Abstract
Objective
The purpose of this study was to determine the prevalence, height, location and morphology of maxillary sinus septa in dentate, partially dentate and edentulous adults as well as in mixed dentition children using cone beam computed tomography (CBCT) for maxillary sinus surgical interventions.
Subjects and Methods
Five hundred and fifty-four sides in the CBCT scans of 272 patients (30 children and 242 adults) were retrospectively analyzed. The prevalence, location and morphology were assessed in axial, sagittal, cross-sectional and panoramic 3-dimensional images. The height of septa was measured with the angle between the direction of the septum and median palatine suture. The differences among age, localization and measurements were statistically analyzed.
Results
The prevalence of maxillary sinus segments with septa was 58%. There were a total of 13 (3.2%) septa of completely edentulous (CE), 198 (53.9%) septa of edentate and 14 (3.8%) septa of the mixed dentition maxillary segments. The location of septa observed in all study groups demonstrated a greater prevalence (69.1%) in the middle region than in the anterior and posterior regions. No statistically significant differences were observed with regard to gender or age, for septum height (p > 0.05). However, maxillary sinus septa are higher in partially edentulous patients than edentate and CE ones (p < 0.05).
Conclusion
Septa of various heights and courses developed in all parts of the maxillary sinus, therefore to prevent possible complications during sinus surgery, extensive evaluation with an appropriate radiographic technique was indispensable.
Key Words: Maxillary sinus septa, Cone beam computed tomography, Maxillary sinus surgery, Dental implants
Introduction
The maxillary sinus in the adult consists of a pyramid-shaped cavity in the facial skull with its base at the lateral nasal wall and its apex extending into the zygomatic process of the maxilla [1]. The proximity of the maxillary sinus to the alveolar crest can be enhanced by sinus pneumatization, as well as resorption of the alveolar ridge due to tooth extraction, trauma or pathology. At the edentate stage of life, the size of the maxillary sinus increases further, often filling a large part of the alveolar process, leaving sometimes only a paper-thin bone wall on the lateral and occlusal sides. This process of pneumatization of the sinus varies greatly from person to person and even from side to side [2].
All the surgical interventions, such as endoscopic sinus surgery and sinus lift surgery, in the posterior maxillary region require detailed knowledge of maxillary sinus anatomy and possible anatomical variations. Detailed knowledge of the patient's morphological conditions allows exact planning of invasive surgery and helps to avoid complications [3,4,5,6,7,8,9]. The presence of anatomical variations within the maxillary sinus, such as septa, has been reported to increase the risk of sinus membrane perforation during the surgical sinus elevation procedure [6,10,11,12]. Maxillary sinus septa were first described by Underwood [13] in 1910 as the walls of cortical bone within the maxillary sinus; the shape has been described as an inverted gothic arch arising from the inferior or lateral walls of the sinus, and may even divide the sinus into two or more cavities. The etiology of antral septa has been the subject of several hypotheses by various authors [6,7,14,15]. Krennmair et al. [7] further classified the septa into primary and secondary septa, with the primary septa arising from the development of the maxilla, whereas the secondary septa were said to arise from the irregular pneumatization of the sinus floor following tooth loss. Evaluation of the anatomical structures inherent to the maxillary sinus is crucial for the success of sinus surgical procedures. Therefore, an exact and definitive radiological assessment is necessary [4,16]. Dental panoramic radiography, computed tomography (CT) and cone beam computed tomography (CBCT) have all been used to identify the maxillary sinus septa [4,5,6,7,8,9,14,15,16,17,18]. CBCT is a technique that has been proposed for maxillofacial imaging during the last decade and was first reported on in the literature by Mozzo et al. [19]. In the last decade, CBCT has been recommended as an excellent, low-cost tool for the evaluation of these anatomical structures with only slightly more radiation than panoramic radiography and far less than a CT scan [20,21,22,23].
Despite various studies which were conducted on height, prevalence and morphology of the maxillary sinus septa in adult patients, only very few studies [24,25] were found for populations of children. Moreover, no study was conducted in our population especially in the mixed dentition stage. Hence, it was considered worthwhile to determine the prevalence, height, location and morphology of maxillary sinus septa in dentate, partially dentate and edentulous adults as well as in mixed dentition children and adolescents using CBCT.
