Abstract
This review positions public health as an endeavour that requires a high order of professionalism in addressing the health of populations; this requires investment in an educational capacity that is designed to meet this need. In the global context, the field has evolved enormously over the past half century, supported by institutions such as the World Bank, the World Health Organization and the Institute of Medicine. Operational structures are formulated by strategic principles, with educational and career pathways guided by competency frameworks, all requiring modulation according to local, national and global realities. Talented and well-motivated individuals are attracted by its multidisciplinary and transdisciplinary environment, and the opportunity to achieve interventions that make real differences to people's lives. The field is globally competitive and open to many professional backgrounds based on merit. Its competencies correspond with assessments of population needs, and the ways in which strategies and services are formulated. Thus, its educational planning is needs-based and evidence-driven. This review explores four public health education levels: graduate, undergraduate, continuing professional education and promotion of health literacy for general populations. The emergence of accreditation schemes is examined, focusing on their relative merits and legitimate international variations. The role of relevant research policies is recognized, along with the need to foster professional and institutional networks in all regions of the world. It is critically important for the health of populations that nations assess their public health human resource needs and develop their ability to deliver this capacity, and not depend on other countries to supply it.
Key Words: Public health sciences, Higher education, Policy, Planning, Health promotion, Health protection, Disease prevention, Health human resources, Global health, Health literacy
Introduction
The 21st century is immersed in transformative change. Most nations, many still emerging from the legacy of colonialism, are confronted with political and economic development challenges; even established world powers must transform or face decline. People everywhere are being uplifted by the diffusion of science, technology and the humanities across cultures. Traditional ways of doing things, belief systems, social and political structures, and institutions, are being tested at their foundations. In synchrony, the need for self-determination is leading, albeit fitfully, to democratization: people striving to take ownership of their lives, to achieve fairness, better living conditions and improved prospects [1].
To fully realize the human potential, it is imperative that all nations have well-grounded health systems; combining sound values with scientific evidence and advocacy, all responsible societies must seek to promote, protect, improve and restore the health of all individuals and population groups. This review addresses in particular how a renaissance in public health professional education must play a key role in shaping the future health of all populations, from local to global, with professional engagement and community participation at the heart of this process.
To describe a global perspective on anything of importance requires pooling the insights of many scholars. However, while drawing from references which reflect attempts to take a world view, this literature is dominated by Western publishing interests. What is synthesized here therefore is but a snapshot in time as perceived by a Western educated public health scholar with experience in public and private sectors in several world regions, from a career spanning over four decades.
It is important also to state what this review is not about: the needed education of all health professionals in the principles of public health, just as they must know something about how their health care system works. Suffice it to acknowledge that, in 2010, the Commission on Education of Health Professionals for the 21st Century offered recommendations for reform, a century after the famous Flexner Report of 1910. The Commission put forward a vision that all health professionals should be educated to mobilize knowledge and engage in critical reasoning and ethical conduct so that they are competent to participate in patient- and population-centred health systems as members of locally responsive and globally connected teams [2]. In fact, all medical faculties desiring accreditation in the UK [3], the USA or Canada [4] must align with guidelines that require that their students are prepared in the elements of public health. All this should take place of course, but because medical education is focused mainly on the key role of physicians as patient care providers, it does not prepare them at a professional level to address population health needs. For that to occur requires in-depth education and development in public health, just as would be required for any other field for which a clinical care provider may specialize in, for instance, neurology or cardiac surgery. This review thus aims to position public health as an endeavour that requires its own high order of professionalism in addressing the health needs of populations, as distinct from the clinical care of individuals. This must go well beyond an introductory orientation, and do so not just for physicians but also for candidates from other backgrounds, to build the competencies required for balanced public health human resources.
The Essential Nature of Public Health
A complex and challenging field, public health encompasses diverse skill sets from the biomedical, social, behavioural and environmental sciences to engineering, law and ethics. Thus, it attracts people who value multidisciplinary and transdisciplinary elements in their work. Public health is multidisciplinary because the many types of professional in this field contribute knowledge and skills from their own disciplines, yet it is also interdisciplinary because its practitioners must analyze, synthesize and harmonize links across disciplines into a coherent whole [5]. Because of this, its working environment is intellectually rich and challenging.
For its advocates, public health is a vocation, not an individual pursuit, and requires team effort; its fullest expression calls for a ‘whole of society’ approach [6]. Its practitioners formulate policies and develop initiatives that, ideally, are grounded in the health situation of a population, encompassing the principles of health promotion, health protection and disease prevention.
This essential interdisciplinary quality of public health drew the attention of a landmark report by the Institute of Medicine (IOM) of the National Academies in 2002 [7]. Focusing on the future of American public health in the 21st century, the report emphasized, inter alia, a population approach that considers determinants of health, building new intersectoral partnerships to draw on the perspectives and resources of diverse communities and actively engage them in action. Yet this is but one stream within a global renaissance in public health thinking; it is relevant to note that these were also central elements of the Ottawa Charter for Health Promotion, sponsored by the World Health Organization (WHO) in 1986, formulated by participants from over 40 countries [8].
In the year following its 2002 report, the IOM launched another major report for its mostly US audience, this being ‘Who will keep the public healthy? Educating Public Health Professionals for the 21st Century’ (2003) [9]. The report opened with the summary statement:
Many achievements in reducing mortality and morbidity during the past century can be traced directly to public health initiatives. The extent to which we are able to make additional improvements in the health of the public depends, in large part, upon the quality and preparedness of the public health workforce, which is, in turn, dependent upon the relevance and quality of its education and training.
The Ottawa Charter was transformative, calling for perspectives and actions that go well beyond the provision of health services. In particular, governments are considered accountable for the health consequences of their policies, or lack thereof, in all sectors (not just the Ministry of Health); this is called ‘healthy public policy’ [10]. The subsequent Bangkok Charter in 2005 [11] built upon this core value, emphasizing actions more applicable to less developed countries: invest in sustainable policies, actions and infrastructure to address determinants of health; build the capacity for policy development, leadership, health promotion practice, knowledge transfer and research, and health literacy; partner and build alliances with public, private, non-governmental and international organizations and civil society to create sustainable actions.
