To the Editor: Early primary gastrointestinal non-Hodgkin's lymphoma represents a diagnostic challenge and may be easily misdiagnosed as Crohn's disease or intestinal tuberculosis.[1] Here, we describe a 58-year-old man who was admitted due to recurrent colic in the middle and upper abdomen with intermittent vomiting for 10 months. The colic was paroxysmal lasting from a few minutes to several hours without obvious triggers. His medical history was otherwise unremarkable. In November 2013, gastrointestinal endoscopy revealed gastroenteritis, and abdominal computed tomography (CT) showed jejunal wall edema and thickening. His symptoms did not improve after 1-month treatment for suspected gastroenteritis.
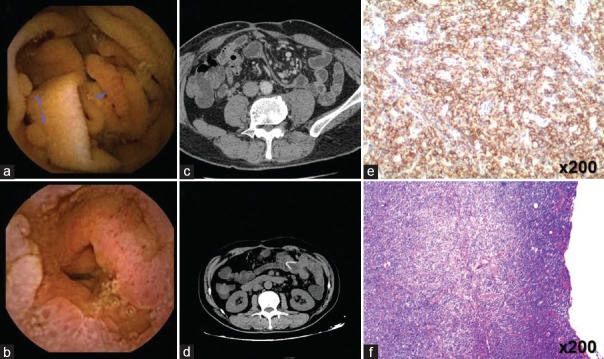
In December 2013, capsule endoscopy showed multiple inflammatory polyps of the small intestine, multiple segmental stenosis, and incomplete intestinal obstruction [Figure 1a and 1b], and a diagnosis of Crohn's disease was made. Two days later, he developed a sudden abdominal pain with hyperpyrexia (39.1°C) and peritoneal irritation. The percentage of blood neutrophils was 90.64%, and C-reactive protein was 196.10 mg/L. He underwent incommodious intestinal resection on consideration of intestinal fistula and abdominal abscess. Biopsy pathology showed features suggestive of Crohn's disease of the small intestine, and immunohistochemistry revealed CD3 (+), CD20 (+), λ (+), κ (+), Ki67 (+), Labeling Index (LI): <5%.
Figure 1.
Capsule endoscopy examination on December 16, 2013, shows multiple inflammatory polyps from the small intestine (arrows) (a) and multiple segmental stenosis in the small intestine (b). (c and d) Enhanced computed tomography scanning on September 28, 2014, shows multiple mesenteric lymph nodes, left upper abdominal mesenteric whirlpool sign, and dilatation of the colon. (e and f) CD20 staining and hematoxylin and eosin staining of the resected specimen, (original magnification ×200).
The patient was discharged and treated with mesalazine slow-release suppository (once/day) and infliximab (300 mg, once/month). Six months later, CT enterography showed multiple thickening of the small intestine wall, and the descending and sigmoid colon, along with multiple air sacs, lumen stenosis, celiac lymph node enlargement, and small intestine incomplete torsion. In September 2014, abdominal CT showed multiple mesenteric lymph nodes, left upper abdominal mesenteric whirlpool sign, and colon dilatation [Figure 1c and 1d]. Azathioprine (100 mg, once/day) was added; however, recurrent postprandial abdominal pain still persisted. In November 2014, small intestine CT enterography showed local lumen stenosis in the jejunum, obstruction of the duodenum and jejunum, thickening of the intestine wall, mesenteric whirlpool sign, and increased and enlarged mesenteric lymph nodes. After 43 days of azathioprine therapy, blood white blood cell count was 2.17 × 109/L and erythrocyte sedimentation rate was 33 mm/h. Double-balloon enteroscopy showed multiple inflammatory polyps in the upper jejunum and circumferential ulceration in the stenosed jejunum (diameter <0.5 cm).
Due to obstruction aggravation, the patient underwent second surgery in December 2014. Pathological biopsy and immunohistochemistry findings (CD20 (+), CD79a (+), CD10 (−), BCL6 (+), MUM (+) CD43 (+), CD5 (+), BCL-2 (+), CD3 (−), PCK (−), EMA (−) KI67 (+), LI: 80% [Figure 1e and 1f]) showed diffuse large B-cell lymphoma. The tumor invaded the intestine wall and the mesentery. The patient started receiving 8 cycles of R-CHOP therapy 2 weeks postoperatively, and his abdominal symptoms were gradually relieved.
Diffuse large B-cell lymphoma, a subtype of small intestine non-Hodgkin's lymphoma, is the most frequent pathological type in the stomach and intestine,[2] and because of missed diagnoses, only 30–40% of patients with early primary gastrointestinal non-Hodgkin's lymphoma receive surgery.[3] The patient had nonspecific symptoms and endoscopic results, leading to a misdiagnosis of Crohn's disease. In the case, small intestinal CT enterography should be performed first, which showed bowel wall thickening and lumen stenosis. This would minimize the chance of capsule endoscopy causing blockage and inducing intestinal obstruction, fistula, and abdominal abscess. Although pathologic biopsy is regarded as golden criteria for diagnosis, misdiagnosis may ensue if clinicians fail to take into consideration of symptoms and therapeutic effect.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank all faculty and staff at the Department of Gastroenterology and Hepatology of our hospital.
Footnotes
Edited by: Li-Min Chen
REFERENCES
- 1.Bautista-Quach MA, Ake CD, Chen M, Wang J. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. J Gastrointest Oncol. 2012;3:209–25. doi: 10.3978/j.issn.2078-6891.2012.024. doi: 10.3978/j.issn.2078-6891.2012.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ding W, Zhao S, Wang J, Yang Q, Sun H, Yan J, et al. Gastrointestinal lymphoma in Southwest China: Subtype distribution of 1,010 cases using the WHO (2008) classifictiona in a single institution. Acta Haematol. 2016;135:21–8. doi: 10.1159/000437130. doi: 10.1159/00043713. [DOI] [PubMed] [Google Scholar]
- 3.Chen JH, Ho CL, Chen YC, Chao TY, Kao WY. Clinicopathological analysis and prognostic factors of 11 patients with primary non-Hodgkin lymphoma of the small intestine in a single institute. Oncol Lett. 2014;8:876–80. doi: 10.3892/ol.2014.2209. doi: 10.3892/ol.2014.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]