Abstract
Objective
The purpose of this study was to retrospectively evaluate the use of locked plating (LP) and retrograde nailing (RN) for treating extra-articular distal femoral fractures.
Materials and Methods
From January 2004 to March 2009, 36 patients with extra-articular distal femoral fractures were surgically treated at our Trauma Center. The patients were divided into two groups according to the treatment method, with 19 patients being treated by LP (LP group) and 17 patients via RN (RN group).
Results
The demographics of age (p = 0.460) and gender (p = 0.481) in both LP and RN groups were similar. No differences were found with respect to postoperative malreduction, deep infection, hardware failure, operating time, knee pain, HSS score and range of knee movement. The mean intraoperative blood loss was significantly higher in the RN group (298 ± 65.2 ml, range 200–410) than in the LP group (200 ± 48.9 ml, range 130–300) (p < 0.01). However, a higher rate of union disturbance was observed in the LP group (36.8%) compared to the RN group (5.9%) (p = 0.044).
Conclusions
The overall union disturbance rate in the LP group was higher than in the RN group. However, further analysis revealed that clinical outcome may largely depend on surgical technique rather than on the choice of implant. Therefore, correct rules (the same for every procedure) should be strictly adhered to, especially in the application of LP.
Key Words: Distal femoral fracture, Locked plate, Retrograde nail
Introduction
The optimal method for the treatment of extra-articular distal femoral fractures remains controversial [1,2,3,4,5]. Open reduction disturbs the natural process of fracture healing and is often associated with a high rate of nonunion and infection [6]. The concept of ‘biological’ osteosynthesis and minimally invasive approaches has resulted in decreased complication rates. Retrograde intramedullary femoral nailing is a ‘biological’ method, which is preferred by some surgeons for its good control of the distal fragment [7,8]. Meanwhile, locked plating (LP) remains a popular and effective alternative method to treat these challenging injuries. The main advantage of an anatomically precontoured locked plate is soft-tissue protection using a limited approach [9,10,11].
Despite the widespread use of both techniques, few clinical studies have directly compared locked plates to nails. Consequently, the present study was undertaken retrospectively to compare LP and retrograde nailing (RN) for the treatment of extra-articular distal femoral fractures.
Subjects and Methods
This was a retrospective study analyzing our population of extra-articular distal femoral fractures who were treated by either LP or RN at our Trauma Center. The inclusion criteria for this study were: (a) acute and unilateral fractures; (b) patients who were able to walk without any assistance before injury; (c) femoral supracondylar fractures and supracondylar fractures with fracture line extension into distal third femoral shaft. The exclusion criteria for this study were: (a) fractures involving an articular surface; (b) old fractures (definitive surgery more than 3 weeks after the injury; (c) pathological fractures; (d) Gustilo III open fractures; (e) fractures associated with neurovascular injuries; (f) fractures associated with cruciate ligament tear; (h) patients requiring intensive care or requiring transfer to other departments for treatment; (i) periprosthetic supracondylar femoral fractures following total knee arthroplasty. The fractures were classified according to the Orthopaedic Trauma Association classification [12].
Between 2004 and 2009, a total of 36 patients with 36 extra-articular distal femoral fractures were matched for inclusion criteria for analysis. The patients were divided into two groups based on the method of treatment: patients treated with LP and those treated by RN (table 1).
Table 1.
