Abstract
Background
Cardiopulmonary resuscitation (CPR) is an important advance directive (AD) topic in patients with progressive cancer; however such discussions are challenging.
Objective
This study investigates whether video educational information about CPR engenders broader advance care planning (ACP) discourse.
Methods
Patients with progressive pancreas or hepatobiliary cancer were randomized to an educational CPR video or a similar CPR narrative. The primary end-point was the difference in ACP documentation one month posttest between arms. Secondary end-points included study impressions; pre- and post-intervention knowledge of and preferences for CPR and mechanical ventilation; and longitudinal patient outcomes.
Results
Fifty-six subjects were consented and analyzed. Rates of ACP documentation (either formal ADs or documented discussions) were 40% in the video arm (12/30) compared to 15% in the narrative arm (4/26), OR=3.6 [95% CI: 0.9–18.0], p=0.07. Post-intervention knowledge was higher in both arms. Posttest, preferences for CPR had changed in the video arm but not in the narrative arm. Preferences regarding mechanical ventilation did not change in either arm. The majority of subjects in both arms reported the information as helpful and comfortable to discuss, and they recommended it to others. More deaths occurred in the video arm compared to the narrative arm, and more subjects died in hospice settings in the video arm.
Conclusions
This pilot randomized trial addressing downstream ACP effects of video versus narrative decision tools demonstrated a trend towards more ACP documentation in video subjects. This trend, as well as other video effects, is the subject of ongoing study.
Introduction
Increasing emphasis is being placed on advance care planning (ACP), the process by which patients, their family, and health care providers address and plan future medical care.1,2 Advance directives (ADs), such as do-not-resuscitate (DNR) orders and living wills, are often limited in completion, scope, portability, timing, and translation into desired care,3,4 and are therefore only one component of ACP, including in oncology. Associated barriers to optimal delivery of care consistent with patient wishes are numerous and include time constraints, limits in patients' health literacy,5 attitudes regarding medical decision making,6,7 patient-physician communication deficiencies,8,9 and lack of disclosure of10–12 and inaccuracy of physician prognosticating in advanced illness.13 ACP often occurs late in the cancer patient illness course, and without the participation of the oncologist.14
Previous efforts to improve communication between patients and providers have been suboptimal, and part of the problem may be the lack of proactive involvement by the treating physician.15 Government legislation and organizational initiatives have recently spotlighted the importance of ACP, including in patients with cancer.16
The use of video decision aids is one innovative solution to help surmount communication barriers. Videos broadly depicting categories of available care (such as life-sustaining therapies, disease-directed therapies, and comfort-directed care) have been demonstrated to impact comfort with, knowledge about, and preferences for medical care in patients with advanced dementia17 as well as brain cancer.18 Decision aids are meant to educate patients about their options, enhance autonomy, and engender discourse with physicians.
An important component of ACP, especially for patients with advanced cancer, is the decision making process regarding cardiopulmonary resuscitation (CPR). Inaccurate depictions of CPR in the media19 contribute to an important discrepancy between common perception of medical care and reality. In addition to a general misunderstanding of CPR20 and its high rate of failure in patients with advanced cancer,21 patient ADs opting out of these interventions are sometimes not honored.15
Building on existing studies using broad goals-of-care videos, we considered that an educational video specifically about CPR might be particularly beneficial in advanced cancers, both for patient preference (the primary outcome of a companion study22 to this study) and for longitudinal ACP documentation, as primarily and uniquely examined here. In a randomized controlled pilot trial, we therefore studied the ACP effects of a CPR video on patients with progressive pancreas and hepatobiliary cancers. This study explored the hypothesis that video, compared to a narrative description, enhances the completion of ADs and/or documented discussions about desired care.
Methods
Participants
Ambulatory patients with gastrointestinal malignancies receiving active follow-up care in the medical oncology clinics at Memorial Sloan-Kettering Cancer Center (MSKCC) were screened for eligibility. Inclusion criteria included English-speaking patients 21 years of age or older with progressive exocrine pancreas or hepatobiliary cancers with no prior AD designation. For the purposes of the trial, ADs referred to any document that instructed caregivers on details of future care (subjects were still eligible if they had a power of attorney or health care proxy, as these documents identify a person designated to make decisions should a subject be unable to do so, but do not necessarily direct or detail desired care).