Subjects and Methods
The study was based on a retrospective evaluation of CBCT scans of 272 subjects (152 females, 120 males). In adult patients, CBCTs were taken for dental implant surgery, impacted third molar surgery or various cystic surgical operations in jaws while in children CBCTs were taken for the evaluation of impacted teeth and various cystic changes around impacted teeth. Our study population consisted of children in the mixed dentition stage (30 patients) and adult patients (242 patients).
The age range of the adult population was 17–83 years whereas that of the children was 6–10 years. Each right and left maxillary sinus was defined as segment. A total of 544 maxillary sinus segments were evaluated with CBCT.
The patient consent forms were prepared according to the principles of the Helsinki Declaration, including all amendments and revisions. The Institutional Review Board and the Ethics Committee reviewed and approved the informed consent form. Informed consent forms showed that the radiographs could be used for scientific studies. The consent forms were signed by the patients or their legal guardians. Subjects with evidence of current orthodontic treatment for erupted or supernumerary teeth overlying maxillary sinus septa or bone disease were excluded from the study.
CBCT scans were obtained using a Newtom 3G (Quantitative Radiology s.r.l., Verona, Italy). All images were recorded at 120 kVP and 3–5 mA using a 9-inch field of view, an axial slice thickness of 0.3 mm and isotropic voxels. The evaluations of maxillary sinus septum morphology, location and prevalence were done in axial, sagittal, cross-sectional and reconstructed panoramic images while 3-dimensional reconstructions were used as necessary (fig. 1). To avoid any errors in the localization of septa, the multiplanar reconstruction technique was used. Each maxillary sinus bearing a septum was divided into three portions: anterior = mesial to distal aspect of second premolar; middle = distal aspect of second premolar to distal aspect of second molar, and posterior = distal aspect of second molar. All examinations and measurements were done by a 12-year experienced oral and maxillofacial radiologist (K.O.). To detect the course and to measure the exact height of the septa in the sinus, 1-mm reconstructed panoramic images were used. The heights of the septa were measured in three regions along the course of the septa across the sinus floor: the lateral, middle and medial aspects based on previous studies [4,5] (fig. 2). The mean of these measurements was set as the final measurement. Meanwhile, the angle between the direction of the septum and median palatine suture was also measured using axial images (fig. 2). All measurements were accomplished with software programmed for an automated image measuring tool. All measurements were done 3 times by the same observer (K.O.). The same observer also performed the study twices with an interval of 2 weeks in order to detect intraobserver variability. Statistical analyses were carried out using the SPSS version 12.0.1 (SPSS, Chicago, Ill., USA) software program. To assess intraobserver reliability, the Wilcoxon matched-pairs signed-ranks test was used for repeat measurements of the observer. Independent groups in the study were compared using the Mann-Whitney U test; the results were expressed as means ± standard deviation. Nonparametric data were compared using the Kruskal-Wallis test. The Pearson χ2 test was performed for statistical analysis among gender, age, localization and measurements (p < 0.05).
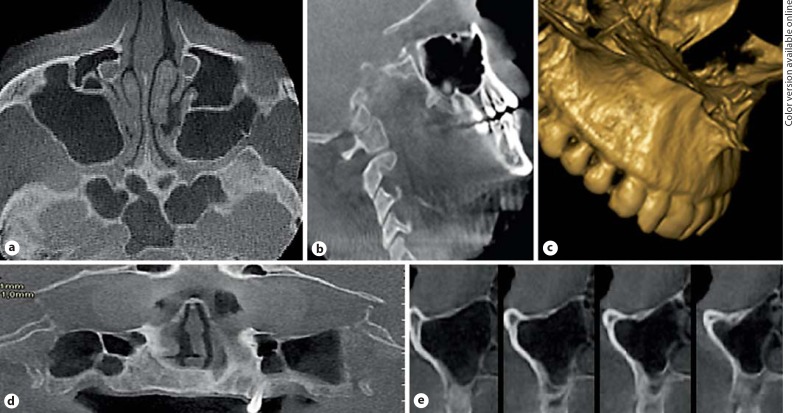
Fig. 1.