While all this was occurring, enormous technological innovation took place globally, especially in communications – e.g. the Internet, social media and mobile phones, to mention but three technological revolutions [12]. Climate change became a legitimate concern for everybody, including the public health community. The world became the ‘global village’ that Marshall McLuhan wrote about [13]. In a mere generation, our appreciation for the full range of globally applicable health determinants grew immeasurably, now seen more clearly as environmental and social, not so much as a function of our health care systems and their technological inputs and limits. As global communications, travel and trade facilitated the export of ‘Western’ lifestyles and other potential sources of health risk, the more fundamental relationships between poverty and health have become increasingly obvious in a world where such issues now transcend political boundaries.
The challenge for professional education is revolutionary; even as new technologies unlock an enormous potential for facilitating learning, education itself has become a commodity for internal and export markets, publishing houses, Internet providers and international aid agencies. In this context, public health professional education faces old and new challenges: in numerous countries it is still viewed as ‘an adjunct to the health care system’, a medically oriented system that deals mostly with ill health after it has occurred. This view is receding wherever there is insightful leadership with political support; increasingly, public health is now understood as a strategic force for a healthy population [14]. As stated by the IOM, ‘there is strong evidence that behaviour and environment are responsible for over 70% of avoidable mortality’ [7]. Health is mostly a function of working conditions, living circumstances and lifestyles. It is affected by economic and social policies, and by investing in healthy policies: ‘Health care is just one of the determinants’.
The health of populations has been well addressed at a global level by the WHO Commission on Social Determinants of Health (2008) [15]. Extrapolating from population health statistical data, the Commission drew attention to the extreme nature of health inequities both between and within countries, with such contrasts as: ‘In Sweden, the risk of a woman dying during pregnancy and childbirth is 1 in 17,400; in Afghanistan, the odds are 1 in 8’, and ‘maternal mortality is 3–4 times higher among the poor compared to the rich in Indonesia’. Whether between or within countries, such differences arise predominantly from the social environment into which people are born, and from how they live, grow, work and age. They are a reflection of the degree to which social justice exists between and within societies and are amenable to corrective actions that may range from policy interventions to programme development [16].
This renaissance in public health thinking is supported by the World Bank [17], and by the WHO Commission on Macroeconomics and Health [18]. Both bodies emphasize the importance of nations investing in their public health capacity: well-trained public health human resources lead to returns in health and economic development. However, public health within nations must not be left to the international community to define; it is primarily the responsibility of the countries themselves to determine their priorities. The global agenda should be viewed as complementary at best, while regions and countries must build their systems more assertively in accordance with their public health needs and with their own resources [19].
This includes building educational capacities and resources at a regional level. For example, the recent release of a new textbook titled Public Health in the Arab World[20] will greatly assist related higher education in this region. Edited by a team from the American University of Beirut, this book is the largest volume of public health literature to emerge from this region. Translated into Arabic by the WHO Regional Office for the Eastern Mediterranean, it attends to the social determinants of health with regional relevance, exploring this in relation to disease entities and the health of population groups; it addresses the context of war and violence and related issues of human security and community resilience; it covers health systems, health care delivery, and the context of political and social reform. The arrival of this book approaches in significance the longstanding role of Public Health and Preventive Medicine[21], the leading reference level public health text in the Americas, and that of the Oxford Textbook of Public Health[22], which plays much the same role in the UK and some Commonwealth countries. Although those texts are written for the global market, their relative strengths remain sensitive to their regional constituencies. It is to be expected that, in time, other regions will develop their own body of distinct, yet globally relevant, public health reference literature.
Building public health educational capacities also aligns with the Global Code of Practice on the International Recruitment of Health Personnel (2010) [23]. Although non-binding on member states and recruitment agencies, this code promotes principles and practices for ethical international recruitment of health personnel. It advocates the strengthening of information systems to support effective research into health human resource policy and planning in member countries.
Strategic Approaches
In theory, practice and teaching around the world, the core strategies of public health are converging. While these may be defined and grouped somewhat differently depending on the setting, a generic set adapted for the purpose of this review now follows [24]:
health assessment and disease surveillance – strategies critical for monitoring population health status, identifying the health needs of particular groups, detecting outbreaks of disease or other health-related issues, and assessing the effectiveness of public health interventions, programmes and services;
preventive interventions – strategies that include immunization, counselling, screening and early detection, and prophylactic or, in some cases, preventive treatments; this may include the development of new strategies based on intervention research;
health protection – strategies that protect people's health through legislation, regulation, inspection and, if necessary, enforcement and prosecution; these strategies emphasize the protection of environments that are critical for life and health (e.g. air, water, food), and protection of people from natural and man-made health hazards;
health promotion – strategies that range from health advocacy for change in public policy or private sector practices, over partnership building and coalition development, to education that helps people develop personal skills for health.
From an organizational perspective, it is the strategic framework itself that helps a public health department to move to the next step: to identify and build the system capacity requirements for success. In turn, all this should be reflected in public health educational capacity development.
Professional Competencies
Worldwide, and especially in developed countries, action is steadily being taken to advance professional competence as a central principle for all health professions, although this is rendered relatively more challenging for public health because of its multi- and transdisciplinary nature. Core competencies refer to those competencies required by all professionals in a given field; function-specific competencies include those required to perform certain functions [25]. Competency in public health thus requires the ability to apply disciplinary skills within defined roles for the benefit of the highest attainable standard of health for everybody.
