Abstract
Background
Heart rate variability (HRV) characterizes cardiac autonomic functioning. The association of HRV with stroke is uncertain. We examined whether 24‐hour HRV added predictive value to the Cardiovascular Health Study clinical stroke risk score (CHS‐SCORE), previously developed at the baseline examination.
Methods and Results
N=884 stroke‐free CHS participants (age 75.3±4.6), with 24‐hour Holters adequate for HRV analysis at the 1994–1995 examination, had 68 strokes over ≤8 year follow‐up (median 7.3 [interquartile range 7.1–7.6] years). The value of adding HRV to the CHS‐SCORE was assessed with stepwise Cox regression analysis. The CHS‐SCORE predicted incident stroke (HR=1.06 per unit increment, P=0.005). Two HRV parameters, decreased coefficient of variance of NN intervals (CV%, P=0.031) and decreased power law slope (SLOPE, P=0.033) also entered the model, but these did not significantly improve the c‐statistic (P=0.47). In a secondary analysis, dichotomization of CV% (LOWCV% ≤12.8%) was found to maximally stratify higher‐risk participants after adjustment for CHS‐SCORE. Similarly, dichotomizing SLOPE (LOWSLOPE <−1.4) maximally stratified higher‐risk participants. When these HRV categories were combined (eg, HIGHCV% with HIGHSLOPE), the c‐statistic for the model with the CHS‐SCORE and combined HRV categories was 0.68, significantly higher than 0.61 for the CHS‐SCORE alone (P=0.02).
Conclusions
In this sample of older adults, 2 HRV parameters, CV% and power law slope, emerged as significantly associated with incident stroke when added to a validated clinical risk score. After each parameter was dichotomized based on its optimal cut point in this sample, their composite significantly improved prediction of incident stroke during ≤8‐year follow‐up. These findings will require validation in separate, larger cohorts.
Keywords: autonomic nervous system, clinical stroke risk model, heart rate variability, prediction, predictors, risk prediction, risk stratification, stroke
Subject Categories: Cerebrovascular Disease/Stroke, Autonomic Nervous System, Electrocardiology (ECG), Electrophysiology, Arrhythmias
Clinical Perspective
What Is New?
Multiple heart rate variability (HRV) measures derived from 24‐hour Holter recordings were used to explore the association between HRV and incident stroke.
The incremental value of HRV measures to a validated clinical risk score for prediction of incident stroke was assessed for the first time.
HRV measures identified an underlying autonomic dysfunction in older individuals with apparently normal sinus rhythm that was associated with onset of stroke years later.
What Are the Clinical Implications?
HRV parameters were independently associated with incident stroke, and could potentially improve stroke risk prediction, a possibility that will require further testing in separate populations.
Early detection of underlying autonomic dysfunction using readily calculated data from an ambulatory Holter recording could prove helpful for planning interventions to prevent incidence of cerebrovascular events.
Introduction
The addition of heart rate variability (HRV) to clinical risk factors has been shown to improve prediction of cardiovascular outcomes in the CHS (Cardiovascular Health Study).1 HRV measures have also been used to gauge the effect of stroke on autonomic control of cardiac activity, and to improve prediction of poststroke outcomes.2, 3, 4, 5, 6, 7, 8, 9, 10, 11 However, the relationship of HRV with incident stroke is less clear.12, 13 We therefore examined whether 24‐hour‐Holter‐based HRV measures and/or ectopy counts would improve the predictive value of the previously validated Cardiovascular Health Study stroke risk score (CHS‐SCORE), when applied to a subset of the CHS with available 24‐hour Holter recordings.14
Methods
Study Population
Recruitment methods for the CHS have been published.15 In brief, a random sample of individuals ≥65 years of age, derived from government‐sponsored health insurance (Medicare) eligibility lists in 4 communities, as well as other biologically unrelated household members who were ≥65 years of age, were invited to participate in the study. Potential participants were excluded if they were institutionalized, unable to attend clinic visits, or had illnesses that were expected to lead to early death. N=5201 participants were recruited in 1989–1990 (original cohort). Another 687 individuals were recruited in 1992–1993 to provide additional representation of blacks (supplemental cohort). All participants signed informed consent upon entry into the study. At the time of the 1994–1995 follow‐up examination, 1196 participants underwent 24‐hour Holter monitoring. After excluding participants who had 24‐hour Holter recordings with atrial fibrillation (AF), paced rhythm, wandering atrial pacemaker or inadequate signal quality for full HRV analysis (N=120), with prevalent stroke at the 1994–1995 visit (N=72), or with missing values for covariates forming part of the CHS stroke risk model (N=9), there were 884 participants eligible for complete HRV analysis. This study conforms to the Declaration of Helsinki and was approved by the local Human Research Protection Organization.
Calculation of Stroke Risk Scores
A CHS‐SCORE was calculated for all of the participants in the 1994–1995 Holter subcohort using the CHS stroke risk model previously developed in the original and supplemental cohorts at their baseline CHS examinations (1989–1990 and 1992–1993, respectively).14 The CHS stroke risk model is shown in Table 1.14 We used clinical covariates obtained at the time of the Holter recording for calculation of the CHS‐SCORE at the 1994–1995 examination. For serum glucose and creatinine, we carried forward measures from the 1992–1993 examination, because fasting values were not available at the 1994–1995 visit.