Reconstructed axial (a), sagittal (b) and 3-dimensional (c) images, as well as panoramic (d) and cross-sectional (e) CBCT images used for detection and measurement of maxillary sinus septa.
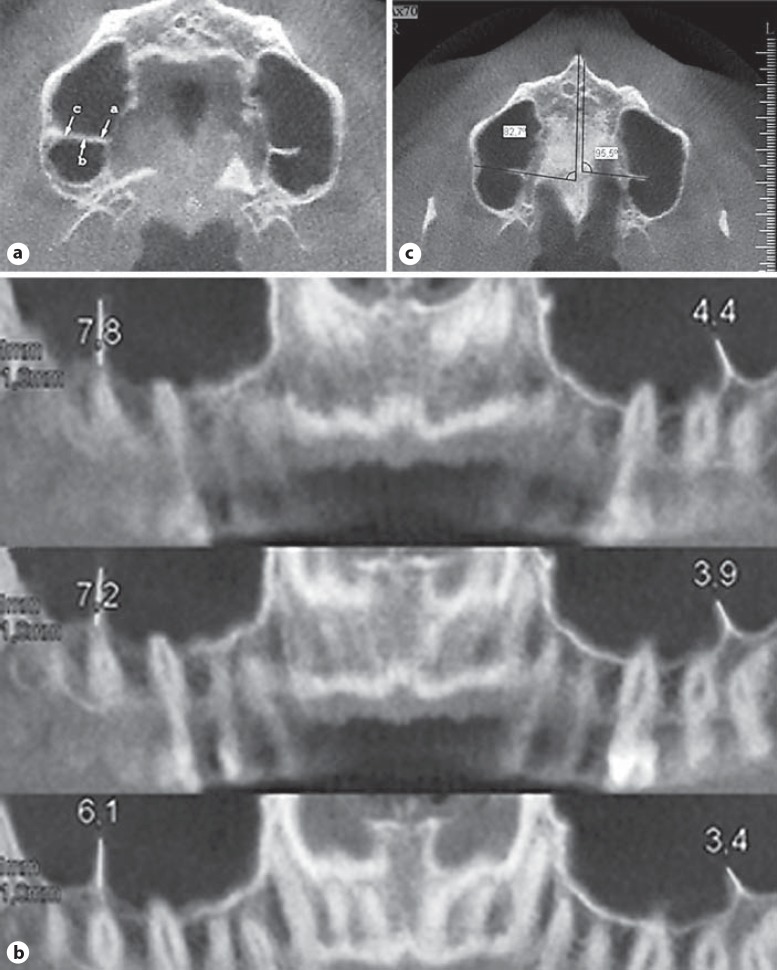
Fig. 2.
a The points related to the septal height measurements medial (arrow a), middle (arrow b) and lateral (arrow c) in axial CBCT images. b Reconstructed panoramic images also showing the vertical dimension of the antral septa at three positions. c Image showing the measurement of the angle between the direction of the septum and median palatine suture.
Results
The intraobserver consistency was rated at 96.9% between two measurements; hence there was no statistically significant difference between the two intraobserver measurements (p > 0.05). The prevalence of maxillary sinus segments with septa was 58% (316/544) in 228 patients (50% in males and 44.8% in females). A total of 369 septa were found in the 544 maxillary segments. A hundred and sixty-six (44.9%) septa were identified on the right side, whereas 203 (55%) were on the left. There were a total of 13 (3.2%) septa of completely edentulous (CE), 198 (53.9%) septa of edentate and 14 (3.8%) septa of the mixed dentition maxillary segments. Primary septa were detected in 85 (23.3%) of the partially edentulous (PE) segments and there were also 59 (16.2%) secondary septa in PE patients. Septa were found unilaterally in 148 segments (40.1%) and bilaterally in 221 (59.8%) segments.