Progressive disease was defined as a life expectancy of less than one year as judged by the treating oncologist and any of the following: unresectable disease with progression on at least one course of treatment (surgery, radiation, or chemotherapy); untreated patients unfit for therapy because of comorbidities or Eastern Cooperative Oncology Group (ECOG) performance status >2; and patients with ECOG performance status 2.23 Treating oncologists had to have confirmed with the research team that they discussed on at least one occasion with the patient that their cancer was incurable (for patient safety, as incurable cancer was mentioned in the video and narrative). Exclusion criteria included (1) a Short Portable Mental Status Questionnaire24 (SPMSQ) score of less than “intact mental functioning” (≥3 errors) and (2) any patient condition (e.g., concern for psychological distress) that the treating oncologist deemed would make the study inappropriate for the patient.
Study design and randomization
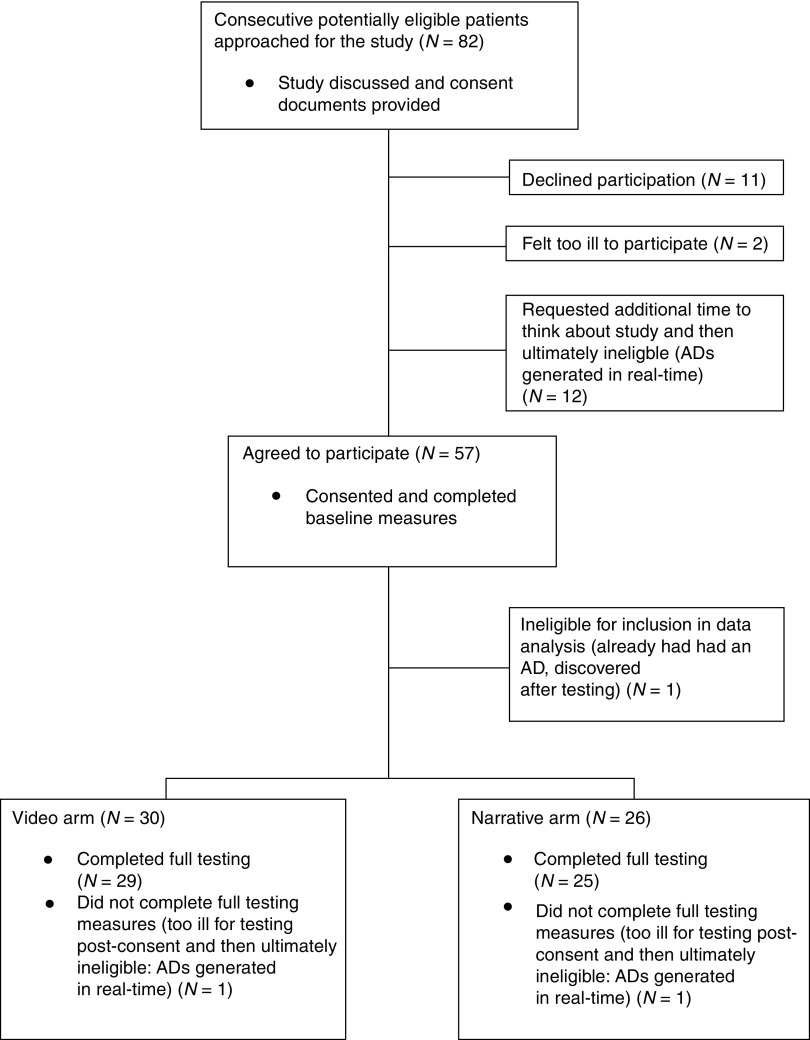
The study was approved by the MSKCC institutional review board. All 14 gastrointestinal medical oncologists at MSKCC agreed to participate; 9 of these had potentially eligible patients. Oncologists were regularly contacted by study staff regarding consecutive patients with potential eligibility (see Figure 1). During follow-up visits, participating oncologists introduced ACP and the research question of whether video education could augment the process. The study procedures were broached with patients, and those who were interested underwent consenting procedures if they scored ≤3 errors on the SPMSQ.24
FIG. 1.
Consort diagram. AD, advance directive.
After consent, subjects were centrally registered and randomized 1:1 by random permuted block to either a CPR video or a CPR narrative arm. Given the nature of the intervention and control, participants were not blinded to their treatment group assignments. Treating oncologists were not informed of the allocation arm of their patients. Testing procedures thereafter were carried out in a quiet, private space with subjects (and any interested family/friends) by one member of the research team (ASE), lasting approximately 30 minutes.
At the start of testing, demographic information was obtained. As in our previous work,18 knowledge of ACP, including details regarding CPR and mechanical ventilation, was assessed with five true/false questions and one multiple choice question (see Table 1). Baseline preferences (“yes,” “no,” “uncertain”) for CPR and mechanical ventilation were queried.
Table 1.