Table 1.
The CHS Stroke Risk Model
| Risk Points | ||
|---|---|---|
| Men | Women | |
| Age, y | ||
| ≤70 | 0 | 0 |
| 71 to 77 | 3 | 5 |
| 78 to 84 | 6 | 10 |
| 85 to 91 | 9 | 15 |
| ≥92 | 12 | 20 |
| History of heart disease | 5 | 1 |
| Atrial fibrillation by ECG | 16 | 5 |
| Systolic blood pressure (mm Hg) | ||
| <120 | 0 | |
| 120 to 129 | 1 | |
| 130 to 139 | 3 | |
| 140 to 149 | 5 | |
| 150 to 159 | 7 | |
| 160 to 169 | 9 | |
| 170 to 179 | 11 | |
| >180 | 13 | |
| 15‐foot walk time | 1 per s (maximum 20) | |
| Left ventricular hypertrophy by ECG | 6 | |
| Creatinine >1.25 mg/dL | 2 | |
| Impaired fasting glucose (American Diabetes Association) | 4 | |
| Diabetes mellitus (American Diabetes Association) | 6 | |
The stroke risk at 5 years ranges from 2.5% in men and 3.5% in women with a total risk score of 1 to 5, to as high as 59% in men and 39% in women for a total risk score of 41 to 45.14 CHS indicates Cardiovascular Health Study.
Ambulatory ECG Monitoring and Assessment of HRV
Holter tapes were recorded on Del Mar Avionics devices, which have a calibrated timing signal. Data were processed by research technicians at the Washington University School of Medicine Heart Rate Variability Laboratory (St Louis, MO), using a GE Marquette MARS 8000 Holter Analyzer (GE‐Marquette, Milwaukee, WI). All Holter analyses were reviewed in detail by 1 investigator (P.K.S.), with special attention paid to ensuring that only normal beats with uniformly detected onsets were labeled as normal. The longest and shortest true normal‐to‐normal (N‐N) intervals were identified for each tape, and intervals outside of these limits, including blocked atrial premature contractions, were excluded from all HRV calculations. Participants with a paced rhythm, AF, or wandering atrial pacemaker were excluded from the analysis. Our prior analysis has shown that the demographic and clinical factors in those who volunteered for Holter recordings and the total CHS cohort were similar.16
Time domain, frequency domain, and nonlinear HRV and ectopy counts were calculated from annotated beat‐to‐beat files exported to a Sun Enterprise 450 server (Sun Microsystems, Santa Clara, CA) using validated research software. We included only participants with complete data (ie, those whose recordings fulfilled prespecified data quality criteria for all HRV analyses). These criteria comprised normal sinus rhythm with ≥18 hours of 5‐minute segments, each of which had ≥80% N‐N intervals present in each segment and <20% ectopic beats. These criteria are based on the fact that some frequency domain HRV measures are calculated per 5 minutes and averaged. For each non‐normal beat, whether because of artifact or ectopy, the interval between the normal beat before it, as well as the interval after the non‐normal beat and the next normal beat, cannot be an N‐N interval and is replaced by an average to avoid adding spurious HRV. Therefore, when 20% or more of beats are removed from a 5‐minute segment, the result is that only 40% or less of N‐N intervals are available for the calculation of HRV and that interval is excluded.
An overview of the different types of HRV measures and the information they provide is given below:
Time domain HRV provides statistical estimates of “how much” HRV there is at various time scales.17 For example, the well‐known HRV measure, standard deviation of normal‐to‐normal‐beats (SDNN), is the SD of the intervals between all of the N‐N intervals (measured in milliseconds) over the entire 24‐hour recording.
Frequency domain HRV parameters express the magnitude of the variance in the N‐N time series associated with specific bands of underlying rhythms using a fast Fourier transform.17 For example, high‐frequency power captures how much of the variance in the N‐N interval time series is explained by oscillations at frequencies consistent with respiration (in adults 9–24 cycles/min) and reflects respiratory sinus arrhythmia.
Less well‐known are the nonlinear HRV measures which, broadly speaking, capture the degree of “organization” of the N‐N interval time series and may capture prognostic information beyond that of time and frequency domain HRV.18 At 1 extreme, the heart rate pattern could be completely, mathematically random, and at the other extreme, it could be completely predictable, consisting of a single underlying oscillatory pattern. Healthy HRV falls somewhere in between these extremes. Thus, a very irregular N‐N interval time series, such as that seen in AF, would have high values for time domain HRV, would have an abnormal distribution of underlying oscillatory frequencies in the frequency domain, and would be clearly abnormally organized in the nonlinear domain.