Although unilaterally, septa were most common (12 cases; 3.25%) in cases with mixed dentition, in patients with dentition bilaterally, septa were most frequently detected (85; 23%). Unilaterally 2 septa were detected in 4 (1.08%) CE cases, bilaterally 1 septum in 4 (1.08%) cases, bilaterally 2 septa on one side and 1 septum on the other side in 1 case (0.2%), unilaterally 3 septa in 2 individuals (0.4%) and bilaterally 3 septa in 2 CE cases (0.4%).
In the PE cases, septa were detected with the following distribution: unilaterally 1 septum was detected in 54 of 187 (28.8%) cases, unilaterally 2 septa in 5 (2.6%) individuals, bilaterally 1 septum in 45 (24%) individuals, bilaterally 2 septa in 2 (1%) cases, bilaterally 2 septa on one side and 1 septum on the other side in 26 individuals (13.9%), unilaterally 3 septa in 2 individuals (2%), bilaterally 3 septa on one side and 1 septum on the other side in 5 individuals (2.6%), bilaterally 3 septa on one side and 2 septa on the other side in 2 patients (1%) were detected (table 1).
Table 1.
Distribution of septa in maxillary sinus segments
| Maxillary septum type | Septa | Patients with septa | Segments with septa | Edentate with septa | PE – primary with septa | PE – other with septa | CE with septa | Mixed dentition with septa |
|---|---|---|---|---|---|---|---|---|
| 1 septum on one side | 123 (33.3) | 123 | 123 | 59 | 27 | 27 | 0 | 10 |
| 2 septa on one side | 22 (5.69) | 11 | 11 | 11 | 3 | 2 | 4 | 2 |
| Bilaterally 1 septum on either side | 136 (36.9) | 68 | 136 | 85 | 26 | 19 | 4 | 2 |
| Bilaterally 2 septa on either side | 12 (3.2) | 3 | 6 | 10 | 1 | 1 | 0 | 0 |
| 2 septa on one side and 1 septum on the other side | 51 (14.1) | 17 | 34 | 24 | 20 | 6 | 1 | 0 |
| 3 septa on one side | 3 (0.8) | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| 3 septa on one side and 1 septum on the other side | 12 (3.8) | 3 | 3 | 3 | 5 | 2 | 2 | 0 |
| 3 septa on one side and 2 septa on the other side | 10 (2.2) | 2 | 2 | 6 | 1 | 1 | 2 | 0 |
| Total | 369 (100) | 228 | 316 | 198 (53.9) | 85 (23.03) | 59 (16.2) | 13 (3.2) | 14 (3.8) |
Results are expressed as numbers with percentages in parentheses.
Analysis of the anatomical location of the septa within the sinus revealed that 45 (12.2%) septa were located in the anterior region, 254 (69.1%) in the middle region and 70 (18.6%) in the posterior region. The location of septa observed in all study groups demonstrated a greater prevalence (69.1%) in the middle region than anterior and posterior regions (table 2). Measurements of the height of each individual septum varied among different regions. Comparison between the average septum measurements of PE and CE regions demonstrated statistically significantly higher values at all points of measurement (p < 0.05) than other areas. Separation of septa found in PE areas into those located apically to remaining teeth (primary septa) and those in the proximity of edentulous areas (other septa) showed that there was no statistically significant difference between the heights of the septa in groups (p > 0.05). On the other hand, primary septa in PE demonstrated statistically higher values compared with CE regions (table 2).
Table 2.
