Short abstract
Although most people agree that academic medicine needs to reform, the nature of the changes is unclear. ICRAM hopes its five scenarios for the future will aid the debate
In 2003, the BMJ and 40 other partners launched the International Campaign to Revitalise Academic Medicine (ICRAM). Led by a core working party of medical academics representing 14 countries (box), the campaign aims to redefine the core values of and contribute to the evidence base for academic medicine; develop strategy around reformed academic training; and stimulate a public debate on the future. As part of this process ICRAM created a team to develop a vision for the future of academic medicine. This resulted in five future scenarios, which are summarised here. A fuller description is being published this week in the Public Library of Science Medicine.1 The full report of the scenario building workshop, with full details, references, and background, is also being published simultaneously by the Milbank Memorial Fund.2
Academic medicine today
Academic medicine might be defined as the capacity of the healthcare system to think, study, research, discover, evaluate, teach, learn, and improve. As such, little could be more important—particularly as new discoveries in science offer tremendous opportunities and emergent diseases pose huge threats. Indeed, academic medicine has been responsible for enormous gains in human health and development over the past century. Yet currently there is persistent concern that something is not right with academic medicine.3-13 At a time of increasing health burden, poverty, globalisation, and innovation, academic medicine seems to be failing to realise its potential and global social responsibility. It also seems to be becoming a less attractive career option.
ICRAM started with only two premises: it was necessary to think globally, and “more of the same” was not the answer. Reinvention was needed. This proved difficult. The members of the group often couldn't agree. They disagreed, for example, over the importance of business, particularly pharmaceutical companies, in academic medicine. Would business interests destroy or enhance academic medicine? Something was needed to break the deadlock, and we decided on scenario planning.
What are scenarios?
Scenarios are alternative ways of looking at the future. They can help test assumptions, recognise uncertainty, widen perspectives, resolve dilemmas and conflicts, deepen understanding, and explore strategic questions.2 Pioneered by Shell in the early 1970s,14 scenario planning has been used in a range of corporate, military, and non-profit company settings in both industrialised and non-industrialised countries.14-18 Recently, UNAIDS, the joint United Nations programme on HIV and AIDS, generated three possible scenarios for how the AIDS epidemic in Africa could evolve over the next 20 years based on decisions taken today.18
Composition of ICRAM
A core working party of 20 medical academics representing 14 countries
Stakeholder groups representing the areas of academia, business and industry, government and policy makers, journal editors, patients, professional associations, and students and trainees
Regional groups covering the world
A facilitating committee that helps plan and execute the ICRAM work
Scenario building works by gathering together a team who consider the instabilities in the present and the drivers of the future and who then imagine plausible but different futures. The aim is not to predict the future, which is impossible, but to enable richer conversations by stretching thinking on what the future might bring. Once the scenarios have been created they can be used to think more deeply about the present and the future. They can also be used for the basis of better short term pragmatic decision making and long term strategic planning.
ICRAM scenarios
That academic medicine is in crisis around the world seems universally agreed, but the prognosis and treatment for academic medicine are much less clear. Although we might agree that some elements of the future are predetermined—they are the inevitable consequences of events that have already taken place—many uncertainties still exist.1,2 Much of what determines the future of academic medicine is outside the control of medical academics. The world will change around them, and they will have to follow. But there will also be change that comes from within academic medicine.
The ICRAM working party, guided by facilitator Philip Hadridge, considered current global instabilities and future drivers of change and then created five scenarios of how academic medicine might look in 2025. In building scenarios, the group used a time span of 20 years, but some of the scenarios are more futuristic than others. The scenarios are summarised below and in the table.
Table 1.
