Abstract
Background
Prior studies have demonstrated a link between the metabolic syndrome and increased risk of cardiovascular mortality. Whether the metabolic syndrome is associated with sudden cardiac death is uncertain.
Methods and Results
We characterized the relationship between sudden cardiac death and metabolic syndrome status among participants of the ARIC (Atherosclerosis Risk in Communities) Study (1987–2012) free of prevalent coronary heart disease or heart failure. Among 13 168 participants, 357 (2.7%) sudden cardiac deaths occurred during a median follow‐up of 23.6 years. Participants with the metabolic syndrome (n=4444) had a higher cumulative incidence of sudden cardiac death than those without it (n=8724) (4.1% versus 2.3%, P<0.001). After adjustment for participant demographics and clinical factors other than components of the metabolic syndrome, the metabolic syndrome was independently associated with sudden cardiac death (hazard ratio, 1.70, 95% confidence interval, 1.37–2.12, P<0.001). This relationship was not modified by sex (interaction P=0.10) or race (interaction P=0.62) and was mediated by the metabolic syndrome criteria components. The risk of sudden cardiac death varied according to the number of metabolic syndrome components (hazard ratio 1.31 per additional component of the metabolic syndrome, 95% confidence interval, 1.19–1.44, P<0.001). Of the 5 components, elevated blood pressure, impaired fasting glucose, and low high‐density lipoprotein were independently associated with sudden cardiac death.
Conclusions
We observed that the metabolic syndrome was associated with a significantly increased risk of sudden cardiac death irrespective of sex or race. The risk of sudden cardiac death was proportional to the number of metabolic syndrome components.
Keywords: metabolic syndrome, sudden cardiac death
Subject Categories: Epidemiology, Risk Factors, Sudden Cardiac Death
Clinical Perspective
What Is New?
In a longitudinal, population‐based sample of 13 168 residents from 4 US communities followed for a median of 23.6 years, participants with the metabolic syndrome had a 4.1% incidence of sudden cardiac death compared with 2.3% among participants without it.
The metabolic syndrome was independently associated with sudden cardiac death irrespective of sex or race.
Sudden cardiac death risk was proportional to the number of metabolic syndrome components.
What Are the Clinical Implications?
Sudden cardiac death risk associated with the metabolic syndrome may be reduced by treatment of high blood pressure, impaired glucose tolerance, and lipid levels.
Introduction
The metabolic syndrome is a clustering of metabolic and cardiovascular risk factors, including high blood pressure, dyslipidemia, elevated fasting glucose, and central adiposity. It affects approximately 1 in 3 Americans, women more so than men.1 Metabolic syndrome contributes considerably to cardiovascular mortality,2, 3, 4, 5, 6 particularly among women.7 Whether it adds incremental value to the prognostication of cardiovascular mortality beyond the constellation of factors comprising it is debated.8
Sudden cardiac death is a leading cause of death in the United States, accounting for up to 350 000 deaths annually.9 It disproportionately affects black men.10 Although a link between the metabolic syndrome and cardiovascular mortality is well established, a potential association between metabolic syndrome and sudden cardiac death has not been fully explored. Accordingly, using the ARIC (Atherosclerosis Risk in Communities) Study database, the current analysis sought (1) to determine whether the metabolic syndrome is independently associated with sudden cardiac death; (2) to assess whether sex or race modify this relationship; and (3) to characterize the association between sudden cardiac death and the metabolic syndrome criteria components individually and cumulatively.
Methods
Data Sources
The ARIC study prospectively enrolled 15 792 predominantly black and white men and women from 1987 to 1989 using population‐based probability sampling from residents of 4 US communities: Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and the northwestern suburbs of Minneapolis, Minnesota.11 Follow‐up examinations were conducted every 3 years on average over the first decade. Since that time, further follow‐up has entailed annual telephone interviews and active surveillance of the ARIC community hospitals.