Knowledge Assessment Questions Used Pre-Intervention and Post-Intervention in Subjects in Both the Narrative and Video Arms (Score Range, 0 to 6)
| Item | Statement | Correct answer |
|---|---|---|
| 1 | True or false: Cardiopulmonary resuscitation or CPR is a medical procedure that is done on patients whose heart stops beating in an attempt to restart their heart. | True |
| 2 | True or false: Most advanced cancer patients that get CPR in the hospital survive and get to leave the hospital. | False |
| 3 | True or false: Most advanced cancer patients who survive CPR and being placed on a breathing machine have very few complications from these procedures. | False |
| 4 | True or false: When patients are on a mechanical ventilator, they are able to speak and eat on their own. | False |
| 5 | True or false: Once you tell your doctor what kind of medical care you want if your cancer becomes very advanced, you cannot change your wishes in the future. | False |
| 6 | Multiple choice: How many advanced cancer patients that get CPR in the hospital survive and get to leave the hospital? | c) |
| a) Almost all (more than 90%) | ||
| b) About half (about 50%) | ||
| c) Very few (less than 10%) |
Subjects randomized to the video arm were shown a short (three minutes) video, wherein narration/voice on the video defined CPR and mechanical ventilation as well as the likelihood of success of these procedures in patients with advanced cancer. Images included a team of physicians performing chest compressions, oxygenation via bag valve mask and tracheal intubation, as well as a sedated patient being mechanically ventilated in an ICU. Originally developed by Volandes using published filming criteria,25 the video and its narrative were drafted and edited by a panel of specialists in oncology, critical care, palliative care, health literacy, and medical ethics. Additionally, the video was shown to focus groups of patients and their families.26 Filming was performed without stage directions or prompts, in order to convey candid realism.27 The narrative arm employed a script identical to the one heard in the video (therefore both arms contained verbal information; the video contained verbal and visual information) and was written with language below an eighth-grade reading level.28 The interviewer (ASE) read the narrative out loud to subjects randomized to the narrative with similar speed and intonation as heard in the video.
After the intervention, subjects answered the same pretest assessments of knowledge as well as preferences about CPR and mechanical ventilation. Subject impressions about the study material were then queried using a Likert scale assessing comfort with viewing the CPR video (or hearing the script), its usefulness, and whether subjects would recommend the information to others.
In the month immediately following testing, the research team reviewed the electronic medical record for ACP documents. Medical records included inpatient and outpatient physician progress notes as well as all other health care provider documentation. Documented ACP was defined as either (1) formal AD documents generated (e.g., treatment-limiting orders such as DNR) or (2) documented discussions about patient wishes/perspectives for care in the setting of their progressive malignancy (e.g., desire to continue or decline cancer-directed treatments, considerations of risk and benefits of treatments, election of comfort-oriented care, etc.). This two-component definition, rather than sole AD completion, was chosen given the limitations of traditional ADs. The one month posttest timeframe was chosen both to grant time to think about the study information and as an estimate of the timeframe in which the majority of subjects would have another visit with their oncologist.
For the purposes of an exploratory, secondary outcome measure, chart abstraction was continued monthly for each subject past the one month posttest timeframe, until death or six months posttest, whichever came first. Information (including outside hospital records) was collected on timing and aspects of further ACP documentation, number and nature of hospitalizations, and place of death.
Statistical analysis
The sample size was powered by using AD estimated completion rates of 25% for subjects in a narrative arm and 70% in subjects allocated to educational visual media. These were estimates used in planning a prior video trial.17 It was estimated that this 70% versus 25% contrast in a sample of 56 subjects (28 per arm) would result in statistical power of 80% with a Type-I error rate of 0.01 in a χ2 test.
For the primary end-point of AD documentation one month posttest, subjects were analyzed according to intention-to-treat (including two who did not complete full testing measures—see Figure 1). Subjects with both documented discussions and completed ADs were counted only once towards this primary data analysis. Fisher's Exact Test was ultimately used for the comparison across the arms for the primary end-point data because of low cell counts in the observed contingency tables. For the secondary outcomes, data with continuous variables were compared using an independent-sample t test assuming no equal variance. Fisher's Exact Test was used for secondary outcome data with discrete variables. McNemar's χ2 test with continuity correction was used to analyze pre- and post-intervention changes in patients' preferences for CPR and mechanical ventilation. For analysis of preference data, answers of “uncertain” were grouped with “no” so as to avoid calculation errors caused by sparse data points in the original 3X2 comparison (continuity correction).