Outcome
Incident stroke after the 1994–1995 examination was the primary outcome. Therefore, time to stroke, as recorded in the CHS database, was adjusted to capture the time to strokes occurring after the Holter recording visit. Follow‐up for incident stroke extended through 2002. At the end of follow‐up, among participants with eligible Holter recordings, there were 68 strokes of which 55 were classified as ischemic, 8 as hemorrhagic, and 5 as unknown. Ascertainment and adjudication of stroke has been previously reported.19 Briefly, potential stroke events were identified during annual follow‐up examinations and at interim 6‐month phone contacts. The participant, or his or her next of kin, was interviewed shortly after the event about the surrounding circumstances. Hospital records for all reported strokes, as well as nonstroke hospitalizations with International Classification of Diseases, 9th Revision, codes 430 through 438 identifying cerebrovascular disease, were abstracted for pertinent information and reviewed by a neurologist at each field center. Information on reported nonhospitalized stroke patients was obtained by physician questionnaire. This information was reviewed by a CHS neurologist at each field center, and any inconsistencies were reviewed with the participant's physician. Potential stroke cases were adjudicated by a committee of neurologists, neuroradiologists, and internists using information from interviews, medical records, and available cerebral imaging studies. Adjudication decisions were usually unanimous in terms of presence of stroke, stroke subtype, and stroke as a cause of death.
Statistical Analysis
Independent‐samples t tests for continuous variables and χ2 tests for categorical variables were used to determine which components of the CHS‐SCORE and which HRV parameters differed between participants with and without incident stroke. Analyses evaluated the CHS‐SCORE and HRV in relation to incident stroke primarily as continuous variables, and secondarily as categorical variables. Cox proportional hazards models were fitted to calculate the unadjusted and adjusted hazard ratios (HRs) and 95% CIs for the CHS‐SCORE and HRV measures in relation to incident stroke. The additional contribution of HRV was assessed by entering the CHS‐SCORE as a continuous variable at the first step of the stepwise forward conditional multivariate Cox regression analysis, including all nonoverlapping 24‐hour HRV and ectopy measures, significantly different between participants with and without incident stroke at the second step, and allowing the software to pick the best model (using P<0.05 for selection based on the Wald statistic). When both time domain and frequency domain parameters reflecting the same underlying autonomic rhythms (eg, total power and SDNN, which each reflect total HRV) were both different between groups, we chose the frequency domain HRV parameter as a candidate variable in the stepwise model. The c‐statistic, a measure of the accuracy of discrimination that can be thought of as an extension of the binary receiver‐operating characteristic curve to multivariable survival analysis, was calculated and compared across successive models.20 Model calibration was assessed using the Hosmer‐Lemeshow goodness‐of‐fit statistic. Statistical Package for Social Sciences, SPSS v.23 (SPSS, Inc, Chicago, IL) was used for all analyses. MedCalc software v.17.1 (www.MedCalc.org) was used to calculate the P values for the difference in c‐statistics. A 2‐sided P<0.05 was considered to be statistically significant.
Results
There were 884 CHS participants (338 men, 546 women; age 75.3±4.6 years) included in the analysis. Among the 68 participants with incident stroke, time to stroke was 3.5±2.0 years (range 0.03–7.7 years).
Table 2 compares the components of the CHS stroke risk model in participants with valid Holter recordings who did and did not suffer a stroke after the 1994–1995 visit. Notably, participants with incident strokes tended to be slightly older, and have significantly higher systolic blood pressure, but many of the specific components of the risk score were not different. However, as can be seen in the table, the CHS‐SCORE itself was significantly higher in participants with incident stroke versus those without (19.1±8.2 versus 16.1±6.9, P=0.004).
Table 2.
Comparison of Components of the CHS Stroke Risk Score Between Participants With Valid 1994–1995 Holter Recordings With and Without an Incident Stroke on Follow‐Up
| No Stroke (N=816) | Incident Stroke (N=68) | P Value | |
|---|---|---|---|
| Systolic blood pressure, mm Hg | 133±20 | 139±20 | 0.013 |
| 15‐foot walk time, s | 5.4±2.1 | 5.8±1.9 | NS |
| Left ventricular hypertrophy by ECG (Y/N) | 41 (5.0%) | 4 (5.9%) | NS |
| Creatinine, mg/dLa | 1.04±0.28 | 1.05±0.27 | NS |
| ADA diabetic statusa | 0.084 | ||
| Normal, % (<110 mg/dL) | 593 (72.7%) | 43 (63.2%) | |
| IFG, % (110–126 mg/dL) | 90 (11.0%) | 9 (13.2%) | |
| Diabetes mellitus, % (>126 mg/dL or taking meds) | 133 (16.3%) | 16 (23.5%) | |
| Age at year 7, y | 75.2±4.5 | 76.5±5.4 | 0.058 |
| Sex, % | NS | ||
| Female | 499 (61.2%) | 47 (69.1%) | |
| Male | 317 (38.8%) | 21 (30.9%) | |
| Atrial fibrillation by ECG, % | 0 | 0 | NS |
| History of heart disease at 1994–1995 visit (y 7) (Y/N) | 159 (19.5%) | 16 (23.5%) | NS |
| CHS stroke risk score | 16.1±6.9 | 19.1±8.2 | 0.004 |
ADA, American Diabetes Association; CHS, Cardiovascular Health Study; IFG, Impaired Fasting Glucose; NS, Not Significant.
Clinical factors measured at the 1994–1995 examination.