Summary of septum location, height and angle measurements according to dental status
| Dental status | Septum location, n |
Mean septum height ± SD, mm |
Mean septum angle 8 SD, mm | |||||
|---|---|---|---|---|---|---|---|---|
| anterior | middle | posterior | total | lateral | middle | medial | ||
| Edentate | 19 | 152 | 27 | 198 (53.9) | 4.15 ± 2.08 | 4.85 ± 2.38 | 5.99 ± 2.92 | 74.75 ± 17.73 |
| PE – primary | 10 | 49 | 26 | 85 (23.03) | 3.18 ± 3.39 | 4.88 ± 3.18 | 6.54 ± 3.27 | 76.22 ± 20.89 |
| PE – other | 10 | 40 | 9 | 59 (16.2) | 4.54 ± 3.87 | 6.22 ± 3.92 | 7.09 ± 4.11 | 74.11 ± 21.63 |
| CE | 3 | 7 | 3 | 13 (3.2) | 4.70 ± 1.82 | 5.33 ± 2.64 | 6.88 ± 3.42 | 77.11 ± 18.90 |
| Mixed dentition (children) | 3 | 6 | 5 | 14 (3.8) | 4.12 ± 2.88 | 4.32 ± 2.90 | 4.55 ± 2.88 | 74.18 ± 20.32 |
| Total | 45 (12.2) | 254 (69.1) | 70 (18.6) | 369 (100) | 3.73 ± 0.76 | 5.12 ± 0.88 | 6.21 ± 1.01 | 75.29 ± 19.89 |
Figures in parentheses indicate percentages.
The mean height of septa for males was 4.86 ± 2.01 mm, for females 5.02 ± 2.14 mm while the mean height for children and adult patients was 4.33 ± 1.92 and 5.5 ± 2.64 mm, respectively. The range of the septa in the study group was 1–10.3 mm for males and 2–15 mm for female patients. There were no statistically significant differences among the height values of maxillary sinus septa, with regard to gender or age (p > 0.05). Moreover, the angle of the septum in the anterior maxillary sinus region ranged from 34.1 to 90.6°, with a mean of 62.2 ± 15.05°, the angle of the septum within the middle region ranged from 44.8 to 118°, with a mean of 75.8 ± 18.6°, and the angle of the septum in the posterior maxillary sinus region ranged from 58.1 to 123.6°, with a mean of 90.75 ± 19.4° (table 2). Significant differences in the angle of the septum were noted between the anterior maxillary sinus region and posterior region (p < 0.05). All detected septa showed a mediolateral orientation.
Discussion
The 58% prevalence of septa in this study was higher than the 16–33% reported in previous studies [4,6,7,13,26]. This difference could be attributed to the difference between the radiographic examinations. The higher prevalence in our study was based on the thin slice interval of CBCT images (0.3 mm). As for the location of the septa, a greater number of incidence was found in the middle regions while several studies [6,7,26] had observed them in the anterior [5,9,13] and in the posterior regions [5,9]. The morphology of septa did, however, demonstrate significant variability. This is evident in the results obtained from measuring each septum at 3 aspects along its medial-lateral dimension. These differences could be due to comparing septa from totally edentulous areas with septa from PE ones [4,6,7,9]. However, our results were contrary to these as the mean height of septa in CE cases was higher than both septum types of PE cases but is similar to the results which were obtained by Koymen et al. [5].
Previous studies reported different heights for the septa ranging from 5.6 to 20.6 mm [5,7,9,13,24,25,26] in other populations. However, the mean adult septum height of our study was lower than those of some other populations [4,6,7,13,24].
The probable reason for the differences is that Neugebauer et al. [24] did not make any distinction between children and the adult population in their study while Naitoh et al. [25] examined only dry skulls of children.
As surgery involving the maxillary sinus segment is applied more frequently, radiological evaluation determining the sizes and localizations of the septa has gained importance. The panoramic radiographs and the CT scans are the most frequently used radiological methods for planning dental implants [6,7,15]. When comparing incidence of septa in both radiological techniques, several authors have observed false-negative results in the panoramic radiographs [6,7,14]. Some authors have had results with 50% false-negative findings [14].
Studies indicate that CT scans are more reliable than panoramic radiographs in the preoperative analysis. Today, CT can be performed in axial and coronal planes with 3-dimensional views for diagnosis and treatment of this region [27,28]. The 3-dimensional CT avoids the superimposition and problems due to magnification and offers to visualize the craniofacial structures with more precision than the 2-dimensional conventional methods. Despite these advantages, the effective dose of CT is much higher than that of the conventional radiographs and also an expensive procedure, and scanners are not easily accessible [22,23].