This movement towards defining criteria for professional competence is taking place in part because it was all too common in the past (and still is in some settings) for individuals to be recruited or promoted within public health agencies based on outmoded concepts of professional qualification, seniority or even political considerations without attention to the adequacy of their knowledge, attitudes and skills in public health per se [26]. When this type of misappropriation occurs, it is to the detriment of the population and properly trained staff members alike. Increasingly, into the future, planners and policy makers will focus less on which professionals have traditionally performed certain public health functions, and more on the skills and competencies required to perform such functions; they will then identify the types of provider who have those skills [25].
Defining core competencies must necessarily be linked to the core strategic functions of public health, as outlined. This move to strengthen the public health human resources by defining competencies is taking place in many jurisdictions from subnational (state, province) to national and regional levels. Keeping in mind that these efforts must also be supported by assessment processes, this is an ongoing work-in-progress wherever it is underway.
The approach in the USA, under the auspices of the Association of Schools of Public Health (ASPH) and the Council on Linkages Between Academia and Public Health Practice, recognizes three tiers of personnel from entry level to senior managers across key domains, within which are defined specific professional and technical skills [27]. In addition to five disciplines (biostatistics, environmental health sciences, epidemiology, health policy and management, and social and behavioural sciences), the skills addressed include: analytical assessment, policy development and programme planning, communications, cultural competency, community practice, public health sciences, financial planning and management, systems thinking and leadership [28].
Interestingly, from a global public health perspective, the ASPH recently released a global health competency model designed to provide a framework for the abilities expected of master's-level students in global health programmes that will prepare them for successful performance in the global public health workforce [29].
Canada, in 2008, identified a set of seven competency themes: public health sciences; assessment and analysis; policy and programme planning, implementation and evaluation; partnership, collaboration and advocacy; diversity and inclusiveness; communication; and leadership. Thirty-six core competencies were released under these headings [30], each illustrated with at least one practice example for a front-line provider, a consultant/specialist or a manager/supervisor. A reference card (PDF, 1 page) is available to assist practitioners in applying the competencies [31].
Europe has been slower in developing competency statements than has North America, but it is making progress [32]. Under the auspices of the ASPH of the European Region, six core themes have emerged: methods; social environment and health; physical, chemical and biological environment and health; health policy, organization, management and economics; health promotion and prevention, and cross-disciplinary themes.
The WHO Regional Office for the Western Pacific is also moving in this direction, having defined characteristics for improving public health based on case studies in Fiji, Malaysia and Vietnam [33]. For the WHO Regional Office for South East Asia, core competency frameworks are emerging and are being aligned with different administrative levels of the health system [34]. Focusing on Latin America and the Caribbean, the Pan American Health Organization (Regional Office of the WHO) passed a resolution on essential public health functions in 2000 [35], and is now running courses that include content on core competencies [36]. There are implications here for other world regions; for example, it has been observed that similar sets of basic characteristics for improving public health are missing so far for the African continent [37], although it is reasonable to project that the remaining two WHO Regional Offices (the Eastern Mediterranean Regional Office and the Regional Office for Africa), which include the continent, will take a leadership role in this development.
In synthesis, there should be no doubt that public health professionals in all parts of the world must ensure that their competencies keep pace with advancing norms and expectations regionally and globally. Equally, public health agencies at all levels need to ensure that their recruitment and promotion standards respect this development; to do otherwise will undermine efforts to uplift the field as a whole. It is a logical extension that defining competencies requires commensurate development in capacities for related education and quality assurance.
Educational Foundations
Graduate Education as the Core of Public Health Professional Development
For more than half a century, most professional training in public health worldwide has been at graduate level. A large majority of Schools of Public Health still offer only graduate programmes. This stands in contrast to many other more vertically integrated professional fields (engineering, psychology, computer science, etc.), which emphasize an undergraduate degree in their respective field as the first step towards professional education. However, in all parts of the world, it is not the norm for individuals to begin public health studies at bachelor's degree level and then progress to a master's degree. Although this can happen where the pathway exists, public health could never achieve its multidisciplinary capacity if this were the main foundation.
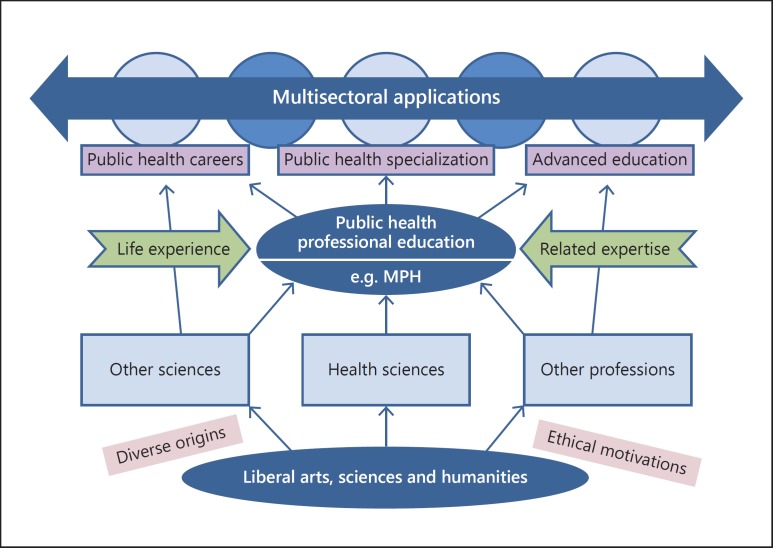
As with some other professional degrees such as the MBA and the MPA (Master of Business Administration and Master of Public Administration), previous education and experience provides a base upon which to acquire more advanced knowledge and skills for public health. Most individuals entering public health training therefore do so at master's level; their diversity in educational, disciplinary and professional backgrounds demonstrates the broad attraction of the field. In public health, as a multidisciplinary field, this approach to recruitment is highly valued as a form of ‘professional hybridization’, as figure 1 demonstrates.
Fig. 1.
Public health professional pathways.