Lab values measured at the 1992–1993 examination.
CHS‐SCORE and Outcome
Consistent with the findings in the original CHS cohort at baseline, the CHS‐SCORE, when calculated at the 1994–1995 visit in the Holter subcohort, was significantly associated with incident stroke (HR=1.06 per unit increment; 95% CI 1.03–1.10, P<0.001). The c‐statistic was 0.61. There was no evidence of miscalibration (Hosmer–Lemeshow goodness‐of‐fit, P=0.628).
Association of HRV With Incident Stroke
Table 3 compares 24‐hour HRV measures between participants with and without incident stroke. Definitions for all HRV parameters are provided in the legend for Table 3. As seen in the table, although 24‐hour heart rate was not different between participants with and without incident stroke, the coefficient of variance, SDNN Index, and natural log‐transformed values for total power, ultra‐low‐frequency power, and very‐low‐frequency power were significantly lower, and power law slope (SLOPE) was significantly more negative in participants with incident stroke. Also, in an exploratory analysis, there were no significant differences in HRV parameters between participants with ischemic versus other (hemorrhagic or unknown) subtypes of stroke (P>0.21), but the sample size was too small (N=55 ischemic strokes, N=13 other or unknown) to consider this finding definitive.
Table 3.
Comparison of 24‐Hour HRV Measures and Ectopy Counts Between Participants With and Without Incident Stroke on Follow‐Up
| Time Domain HRV Variables | No Stroke (N=816) | Incident Stroke (N=68) | P Value |
|---|---|---|---|
| Heart rate, beats per min | 73.5±9.7 | 73.1±9.5 | NS |
| SDNN, ms | 115.9±34.5 | 106.9±36.6 | 0.054 |
| SDANN, ms | 105.2±33 | 97.8±36.9 | NS |
| CV, % | 13.9±3.6 | 12.8±3.9 | 0.019 |
| SDNN index, ms | 41.9±15.4 | 38.1±13.2 | 0.025 |
| RMSSD, ms | 26.1±15.9 | 24±12.5 | NS |
| Frequency domain HRV variables | |||
| ln (total power) | 4.1±0.28 | 4.0±0.29 | 0.035 |
| ln (ultra‐low‐frequency power) | 4.0±0.29 | 3.9±0.30 | 0.048 |
| ln (very‐low‐frequency power) | 2.9±0.30 | 2.8±0.33 | 0.033 |
| Normalized low‐frequency power (5‐min averages) | 59.2±11 | 57.2±10.3 | NS |
| Normalized high‐frequency power (5‐min averages) | 26.6±9.6 | 27.8±9.2 | NS |
| ln (low‐frequency power) (5‐min averages) | 2.5±0.39 | 2.4±0.41 | 0.052 |
| ln (high‐frequency power) (5‐min averages) | 2.1±0.46 | 2.0±0.42 | NS |
| Nonlinear HRV variables | |||
| Short‐term fractal scaling exponent (DFA1) | 1.13±0.21 | 1.10±0.20 | NS |
| Intermediate‐term fractal scaling exponent (DFA2) | 1.23±0.15 | 1.24±0.13 | NS |
| SD1/SD2 | 0.28±0.11 | 0.29±0.09 | NS |
| Power law slope (SLOPE) | −1.36±0.15 | −1.42±0.14 | 0.003 |
| Ectopy counts | N=816 | N=68 | |
| ln (VPC+1) | 3.7±2.3 | 4.0±2.3 | NS |
| ln (APC+1) | 4.5±1.6 | 4.5±1.4 | NS |
Time domain heart rate variability (HRV) variables: SDNN (ms)=SD of all normal‐to‐normal (N‐N) intervals; SDANN (ms)=SD of the averages of N‐N intervals for all 5‐min segments; CV (%)=average coefficient of variance of N‐Ns for 5‐min segments for 24 ; SDNN Index (ms)=mean of 5‐min SDs of all N‐N intervals for 24 h; RMSSD (ms)=square root of the mean of the squared differences between successive N‐N intervals for 24 h. Frequency domain HRV: Total Power=all of the variance in HRV; Ultra‐low‐frequency power=all variance in 24‐h HRV at frequencies of every 5 min to every 24 h, thus reflecting primarily circadian HRV; Very‐low‐frequency power=variance in HRV at underlying frequencies of every 25 s to every 5 min calculated for every 15‐min segment and averaged; Normalized low‐frequency power=the average proportion of HRV in each 5 min that is explained by oscillations at underlying frequencies of 0.04 to 0.15 Hz (the low‐frequency band) divided by the total HRV in that 5‐min period; Normalized high‐frequency power=the average amount of HRV in each 5 minutes that is explained by oscillations at underlying frequencies 0.15 to 0.4 Hz (high‐frequency or respiratory frequency band) divided by total HRV in that 5‐min period; ln (LF)=natural log of low‐frequency power. LF captures the variance in HRV at underlying frequencies of 0.04 to 0.15 Hz; ln (HF)=natural log of high‐frequency power. High frequency captures the variance in HRV at underlying frequencies of 0.18 to 0.4 Hz. Nonlinear HRV variables: DFA1=short‐term fractal scaling exponent calculated over 3 to 11 beats and averaged over 1000 beats for 24 h; DFA2=longer‐term fractal exponent calculated over 12 to 20 beats and averaged over 1000 beats for 24 h; SD12=Poincaré ratio. The Poincaré plot is a scatterplot of each N‐N interval vs the next. SD1 is the short axis of an ellipse fitted to the Poincaré plot. SD2 is the long axis of the same ellipse. SD12 (SD1/SD2) is the ratio of the short and long axes of ellipse and reflects the organization of the N‐N interval time series. SD12 was calculated for each 1000 beats and averaged; Power law slope=slope of a line fitted to a plot of log spectral power vs log of underlying frequency between 10−2 and 10−4 Hz over 24 h. Ectopy counts: ln (VPC+1)=natural log transformation of the number of premature ventricular contractions +1; ln (APC+1)=natural log transformation of the number of premature atrial contractions +1. NS indicates Not Significant.