In the last decade, a technique called CBCT was proposed for maxillocraniofacial imaging [19]. The comparison of absorbed doses shows that the CBCT is similar to dental panoramic radiology, which has requirements that are considerably lower than medical CT imaging [21,22,23]. The effective dose (ICRP 2007) from a standard dental protocol scan using a traditional CT was 1.5–12.3 times greater than comparable medium field of view dental CBCT scans [23]. It was also stated that the image quality of CBCT was adjudged to be equivalent to that of traditional CT for visualizing the maxillofacial structures. Moreover, beam-hardening artifacts due to dental-care material and implants were weaker at CBCT than at multislice CT [29]. From the radiation point of view, CBCT examinations can be used instead of CT in order to evaluate anatomical structures like the maxillary sinus.
There are limited studies examining children's septa [24,25] that have been published. With the advent of endoscopic sinus surgery in adults, studies were initiated to evaluate its safety and efficacy in children. Precise knowledge of the children's maxillary sinus septum morphology is important and allows exact planning of endoscopic sinus surgery and helps to avoid complications. It should be noted that maxillary septa also exist in children. The height of these maxillary septa was similar to those of adult patients without a significant difference in this study. The prevalence of septa has no relation with the patient's gender or age, but there are differences based on the type of edentulism. Differences between the results obtained from different studies may reflect variability between methods of measurement, tools utilized to gather data, and variation among populations studied [24,25,26,27,28,29,30].
Conclusion
Septa of various heights and courses developed in all parts of the maxillary sinus; therefore, to prevent possible complications during sinus surgery, extensive evaluation with an appropriate radiographic technique is indispensable. CBCT was a powerful tool for the examination of this zone capable of making measurements and 3-dimensional representations of the region with less ionizing radiation.
References
- 1.McGowan DA, Baxter PW, James J. The Maxillary Sinus and Its Dental Implications. Oxford: Wright, Butter-Worth-Heinemann; 1993. pp. 1–125. [Google Scholar]
- 2.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 3.González-Santana H, Peñarrocha-Diago M, Guarinos-Carbó J, Sorní-Bröker M. A study of the septa in the maxillary sinuses and the subantral alveolar processes in 30 patients. J Oral Implantol. 2007;33:340–343. doi: 10.1563/1548-1336(2007)33[340:ASOTSI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Kim MJ, Jung UW, Kim CS, Kim KD, Choi SH, Kim CK. Maxillary sinus septa: prevalence, height, location and morphology. A reformatted computed tomography scan analysis. J Periodontol. 2006;5:903–908. doi: 10.1902/jop.2006.050247. [DOI] [PubMed] [Google Scholar]
- 5.Koymen R, Gocmen-Mas N, Karacayli U, Ortakoglu K, Ozen T, Yazici AC. Anatomic evaluation of maxillary sinus septa. Surgery and Radiology Clin Anat. 2009;22:563–570. doi: 10.1002/ca.20813. [DOI] [PubMed] [Google Scholar]
- 6.Krennmair G, Ulm C, Lugmayr H. Maxillary sinus septa: incidence, morphology and clinical implications. J Craniomaxillofac Surg. 1997;25:261–265. doi: 10.1016/s1010-5182(97)80063-7. [DOI] [PubMed] [Google Scholar]
- 7.Krennmair G, Ulm GW, Lugmayr H, Solar P. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg. 1999;57:667–771. doi: 10.1016/s0278-2391(99)90427-5. [DOI] [PubMed] [Google Scholar]
- 8.Naitoh M, Suenaga Y, Kondo S, Gotoh K, Ariji E. Assessment of maxillary sinus septa using cone-beam computed tomography: etiological consideration. Clin Implant Dent Relat Res. 2009;11(suppl 1):52–58. doi: 10.1111/j.1708-8208.2009.00194.x. [DOI] [PubMed] [Google Scholar]
- 9.Velasquez-Plata D, Hovey LR, Peach CC, Alder ME. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants. 2002;17:854–860. [PubMed] [Google Scholar]