Summary of scenarios
| Academic Inc | Reformation | In the public eye | Global academic partnership | Fully engaged | |
|---|---|---|---|---|---|
| Description | Academic medicine flourishes in the private sector | All teach, learn, research, and improve | Success comes from delighting patients, the public, and media | Academic medicine for global health equity | Academic medicine engages energetically with all stakeholders |
| Main features | Medical research, training, and service are commercial business activities | Academic medicine disappears | Extreme consumerism | Global cooperative networks devoted to redressing health inequalities and 10:90 gap | Strong connections among patients, policy makers, practitioners, and the public |
| Research and education integrated with health care | Patients govern academic medicine | ||||
| Continual use of media | |||||
| Medical education | Private medical schools | Teamwork | Conducted by expert patients | Centred around improving global health | Medical training is energised and community based |
| Major investment in information technology | Learning by doing | Responsiveness to patients is key value | Partnerships between medical schools in developed and developing countries | Students help drive the agenda | |
| Some niche schools (care of elderly people, rural medicine, etc) | Competency based assessment | ||||
| Research | Privatised, takes place in an array of different companies | Research and quality improvement are simultaneous | Patients determine priorities, through game shows or citizens' juries | Public health and basic science equally valued | Conducted by groups of diversely skilled individuals, including stakeholders |
| Responsive to the needs of customers | Translational research favoured | ||||
| Decision making and governance | Corporate governance | Leadership provided by societies of practitioners and patients | Bottom up: patients in charge | Global governance made up of institutional networks, policy makers, politicians, and the public | Dynamic organisations of all stakeholders to guide academic medicine |
| Disadvantages | Efficiency and effectiveness trump equity | Lacks stability because requires shared values | Advances in science and technology subject to fads and fashion | Idealistic | Academic medicine may be perceived as “dumbed down” |
| Two tier system—brain drain and 10:90 gap preserved | Decision making could be slow | Job insecurity among practitioners | Requires enormous political will and global cooperation | May lose elite status, originality, and independent thinking | |
| Innovation may suffer | Individuals sometimes could not shine | Little regulation of health information |
Scenario 1: Academic Inc
In this scenario academic medicine flourished in the private sector. Slowly but surely the public sector around the world realised that it could not support the costs of academic medicine. Medical students had high earnings during a professional lifetime: why shouldn't they pay for their education? And if researchers were doing something valuable, shouldn't they be able to find a market for their product—accepting that sometimes payment would come from the public sector? During development medical schools became private, with many providing niche training; high fees and staff salaries were introduced alongside cutting edge facilities and technology. Intense competition resulted in pressure to reduce costs and improve quality.
Research took place in a range of private companies, but many training and research companies failed. Those that succeeded were responsive to customers' needs (governments, researchers, patients). Overall, efficiency and effectiveness of academic medicine improved, but equity suffered. A two tier system resulted, the 10:90 gap persisted, and the brain drain accelerated. Accountability to shareholders often reduced innovation.
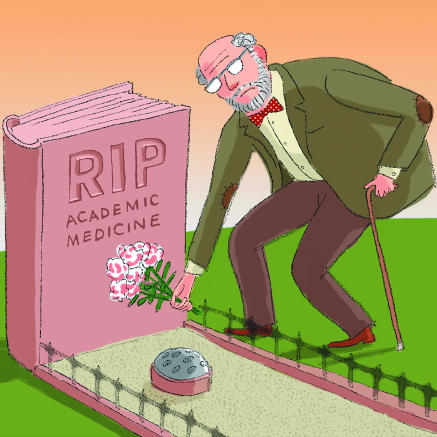
Figure 1.
Academic Inc
Scenario 2: Reformation
Concern increased about the gap between academic medicine and practice. Important research results were not being implemented, there was too much irrelevant research, students were bored, and practitioners stopped learning. The response was not to try to strengthen academic medicine but to abolish it and instead to bring the processes of teaching, learning, and researching into the mainstream of health care. This innovative—though not initially welcomed—response proved highly successful and was copied everywhere. A century of separation of academic medicine was ended. Professors disappeared. It was akin to the destruction of the monasteries and so became known as the reformation of academic medicine. The key features were:
Education, research, and quality improvement took place in the practice setting
A medical academic was no longer a jack of all trades (teacher, researcher, practitioner)
A team approach was adopted, supported by advanced learning and communication technologies
Teams comprised patients, multidisciplinary practitioners, students, and professional researchers
Research questions arose in professional-patient interactions, and a national question answering service provided evidence based responses
Leadership came from diverse specialist societies, which organised in an international academy that had influence on world leaders
Medical students first learnt how to learn, then learnt by doing
Teamwork fostered learning, but because teams did not always hold shared values stability, consensus, and decision making were threatened. The emphasis on teams also made it hard for brilliant individuals to shine as leaders.
Figure 2.