Baseline assessment consisted of a clinic visit, during which trained staff conducted extensive physical examinations of study participants and risk factor assessment. Waist circumference was measured at the umbilical level. Systolic and diastolic blood pressure were measured 3 times with participant in a seated position and after 5 minutes of rest. The average of the second and third measurements was taken as the blood pressure measurement. Participants were asked to fast 12 hours before a blood draw. Actual fasting times were recorded. Blood was drawn from an antecubital vein into tubes containing EDTA at each clinical visit following a minimum of 8 hours of fasting. Plasma was separated by centrifugation at 4°C and aliquots were stored at −70°C until analysis. Glucose was measured by the hexokinase/glucose‐6 phosphate dehydrogenase method. High‐density lipoprotein‐cholesterol (HDL‐C) levels were measured using the method of Warnick et al.12 Low‐density lipoprotein was calculated using the Friedewald formula.13 Triglycerides were measured with enzymatic methods. Medication use was assessed at the time of baseline visit from participants’ self‐report.
The ARIC protocols were approved by the institutional review board at each participating center, and informed consent was obtained from each study participant. A de‐identified data set of relevant variables was transferred from the ARIC Coordinating Center at the University of North Carolina at Chapel Hill, North Carolina, to the Duke Clinical Research Institute in Durham, North Carolina, for analysis. Use of the data set achieved exempt status from the Duke Institutional Review Board.
Definition of the Metabolic Syndrome
The definition of the metabolic syndrome used in the current analysis was established in 2009 by the International Diabetes Federation Task Force on Epidemiology and Prevention; the National Heart, Lung, and Blood Institute; the American Heart Association; the World Heart Federation; the International Atherosclerosis Society; and the International Association for the Study of Obesity.14 In brief, a participant was classified as having the metabolic syndrome if 3 or more of the following individual components were present: waist circumference ≥35 inches (88 cm) for women or ≥40 inches (102 cm) for men; fasting blood glucose ≥100 mg/dL (5.5 mmol/L) or treatment with hypoglycemic agents or insulin; systolic blood pressure ≥130 or diastolic blood pressure ≥85 mm Hg or antihypertensive drug treatment; serum triglycerides ≥150 mg/dL (1.7 mmol/L) or treatment for hypertriglyceridemia (with niacin or fibrates); and HDL‐C<40 mg/dL (1.0 mmol/L) in men or <50 mg/dL (1.3 mmol/L) in women.
Adjudication of Sudden Cardiac Death
Sudden cardiac death was defined as a sudden pulseless condition presumed attributable to a ventricular tachyarrhythmia in a previously stable individual without evidence of a noncardiac cause of cardiac arrest. All cardiac arrest events occurred out of the hospital or in the emergency room.15 A committee of electrophysiologists, general cardiologists, and internists reviewed and adjudicated cases of fatal cardiovascular death in 2 phases. In the first phase, 5 physicians adjudicated cardiovascular deaths occurring on or before December 31, 2001. In the second phase, a committee of 11 physicians adjudicated cardiovascular deaths occurring between January 1, 2002, and December 31, 2012. Deaths were classified with the use of death certificates, informant interviews, physician questionnaires, coroner reports, prior medical history as recorded in the ARIC database, hospital discharge summaries, and circumstances surrounding the event.
Study Cohort
Study participants with prevalent cardiovascular heart disease, defined as self‐reported myocardial infarction, heart or vascular surgery, coronary bypass, coronary angioplasty, ECG evidence of myocardial infarction, or angina diagnosed by Rose questionnaire16 (n=1110), or prevalent heart failure (n=1039) at baseline were excluded. Participants with a race other than black or white (n=48) or those reporting black race in Minnesota or Maryland (n=55) were also excluded. Participants with missing data on any component of the metabolic syndrome (n=281), whose fasting status was not determined, or who did not fast at least 8 hours before the blood draw (n=592) were excluded as well. A total of 2624 unique patients were excluded from the analysis.