In most countries, the Master of Public Health (MPH) degree, or its equivalent (e.g. Master of Science in Public Health, Master of Health Sciences), has become the most common professional entry level qualification for public health. With appropriate attention to continuing education, this level of formal qualification is sufficient for a lifetime of valuable work. When properly developed, the MPH degree is intellectually challenging – emphasizing active, student-centred learning, problem solving and the acquisition of skills essential to the practice of public health. Successful applicants are normally mature students who hold at least an undergraduate degree in a field relevant to public health – most often a health discipline such as medicine, dentistry, nursing, veterinary science or medical laboratory sciences, but maybe also in fields such as engineering, law, informatics and environmental sciences. Typically, every MPH student (at least in US accredited schools) pursues studies in the five core disciplinary areas: epidemiology; biostatistics; environmental and occupational health sciences; health policy and health services administration; and social and behavioural sciences. Beyond these disciplines there is scope for a range of applications from intervention research over indigenous health to global health, among others. This scope is normally tailored to the realities of a given setting, e.g. region or country, much of which is realized through practicums in which students are attached to public health operations, culminating in a ‘capstone project’ in which candidates demonstrate and document their acquired skills to apply public health sciences.
In advanced economies, with exceptions, a public health master's degree has become a virtual prerequisite for advancement within a public health leadership structure, because not only does the field require the skill set that comes with this, it should be designed to instil common core professional values and competencies. In addition to the MPH, specialized master's degrees and postgraduate diplomas in core public health subdisciplines are also available in such areas as: environmental health, epidemiology, health policy and management, health promotion, occupational health and safety, and public health nutrition, among others. Although, in contrast to the MPH, these occupy what could be considered ‘market niches’, they are in fact equally essential; a balanced public health capacity cannot thrive on the MPH alone.
As a corollary, some institutions offering specialized programmes experience pressure to broaden their scope to include an MPH degree as well, or even to modify what they do well to deliver an MPH as their degree outcome. However, this is not always in the best interests of the academic unit concerned, especially if an MPH (perhaps required for accreditation) is difficult to develop in their setting. Nonetheless, given the high profile now enjoyed by MPH degrees, and that these are usually obtained in a shorter time than a research-based Master of Science in a public health discipline, the ‘business case’ may be difficult to resist in an era when institutions of higher education are increasingly led by people committed to a market model. Nonetheless, academic units contemplating their potential to launch a public health-related graduate degree, taking into account their comparative advantages and deficits, should consider not only the MPH but also the option of a more specialized degree.
Higher qualifications are also obtainable, such as the Doctor of Public Health, which produces a broadly trained professional (a needed cadre, especially for leadership posts), or the Doctor of Philosophy, which emphasizes research in a subdiscipline. For candidates with a medical background, public health-oriented residency training programmes also exist in some countries, e.g. in Australia, Australasia, Canada, New Zealand, Pakistan [38], the UK and the USA; these integrate the equivalent of a master's degree (course work) with supervised training and sometimes a dissertation, followed by a written and oral comprehensive examination that leads to board certification or fellowship, a level broadly comparable to the Doctor of Public Health. These programmes tend to have a particular emphasis – e.g. preventive medicine, community medicine, public health medicine – and take between 3 and 5 years to complete, depending on the country. A pathway for non-medical graduates to achieve this certification exists in the UK, although not so far elsewhere. While such higher qualifications may be required for academic leadership posts, for most operational roles individuals who combine a prior qualification from another field with a public health master's degree are the mainstay, and can advance to senior levels on merit.
Undergraduate Programmes Relevant to Public Health
The past two decades have witnessed a surge in bachelor's degree level education relevant to public health. Mostly this has taken place in North America [39], although a similar development is now being advocated for the European region [40]. There are three broad rationales:
to promote a higher level of health literacy in the population at large, and to recognize public health as a legitimate option within a liberal arts education;
to provide a platform for students seeking entry-level employment in public and private health agencies, thereby to meet the market needs for individuals with relevant training, rather than to recruit junior administrative and technical staff mostly from non-health fields;
to serve the undergraduate needs of students who discover at an early stage that they wish to pursue higher degrees and professional training in public health or a related discipline.
The first rationale was initially advocated in 1976 by epidemiologist Abraham Lilienfeld, and gave rise to an undergraduate public health programme at Johns Hopkins University. This advocacy was renewed in 1987 by another epidemiologist, David Fraser, then President of Swarthmore College [41]. In 2003, the IOM recommended that ‘all undergraduates should have access to education in public health’ [42]. In 2006, the Association of American Colleges and Universities launched an initiative titled ‘The educated citizen and public health’ [43] with this statement:
An understanding of public health is a critical component of good citizenship and a prerequisite for taking responsibility for building healthy societies. At its best, the study of public health combines the social sciences, sciences, mathematics, humanities, and the arts. At the same time, it serves as a vehicle for the development of written and oral communication skills, critical and creative thinking, quantitative and information literacy, and teamwork and problem solving. It incorporates civic knowledge and engagement – both local and global – intercultural competence, and ethical reasoning and action, while forming the foundation for lifelong learning. The study of public health, in other words, models a capacious vision of liberal education.
It is thus argued that providing this as a competitive option for individuals entering university, even if it is not their ultimate career path, elevates awareness and general knowledge of issues that affect individuals, families and communities. The supplementary social gain is to promote health literacy, and the development of a more vibrant civil society in the health field [44].
Regarding the second rationale, it is an unfortunate fact of life in many health-related agencies around the world that – in the relative absence of appropriately trained individuals – they must resort to recruiting persons with no health-related education, although qualified in other fields, e.g. commerce, art, music or religious studies. For such recruits, on-the-job training is then supplied. This is a chronic problem in many countries, with implications for quality and cost-effectiveness. By contrast, possession of a bachelor's degree in health and community studies (for example) would enable entry-level employees at a health agency not only to understand more readily its scope and purpose, but simultaneously to bring relevant orientation and valuable related skills.