HRV Parameters Independently Associated With Risk of Stroke
After inclusion of the continuous CHS‐SCORE, the HRV parameters, coefficient of variance (CV%) (HR=0.92, 95% CI 0.86–0.99, P=0.031) and SLOPE (HR=0.17, 95% CI 0.03–0.87, P=0.033) were retained in the multivariable Cox model. The c‐statistic for the model with the CHS SCORE and both HRV parameters added was 0.63. The change in the c‐statistic compared with the model with the CHS‐SCORE alone was not statistically significant (P=0.47). However, the association between the CHS‐SCORE and incident stroke (HR=1.05 per unit increment, 95% CI, 1.01–1.08, P=0.005) was not meaningfully attenuated by the addition of HRV parameters.
CV% and SLOPE capture completely different aspects of HRV. We therefore performed a detailed secondary analysis to further explore the relationship between decreased CV%, more negative SLOPE, and incident stroke. Clinical cut points for CV% and SLOPE have not been established. We therefore dichotomized each at the cut point that maximally separated participants with and without incident stroke after adjustment for the continuous CHS‐SCORE. For CV%, optimal risk separation occurred at a cut point of CV% ≤12.8 (LOWCV%). Among the 884 study participants, 379 had LOWCV% and 505 had CV% >12.8 (HIGHCV%). Among the participants with LOWCV%, N=43 (11.3%) had incident stroke and among the participants with HIGHCV%, N=25 (5%) had incident stroke. When categorized CV% was added to the continuous CHS‐SCORE, being in the LOWCV% group was associated with an HR=2.24 (95% CI=1.37–3.68, P=0.001) for incident stroke. The optimal risk separation for SLOPE occurred at SLOPE=−1.4. Among the 884 study participants, 350 had SLOPE <−1.4 (LOWSLOPE) and 534 had SLOPE ≥−1.4 (HIGHSLOPE). Among the participants with LOWSLOPE, N=39 (11.1%) had an incident stroke and among the participants with HIGHSLOPE, N=29 (5.4%) had an incident stroke. After adjustment for the CHS‐SCORE, being in the LOWSLOPE group was associated with HR=1.82 (95% CI=1.10–3.00, P=0.018) for incident stroke.
To explore whether having both types of abnormal HRV would be associated with an additional risk of incident stroke, we created combined categories of high‐ and low‐risk groups for CV% and SLOPE. When combined categories of HRV were added to the continuous CHS‐SCORE in the Cox model, being in the higher risk category for both HRV measures (LOWCV% and LOWSLOPE) was associated with a HR=3.5 (95% CI=1.8–6.8, P<0.001) for incident stroke compared with being in the lowest risk group for both parameters. Figure shows the incident stroke survival curves by combined categories of HRV after adjustment for the continuous CHS‐SCORE. The corresponding risk estimate for each category of combined HRV parameters compared with the reference category of HIGHCV%‐HIGHSLOPE is shown in the legend for Figure. The c‐statistic of the model with combined categories of HRV parameters adjusted for the CHS‐SCORE was 0.68 compared with the c‐statistic of 0.61 of the model with CHS‐SCORE alone (P value for the difference in c‐statistic=0.02). There was no evidence of miscalibration (Hosmer–Lemeshow goodness‐of‐fit P=0.723).
Figure 1.