Statistical Analysis
Baseline characteristics of the study population were stratified by the presence or absence of the metabolic syndrome as well as by study center. Continuous variables are presented as medians with 25th to 75th percentile ranges, while categorical variables are presented as counts. Potential between‐group differences for continuous variables were assessed using the Kruskal–Wallis test or ANOVA as appropriate. Categorical variables were compared using Pearson's χ2 test or Fisher exact test in instances of low frequencies. Cumulative estimates of the risk of sudden cardiac death among participants with metabolic syndrome and those without metabolic syndrome were constructed. A potential between‐group difference was assessed using Gray's K‐sample test.
We used Cox proportional hazards modeling to assess whether the metabolic syndrome was associated with the risk of sudden cardiac death. Cox proportional hazards model assumption was tested and the proportionality was met. Unadjusted and adjusted hazard ratio (HR) estimates for metabolic syndrome were then derived from models stratified by field center. Potential confounders not included in the definition of the metabolic syndrome were identified by means of backward selection using an α level of 0.15 and included age, sex, race, heart rate, smoking status, left ventricular hypertrophy identified by the Cornell electrocardiographic criteria, use of a calcium channel blocker, magnesium, and use of angiotensin‐converting enzyme inhibitors. In view of their potential clinical relevance, β‐blockers and antiarrhythmic medications were retained in the models irrespective of statistical significance. To assess whether the association of metabolic syndrome with sudden cardiac death differs among subgroups, the multiplicative interaction terms of metabolic syndrome by sex and metabolic syndrome by race were evaluated in sequential models. The HRs of sudden cardiac death associated with the individual components of the metabolic syndrome were then assessed in separate Cox models adjusted for these risk factors. To evaluate whether the construct of the metabolic syndrome provides prognostic value above its components, a model including an indicator of the metabolic syndrome as well the individual components of the metabolic syndrome was fitted. The shape and relationship of the number of metabolic syndrome components as a continuous variable was fitted using a restricted‐cubic spline plot. The Cox model linearity assumption was assessed with Wald χ2 plotted against the log (HR). Analyses were performed with SAS, release 9.4 (SAS Institute Inc, Cary, NC).
Results
Among 13 168 participants free of coronary heart disease or heart failure at baseline, 4444 were classified as having metabolic syndrome. Compared with participants who did not have the metabolic syndrome, those with metabolic syndrome were older and more often female and black. They more frequently had diabetes mellitus and a higher body mass index and more commonly were taking β‐blockers and angiotensin‐converting enzyme inhibitors (Table 1). Baseline characteristics varied according to field center (Table S1).
Table 1.
Baseline Participant Characteristics Stratified by Metabolic Syndrome Status
| Characteristic | Total (N=13 168) | With Metabolic Syndrome (N=4444) | Without Metabolic Syndrome (N=8724) | P Value |
|---|---|---|---|---|
| Age, y | 54 (49, 59) | 55 (50, 60) | 53 (49, 58) | <0.001 |
| Female sex, % | 56.0 | 56.5 | 55.7 | 0.392 |
| Race, % | 0.006 | |||