The third rationale is to provide a pathway for candidates who wish to move directly to a master's education having completed a bachelor's degree. However, this brings us full circle, i.e. to re-emphasize that this avenue cannot supply all human resource needs for the public health market, a field that needs many of its recruits to be prepared in another complementary discipline which may be rigorously hybridized with postgraduate education in public health.
Accreditation of Public Health Educational Programmes
Although core strategic frameworks and competency guidelines must be determined by each jurisdiction according to their priorities, the education needed to develop the public health human resources is similar in most countries. This raises the prospect of common accreditation schemes.
For example, the USA has maintained such a system for many years, which operates globally through a Council on Education for Public Health (CEPH). Although these are primarily national standards for the USA [45], it is noteworthy that in Canada, which does not yet have an accreditation system, at least one Canadian school of public health (SPH) has chosen this route [46]; most others so far have not. Similarly, the American University in Beirut has achieved CEPH accreditation. CEPH-accredited schools may join an ASPH, with provision for associate members (schools that intend to seek accreditation with the CEPH) [47].
A European Agency for Accreditation in Public Health Education (APHEA) was launched in 2010, with the aim of accrediting MPH programmes. Its development over two decades was fostered by the ASPH of the European Region [48]. Like its American counterpart (CEPH), membership is possible for schools based outside the region. The first school to undergo APHEA accreditation is the London School of Hygiene and Tropical Medicine (founded 1899, and an acknowledged leader in the field), which achieved accreditation of three distinct MPH programmes during 2012 [49].
There are practical advantages to aligning with an accreditation body that promotes common standards. Belonging to such a network acts as an institutional stimulus to stay current with one of the mainstreams in public health, and brings desired recognition to member schools. For some students (those seeking employment in the USA) it constitutes a competitive advantage as this can be a job requirement, a feature used by some institutions as part of their marketing strategy.
There are also potential disadvantages to accreditation: norms developed in the USA or Europe may not be appropriate to all settings; some requirements may be excessive when judged against locally or nationally determined priorities, while others may be insufficient. Thus, it is not desirable that accreditation norms should constrain an institutional response to a nationally determined need, or tailor a response to that need, taking into account resource limitations.
Clearly, then, to align with public health accreditation guidelines must be a matter for each programme or institution to decide. However, for schools and programmes to develop without regard for accreditation guidelines, at least as a reference point, may encourage an unstandardized approach that could result in questionable quality and failure of some to keep pace with evolving standards, or to be manipulated away from their original focus, especially if located in a faculty whose mission may not be mainstream public health. For example, the writer has observed some departments based in medical schools steadily drift away from their original population health mandates to become primarily a support base for researchers in clinical departments; the same could occur in other faculties. Lack of a standard educational core also poses difficulties from a planning standpoint: for example, the Commission on Education of Health Professionals for the 21st Century found it unfeasible to construct global estimates of public health graduates because of data and definitional limitations [50]. The issue here is not that all schools and programmes everywhere must necessarily align with accreditation standards, but that the emergence of standards – first in North America, now in Europe, and potentially elsewhere – is a sound development from a global perspective as it helps to ‘anchor the field’.
International Variations in Public Health Professional Education
Thus, while a case exists for some level of international standardization for graduate- or professional-level public health education and accreditation, this does not mean that ‘one size (or shape) fits all’ when it comes to designing a professional education capacity for particular settings, nor should there be. For example, the Commission on Education of Health Professionals for the 21st Century examined leading public health institutes in three Arab settings and found that they were uniquely shaped by national contexts, ranging from a strong state in Egypt over civil conflict in Lebanon to absent state structures in occupied Palestinian territory [2] – and, consequently, all adopted different approaches. Similarly, the Public Health Foundation of India is a public-private partnership bringing together pooled resources from the Indian government and private philanthropy to address India's priority health challenges. The Foundation is crafting partnerships with four state governments to create eight public health training institutes in the country. In Bangladesh, the James P. Grant School of Public Health launched by BRAC University (part of the world's largest non-governmental organization, NGO) offers an innovative 12-month curriculum for an MPH degree that begins with 6 months on its Savar rural campus, acquiring basic public health skills in rural health action, followed by the remaining 6 months of thematic and research training. Importantly, both of these South Asian schools are developing curricula shaped to national and global priorities, neither adopting wholesale a Western model of public health education [2].
Human Resource Planning for Professional Public Health Education
‘Health human resources’ is defined by the WHO as ‘all people engaged in actions whose primary intent is to enhance health’ [51]. This includes all people who contribute to a functional health system: those who provide health care directly and those (like public health professionals) who address the underlying health determinants, and others who support the overall effort in other ways [52]. The public health contribution includes: assessing the health status of a particular population on an ongoing basis; conducting investigations into priority health conditions so as to design effective public health interventions; facilitating community health and development services, and health programme planning and evaluation.
Health human resources planners generally agree that needs assessment is a crucial first step for any educational initiative to be successful [53]. Such an exercise is intrinsic to the planning cycle, as represented by the four classical questions [54]: (1) Where are we? (2) Where do we want to be? (3) How will we get there? (4) How will we know we are getting there? Needs assessment is achieved by answering questions 1 and 2, which can also be referred to as a ‘gap analysis’. Needs assessment techniques can range from simple to complex, such as the use of mathematical models and computer-based simulations. For the purpose of this review, three approaches to assessing public health educational needs are now outlined.
Situation Analysis to Determine the Status Quo
The status quo may be assessed by interviewing key informants and reviewing relevant documents; the findings of such an exercise may then be compared with the conditions desired. Take for example, the findings of the WHO and of the World Bank in reference to the state of public health in the Middle East region, as quoted below:
One of the main challenges facing public health in the … region is the recruitment and retention of appropriate skills and expertise, in terms of both quality and quantity [55].
This deficit in the capability to assess and monitor population health will have to be addressed if effective plans for public health capacity building are to be put in place [56].