Demographics and fracture pattern in the two groups
| Parameters | LP group (n = 19) | RN group (n = 17) | p value |
|---|---|---|---|
| Gender | 0.481 | ||
| Male | 12 | 13 | |
| Female | 7 | 4 | |
| Mean age ± SD, years | 54.7 ± 16.1 | 50.6 ± 16.3 | 0.460 |
| Side | 0.322 | ||
| Left | 10 | 12 | |
| Right | 9 | 5 | |
| High energy trauma | 12 | 13 | 0.481 |
| Classification (AO/OTA) | 0.910 | ||
| 33-A1 | 8 | 6 | |
| 33-A2 | 7 | 8 | |
| 33-A3 | 4 | 3 | |
| Mean preoperation stay ± SD, days | 2.1 ± 1.0 | 1.7 ± 0.8 | 0.275 |
| Diabetes | 3 | 2 | 1.000 |
| Heavy smoker | 5 | 3 | 0.695 |
| Multiple injury | 3 | 5 | 0.434 |
Operative Techniques
All the surgeries were performed by the same team of orthopaedic surgeons who had no preference for one particular method of fixation. All the patients in the LP group were positioned supine on a radiolucent table. The knee was placed in a slight flexion over a folded blanket, which helped to improve the sagittal plane reduction of the fracture by relaxing the primary deforming force of the gastrocnemius. A lateral parapatellar approach was used to insert a submuscular plate, having achieved a satisfactory reduction via a closed manner. Seventeen fractures were stabilized by a less invasive stabilization system (LISS, Synthes, Shanghai, PR China), and the other 2 by periarticular anatomic locked plates (Zimmer, Shanghai, PR China).
In the RN group, nailing was performed with the patient supine on the radiolucent table. A 3-cm incision was made just medial to the patellar tendon. The intercondylar notch was palpated through the percutaneous approach. The precise location of the central guide pin was confirmed by means of anterior-posterior and lateral fluoroscopy. If the fracture reduction was not satisfactory when the nail was inserted, the nail was removed, and Kirschner wires (K-wires) as blocking screws were introduced. The placement of K-wires was performed under the guidance of image intensification. After the placement of the K-wires, the medullary cavity was rereamed and the nail reinserted. Then cortical screws were substituted for the K-wires. All the cases were statically locked with at least 2 distal locking screws after the nails had been inserted. Every effort was made to ensure that the nail was at least 3 mm deep to the articular surface. Prior to proximal locking, a final determination of length, rotation, and alignment was made under fluoroscopy. Short (230 mm) and long nails were used in 3 (Stryker, Suzhou, PR China) and 14 patients (Smith and Nephew, Shanghai, PR China), respectively. No pneumatic tourniquet was used in either group.
Postoperative Management
The patients began to use an active range of motion of the knee after surgery. Full weight-bearing was usually delayed until a callus was apparent on the postoperative radiographs. All radiographs were evaluated by an independent assessor (W.G.). In this study, delayed union was defined as a fracture which had not united 6 months after surgery. A fracture of the distal femur was defined as a nonunion when a minimum of 9 months had elapsed since injury and the fracture showed no visible progressive signs of healing over 3 months, or if loss of initial fracture fixation occurred in less than 9 months. Postoperative malreduction was defined as more than 5° deformity in the sagittal or coronal plane. Implant failure included screw loosening and/or breakage, and nail or plate fracture. The rate of implant removal was not assessed in this study because some of the implants were removed at the patients’ request without any complications. Knee function evaluation was performed at the last visit according to HSS scores [12]. The range of movement was recorded during each visit.
Statistical Analysis
The Fisher exact test was used for categorical variables between the two groups, such as gender, injured side, high energy trauma, fracture characteristics, diabetes, heavy smoker, multiple injuries, delayed union, nonunion, malunion, deep infection, hardware breakage or loosening and knee pain. A Student's t test was used for continuous variables, such as age, preoperation stay, operating time, follow-up period, intraoperative blood loss, HSS score and knee range of movement. The statistical software SPSS 11.0 (Chicago, Ill., USA) was used to perform Fisher's exact test and independent sample t test. A statistical power analysis was conducted to calculate the true power of the study (PASS V11.0.7); p values below 0.05 were considered to be statistically significant (tables 1, 2).
Table 2.