Reformation
Scenario 3: In the public eye
Academic medicine was slow to recognise the rise of global media, “celebrity culture,” and the use of public relations (or spin) to drive the political process, but once it did it responded dramatically. Whereas it had once been suspicious of the media and public appeal and rather patronising to patients, academic medicine realised that to succeed it must delight patients and the public and learn to use the media. The most successful academics became those who were responsive to patients and the public, capturing their imaginations, and appearing regularly on their television screens. Some medical academics became as well known as film and rock stars and were feted by politicians.
Academic institutions became dominated by citizens and patients, with the public relations department the most important. Grants and prizes were given on academic game and reality shows, and citizens' juries made decisions about research priorities and funding. Students received most of their training from expert patients.
The changes created great diversity in the form and size of institutions, and competition was intense for the best teachers and researchers. Academic institutions had strong links with consumer movements and local non-governmental organisations. However, academics were anxious about job security and their ability to succeed. Because scientific advances were shaped by popular appeal, they were subject to fads. In addition, there was little regulation of health information.
Scenario 4: Global academic partnership
The world began to find the growing gap between the rich and poor unacceptable. Concern was driven partly by the media and global travel bringing the plight of the poor in front of the eyes of the rich, but also driven by anxieties over global security. Terrorism was recognised to be fuelled by the obscene disparities between rich and poor. Global policy makers also understood that investment in health produced some of the richest returns in economic and social development. Health care was an essential not a bonus.
The primary concern of academic medicine became to improve global health. This global health focus offered academics intellectual stimulation and prestige. Academics championed human rights, economics, and the environment as key determinants of health, but basic science remained important because of emerging global diseases. As a result:
The G8 governments signed an accord that prohibited recruitment of academic health professionals from developing countries
Universities in the developed world committed 10% of faculty time to developing countries
North-South and South-South academic partnerships and networks flourished
The 10:90 gap narrowed rapidly
Nevertheless, the policy was idealistic and suffered because political will and global cooperation were often lacking.
Figure 3.
In the public eye
Scenario 5: Fully engaged
Academic medicine realised that its relationships with its stakeholders were mostly poor. The public had little or no understanding of what academic medicine was or why it mattered. Its very name implied irrelevance to many. Patients often felt patronised by academics, and many practitioners—including doctors—were unconvinced of the value of academic medicine. Policy makers found that academics didn't understand their problems and that the studies they produced came too late to be useful. Some leading academics did have good relationships with politicians, who recognised that biotechnology might be important in creating future wealth, but the public profile of academic medicine was both low and clouded.
Common features of all scenarios
Academic medicine will have to put more effort into relating to its stakeholders—the public, patients, practitioners, politicians, and policy makers. New institutions may have to be developed that include all these groups
Academic institutions will need to be more globally minded
Teaching, researching, improving, leading, and providing service will continue to be important, but expecting individuals to be competent in them all will be increasingly impractical
Teamwork will become more important, but it will also be necessary to allow individuals to shine and flourish
Competition among academic institutions is likely to increase, and the competition will increasingly be international
Academic institutions will need to become more business-like and more adept at using the media
Teaching and learning will be increasingly important—not least because dissatisfied students may go elsewhere. Learning will be lifelong and will depend heavily on information technology
It will be increasingly important to combine research, both basic and applied, with implementation and improvement
The range of types of academic institutions is likely to become more diverse
Academic medicine will need to be ever broader in its thinking and skill set, combining with and learning from other disciplines such as economics, law, ecology, and humanities
Thinking about the future will become increasingly important for academic institutions but also increasingly difficult
Medical academics worried that they were misunderstood, underappreciated, and seen as irrelevant. The main goal became to engage fully with the stakeholders of academic medicine—patients, practitioners, policy makers, and the public:
New organisations were created, and existing ones were reshaped, embracing openness
The media was used to interact with the public
Governance involved all stakeholders; sometimes the academy president was a prominent patient, journalist, or community leader
Medical students drove medical education rather than simply being its consumers
Although medical academics diversified and intellectual silos were breached, critics worried about the dumbing down and popularisation of academic medicine. Academic medicine had to fight to remain truly original and independent.
Lessons from the scenarios
These scenarios are tools and not ends in themselves. None of them will come to exist as they are described here, but the future is likely to contain some elements from each of them. The ICRAM working party tried to identify common features in the scenarios to learn lessons for now (box). The hope is that other groups may find the scenarios useful in thinking about both the present and the future of academic medicine. The scenarios will need to be adapted to the particular social, economic, and political conditions of different regional and national settings. The working party seeks broader thinking rather than agreement. Critical feedback is welcomed. Please send your comments through BMJ 's rapid responses and participate in our online poll.