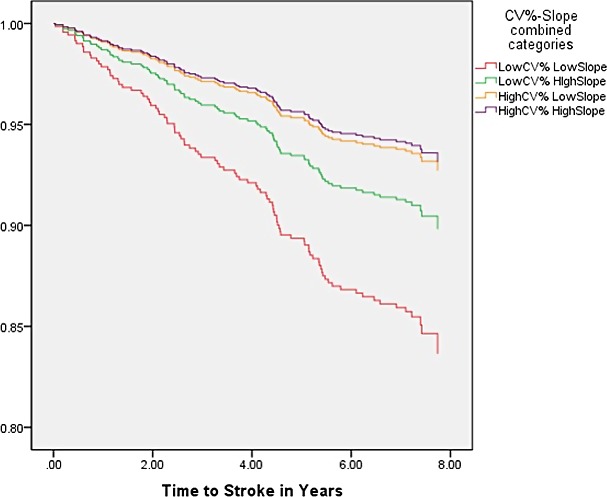
Survival curves for incident stroke based on combined categories of higher and lower coefficient of variance (CV%) and power law slope (SLOPE) after adjustment for continuous CHS‐SCORE. Reference category is HIGHCV%‐HIGHSLOPE. HIGHCV%‐LOWSLOPE: HR=1.3 (95% CI=0.6–2.8, P=0.59); LOWCV%‐HIGHSLOPE: HR=1.6 (95% CI=0.8–3.4, P=0.19); LOWCV%‐LOWSLOPE: HR=3.5 (95% CI=1.8–6.8, P<0.001) where LOWCV%=CV% ≤12.8%, HIGHCV%=CV% >12.8%, LOWSLOPE=SLOPE <−1.4, HIGHSLOPE=SLOPE ≥−1.4. CHS‐SCORE indicates Cardiovascular Health Study stroke risk score; HR, hazard ratio.
Discussion
Results of our study show that information from 24‐hour Holter monitoring is significantly associated with incident stroke among community‐dwelling older adults in normal sinus rhythm, even after calculation of their stroke risk using a validated clinical score, and could potentially improve risk stratification for incident stroke in this population. The CHS‐SCORE includes commonly assessed risk factors, namely, age, sex, systolic blood pressure, 15‐foot walk time, diabetic status, left ventricular hypertrophy on ECG, history of heart disease, and AF by ECG, the last of which was an exclusion criterion in the current study. Although having these risk factors could result in decreased HRV, abnormal HRV parameters proved independent of this composite index in this cohort late in life.
A strength of this study is that participants were well characterized and events were carefully adjudicated. Furthermore, all Holter recordings were analyzed to research standards. Findings are consistent with pre‐existing autonomic dysfunction occurring, in many cases, years before the stroke itself.
The parameter CV% was 1 of 2 HRV measures that were significantly associated with incident stroke when added to the CHS‐SCORE. CV% is defined as the mean over 24 hours of the variance of the N‐N interval time series for each 5‐minute period divided by the mean N‐N interval for that 5‐minute period, expressed as a percentage, essentially the heart rate–adjusted localized HRV. Our results suggest that decreased CV% may capture a diminished global autonomic functioning that is related to stroke risk independent of clinical measures subsumed by the CHS‐SCORE. Moreover, when CV% was dichotomized into HIGHCV% (>12.8%) and LOWCV% (≤12.8%) based on maximal discrimination of stroke risk in the current cohort—no cut point for CV% has been published previously—participants in the LOWCV% group were 2.2 times more likely to suffer a subsequent stroke than those in the HIGHCV% group, independent of their CHS‐SCORE. Because this cut point is based on the present data, it will need to be validated in other populations.
The SLOPE was the second HRV measure that demonstrated a significant association with future stroke, independent of the CHS‐SCORE. A negative number, the SLOPE reflects the distribution of the spectral characteristics of N‐N interval oscillations. It is the slope of a line fitted to a plot of log spectral power versus log of underlying frequency between 10−2 and 10−4 Hz over 24 hours. Consistent with our results, it has previously been reported that decreased SLOPE is associated with increased risk of cerebrovascular death in the elderly.21 It is possible that altered cardiovascular neural regulation, expressed by a lower value of SLOPE, is a sign of subclinical vascular disease predisposing to stroke as well as cerebrovascular death. Lower values for SLOPE may also reflect impairment in the intrinsic physiological regulatory and adaptive systems associated with aging, leading to cardiovascular and cerebrovascular events as well as death. When slope was dichotomized as <−1.40 (LOWSLOPE) and ≥−1.40 (HIGHSLOPE) to optimize discrimination in the current sample, participants in the lower category had a 1.8‐fold higher risk of incident stroke than those in the higher category. This cut point will require validation in separate cohorts.
There was an additive effect of CV% and SLOPE, wherein participants with LOWCV% and LOWSLOPE had the highest overall risk of stroke. Furthermore, in this secondary analysis, the combined categories of HRV significantly improved risk prediction when added to the CHS score. Once again, because the cut points selected for categorization of the HRV parameters were derived from our sample, future studies will need to test discriminative performance of this categorization in different populations.
We are aware of only 1 other study, by Binici et al,12 examining HRV and risk of incident stroke. This study was a population‐based cohort, the Copenhagen Holter Study, with 678 participants who had 48‐hour ambulatory ECG monitoring. Although SDNN was the HRV parameter of interest, surprisingly, SDNN as a predictor of incident stroke was measured from 2:00 to 2:15 am only and even so, it could only be evaluated in 653 participants. The investigators found a significant association between 15 minutes of nighttime HRV and stroke, and concluded that nocturnal HRV was a marker for development of stroke in healthy adults. In contrast, our study had multiple measures of HRV calculated from longer durations. Although, in theory, we could calculate SDNN between 2:00 and 2:15 am for each participant, it is unlikely that this would improve risk stratification for incident stroke.