- 10.Betts NJ, Miloro M. Modification of the sinus lifts procedure for septa in the maxillary antrum. J Oral Maxillofac Surg. 1994;52:332–333. doi: 10.1016/0278-2391(94)90313-1. [DOI] [PubMed] [Google Scholar]
- 11.Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology – eleven years of surgical experience. J Oral Implantol. 1990;16:199–209. [PubMed] [Google Scholar]
- 12.Van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000;11:256–265. doi: 10.1034/j.1600-0501.2000.011003256.x. [DOI] [PubMed] [Google Scholar]
- 13.Underwood AS. An inquiry into the anatomy and pathology of the maxillary sinus. J Anat Physiol. 1910;44:354–369. [PMC free article] [PubMed] [Google Scholar]
- 14.Kasabah S, Slezak R, Simunek A, Krug J, Lecaro MC. Evaluation of the accuracy of panoramic radiograph in the definition of maxillary sinus septa. Acta Med. 2002;45:173–175. [PubMed] [Google Scholar]
- 15.Lugmayr H, Krennmair G, Holzer H. The morphology and incidence of maxillary sinus septa. Rofo. 1996;165:452–454. doi: 10.1055/s-2007-1015788. [DOI] [PubMed] [Google Scholar]
- 16.Abrahams JJ. Dental CT imaging: a look at the jaw. Radiology. 2001;219:334–345. doi: 10.1148/radiology.219.2.r01ma33334. [DOI] [PubMed] [Google Scholar]
- 17.Alder ME, Deahl ST, Matteson SR. Clinical usefulness of two dimensional reformatted and three-dimensionally rendered computerized tomographic images: literature review and a survey of surgeons opinions. J Oral Maxillofac Surg. 1995;53:375–386. doi: 10.1016/0278-2391(95)90707-6. [DOI] [PubMed] [Google Scholar]
- 18.Almog DM, Romano PR. CT-based dental imaging for implant planning and surgical guidance. NY State Dent J. 2007;73:51–53. [PubMed] [Google Scholar]
- 19.Mozzo P, Procacci C, Tacconi A, Martini PT, Bergamo IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8:1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 20.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT). I. On subjective image quality. Eur J Radiol. 2010;75:265–269. doi: 10.1016/j.ejrad.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 21.Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, Marchal G, Sanderink G, Jacobs R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71:461–468. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 23.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–114. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 24.Neugebauer J, Ritter L, Mischkowski RA, Dreiseidler T, Scherer P, Ketterle M, Rothamel D, Zöller JE. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int J Oral Maxillofac Implants. 2010;25:258–265. [PubMed] [Google Scholar]
- 25.Naitoh M, Suenaga Y, Gotoh K, Ito M, Kondo S, Ariji E. Observation of maxillary sinus septa and bony bridges using dry skulls between Hellman's dental age of IA and IIIC. Okajimas Folia Anat Jpn. 2010;87:41–47. doi: 10.2535/ofaj.87.41. [DOI] [PubMed] [Google Scholar]
- 26.Ulm CW, Solar P, Krennmair G, Matejka M, Watzek G. Incidence and suggested surgical management of septa in sinus-lift procedures. Int J Oral Maxillofac Implants. 1995;10:462–465. [PubMed] [Google Scholar]
- 27.Zinreich JS, Benson LM, Oliverio JP. Sinonasal cavities: CT normal anatomy, imaging of the osteomeatal complex and functional endoscopic surgery. In: Som PM, Curtin HD, editors. Head and Neck Imaging. ed 3. St Louis: Mosby; 1996. p. 98. [Google Scholar]
- 28.Kumar V, Ludlow JB, Mol A, Cevidanes L. Comparison of conventional and cone beam CT synthesized cephalograms. Dentomaxillofac Radiol. 2007;36:263–269. doi: 10.1259/dmfr/98032356. [DOI] [PubMed] [Google Scholar]
- 29.Carrafiello G, Dizonno M, Colli V, Strocchi S, Pozzi Taubert S, Leonardi A. Comparative study of jaws with multislice computed tomography and cone-beam computed tomography. Radiol Med. 2010;115:600–611. doi: 10.1007/s11547-010-0520-5. [DOI] [PubMed] [Google Scholar]
- 30.Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13:11–12. [PubMed] [Google Scholar]