| Black | 24.8 | 26.3 | 24.1 | |
| White | 75.2 | 73.7 | 75.9 | |
| Metabolic syndrome components | ||||
| Waist circumference, in | 96.0 (87.0, 104.0) | 104.0 (97.0, 112.0) | 91.0 (84.0, 99.0) | <0.001 |
| Fasting blood glucose, mmol/L | 5.5 (5.1, 5.9) | 5.9 (5.6, 6.6) | 5.3 (5.1, 5.6) | <0.001 |
| Systolic blood pressure, mm Hg | 118 (108, 131) | 128 (116, 140) | 115 (105, 125) | <0.001 |
| Diastolic blood pressure, mm Hg | 73 (66, 80) | 77 (70, 84) | 71 (65, 78) | <0.001 |
| Serum triglycerides mmol/L | 1.2 (0.9, 1.7) | 1.8 (1.3, 2.4) | 1.0 (0.8, 1.3) | <0.001 |
| HDL mmol/L | 1.3 (1.0, 1.6) | 1.0 (0.9, 1.2) | 1.4 (1.2, 1.7) | <0.001 |
| Comorbidities, % | ||||
| Atrial fibrillation | 0.1 | 0.2 | 0.1 | 0.289 |
| Diabetes mellitus | 7.5 | 16.5 | 2.8 | <0.001 |
| Current smoker | 25.2 | 24.7 | 25.5 | 0.339 |
| Laboratory values | ||||
| Sodium | 141.0 (139.0, 142.0) | 141.0 (140.0, 143.0) | 141.0 (139.0, 142.0) | <0.001 |
| Potassium | 4.4 (4.1, 4.7) | 4.4 (4.1, 4.7) | 4.4 (4.1, 4.8) | <0.001 |
| Creatinine | 1.1 (1.0, 1.2) | 1.1 (1.0, 1.2) | 1.1 (1.0, 1.2) | 0.002 |
| Magnesium | 1.6 (1.5, 1.7) | 1.6 (1.5, 1.7) | 1.7 (1.6, 1.7) | <0.001 |
| Body mass index | 26.7 (23.9, 30.2) | 29.8 (27.0, 33.0) | 25.4 (22.9, 28.0) | <0.001 |
| Left ventricular hypertrophy by Cornell criteria, % | 1.9 | 2.8 | 1.4 | <0.001 |
| Resting heart rate | 66 (60, 73) | 68 (61, 75) | 65 (59, 71) | <0.001 |
| Medications, % | ||||
| β‐Blockers | 4.2 | 7.2 | 2.6 | <0.001 |
| Angiotensin‐converting enzyme inhibitors | 2.6 | 4.1 | 1.8 | <0.001 |
| Antiarrhythmic drugs | 0.4 | 0.4 | 0.4 | 0.900 |
Data are based on participants with available data for each characteristic. Values are presented as medians with 25th and 75th percentiles unless otherwise indicated. HDL indicates high‐density lipoprotein.
During a median follow‐up of 23.6 years, we observed 357 sudden cardiac deaths. Participants with the metabolic syndrome had a higher cumulative incidence of sudden cardiac death than those without it (4.1% versus 2.3%, P<0.001, Figure 1). The metabolic syndrome was independently associated with sudden cardiac death in an unadjusted model (HR, 1.93, 95% CI, 1.56–2.37, P<0.001) and in a multivariable model (HR, 1.70; 95% CI, 1.37–2.12; P<0.001). This relationship was not modified by sex (HR, 1.48; 95% CI, 1.12–1.95 for males; HR, 2.13; 95% CI, 1.51–3.02 for females, interaction P=0.10) or race (interaction P=0.62). The risk of sudden cardiac death in association with the number of metabolic syndrome components was fitted using restricted cubic‐spline in the Cox model and has been shown to be linear (Wald χ2 P=0.25). We observed an increased risk of sudden cardiac death for every unit increase in the number of metabolic syndrome components compared with none (HR, 1.31; 95% confidence interval [CI], 1.19–1.44; P<0.001). The risk of sudden cardiac death varied according to the number of components (Figure 2). After adjustment for the individual components of the metabolic syndrome, the composite metabolic syndrome construct was not independently associated with the risk of sudden cardiac death (HR, 1.01; 95% CI, 0.68–1.50; P=0.95). Of the 5 metabolic syndrome components, elevated blood pressure (HR, 1.81; 95% CI, 1.45–2.27; P<0.001), impaired fasting glucose (HR, 1.35; 95% CI, 1.08–1.70; P=0.009), and low HDL‐C (HR, 1.27; 95% CI, 1.01–1.60; P=0.043) were independently associated with the risk of sudden cardiac death. Elevated blood pressure was the largest risk contributor with a Wald χ2 of 26.7 (Table 2).