Results
Study participants
Eighty-two potentially eligible patients were approached (see Figure 1) between July 27, 2010, and May 20, 2011. No subjects were ineligible on the basis of mental incapacity. Eleven of the approached patients (13%) were potentially eligible but declined participation, the most common reason for declining being not wanting to discuss the study topics. A total of 57 participants were consented and randomized (70% of the 82 total approached). The characteristics of the subjects who underwent testing and data analysis are shown in Table 2. No statistical differences were found between the arms.
Table 2.
Baseline Demographics of Subjects in Video and Narrative Arms
| Demographic (available at time of consent) | Video (N=30) | Narrative (N=26) |
|---|---|---|
| Age (mean age in years, range) | 64.8 (29–81) | 65.9 (49–86) |
| Gender | ||
| Male | 15 (50%) | 14 (54%) |
| Malignancy type | ||
| Exocrine pancreas Carcinoma | 23 (77%) | 21 (81%) |
| Ampullary carcinoma | 2 (7%) | 0 (0%) |
| Gall bladder carcinoma | 1 (3%) | 1 (4%) |
| Cholangiocarcinoma | 3 (10%) | 2 (8%) |
| Hepatocellular carcinoma | 1 (3%) | 2 (8%) |
| Mean ECOG Performance Status (range) | 1 (0–2) | 1 (0–3) |
| Demographic (available at time of testing) | Video (N=29) | Narrative (N=25) |
|---|---|---|
| Education | ||
| Grade school | 2 (7%) | 0 (0%) |
| High school | 3 (10%) | 4 (16%) |
| College | 14 (48%) | 15 (60%) |
| Postgraduate | 10 (35%) | 6 (24%) |
| Race | ||
| White | 20 (69%) | 15 (60%) |
| Asian | 3 (10%) | 6 (24%) |
| Black | 1 (3%) | 2 (8%) |
| Other | 5 (17%) | 2 (8%) |
| Religion | 4 (14%) | 5 (20%) |
| Catholic | 13 (45%) | 10 (40%) |
| Protestant | 2 (7%) | 1 (4%) |
| Other Christian | 1 (3%) | 1 (4%) |
| Jewish | 8 (28%) | 7 (28%) |
| Muslim | 2 (7%) | 0 (0%) |
| Other | 3 (10%) | 6 (24%) |
| Attendance at religious services | ||
| Never | 3 (10%) | 4 (16%) |
| Once monthly | 16 (55%) | 14 (56%) |
| Twice monthly or more | 10 (35%) | 7 (28%) |
| Marital status | ||
| Married/partnered | 22 (76%) | 17 (68%) |
| Widowed | 2 (7%) | 2 (8%) |
| Never married | 4 (14%) | 3 (12%) |
| Divorced | 1 (3%) | 3 (12%) |
| Family history of cancer | 22 (76%) | 19 (56%) |
| Close with someone with advanced cancer | 18 (62%) | 15 (60%) |
| If Yes, was the subject with that person during last month of life? | 14Y, 4N | 12Y, 3N |
| If Yes, was the subject with that person during last week of life? | 15Y, 3N | 13Y, 2N |
| Prior discussions about wishes at end-of-life | 12 (41%) | 16 (64%) |
No statistically reliable difference was found across the two groups in any of the variables.
ECOG, Eastern Cooperative Oncology Group.
AD documentation one month posttest (primary outcome)
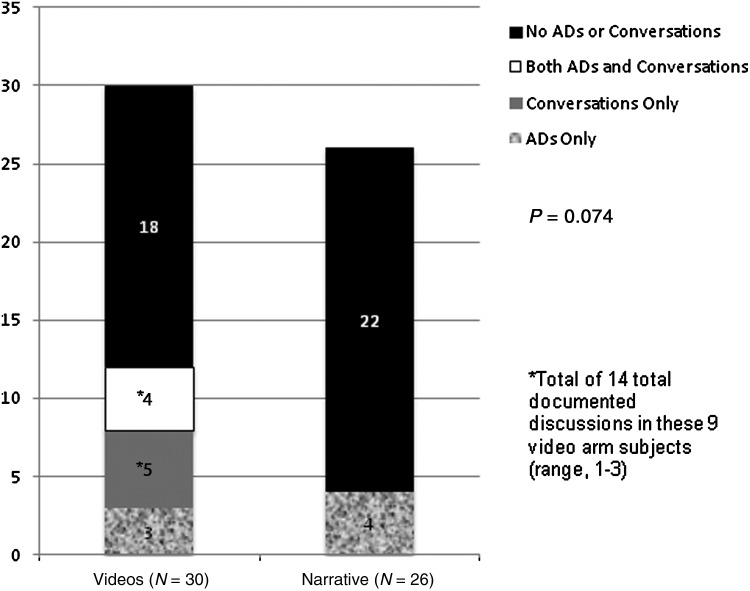
Rates of ACP documentation within one month posttest (either formal ADs or documented discussions about patient wishes) were not statistically different between the video arm (12/30, 40%) and the narrative arm (4/26, 15%; OR=3.6 [95% CI: 0.9–18.0], p=0.07) (see Figure 2). The ADs were all DNR orders. The content of the majority of documented conversations was patients either declining life-sustaining interventions, or otherwise needing to think more about end-of-life wishes before deciding. The majority of conversations were documented by physicians, the minority by other providers (e.g., social workers).