Implicit in all this is the actual health situation facing a region or a country: when so much morbidity and mortality is now related to environment and human behaviour and therefore largely preventable, improving the situation will not be advanced by continuing to produce professionals concerned only with patient care after illness has emerged as a consequence. Instead, there is an overarching need to improve how we address health determinants; this requires new cadres of professionals more appropriately trained in public health measures.
Market Surveys to Determine Perceived Need/Demand for Graduates
In conducting such surveys, designing the appropriate sampling frame is a critical first step; all potential employment agencies should be included. In the diverse field of public health, one must ‘think out of the box’: well beyond hospitals, medical care, and the more traditional public sector and educational institutions, also to be considered are the intergovernmental, non-governmental and private sectors – for example, the WHO, UNICEF (United Nations Children's Fund), UNFPA (United Nations Population Fund), the International Red Cross and Red Crescent Societies as well as other NGO involved in health development and humanitarian relief. The private sector also needs this expertise to meet its responsibilities for safe and healthy workplaces and the environment (consider e.g. the oil, gas and chemical industries, agriculture, transportation and manufacturing). Consulting firms need this expertise to be competent in related planning, monitoring and evaluation.
Equally, before determining the perceived need or demand for graduates, potential employers must understand what they will be capable of achieving that graduates of other (existing) programmes are less able to do. This is a challenge in settings where a particular skill set has not been available before; its relevance can be difficult even for seasoned operational managers to comprehend. There are parallels to this across the health sciences – for example, the resistance by many physicians to evidence-based medicine, despite the emergence of Cochrane reviews.
Public health market surveys may be designed to focus on particular periods, from the present to various planning horizons, e.g. 5, 10 or 15 years. They should be conducted with rigour, and with sufficient follow-up to ensure an acceptable response rate. Quality checks are required to ensure that the response is provided by someone who is able to provide a valid and reliable answer.
Application of International Norms
Using this method, experience from one world setting is extrapolated to another. For example, the Commission on Education of Health Professionals for the 21st Century (2010) [2] attempted to estimate the number of degree-granting institutions globally, although lacking standard definitions that would render such comparisons valid and reliable. From this rough exercise, measures of frequency emerged to reveal that some world regions are less well supplied with higher education in public health disciplines than others. For example, 111 recognizable programmes were identified in Asia (excluding high-income Asian-Pacific countries), this for a population of 4.2 billion, or 1 such programme per 38 million people; by contrast, South America had 82 programmes for 385.7 million, or 1 per 4.7 million. At face value, this implies that such programmes are about 8 times more available in South America than in most of mainland Asia.
Extrapolation may be done at various levels of disaggregation, from SPH to public health degree programmes to both these levels combined, and to numbers of students enrolled. For example, applying US data from the CEPH and the Graduate School Guide [45,57], 50 accredited schools of public health are in place, all offering a core MPH programme, and another 92 accredited MPH programmes are located in other faculties. Combining accredited and non-accredited schools and programmes, 290 such capacities thus exist in the USA – a ratio of 1 per 1.3 million. Now consider the following two settings, for illustrative comparison.
In the English-speaking Caribbean, the University of the West Indies launched an MPH programme in Trinidad and Tobago (population 1.3 million) in 2009, with assistance from the University of Alabama at Birmingham (USA) [58]. Mindful that this school will serve as a resource for the English-speaking Caribbean (population 7 million) complementing the long-standing MPH programme at the UWI in Jamaica, the combined ratio of two such schools comes to approximately 1 per 3.5 million people, midway between the US and South American ratios. This will have the effect of providing relevant public health education at lower cost for people of the West Indies, most of whom in the past have had to study abroad to obtain such education at much higher cost.
The second setting encompassed selected Middle Eastern countries. In Lebanon (population 4.3 million), the American University of Beirut Faculty of Health Sciences (an accredited SPH under the CEPH) represents a ratio of 1 per 4.3 million people, again – like the English-speaking Caribbean – not so far off the US ratio. However, the provision for public health education in Egypt (population 85 million) by the High Institute of Public Health at Alexandria University represents less access (ratio less than 2% of that of the USA). Now, examining the Arab Near East (which groups Kuwait, Saudi Arabia, the United Arab Emirates, Oman, Qatar, Bahrain, Yemen, Egypt, Syria, Jordan, Palestine, Lebanon and Iraq), where approximately 10 schools and/or programmes are in place, a ratio of 1 per 22.2 million emerges, more equitable than in Egypt, but only about one fifth the US level of provision.
These informal analyses are purely illustrative of how international comparisons may help to assess the adequacy of provisions for higher education in public health, and are not intended to advocate the application of US ratios per se. Nonetheless, similar indicative comparisons could be done for other world regions such as South Asia and Sub-Saharan Africa, most likely finding a few countries having well-developed educational resources within an overall regional deficit.
In an analysis at the level of graduates, a recent Canadian report states that each year some 500 new graduates receive public health qualifications at master's level [59]. This is in the context of a population of 34.5 million people, or approximately 14 graduates per million. This ratio could be applied for illustrative purposes to countries which lack such a programme; for example, if applied to Jordan (population 6.5 million), it would be 91, for Iraq (population 32 million) 450, for Egypt 1,217, and so on.
Continuing Professional Education
Public health professionals in countries lacking an educational infrastructure for the field almost invariably have limited access to appropriate continuing education: to travel abroad is costly, and even when possible, those continuing professional education (CPE) offerings may not be well suited to the needs of underserved settings. This recognized, a middle ground can sometimes be developed where an external institution may engage in partnering with ministries of health and/or universities to provide a critical infusion of missing capacities, e.g. by conducting local workshops. Such initiatives usually require grant support and should address negotiated priority issues.