Figure 1.
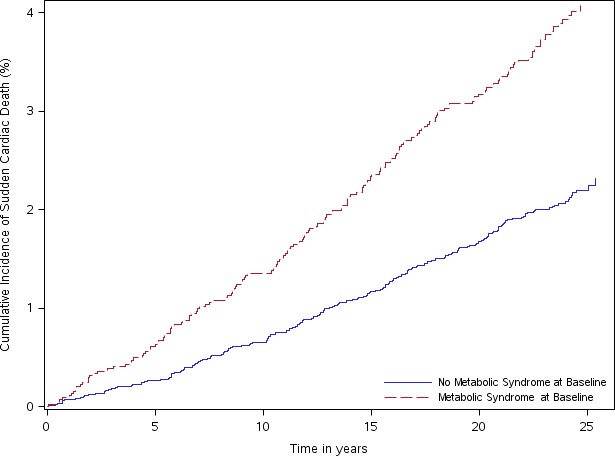
Cumulative incidence of sudden cardiac death by metabolic syndrome status at baseline. The ARIC Study Cohort 1987 to 2012. The incidence of sudden cardiac death was higher among patients with the metabolic syndrome compared with patients without the metabolic syndrome early in the study period, and the curves continued to separate over time. ARIC indicates Atherosclerosis Risk in Communities.
Figure 2.
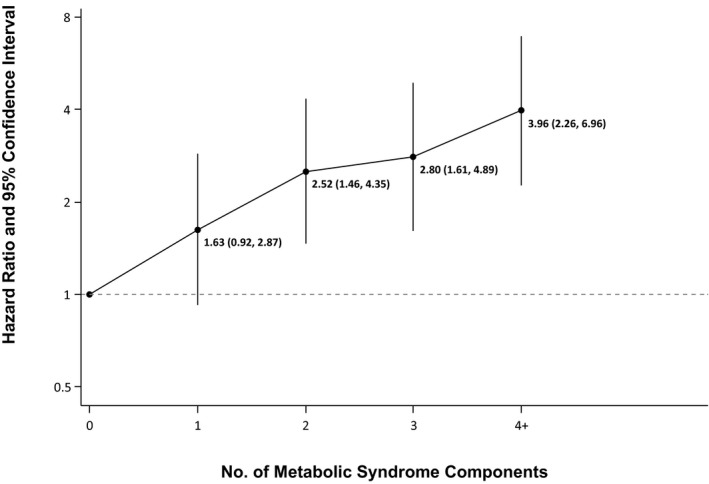
Risk of sudden cardiac death according to the number of metabolic syndrome criteria. The ARIC Study Cohort 1987 to 2012. Sudden cardiac death risk varied according to the number of metabolic syndrome components. Risk estimates were adjusted for age, sex, race, heart rate, smoking status, left ventricular hypertrophy, use of calcium channel blockers, use of β‐blockers, and use of antiarrhythmic medications. ARIC indicates Atherosclerosis Risk in Communities.
Table 2.
Associations of Metabolic Syndrome Components With the Risk of Sudden Cardiac Death. The ARIC Study Cohort 1987 to 2012
| Metabolic Syndrome Component | Wald χ2 | Hazard Ratio | 95% CI | P Value |
|---|---|---|---|---|
| Blood pressure ≥130/85 mm Hg or antihypertensive drug treatment | 26.73 | 1.81 | 1.45 to 2.27 | <0.001 |
| Fasting blood glucose ≥100 mg/dL or treatment with hypoglycemic agents or insulin | 6.89 | 1.35 | 1.08 to 1.70 | 0.009 |
| HDL‐C<40 mg/dL in men or <50 mg/dL in women | 4.11 | 1.27 | 1.01 to 1.60 | 0.043 |
| Waist circumference ≥35 in for women or ≥40 in for men | 3.40 | 1.25 | 0.99 to 1.58 | 0.065 |
| Triglycerides ≥150 mg/dL or treatment for hypertriglyceridemia | 0.09 | 0.96 | 0.75 to 1.24 | 0.766 |
ARIC indicates Atherosclerosis Risk in Communities; CI, confidence interval; HDL‐C, high‐density lipoprotein cholesterol.