Postoperative parameters in the two groups
| Parameters | LP group (n = 19) | RN group (n = 17) | p value |
|---|---|---|---|
| Follow-up period, months | 23.37 ± 5.33 | 26.29 ± 12.71 | 0.387 |
| Union rate, % | 84.2 | 94.1 | 0.605 |
| Complications | |||
| Union disturbance rate, % | 36.8 | 5.9 | 0.044 |
| Delayed unions, n | 4 | 0 | 0.106 |
| Nonunion, n | 3 | 1 | 0.605 |
| Postoperative malreduction, n | 1 | 2 | 0.593 |
| Deep infection, n | 1 | 0 | 1.000 |
| Hardware breakage or loosening, n | 2 | 0 | 0.487 |
| Knee pain, n | 1 | 3 | 0.326 |
| Intraoperative blood loss, ml | 200 ± 48.9 | 298 ± 65.2 | <0.01 |
| Operating time, min | 79.7 ± 14.3 | 87.4 ± 13.2 | 0.106 |
| HSS score | 85.0 ± 11.3 | 86.2 ± 6.8 | 0.406 |
| Range of knee movements, ° | 98.2 ± 21.5 | 103.5 ± 11.0 | 0.346 |
Results
Baseline characteristics, such as the cause of injury, fracture type, open fracture grade, mean age, gender distribution, associated medical conditions and preoperative stay were similar in the two groups of patients (table 1).
All the patients were followed up completely. The mean period of follow-up in the LP group was 23.37 ± 5.33 months (range 13–29), while in the RN group it was 26.29 ± 12.71 months (range 12–70) (p = 0.387, statistical power: 13.4%).
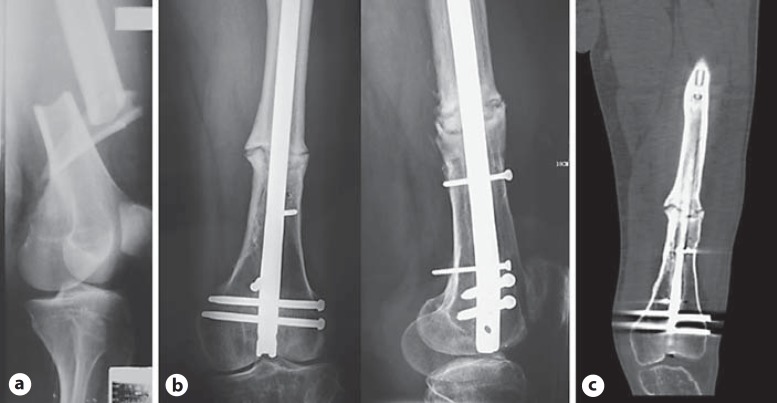
There was a statistically significant difference in the overall union disturbance rate (p = 0.044). Four cases of delayed union (fig. 1) and 3 cases of nonunion occurred in the LP group. One of the nonunion cases was the result of screw breakage (fig. 2). Cases of nonunion in the LP group were treated with exchange implants and autologous bone grafting and eventually adequate healing was achieved. One case in the LP group lost alignment into serious genu valgum deformity after the plate was removed (fig. 3). However, the patient refused to receive corrective osteotomy. All but one of the fractures in the RN group united within 6 months. The nonunion in the RN group (fig. 4) was managed with augmentative LP and autologous iliac bone graft. The nonunion united 5 months after revision surgery. There was no statistically significant difference in the final union rate between the two groups (84.2 vs. 94.1%, p = 0.605, statistical power: 13.6%).
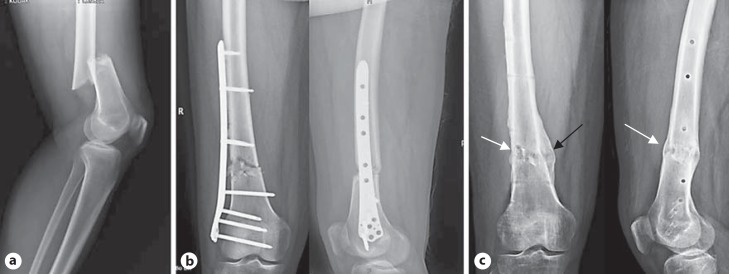
Fig. 1.
A 53-year-old man with a simple extra-articular distal femoral fracture (AO/OTA 33-A1) that was managed with submuscular LISS plating. He developed a delayed union. a Preoperative radiograph. b Radiographs taken after LISS plating showing suboptimal placement of plate and screws. c Radiographs taken after hardware removal showed asymmetric callus formation. The most and least callus formed medially (black arrow) and anterolaterally (white arrows), respectively.