For example, a new regional network is emerging in the Middle East: EMPHNET (the Eastern Mediterranean Public Health Network). EMPHNET in turn belongs to a global group of initiatives supported by the US Centers for Disease Control and Prevention and its associated Training Programs in Epidemiology and Public Health Interventions Network (TEPHINET) [60]. Launched in 2009 and headquartered in Amman, Jordan, members of the network include Field Epidemiology Training Programs (FETP) in the Eastern Mediterranean region, and field-based epidemiology and public health training programmes in Afghanistan, Egypt, Iraq, Jordan, Morocco, Pakistan, Saudi Arabia and Yemen. Created in 1997, TEPHINET itself (the parent organization) is a professional network of FETP located in 53 countries around the world. TEPHINET aims to strengthen public health capacity internationally by training field epidemiologists through an applied apprenticeship programme. Trainees of FETP master a set of core competencies that are vital to the practice of public health, while providing a valuable public health service to their countries and regions.
The emergence of on-line courses is also a promising new development for continuing education, with certificate and degree programmes available from several reputable institutions. However, this is no substitute for building an educational infrastructure within a country, although it may indeed also be part of it. Such developments as TEPHINET and on-line courses make sense if viewed as a component of, or adjunct to, internal capacity development, not a replacement for it.
Within the capacity that needs to be developed in virtually all countries, a CPE programme will normally offer certificate-level credentials, usually based on completion of short courses, geared towards adult learners. Such a programme must cater to distinct needs – for example, to augment the knowledge and skills of individuals working in public health, but who lack formal qualifications, and/or to address the CPE needs of persons with formal qualifications. Certificates could be developed in areas of national priority, defined by each country according to its situation.
Health Literacy and Community Outreach
To clarify terms: health literacy is the ability to read, understand and act on health information. Health illiteracy conversely would be the inability to read, understand and act on health information. Health literacy takes us into the domain of ‘determinants of health’, of which health care is only one ingredient; social and environmental determinants are more important. Health literacy therefore needs to encompass why people become ill in the first place, as well as what they do once ill health arises. A useful framework for appreciating the scope of this concept has been published elsewhere [61].
There is a great need in underserved settings to address health literacy at the community level. This cannot afford to wait for new generations of students to complete a degree programme and eventually make an impact on society. It is of equal or greater importance to address this need now by engaging the whole of society through community outreach programmes; these can be developed by educational institutions, which in turn can also provide a valuable forum for student involvement and education, and provide an avenue for relevant public health research. In this way an educational institute can give substance to its community service mission. This duly recognized, developing community outreach to enhance health literacy in a population is a huge topic, and to explore it further in this review is beyond our present scope.
The Lessons of Modern History
Health and life expectancy in many world regions improved dramatically during the 20th century. In Western industrialized countries, life expectancy increased from less than 45 to over 75 years of age; epidemiological models reveal that 25 of the 30 years of life expectancy added can be attributed to public health measures such as better nutrition, sanitation and safer housing. Medical care, though important, contributed only 5 years of the gain in life expectancy [62,63]. While the social mechanisms are complex, these gains in life expectancy appear to have been an empowering influence in the evolution of expectations regarding the quality of life, including the roles of families and society in enabling positive choices; they can be viewed as societal accomplishments. Going forward, it is important to recognize that future population health challenges – whether they be non-communicable diseases, mental disorders, violence or related to climate change or the development of extreme economic inequities – also will not be solved primarily by a medical response. Increasingly, we must build on success and solve these issues also through public health strategies: health promotion, health protection, disease prevention and control.
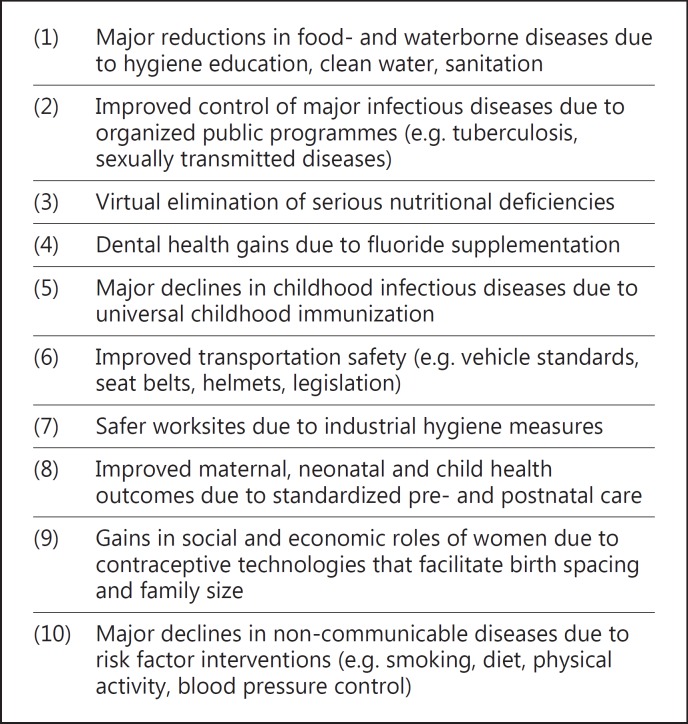
As the 21st century dawned, institutions in several Western countries reviewed their public health accomplishments over the previous hundred years [64,65,66]. These are mirrored to a substantial degree in other high-income nations, and similar impacts are now occurring in economically less advanced nations through efforts underway to address social and environmental conditions for health. A vast literature documents the top ten health gains summarized in the accompanying figure (fig. 2); this set is a blend of two overlapping lists from Canada and the USA. None of these achievements came easily; they were the result of persevering efforts by people working at all levels from the grassroots to national leadership, supported by an intensive and extensive research and development effort committed to building a sound evidence base.
Fig. 2.
Ten leading public health accomplishments in the 20th century. The North American scenario.
The Role of Research and Development in Public Health Education
According to a pioneering 1990 report of the international Commission on Health Research for Development, ‘strengthening research capacity in developing countries is one of the most powerful, cost-effective, and sustainable means of advancing health and development’ [67]. In this context, health science research must be viewed as a broad and robust concept that goes well beyond biomedical and clinical research to embrace public health research. This includes epidemiological and related public health research, health systems research, health policy, economics and health services research, as well as other forms of relevant operational research.