Discussion
The current analysis has 4 main findings. First, after accounting for participant demographic and clinical factors other than the components of the metabolic syndrome, we observed that the metabolic syndrome was associated with an ≈70% increased risk of sudden cardiac death. Second, this relationship was not modified by either sex or race. Third, the association between metabolic syndrome and sudden cardiac death was mediated by criteria components rather than the construct per se. Finally, the risk of sudden cardiac death varied according to the number of metabolic syndrome components, most importantly blood pressure, impaired fasting glucose, and low HDL.
A large body of evidence suggests that individuals with metabolic syndrome are at increased risk of cardiovascular events and death.7 Systolic blood pressure, diabetes mellitus, and HDL level are in fact integral to a global assessment of sudden cardiac death risk.17 However, to our knowledge, only 1 prior study has examined a potential association between the metabolic syndrome and the risk of sudden cardiac death. In a cohort of 6678 French men, 963 had the metabolic syndrome at baseline. During a median follow‐up of 21 years, 105 sudden cardiac deaths occurred. After multivariable adjustment, the authors found that metabolic syndrome was associated with a 68% increase in risk of sudden death (95% CI, 1.05–2.70).18 In comparison, the current analysis has a larger sample size and a greater number of sudden cardiac deaths. It confirms an association between the metabolic syndrome and sudden cardiac death of a similar magnitude and extends the finding to a population‐based cohort of Americans. It further characterizes the relationship with regard to sex and race and deepens our understanding of the prognostic importance of the individual metabolic syndrome components as well as their number.
Prior studies suggest that the association between the metabolic syndrome and cardiovascular events is stronger among women.7 Nonetheless, sudden cardiac death occurs more often among black men.10 That sex or race/ethnicity may modify the association between the metabolic syndrome and sudden cardiac death is plausible. However, the findings of the current analysis suggest that neither is prognostically important. Rather, the comparatively high rate of sudden cardiac death observed among black men is likely mediated by high blood pressure, which affects them disproportionately.19
A graded relationship between the number of cardiovascular risk factors has previously been observed with regard to the risk of cardiovascular events,20 including incident stroke,21 coronary heart disease,22 and atrial fibrillation.23 To our knowledge, the current analysis is the first to examine the relative contribution of the number of components of the metabolic syndrome in reference to sudden cardiac death. A graded relationship between the number of metabolic syndrome components and outcome was again observed.
The prognostic utility of the metabolic syndrome construct has previously been called into question.24 Initial studies adjusting for traditional cardiovascular risk factors suggested that the metabolic syndrome construct carries prognostic weight.7, 25, 26 More recent studies accounting for the actual components of the metabolic syndrome imply that the metabolic syndrome construct does not add explanatory power beyond that afforded by its components.27 The current analysis supports the latter notion with regard to sudden cardiac death.
How to best treat patients with metabolic syndrome is often unclear, and data informing clinical practice are lacking with rare exception.28 However, the therapeutic and public health implications of the current analysis are of interest. The risk of sudden cardiac death associated with metabolic syndrome may in part be reduced by treatment of high blood pressure, impaired glucose tolerance, and lipid levels. Hence, treatment of cardiovascular risk factors should be undertaken when possible.
Limitations
The current analysis has several limitations. First, change in therapy over time may impact the relationship between the metabolic syndrome and sudden cardiac death, but such information was not available for analysis. Second, the ARIC cohort included predominantly white and black participants. Consequently, our findings may not be generalizable to other racial groups. Third, given the observational nature of the analysis, residual or unmeasured confounding may exist. Fourth, while a comparison of the influence of metabolic syndrome on sudden cardiac death versus nonsudden cardiac death would be informative, data on nonsudden cardiac death were not available in the limited data set. Finally, left ventricular ejection fraction, which is the mainstay of assessing sudden cardiac death risk from a clinical perspective, was not included in the current analysis. However, most sudden cardiac deaths occur among those without known heart disease,29 as was the case with our study cohort at baseline.