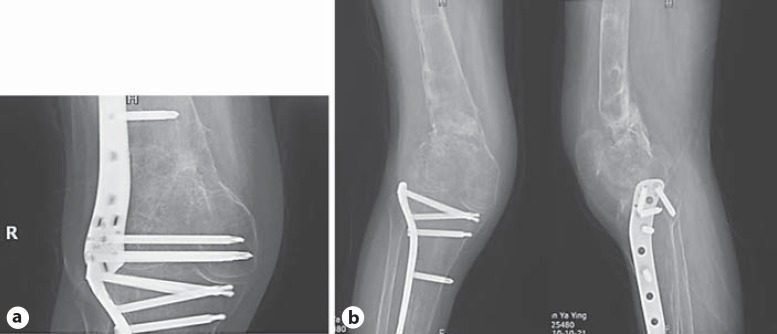
Fig. 2.

A 76-year-old man with distal femoral fracture was managed with indirect reduction and submuscular LISS plating. Screw breakage shown on radiograph 9 months postoperatively (black arrows).
Fig. 3.
A 54-year-old female who had a history of tibial plateau fracture 2 years before she suffered from ipsilateral supracondylar distal femur fracture due to a fall. She was managed with LISS plating. a Radiograph taken 19 months after LISS plating. b Radiographs taken 4 months after implant removal showed loss of alignment.
Fig. 4.
A 45-year-old man with distal femur fracture (AO/OTA 33-A2) that was managed with RN and blocking screws. a Preoperative radiograph. b Radiographs taken 58 months after short retrograde nail fixation showed persistent nonunion. c CT confirmed nonunion.
One (5.3%) patient in the LP group developed a late-onset deep infection 5 months after surgery. The patient underwent implant removal, débridement and received antibiotic-impregnated acrylic beads. The infection resolved completely 6 weeks later. No deep infection was documented in the RN group. The difference in deep infection rate was not significant (p = 1.000, statistical power: 1.6%). There was no statistically significant difference in postoperative malreduction (p = 0.593, statistical power: 5.3%) and hardware failure (p = 0.487, statistical power: 13.2%). Knee pain was more common after nailing but there was no significant difference between the two groups (p = 0.326, statistical power: 15.5%) (table 2).
The mean intraoperative blood loss was significantly higher in the RN group than in the LP group. There was no statistically significant difference in the mean operating time between the two groups (p = 0.106, statistical power: 37.3%) (table 2).
There was no statistically significant difference in the range of movement (p = 0.346, statistical power: 15.0%) and HSS score (p = 0.406, statistical power: 6.7%) between the two groups at the last visit. The mean range of movement was 98.2 ± 21.5° (range, 20–120°) in the LP group and 103.5 ± 11.0°(range, 80–120°), respectively. The mean HSS score was 85.0 ± 11.3 points (range, 50–98) in the LP group and 86.2 ± 6.8 points (range, 70–95), respectively (table 2).
Discussion
The present study showed asymmetric callus formation in the majority of LP cases, as the most and least callus formed medially (far away from the plate) and laterally (close to the plate), respectively. This finding supports those of Lujan et al. [13], that locked plates could be too stiff to reliably promote secondary bone healing compared to centric load-sharing nails. Our finding that the overall union disturbance rate in the LP group was higher than in the RN group confirmed the findings of Herrera et al. [2], who found a 3.5-fold increase of nonunion associated with locked plates as compared with intramedullary nailing, and Henderson et al. [14], who reported that complications of healing including nonunion, delayed union, and implant failure were not infrequent on distal femur fractures treated with locked plates. However, Markmiller et al. [3] and Zlowodzki et al. [1] reported nailing was 5.5 and 5.3%, respectively, hence there was no difference between LN and RN.