Supplementary Material
 Members of the ICRAM working party are listed on bmj.com
Members of the ICRAM working party are listed on bmj.com
Contributors and sources: All members of ICRAM contributed to the scenarios report. JC wrote this summary.
Competing interests: JC is employed by the BMJ Publishing Group as the project manager of ICRAM.
References
- 1.Awasthi S, Beardmore J, Clark J, Hadridge P, Madani H, et al. Five futures for academic medicine. PLoS Med 2005;2(7):e207. http://medicine.plosjournals.org/perlserv/?request=get-document&doi =10.1371/journal.pmed.0020207 [DOI] [PMC free article] [PubMed]
- 2.International Campaign to Revitalise Academic Medicine. The future of academic medicine: five scenarios to 2025. New York: Milbank Memorial Fund, 2005. www.milbank.org/reports/0507FiveFutures/0507FiveFutures.html
- 3.Academic medicine: resuscitation in progress. CMAJ 2004;170: 309. [PMC free article] [PubMed] [Google Scholar]
- 4.Bhutta Z. Practising just medicine in an unjust world. BMJ 2003;327: 1000-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark J, Tugwell P. Who cares about academic medicine? BMJ 2004;329: 751-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Academy of Medical Sciences. Clinical academic medicine in jeopardy: recommendations for change. London: AMS, 2002. www.acmedsci.ac.uk/p_clinacad.pdf (accessed 18 May 2005).
- 7.Academy of Medical Sciences. Strengthening clinical research. London: AMS, 2003. www.acmedsci.ac.uk/p_scr.pdf (accessed 18 May 2005).
- 8.Forum on Academic Medicine. Clinical academic medicine: the way forward. London: Royal College of Physicians, 2004. www.rcplondon.ac.uk/pubs/books/clinacad/ClinAcadMed.pdf (accessed 18 May 2005).
- 9.Association of Academic Health Centers, Association of Canadian Medical Colleges, Nuffield Trust. The challenge to academic medicine: leading or following? London: Nuffield Trust, 2002. www.nuffieldtrust.org.uk/policy_themes/docs/academicchallenge1.pdf (accessed 18 May 2005).
- 10.Commonwealth Fund Task Force on Academic Heath Centers. Envisioning the future of academic health centers. New York: Commonwealth Fund, 2003. www.cmwf.org/usr_doc/ahc_envisioningfuture_600.pdf (accessed 18 May 2005).
- 11.Donaldson L. On the state of the public health: annual report of the chief medical officer. London: Department of Health, 2003:36-43. www.dh.gov.uk/assetRoot/04/08/68/11/04086811.pdf (accessed 21 Jun 2005).
- 12.Committee on the Roles of Academic Health Centers in the 21st Century. Academic health centers: leading change in the 21st century. Washington, DC: Institute of Medicine, 2003. www.iom.edu/Object.File/Master/13/779/0.pdf (accessed 18 May 2005).
- 13.American Association of Medical Colleges Ad Hoc Committee of Deans. Educating doctors to provide high quality medical care: a vision for medical education in the United States. Washington, DC: AAMC, 2004. https://services.aamc.org/Publications/show.le.cfm?.le=version27.pdf&prd_id=115&prv_id=130 (accessed 18 May 2005).
- 14.Davis G. Scenarios as a tool for the 21st century. Shell International, 2002. www.shell.com/static/royal-en/downloads/gd_scenarios_as_a_tool_12072002.pdf (accessed 16 Jun 2005).
- 15.Abbasi K, Butterfield M, Connor J, Delamothe T, Dutton S, Hadridge P, et al. Four futures for scientific and medical publishing. BMJ 2002;325: 1472-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Mont Fleur scenarios: what will South Africa be like in 2002? Deeper News 2000;7(1). www.arlingtoninstitute.org/future/Mont_Fleur.pdf (accessed 16 Jun 2005).
- 17.Wack P. Scenarios: uncharted waters ahead. Harvard Business Rev 1985. Sep-Oct: 139-50.
- 18.UNAIDS. AIDS in Africa: Three scenarios to 2025. Geneva: UNAIDS, 2005. http://aidsscenarios.unaids.org/scenarios/ (accessed 16 Jun 2005).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.