervention strategy.
Patient
The participants had (sub)acute or recurrent low back pain. As many episodes of acute low back pain resolve rapidly,2 one might claim that the fact that we found no effect may (partly) be explained by a favourable natural course of symptoms in both groups. Tables 2 and 3 confirm that in 60-70% of the patients symptoms resolved within 6-13 weeks. One might hypothesise that it may be more relevant to apply the minimal intervention strategy to the subgroup of patients who do not have such a favourable prognosis rather than to all patients visiting their general practitioner because of low back pain. Analyses of subgroups consisting of patients who had one characteristic in common (for example, a high baseline score on distress) showed no benefit from the minimal intervention strategy over usual care. As the crux of a relevant subgroup may be the presence of a certain combination of factors, prediction rules could be developed to identify patients with an unfavourable prognosis or patients most likely to respond to the minimal intervention strategy.
Methodological considerations
By using a prerandomisation design in which patients were kept unaware that two interventions were compared, we controlled for contamination between groups and prevented selective withdrawal from the study. As both patient groups were similar at baseline, selection bias is unlikely to have influenced our findings. Furthermore, given our relatively large sample size (314), the low dropout rate (8%), and the use of multilevel analysis in which we adjusted for possible effects of clustering, we conclude that the fact that we found no effect cannot be attributed to methodological flaws.
Conclusion
This study provides no evidence that (Dutch) general practitioners should adopt our new treatment strategy aimed at psychosocial prognostic factors in patients with (sub)acute low back pain. However, as this study is the first, and as yet the only, study to investigate management of psychosocial factors by general practitioners in patients with low back pain, we need more studies on the effectiveness of psychosocial interventions in general practice. Further research should also examine why the minimal intervention strategy was not more effective than usual care.
What is already known on this topic
Psychosocial factors play an important role in the development of chronic pain
Whether a psychosocial intervention delivered by general practitioners may prevent chronic low back pain is unclear
What this study adds
An intervention aimed at psychosocial factors was no more effective than usual care in accelerating recovery and reducing functional disability and sick leave, either in the whole group or in relevant subgroups
This study provides no evidence that (Dutch) general practitioners should aim their treatment at psychosocial prognostic factors in patients with (sub)acute low back pain
We thank all participating patients and general practitioners for their time and effort.
Contributors: DAWMvdW and LMB developed the protocol and secured funding. PJ, DAWMvdW, and HEvdH were responsible for the conception, design, and organisation of the trial. PJ collected the data, did the statistical analyses with JWRT, and wrote the original draft. PJ, DAWMvdW, HEvdH, JWRT, WABS, and LMB contributed substantially to interpreting the data, revised the draft critically for important intellectual content, and approved the final version of the paper. PJ, DAWMvdW, HEvdH, WABS, and LMB are guarantors.
Funding: This study was supported by a grant (No 2200.0095) from the Netherlands Organization for Health Research and Development (ZonMw), the Hague. The funding source had no involvement in the work.
Competing interests: None declared.
Ethical approval: The study was approved by the medical ethics committee of the VU University Medical Center, Amsterdam.
References
- 1.Picavet HSJ, Schouten JSAG. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain 2003;102: 167-78. [DOI] [PubMed] [Google Scholar]
- 2.Pengel LHM, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ 2003;327: 323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas E, Silman AJ, Croft PR, Papageorgiou AC, Jayson MI, Macfarlane GJ. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ 1999;318: 1662-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002;27: E109-20. [DOI] [PubMed] [Google Scholar]
- 5.Van der Linden MW, Westert GP, De Bakker DH, Schellevis FG. Tweede Nationale studie naar ziekten en verrichtingen in de huisartpraktijk: klachten en aandoeningen in de bevolking en in de huisartspraktijk. Utrecht/Bilthoven: NIVEL/RIVM, 2004.