What is also notable is the difference in the HRV risk factors associated with incident stroke compared with the HRV risk factors previously found to be associated with risk of cardiovascular mortality in the CHS.1 For example, decreased values for the short‐term fractal scaling exponent (DFA1 [a measure of the organization, ie, randomness versus predictability of the heart rate time series]) has strongly predicted cardiovascular mortality in the CHS and in other populations,1 but DFA1 was not significantly different between participants with and without incident stroke. Also, greater atrial and ventricular ectopy counts were risk markers for worse cardiovascular outcomes in the CHS,22 but no significant difference was found in the atrial or ventricular ectopy counts between those who did and did not suffer a stroke. Finally, 24‐hour averaged heart rate, another risk factor for adverse cardiovascular outcomes, was not different among the participants who did and did not suffer a stroke.
Limitations
A limitation of the current study is the modest sample size. Also, while the clinical stroke risk model can be applied to all older adults in whom the components have been measured, the HRV‐adjusted model can only be applied to people in normal sinus rhythm and with fewer than 20% ectopic beats. Recordings from participants with AF/flutter, wandering atrial pacemaker, or a paced rhythm were excluded from analysis a priori. This may account for the lack of association between atrial premature contractions counts and stroke, although an association between atrial premature contractions and AF,23 and AF and incident stroke has been previously been demonstrated in the CHS.24 Furthermore, we limited our analysis to participants with recordings adequate for 24‐hour time domain, frequency domain, and nonlinear HRV analysis. The healthier resulting subcohort may account for the difference in the c‐statistic for the CHS‐SCORE in the present study (0.61) as compared with that obtained in the original cohort of 5888 participants in whom the CHS‐SCORE was developed and validated (0.73). Given the modest discriminatory capacity of the CHS‐SCORE in our subcohort, further research is needed to determine to what extent HRV measures might improve risk prediction over optimally performing clinical scores. Also, we have evaluated the incremental predictive value of HRV parameters against the CHS score, but not against the individual components of the score itself because of the low number of events. Finally, there were not enough events to determine whether HRV would be different in participants with ischemic versus nonischemic stroke, but when the CHS stroke risk score was developed, the model predicted both types of stroke equally well.14
Future Directions
Our results support the associations of CV% and SLOPE with incident stroke independent of the CHS‐SCORE. These findings suggest that HRV might be useful for further risk stratification of older adults in relation to incident stroke, which could allow enhanced preventive approaches in this population. The present findings require separate investigation in larger cohorts to better determine the clinical value of HRV from 24‐hour Holters, including for confirmation of the primacy of the 2 HRV measures identified here, and for validation of the cut points selected. Moreover, future studies need to test the added value of HRV measures for risk stratification for incident stroke against other validated clinical risk scores, as well as the potential for HRV derived from shorter recordings to add to risk stratification. Pending confirmation, additional studies could also examine whether the efficacy of interventions that might decrease risk is reflected in improvements in HRV.
Conclusions
Among community‐dwelling older adults in the CHS, we have shown, for the first time, that HRV parameters are significantly associated with risk of incident stroke, and that a composite measure involving optimized cut points of 2 such parameters, CV% and SLOPE, improves prediction of incident stroke over a validated clinical risk score during 8 years of follow‐up. These findings will require additional investigation in larger samples and in different populations.
Sources of Funding
This work was supported in part by National Heart, Lung, and Blood Institute contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086; and National Heart, Lung, and Blood Institute grants U01HL080295, with additional contribution from the National Institute of Neurological Disorders and Stroke. Additional support was provided through R01AG023629 from the National Institute on Aging. A full list of principal CHS investigators and institutions can be found at CHS‐NHLBI.org.
Disclosures
None.
Acknowledgments
The authors express their gratitude to the CHS participants. A full list of participating CHS investigators and institutions is at https://chs-nhlbi.org.
(J Am Heart Assoc. 2017;6:e004305 DOI: 10.1161/JAHA.116.004305.)28733431
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute, the National Institutes of Health.