FIG. 2.
Subject ADs and/or ACP conversations documented in the medical record one month posttest (primary outcome). AD, advance directive.
Knowledge scores
There were no differences between the mean pretest CPR knowledge scores (correct answer score range, 0–6) between the video and narrative arms, respectively (3.4 and 3.4, p=0.783; 95% CI: −0.6–0.8). Knowledge scores increased significantly in both arms after the intervention (p<0.001; 95% CI: 1.2–2.1 in the video arm and p<0.001; 95% CI: 0.9–1.9 in the narrative arm) but were not different across the two arms posttest (4.9 and 4.9, p=0.746; 95% CI: −0.9–0.6).
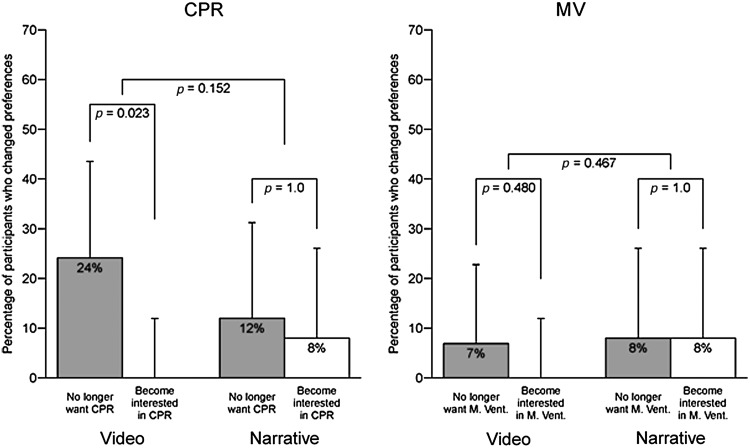
Preferences for CPR and mechanical ventilation
In the video and narrative arms, respectively, there were no statistical differences in subjects' pretest preferences: 42% and 20% (p=0.121) for CPR; 28% and 12% for mechanical ventilation (p=0.317).
In the video and narrative arms, respectively, there were no statistical differences in subjects' posttest preferences: 17% and 16% (p=0.614) for CPR; 21% and 12% for mechanical ventilation (p=0.683).
Figure 3 illustrates the changes in preference from pre- to posttest: preferences for CPR changed significantly in the video arm (24% no longer wanted CPR and 0% became interested in CPR; χ2=5.1, p=0.023) but not in the narrative arm (χ2=0, p=1). Preferences regarding mechanical ventilation did not change from pre- to posttest in the video arm (χ2=0.5, p=0.480) or in the narrative arm (χ2=0, p=1).
FIG. 3.
Changes in pre- and posttest preference for CPR and mechanical ventilation.
Subject impressions and tolerability of study information
The study information was well received by subjects in both arms (see Table 3). Subjects in both the video and narrative arms, respectively, reported the CPR information to be “very helpful” (48%, 48%), “very comfortable” to receive (69%, 68%), and “definitely” or “probably” recommended to other people facing similar health care decisions (86%, 96%). There were no adverse events reported in either group.
Table 3.
Subject Impressions of Study Information
| Video (N=29) | Narrative (N=25) | Odds ratio (95% CI) | p-value1 | |
|---|---|---|---|---|
| Helpfulness of the CPR information | ||||
| “Very helpful” | 14 (48%) | 12 (48%) | 1.01 (0.30– 3.36) | 1.00 |
| Comfort with the CPR information | ||||
| “Very comfortable” | 20 (69%) | 17 (68%) | 1.04 (0.28– 3.84) | 1.00 |
| Recommend CPR info to others facing similar decision | ||||
| “Definitely” or “Probably yes” | 25 (86%) | 24 (96%) | 0.27 (0.01– 2.95) | 0.36 |
Fisher's Exact Test
CPR, cardiopulmonary resuscitation.