- 6.Faas A, Chavannes AW, Koes BW, Van den Hoogen JMM, Mens JMA, Smeele LJM, et al. NGH-Standaard Lage-Rugpijn. Huisarts en Wetenschap 1996;39: 18-31. [Google Scholar]
- 7.Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W. Pitfalls of patient education: limited success of a program for back pain in primary care. Spine 1996;21: 345-55. [DOI] [PubMed] [Google Scholar]
- 8.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect: a randomised controlled trial of a novel educational booklet in primary care. Spine 1999;24: 2484-91. [DOI] [PubMed] [Google Scholar]
- 9.Roberts L, Little P, Chapman J, Cantrell T, Pickering R, Langridge J. The back home trial: general practitioner-supported leaflets may change back pain behavior. Spine 2002;27: 1821-8. [DOI] [PubMed] [Google Scholar]
- 10.Main CJ, Watson P. Assessment and management of the distressed and angry low back pain patients in primary care, private practice and community settings. In: Gifford L, ed. Topical issues in pain. Volume 3. Falmouth: CNS Press, 2001.
- 11.Kendall NAS, Linton SJ, Main CJ. Guide to assessing psychosocial yellow flags in acute low back pain: risk factors for long-term disability and work loss. Wellington, New Zealand: Accident Rehabilitation and Compensation Insurance Corporation of New Zealand and the National Health Committee, 1997.
- 12.Van der Horst HE, Schellevis FG, Van Eijk JTM, Bleijenberg G. Managing patients with irritable bowel syndrome in general practice: how to promote and reinforce self-care activities? Patient Educ Couns 1998;35: 149-56. [DOI] [PubMed] [Google Scholar]
- 13.Academisch Ziekenhuis Maastricht. Het rugboekje. Maastricht, Netherlands: Pijn Kennis Centrum, 2000.
- 14.Royal College of General Practitioners. The back book. Norwich: Stationery Office, 1996.
- 15.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low back pain. Spine 1983;8: 141-4. [DOI] [PubMed] [Google Scholar]
- 16.Van der Heijden GJ, Leffers P, Wolters PJ, Verheijden JJ, van Mameren H, Houben JP, et al. Effect of bipolar interferential electrotherapy and pulsed ultrasound for soft tissue shoulder disorders: a randomised controlled trial. Ann Rheum Dis 1999;58: 530-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundeberg T, Lund I, Dahlin L, Borg E, Gustafsson C, Sandin L, et al. Reliability and responsiveness of three different pain assessments. Rehabil Med 2001;33: 279-83. [DOI] [PubMed] [Google Scholar]
- 18.Beurskens AJ, de Vet HC, Köke AJ, Lindeman E, van der Heijden GJ, Regtop W, et al. A patient-specific approach for measuring functional status in low back pain. J Manipulative Physiol Ther 1999;22: 144-8. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE, Sherbourne CD. The MOS-36-item short-form health status survey (SF-36). 1: conceptual framework and item selection. Med Care 1992;30: 473-83. [PubMed] [Google Scholar]
- 20.Waddell G, Somerville D, Henderson I, Newton M, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52: 157-68. [DOI] [PubMed] [Google Scholar]
- 21.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 1983;17: 33-44. [DOI] [PubMed] [Google Scholar]
- 22.Terluin B, van Rhenen W, Schaufeli WB, de Haan M. The four-dimensional symptom questionnaire (4DSQ): measuring distress and other mental health problems in a working population. Work Stress 2004;18: 187-207. [Google Scholar]
- 23.Bombardier C, Hayden J, Beaton D. Minimal clinically important difference: low back pain: outcome measures. J Rheumatol 2001;28: 431-8. [PubMed] [Google Scholar]
- 24.Cosby RH, Howard M, Kaczorowski J, Willan AR, Sellors JW. Randomizing patients by family practice: sample size estimation, intracluster correlation and data analysis. Fam Pract 2002;20: 77-82. [DOI] [PubMed] [Google Scholar]
- 25.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine 2003;28: 2551-60. [DOI] [PubMed] [Google Scholar]