Conclusions
In this analysis, the metabolic syndrome was independently associated with a 70% increase in the risk of sudden cardiac death. This relationship did not vary by sex or race and was mediated by criteria components of the composite metabolic syndrome construct. A graded relationship between the number of metabolic syndrome components and sudden cardiac death risk was observed. High blood pressure, impaired fasting glucose, and low HDL were the principal drivers of the observed increase in the risk of sudden cardiac death. Whether treating these conditions reduces the risk of sudden cardiac death is unknown and requires further study.
Sources of Funding
D.J.F. was funded by the National Institutes of Health T 32 training grant HL069749‐13. The ARIC study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). Sudden cardiac death adjudication was supported by National Heart, Lung, and Blood Institute contract HL111089.
Disclosures
D.J.F. has received educational grants from Boston Scientific and St. Jude, and research grants from the National Cardiovascular Data Registry and Boston Scientific. The remaining authors have no disclosures to report.
Supporting information
Table S1. Baseline Participant Characteristics Stratified by Field Center
Acknowledgments
We would like to thank the staff and participants of the ARIC study for their important contributions. We also would like to acknowledge the sudden cardiac death mortality classification committee members: Nona Sotoodehnia (lead), Selcuk Adabag, Sunil Agarwal, Lin Chen, Raj Deo, Leonard Ilkhanoff, Liviu Klein, Saman Nazarian, Ashleigh Owen, Kris Patton, and Larisa Tereschchenko.
(J Am Heart Assoc. 2017;6:e006103 DOI: 10.1161/JAHA.117.006103.)28835363
References
- 1. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003‐2012. JAMA. 2015;313:1973–1974. [DOI] [PubMed] [Google Scholar]
- 2. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle‐aged men. JAMA. 2002;288:2709–2716. [DOI] [PubMed] [Google Scholar]
- 3. Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR, Williams GR. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:1245–1250. [DOI] [PubMed] [Google Scholar]
- 4. Wang J, Ruotsalainen S, Moilanen L, Lepisto P, Laakso M, Kuusisto J. The metabolic syndrome predicts cardiovascular mortality: a 13‐year follow‐up study in elderly non‐diabetic Finns. Eur Heart J. 2007;28:857–864. [DOI] [PubMed] [Google Scholar]
- 5. Mozaffarian D, Kamineni A, Prineas RJ, Siscovick DS. Metabolic syndrome and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2008;168:969–978. [DOI] [PubMed] [Google Scholar]
- 6. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, Rinfret S, Schiffrin EL, Eisenberg MJ. The metabolic syndrome and cardiovascular risk a systematic review and meta‐analysis. J Am Coll Cardiol. 2010;56:1113–1132. [DOI] [PubMed] [Google Scholar]
- 7. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta‐analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. [DOI] [PubMed] [Google Scholar]
- 8. Tikhonoff V, Casiglia E. Metabolic syndrome: nothing more than a constellation? Eur Heart J. 2007;28:780–781. [DOI] [PubMed] [Google Scholar]
- 9. Kong MH, Fonarow GC, Peterson ED, Curtis AB, Hernandez AF, Sanders GD, Thomas KL, Hayes DL, Al‐Khatib SM. Systematic review of the incidence of sudden cardiac death in the United States. J Am Coll Cardiol. 2011;57:794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. [DOI] [PubMed] [Google Scholar]
- 11. The ARIC investigators . The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 12. Warnick GR, Benderson J, Albers JJ. Dextran sulfate‐Mg2+ precipitation procedure for quantitation of high‐density‐lipoprotein cholesterol. Clin Chem. 1982;28:1379–1388. [PubMed] [Google Scholar]