Longitudinal patient outcomes
Outcomes until six months posttest or death, whichever occurred first, are shown in Table 4. More deaths occurred in the video arm compared to the narrative arm (20 [67%] versus 9 [35%]; OR=3.7 [95% CI: 1.1–13]), and more patients died in hospice settings in the video arm (16 [53%] versus 7 [27%]) (see Table 4). Fifty-two percent of all subjects died by study end, the majority receiving hospice care.
Table 4.
Longitudinal Patient Outcomes
| Outcome | Video (n=30) | Narrative (n=26) | 95% Cl |
|---|---|---|---|
| # ADs before 6 mo or death | 19 | 15 | 0.3–4.0 (OR=1.3) |
| Median testing → AD (d) | 60 | 72 | −94–70 |
| Mean | 76 | 82 | −51–39 |
| Range | 0–189 | 0–182 | N/A |
| # deaths in 6 mo & location | 20 (12 HH, 4 IPH, 4 IP) | 9 (4 HH, 3 IPH, 2 IP) | 1.1–13.0 (OR=3.7) |
| Median AD → death (d) | 21 | 20 | −20–22 |
| Mean | 35 | 25 | −14–33 |
| Range | 3–172 | 1–60 | N/A |
| Median # discussions documented>1 mo post | 0 | 1 | −0.1–2.0 |
| Mean | 1 | 2 | −0.5–2.0 |
| Range | 0–7 | 0–9 | N/A |
| Median # hospital admits | 1 | 1 | −0.9–0.9 |
| Mean | 1 | 1 | −0.5–1.0 |
| Range | 0–4 | 0–8 | N/A |
| Median hospital LOS (d) | 5 | 7 | −8–4 |
| Mean | 7 | 10 | −3–10 |
| Range | 0–30 | 54 | N/A |
| Total # ICU admissions | 0 | 3 | N/A |
| Total # CPR and/or MV | 1 | 3 | N/A |
AD, advance directive; CI, confidence interval; CPR, cardiopulmonary resuscitation; d, days; HH, home hospice; ICU, intensive care unit; IP, inpatient; IPH, inpatient hospice; LOS, length of stay; MV, mechanical ventilation; OR, odds ratio; N/A, not applicable.
Discussion
This pilot randomized trial of an educational CPR video in subjects with progressive exocrine pancreas and hepatobiliary cancers demonstrated a statistical trend in the one month posttest towards more ACP documentation (AD or documented discussions with medical providers) compared to a narrative. The interventions in both arms were well received and improved subject knowledge about CPR and mechanical ventilation. The video changed subject preferences for CPR, whereas the narrative did not. The significance of the higher death rate and more deaths in hospice, both observed in the video arm, is unclear. These secondary data are solely exploratory in nature. However, they suggest that video decision-making tools may have effects on patient care, and that these effects may last months after viewing.
We view the trend towards statistical significance for higher one month posttest ACP documentation in the video arm as suggestive of a clinical signal of enhanced discourse between patient and physicians, a phenomenon which to our knowledge, has not previously been demonstrated. Our prior studies have illustrated that more broadly educational visual media are similarly palatable and effective in enhancing knowledge and elucidating care preferences consistent with patient wishes,17,18 but until this study (as well as a multisite companion study primarily examining patient preference22) had not utilized a video focusing on CPR. Unlike our companion study22 and the existing literature, this study was unique in prospectively examining the clinical effects of video education on documented patient-physician communication. Independent of knowledge (which increased posttest in both arms) and preference (which changed for CPR but not mechanical ventilation, a finding itself which requires further consideration, i.e., what underlies the differential perception and preferences regarding CPR versus mechanical ventilation), it is possible that video, over verbal information, leaves a potent impression that drives patients to initiate with clinicians discourse about ACP, the details of which are ultimately documented.
The fact that the study design lacked physician prompts at follow-up visits further suggests the power of such patient education tools. Our results are also in keeping with nonvideo studies of ACP in cancer: end-of-life discussions are associated with avoidance of CPR near death, as well as earlier hospice referrals.29,30 This suggests that patients with better understanding of CPR and its likely outcomes tend to choose less intensive medical care at the end of life, which is consistent with our findings.
The lack of statistical significance seen in our primary outcome results might indicate no true intervention arm effect (after all, posttest knowledge was similarly higher in both arms, whereas in our group's other randomized cancer studies,18,22 knowledge increased more in the video arm) but otherwise might be explained by the AD estimates from which we powered the study. In retrospect, using estimated AD prevalence figures from a study with dementia subjects (25% in the narrative arm compared to 70% in the video arm)17 was suboptimal for our ambulatory cancer population, which has far fewer ADs documented relative to the dementia population. In a study examining the characteristics of DNRs in all patients seen at MSKCC between 2000 and 2005, the yearly prevalence of DNRs in the entire population was approximately 10%.31 While the prevalence was between 80% and 90% for patients who died at MSKCC, DNR completion most often occurred the day the patient died.31 This is also consistent with a cohort of 1186 consecutive advanced pancreas cancer patients at the Mayo Clinic, wherein only 15% had an AD as part of the medical record.32 One additional indication of patient wishes in the video arm (or one fewer in the narrative arm) would have made for statistical significance in our study.