These results should be interpreted with caution because the stiffness of a fixation construct is a principal determinant of the motion of a fracture site and therefore affects the mechanism and progression by which a fracture is healed [15]. Generally bridge plating works best with a multifragmentary or comminuted fracture. However, in simple fracture patterns, the screws should be positioned away from the fracture line in order to allow for elastic deformation of the plate-screw construct [5,16]. As in this study in the LP group, one delayed union (originally a simple supracondylar fracture) might be the result of suboptimal placement of plate and locking screws (fig. 1), thereby supporting the notion that clinical outcome may largely depend on surgical technique rather than on the choice of implant [5]. However, the current modern-day locked plates with innovations in implant design, such as far cortical locking, may reduce the stiffness of the LP construct while retaining construct strength [15,17,18,19,20]. This speculation will await future study comparing newly designed LP and RN for distal femur fractures is warranted.
Deep infection rate has largely diminished since the introduction of the minimally invasive procedures as in our current study, where only 1 of 19 patients in the LP group developed a late-onset deep infection and no infection was documented in the RN group, which confirmed previous studies that infection rates were similar in both techniques [1,3].
Loss of alignment after plate removal was found in 1 case of the LP series (fig. 2). This failure is attributed to deficient callus formation at the lateral cortex of the distal femur. In this case, regular use of computed tomography is recommended if any suspicion of poor healing exists, especially before the plate is removed in osteoporotic bone because the plate sometimes shadows the lateral cortex in the anteroposterior view.
A theoretically higher level of knee pain is a huge concern associated with RN [21]. But this was not able to produce a statistically significant difference in the incidence of knee pain between the two groups, probably because great effort was made to avoid injuring the patellar cartilage and to minimize damage to the femoral cartilage during the nailing procedure.
Although angular malunion after RN is a known complication [8,22,23], there was no statistically significant difference between the two techniques probably due to careful blocking of screws in RN for distal femoral fractures.
Submuscular LISS plating and percutaneous screw insertion facilitated by an aiming device seem to be a faster procedure compared to RN, which needs time-consuming reaming before nail insertion, while the additional use of blocking screws during nailing may further increase the operating time. However, no statistically significant differences in operating time were found between the two groups. The fact is that closed reduction of fragments and restoration of alignment for distal femur fractures through a single lateral small incision during LISS fixation are technically demanding, and this may offset any convenience in implant insertion. For RN, reaming the medullary cavity may result in more intraoperative blood loss compared to submuscular plating, if no pneumatic tourniquets are used intraoperatively.
Limitations of this study: (a) limited number of patients that was not large enough to strengthen the significance of the differences in rates of nonunion and also delayed union; (b) participating surgeons had less experience with LISS fixation at their early learning stage, results probably were biased in favor of RN fixation; (c) being a retrospective study, there was scope for selection bias; however, the groups were properly matched for age, sex, injured side, OTA classification, mean duration between surgery and the occurrence of injuries and associated injuries, and (d) short follow-up period that was not adequate for obtaining long-term outcomes.
Conclusion
The overall union disturbance rate in the LP group was higher than in the RN group. However, further analysis revealed that clinical outcome may largely depend on surgical technique rather than on the choice of implant. Therefore, correct rules (the same for every procedure) should be strictly adhered to, especially in the application of LP.