- 13. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the density of low‐density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 14. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. [DOI] [PubMed] [Google Scholar]
- 15. White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–233. [DOI] [PubMed] [Google Scholar]
- 16. Rose GA, Blackburn H, Gilllum RF. Cardiovascular Survey Methods. 2nd ed World Health Organization ‐ Monograph Series; Geneva, Switzerland; 1982. [PubMed] [Google Scholar]
- 17. Deo R, Norby FL, Katz R, Sotoodehnia N, Adabag S, DeFilippi CR, Kestenbaum B, Chen LY, Heckbert SR, Folsom AR, Kronmal RA, Konety S, Patton KK, Siscovick D, Shlipak MG, Alonso A. Development and validation of a sudden cardiac death prediction model for the general population. Circulation. 2016;134:806–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Empana JP, Duciemetiere P, Balkau B, Jouven X. Contribution of the metabolic syndrome to sudden death risk in asymptomatic men: the Paris Prospective Study I. Eur Heart J. 2007;28:1149–1154. [DOI] [PubMed] [Google Scholar]
- 19. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 20. Ridker PM, Buring JE, Cook NR, Rifai N. C‐reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8‐year follow‐up of 14 719 initially healthy American women. Circulation. 2003;107:391–397. [DOI] [PubMed] [Google Scholar]
- 21. Rodriguez‐Colon SM, Mo J, Duan Y, Liu J, Caulfield JE, Jin X, Liao D. Metabolic syndrome clusters and the risk of incident stroke: the atherosclerosis risk in communities (ARIC) study. Stroke. 2009;40:200–205. [DOI] [PubMed] [Google Scholar]
- 22. Schmiegelow MD, Hedlin H, Mackey RH, Martin LW, Vitolins MZ, Stefanick ML , Perez MV, Allison M, Hlatky MA. Race and ethnicity, obesity, metabolic health, and risk of cardiovascular disease in postmenopausal women. J Am Heart Assoc. 2015;4:e001695 DOI: 10.1161/JAHA.114.001695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chamberlain AM, Agarwal SK, Ambrose M, Folsom AR, Soliman EZ, Alonso A. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2010;159:850–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28:2289–2304. [DOI] [PubMed] [Google Scholar]
- 25. Sattar N, Gaw A, Scherbakova O, Ford I, O'Reilly DS, Haffner SM, Isles C, Macfarlane PW, Packard CJ, Cobbe SM, Shepherd J. Metabolic syndrome with and without C‐reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003;108:414–419. [DOI] [PubMed] [Google Scholar]
- 26. Schillaci G, Pirro M, Vaudo G, Gemelli F, Marchesi S, Porcellati C, Mannarino E. Prognostic value of the metabolic syndrome in essential hypertension. J Am Coll Cardiol. 2004;43:1817–1822. [DOI] [PubMed] [Google Scholar]
- 27. McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11‐year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28:385–390. [DOI] [PubMed] [Google Scholar]
- 28. Pyorala K, Ballantyne CM, Gumbiner B, Lee MW, Shah A, Davies MJ, Mitchel YB, Pedersen TR, Kjekshus J; Scandinavian Simvastatin Survival Study(4S) . Reduction of cardiovascular events by simvastatin in nondiabetic coronary heart disease patients with and without the metabolic syndrome: subgroup analyses of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care. 2004;27:1735–1740. [DOI] [PubMed] [Google Scholar]
- 29. Wellens HJ, Schwartz PJ, Lindemans FW, Buxton AE, Goldberger JJ, Hohnloser SH, Huikuri HV, Kaab S, La Rovere MT, Malik M, Myerburg RJ, Simoons ML, Swedberg K, Tijssen J, Voors AA, Wilde AA. Risk stratification for sudden cardiac death: current status and challenges for the future. Eur Heart J. 2014;35:1642–1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline Participant Characteristics Stratified by Field Center