Our study has limitations. First, the majority of the population we studied was highly educated (which could have factored into the apparent ceiling effect observed in the knowledge assessment items used), Caucasian, and comprised a specific grouping of progressive cancers undergoing treatment at a quaternary medical center. However, our companion study22 broadens the generalizability of this work, which was a small pilot study examining a specific primary end-point and generating additional data for future investigations. Second, it is possible that bias was introduced from participating clinician individual practice and documentation styles, as well as by the lack of blinding of testing staff. Third, 13% of the potentially eligible patients approached declined involvement in the study. However, these patients represent the minority. Finally, chart abstraction methodology inherently limits data objectiveness and completeness. However, randomization allocation was not visible during abstraction, and outside hospital records were able to be obtained for review in all necessary cases.
Conclusions
Despite these limitations, this study shows that innovative strategies such as video educational aids are easy to use, well received, and may enhance documented discourse between patients and treating oncologists. This discourse rests at the crux of the ACP process—while not proven causal herein, discourse is likelier to impact patient care than traditional AD documents, which are limited3,4 and therefore sometimes not recognized or honored. The trend in our primary outcome is therefore the subject of ongoing study and suggests that video may assist both in the generation of ADs (which might impact downstream care33) and may contribute in the more overarching and rational ACP strategy34 of outpatient physicians helping patients and families empower themselves to make future decisions in the most well-informed manner possible. Moving forward, our research continues to incorporate video educational aids and is addressing the underpinnings of individual patient values to best meet various communication needs.
Prior Presentations
The study data was presented at the 2012 Annual Meeting of the American Society of Clinical Oncology, and at the 2012 Annual Meeting of the International Society of Advance Care Planning and End-of-Life Care, both this spring in Chicago, Illinois.
Acknowledgments
This work was supported by the American Society of Clinical Oncology 2010 Young Investigator Award to Andrew S. Epstein, MD.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Fried TR. Bradley EH. Towle VR. Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 2.Gillick MR. Advance care planning. N Engl J Med. 2004;350(1):7–8. doi: 10.1056/NEJMp038202. [DOI] [PubMed] [Google Scholar]
- 3.Fagerlin A. Schneider CE. Enough: The failure of the living will. Hastings Cent Rep. 2004;34(2):30–42. [PubMed] [Google Scholar]
- 4.Tonelli MR. Pulling the plug on living wills. A critical analysis of advance directives. Chest. 1996;110(3):816–822. doi: 10.1378/chest.110.3.816. [DOI] [PubMed] [Google Scholar]
- 5.Paasche-Orlow M. Caring for patients with limited health literacy: A 76-year-old man with multiple medical problems. JAMA. 2011;306(10):1122–1129. doi: 10.1001/jama.2011.1203. [DOI] [PubMed] [Google Scholar]
- 6.Dow LA. Matsuyama RK. Ramakrishnan V, et al. Paradoxes in advance care planning: The complex relationship of oncology patients, their physicians, and advance medical directives. J Clin Oncol. 2010;28(2):299–304. doi: 10.1200/JCO.2009.24.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamont EB. Siegler M. Paradoxes in cancer patients' advance care planning. J Palliat Med. 2000;3(1):27–35. doi: 10.1089/jpm.2000.3.27. [DOI] [PubMed] [Google Scholar]
- 8.Olson DP. Windish DM. Communication discrepancies between physicians and hospitalized patients. Arch Intern Med. 2010;170(15):1302–1307. doi: 10.1001/archinternmed.2010.239. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins V. Solis-Trapala I. Langridge C. Catt S. Talbot DC. Fallowfield LJ. What oncologists believe they said and what patients believe they heard: An analysis of Phase I trial discussions. J Clin Oncol. 2011;29(1):61–68. doi: 10.1200/JCO.2010.30.0814. [DOI] [PubMed] [Google Scholar]
- 10.Keating NL. Landrum MB. Rogers SO, Jr., et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;11:11. doi: 10.1002/cncr.24761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baile WF. Lenzi R. Parker PA. Buckman R. Cohen L. Oncologists' attitudes toward and practices in giving bad news: An exploratory study. J Clin Oncol. 2002;20(8):2189–2196. doi: 10.1200/JCO.2002.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Winkler EC. Reiter-Theil S. Lange-Riess D. Schmahl-Menges N. Hiddemann W. Patient involvement in decisions to limit treatment: The crucial role of agreement between physician and patient. J Clin Oncol. 2009;27(13):2225–2230. doi: 10.1200/JCO.2008.17.9515. [DOI] [PubMed] [Google Scholar]