References
- 1.Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005) J Orthop Trauma. 2006;20:366–371. doi: 10.1097/00005131-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981–2006) Acta Orthop. 2008;79:22–27. doi: 10.1080/17453670710014716. [DOI] [PubMed] [Google Scholar]
- 3.Markmiller M, Konrad G, Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004;426:252–257. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 4.Pospula W, Abu Noor T. The periprosthetic fractures of the femur after hip and knee replacement: analysis of treatment results in Al Razi Hospital. Med Princ Pract. 2009;18:198–203. doi: 10.1159/000204350. [DOI] [PubMed] [Google Scholar]
- 5.Hierholzer C, von Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop. 2011;45:243–250. doi: 10.4103/0019-5413.80043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomson AB, Driver R, Kregor PJ, Obremskey WT. Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing. Orthopedics. 2008;3:748–750. doi: 10.3928/01477447-20080801-33. [DOI] [PubMed] [Google Scholar]
- 7.Gurkan V, Orhun H, Doganay M, Salioğlu F, Ercan T, Dursun M, Bülbül M. Retrograde intramedullary interlocking nailing in fractures of the distal femur. Acta Orthop Traumatol Turc. 2009;43:199–205. doi: 10.3944/AOTT.2009.199. [DOI] [PubMed] [Google Scholar]
- 8.Ostrum RF, Maurer JP. Distal third femur fractures treated with retrograde femoral nailing and blocking screws. J Orthop Trauma. 2009;23:681–684. doi: 10.1097/BOT.0b013e3181ad61f2. [DOI] [PubMed] [Google Scholar]
- 9.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13:401–406. doi: 10.1097/00005131-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Kolb W, Guhlmann H, Windisch C, Marx F, Kolb K, Koller H. Fixation of distal femoral fractures with the Less Invasive Stabilization System: a minimally invasive treatment with locked fixed-angle screws. J Trauma. 2008;65:1425–1434. doi: 10.1097/TA.0b013e318166d24a. [DOI] [PubMed] [Google Scholar]
- 11.Smith TO, Hedges C, MacNair R, Schankat K, Wimhurst JA. The clinical and radiological outcomes of the LISS plate for distal femoral fractures: a systematic review. Injury. 2009;40:1049–1063. doi: 10.1016/j.injury.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Orthopaedic Trauma Association Classification Database and Outcomes Committee Fractures and dislocation compendium: femur. J Orthop Trauma. 2007;21:S31–S42. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 13.Lujan TJ, Henderson CE, Madey SM, Fitzpatrick DC, Marsh J, Bottlang M. Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma. 2010;24:156–162. doi: 10.1097/BOT.0b013e3181be6720. [DOI] [PubMed] [Google Scholar]
- 14.Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma. 2011;25(suppl 1):S8–S14. doi: 10.1097/BOT.0b013e3182070127. [DOI] [PubMed] [Google Scholar]
- 15.Doornink J, Fitzpatrick DC, Madey SM, Bottlang M. Far cortical locking enables flexible fixation with periarticular locking plates. J Orthop Trauma. 2011;25(suppl 1):S29–S34. doi: 10.1097/BOT.0b013e3182070cda. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ehlinger M, Adam P, Arlettaz Y, Moor BK, DiMarco A, Brinkert D, Bonnomet F. Minimally-invasive fixation of distal extra-articular femur fractures with locking plates: limitations and failures. Orthop Traumatol Surg Res. 2011;97:668–674. doi: 10.1016/j.otsr.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Bottlang M, Lesser M, Koerber J, Doornink J, von Rechenberg B, Augat P, Fitzpatrick DC, Madey SM, Marsh JL. Far cortical locking can improve healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92:1652–1660. doi: 10.2106/JBJS.I.01111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bottlang M, Feist F. Biomechanics of far cortical locking. J Orthop Trauma. 2011;25(suppl 1):S21–28. doi: 10.1097/BOT.0b013e318207885b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bottlang M, Lesser M, Koerber J, Doornink J, von Rechenberg B, Augat P, Fitzpatrick DC, Madey SM, Marsh JL. Far cortical locking can improve healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92:1652–1660. doi: 10.2106/JBJS.I.01111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sellei RM, Garrison RL, Kobbe P, Lichte P, Knobe M, Pape HC. Effects of near cortical slotted holes in locking plate constructs. J Orthop Trauma. 2011;25(suppl 1):S35–S40. doi: 10.1097/BOT.0b013e3182070f2d. [DOI] [PubMed] [Google Scholar]
- 21.El Moumni M, Schraven P, ten Duis HJ, Wendt K. Persistent knee complaints after retrograde unreamed nailing of femoral shaft fractures. Acta Orthop Belg. 2010;76:219–225. [PubMed] [Google Scholar]
- 22.Ricci WM, Bellabarba C, Lewis R, Evanoff B, Herscovici D, Dipasquale T, Sanders R. Angular malalignment after intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:90–95. doi: 10.1097/00005131-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Acharya KN, Rao MR. Retrograde nailing for distal third femoral shaft fractures: a prospective study. J Orthop Surg. 2006;14:253–258. doi: 10.1177/230949900601400305. [DOI] [PubMed] [Google Scholar]