References
- 1. Stein PK, Barzilay JI, Chaves PH, Mistretta SQ, Domitrovich PP, Gottdiener JS, Rich MW, Kleiger RE. Novel measures of heart rate variability predict cardiovascular mortality in older adults independent of traditional cardiovascular risk factors: the Cardiovascular Health Study (CHS). J Cardiovasc Electrophysiol. 2008;19:1169–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barron SA, Rogovski Z, Hemli J. Autonomic consequences of cerebral hemisphere infarction. Stroke. 1994;25:113–116. [DOI] [PubMed] [Google Scholar]
- 3. Rardon DP, Bailey JC. Parasympathetic effects on electrophysiologic properties of cardiac ventricular tissue. J Am Coll Cardiol. 1983;2:1200–1209. [DOI] [PubMed] [Google Scholar]
- 4. Naver HK, Blomstrand C, Wallin BG. Reduced heart rate variability after right‐sided stroke. Stroke. 1996;27:247–251. [DOI] [PubMed] [Google Scholar]
- 5. Korpelainen JT, Sotaniemi KA, Mäkikallio A, Huikuri HV, Myllylä VV. Dynamic behavior of heart rate in ischemic stroke. Stroke. 1999;30:1008–1013. [DOI] [PubMed] [Google Scholar]
- 6. Colivicchi F, Bassi A, Santini M, Caltagirone C. Cardiac autonomic derangement & arrhythmias in right‐sided stroke with insular involvement. Stroke. 2004;35:2094–2098. [DOI] [PubMed] [Google Scholar]
- 7. Mäkikallio AM, Mäkikallio TH, Korpelainen JT, Sotaniemi KA, Huikuri HV, Myllylä VV. Heart rate dynamics predict poststroke mortality. Neurology. 2004;62:1822–1826. [DOI] [PubMed] [Google Scholar]
- 8. Gujjar AR, Sathyaprabha TN, Nagaraja D, Thennarasu K, Pradhan N. Heart rate variability and outcome in acute severe stroke: role of power spectral analysis. Neurocrit Care. 2004;1:347–353. [DOI] [PubMed] [Google Scholar]
- 9. Günther A, Salzmann I, Nowack S, Schwab M, Surber R, Hoyer H. Heart rate variability—a potential early marker of sub‐acute post‐stroke infections. Acta Neurol Scand. 2012;126:189–196. [DOI] [PubMed] [Google Scholar]
- 10. Graff B, Gąsecki D, Rojek A, Boutouyrie P, Nyka W, Laurent S, Narkiewicz K. Heart rate variability and functional outcome in ischemic stroke: a multiparameter approach. J Hypertens. 2013;31:1629–1636. [DOI] [PubMed] [Google Scholar]
- 11. Tang SC, Jen HI, Lin YH, Hung CS, Jou WJ, Huang PW, Shieh JS, Ho YL, Lai DM, Wu AY, Jeng JS, Chen MF. Complexity of heart rate variability predicts outcome in intensive care unit admitted patients with acute stroke. J Neurol Neurosurg Psychiatry. 2015;86:95–100. [DOI] [PubMed] [Google Scholar]
- 12. Binici Z, Mouridsen MR, Køber L, Sajadieh A. Decreased nighttime heart rate variability is associated with increased stroke risk. Stroke. 2011;42:3196–3201. [DOI] [PubMed] [Google Scholar]
- 13. Melillo P, Izzo R, Orrico A, Scala P, Attanasio M, Mirra M, De Luca N, Pecchia L. Automatic prediction of cardiovascular and cerebrovascular events using heart rate variability analysis. PLoS One. 2015;10:e0118504. eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lumley T, Kronmal RA, Cushman M, Manolio TA, Goldstein S. A stroke prediction score in the elderly: validation and Web‐based application. J Clin Epidemiol. 2002;55:129–136. [DOI] [PubMed] [Google Scholar]
- 15. Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 16. Stein PK, Barzilay JI, Domitrovich PP, Chaves PM, Gottdiener JS, Heckbert SR, Kronmal RM. Heart rate variability and its relationship to glucose disorders and metabolic syndrome: the Cardiovascular Health Study. Diabet Med. 2007;24:855–863. [DOI] [PubMed] [Google Scholar]
- 17. Huikuri HV, Stein PK. Heart rate variability in risk stratification of cardiac patients. Prog Cardiovasc Dis. 2013;56:153–159. Epub 2013 Aug 12. Review. [DOI] [PubMed] [Google Scholar]
- 18. Stein PK, Domitrovich PP, Huikuri HV, Kleiger RE; Cast Investigators . Traditional and nonlinear heart rate variability are each independently associated with mortality after myocardial infarction. J Cardiovasc Electrophysiol. 2005;16:13–20. [DOI] [PubMed] [Google Scholar]
- 19. Manolio TA, Kronmal RA, Burke GL, O'Leary DH, Price TR; for the CHS Collaborative Research Group . Short‐term predictors of incident stroke in older adults: the Cardiovascular Health Study. Stroke. 1996;27:1479–1486. [DOI] [PubMed] [Google Scholar]
- 20. Harrell E Jr, Califf R, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247:2543–2546. [PubMed] [Google Scholar]
- 21. Huikuri HV, Mäkikallio TH, Airaksinen KE, Seppänen T, Puukka P, Räihä IJ, Sourander LB. Power‐law relationship of heart rate variability as a predictor of mortality in the elderly. Circulation. 1998;97:2031–2036. [DOI] [PubMed] [Google Scholar]
- 22. Dukes JW, Dewland TA, Vittinghoff E, Mandyam MC, Heckbert SR, Siscovick DS, Stein PK, Psaty BM, Sotoodehnia N, Gottdiener JS, Marcus GM. Ventricular ectopy as a predictor of heart failure and death. J Am Coll Cardiol. 2015;66:101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dewland TA, Vittinghoff E, Mandyam MC, Heckbert SR, Siscovick DS, Stein PK, Psaty BM, Sotoodehnia N, Gottdiener JS, Marcus GM. Atrial ectopy as a predictor of incident atrial fibrillation: a cohort study. Ann Intern Med. 2013;159:721–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Prisco D, Cenci C, Silvestri E, Ciucciarelli L, Tomberli B, Tamburini C. Atrial fibrillation and its influence on stroke risk. Res Rep Clin Cardiol. 2015;6:11–15. [Google Scholar]