- 13.Christakis NA. Lamont EB. Extent and determinants of error in doctors' prognoses in terminally ill patients: Prospective cohort study. BMJ. 2000;320(7233):469–472. doi: 10.1136/bmj.320.7233.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mack JW. Cronin A. Taback N, et al. End-of-life care discussions among patients with advanced cancer: A cohort study. Ann Intern Med. 2012;156(3):204–210. doi: 10.1059/0003-4819-156-3-201202070-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SUPPORT Principal Investigators: A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 16.Epstein AS. Volandes AE. O'Reilly EM. Building on individual, state, and federal initiatives for advance care planning, an integral component of palliative and end-of-life cancer care. J Onc Pract. 2011;7(6):355–359. doi: 10.1200/JOP.2011.000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volandes AE. Paasche-Orlow MK. Barry MJ, et al. Video decision support tool for advance care planning in dementia: Randomised controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Jawahri A. Podgurski LM. Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. J Clin Oncol. 2010;28(2):305–310. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diem SJ. Lantos JD. Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med. 1996;334(24):1578–1582. doi: 10.1056/NEJM199606133342406. [DOI] [PubMed] [Google Scholar]
- 20.Thorevska N. Tilluckdharry L. Tickoo S. Havasi A. Amoateng-Adjepong Y. Manthous CA. Patients' understanding of advance directives and cardiopulmonary resuscitation. J Crit Care. 2005;20(1):26–34. doi: 10.1016/j.jcrc.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Reisfield GM. Wallace SK. Munsell MF. Webb FJ. Alvarez ER. Wilson GR. Survival in cancer patients undergoing in-hospital cardiopulmonary resuscitation: A meta-analysis. Resuscitation. 2006;71(2):152–160. doi: 10.1016/j.resuscitation.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Volandes AE. Paasche-Orlow MK. Mitchell SL, et al. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. J Clin Oncol. 2012;31:380–384. doi: 10.1200/JCO.2012.43.9570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oken MM. Creech RH. Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. [PubMed] [Google Scholar]
- 24.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 25.Volandes A. El-Jawahri A. Improving CPR decision-making for patients and families with video decision aids. In: Doyle LJ, editor; Saltsman RA, editor. Cardiopulmonary Resuscitation: Procedures and Challenges. New York: Nova Science Publishers; 2012. [Google Scholar]
- 26.Gillick M. Volandes A. The psychology of using and creating video decision aids for advance care planning. In: Lynch TE (ed): Psychology of Decision Making in Medicine and Health Care. New York: Nova Science Publishers; 2007. pp. 193–206. [Google Scholar]
- 27.Grant B. Sloniowski J. Documenting the Documentary: Close Readings of Documentary Film and Video. Detroit, MI: Wayne State University Press; 1998. [Google Scholar]
- 28.Kincaid J. Fishburne R. Rogers R. Chissom B. Memphis, TN: Memphis Naval Air Station; 1975. Derivation of new readability formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy enlisted personnel. [Google Scholar]
- 29.Wright AA. Zhang B. Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prigerson HG. Socialization to dying: Social determinants of death acknowledgement and treatment among terminally ill geriatric patients. J Health Soc Behav. 1992;33(4):378–395. [PubMed] [Google Scholar]
- 31.Levin TT. Li Y. Weiner JS, et al. How do-not-resuscitate orders are utilized in cancer patients: Timing relative to death and communication-training implications. Palliat Support Care. 2008;6(4):341–348. doi: 10.1017/S1478951508000540. [DOI] [PubMed] [Google Scholar]
- 32.Tan TS. Jatoi A. An update on advance directives in the medical record: Findings from 1186 consecutive patients with unresectable exocrine pancreas cancer. J Gastrointest Cancer. 2008;39(1–4):100–103. doi: 10.1007/s12029-008-9041-z. [DOI] [PubMed] [Google Scholar]
- 33.Nicholas LH. Langa KM. Iwashyna TJ. Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. 2011;306(13):1447–1453. doi: 10.1001/jama.2011.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sudore RL. Fried TR. Redefining the “planning” in advance care planning: Preparing for end-of-life decision making. Ann Intern Med. 2010;153(4):256–261. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]