Ensuring that research outputs are relevant is where the Essential National Health Research concept serves as a model, by linking research to national priorities, policies and programmatic applications [68]. Now advocated in all regions of the world, the principle is to link research with development needs, which is equally relevant to regional, state-provincial, local and institutional levels, although needs and priorities are not synonymous across these levels.
The research process is implicit within functions that lie at the core of public health: planning, evaluation, surveillance, investigation, and problem and pathway analyses. In this sense, the development and application of operational research skills is fundamental to effective and efficient public health programmes [29]. It follows that building public health educational capacity requires building robust research and development skills among students, practitioners and faculty alike. This includes a balanced range of quantitative, qualitative and mixed-method research approaches that will help to build evidence-based, effective and evaluable public health initiatives. Building capacity for professional public health education necessitates research into related human resource planning – as presented earlier in this review – and a new level of effort to translate public health research findings into effective, efficient and sustainable health policies and programmes [69].
However, the evidence-to-performance pathway is a complex process shaped by numerous influences, many of which work against prompt sharing of ‘good practices’. A major challenge is the need for more effective and efficient communication of research (mainly concentrated within universities) to policy makers (mostly based in government). Responsibility for this inefficient pathway belongs to both sides, according to health policy research carried out in four countries [70], which revealed that policymakers tended to view research as lacking in clear recommendations, while researchers tended to see such decision-makers as lacking understanding or respect for their work. Public health capacity development also entails improving this knowledge-to-policy pathway. It depends on developing new mechanisms for supporting applied research and on developing appropriate forms of research translation and dissemination [71].
The Importance of Coalition Building
To avoid the development of one more ‘ivory tower’, when building educational capacity one should recognize and involve public health coalitions. The history of public health movements internationally has long embraced a civil society component, in the form of organized professional and lay networks. Such organizations (legally constituted as ‘associations’) have been a vital source of advocacy for the public good, from improved social conditions over child health advocacy to traffic safety measures, and a contemporary force in addressing the underlying determinants of non-communicable diseases. When individuals join a public health association, they do so as individuals – not in any official capacity that they may otherwise hold. They may serve as an elected board member, lead a working group or contribute in other ways. A properly constituted association may interact formally with a Ministry of Health and other entities. Educational leaders need to be part of this process as well, to help build the coalition.
When a national public health association is formed in a country, it may join larger networks such as, to take a British example, a National Council for Voluntary Organisations [72]. Many national associations also become institutional members of the World Federation of Public Health Associations (WFPHA) [73]. Accredited as an NGO in official relations with the WHO, the WFPHA facilitates information sharing and technical support, thereby helping national associations to avoid obstacles they might otherwise encounter.
Similarly, there is a need to improve intergovernmental collaboration on public health issues; the emergence of an International Association of National Public Health Institutes (IANPHI) as a global movement of governmental public health agencies mirrors the existence of the longer-established WFPHA. While the WFPHA is more of a ‘people-to-people’ network, IANPHI can be legitimately described as an ‘institution-to-institution’ approach [74]. IANPHI spearheads improvements in national public health systems through peer-assistance evaluation, grant support and efforts focused on NPHI advocacy, collaboration and sustainability; its main emphasis is on capacity building which (by definition) includes relevant educational development.
Conclusion
Educational planning for public health professionals is critically important in all world regions. Like the best of any such planning, it must be needs-based and evidence-driven, focused on the development of professional competencies appropriate to the settings for which they will be applied. This effort depends on developing a health human resource research capacity. All this duly acknowledged, it is also important that external reference points are developed, such as by alignment with relevant accreditation schemes or participation in the work of coalitions which share a common purpose in developing and promoting the interests of the field. Ultimately, public health educational planning must include a vision for everyone involved: from front-line workers with the orientation and expertise to work with local communities to develop strategies that work, to specialized professionals and high-level generalists, leaders at all levels. It is important that all nations assess their public health human resource needs and develop the ability to deliver this capacity, and not depend on other countries or regions to supply it. The health prospects of all populations, now and in the future, require this vision and these actions. The ultimate beneficiaries comprise most people around the world; their future depends on whether their nations listen to their voices and respond with health initiatives that meet their needs and help them make sound decisions about their own health.
Acknowledgements
This work is a by-product of reviews conducted in support of public health capacity building at Kuwait University. Debra Nanan, MPH, Pacific Health & Development Sciences Inc., critiqued several iterations, and Dr. Joseph Longenecker, Kuwait University, encouraged its development. The views presented are those of the author and do not necessarily reflect those of the University.
References
- 1.White F, Stallones L, Last JM. Global Public Health: Ecological Foundations. New York: Oxford UP; 2013. pp. xiii–xiv. [Google Scholar]
- 2.Bhutta ZA, Chen L, Cohen J, et al. Education of Health Professionals for the 21st Century: a global independent Commission. Lancet. 2010;375:1137–1138. doi: 10.1016/S0140-6736(10)60450-3. [DOI] [PubMed] [Google Scholar]
- 3.General Medical Council Tomorrow's dυoctors. 2009 http://www.gmc-uk.org/TomorrowsDoctors_2009.pdf_39260971.pdf (accessed February 25, 2012).
- 4.Liaison Committee on Medical Education Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. 2013 http://www.lcme.org/functions.pdf (accessed April 24, 2013).
- 5.Choi BCK, Pak AWP. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy. 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29:351–364. [PubMed] [Google Scholar]
- 6.Canadian Agri-Food Policy Institute A ‘whole-of-society’ approach to an integrated health and agri-food strategy. http://www.capi-icpa.ca/converge-summ/five.html (accessed April 4, 2013).
- 7.Institute of Medicine . The future of the public's health in the 21st century. Washington: National Academies Press; 2003. http://www.nap.edu/openbook.php?record_id=10548&page=424 (accessed March 25, 2013). [Google Scholar]
- 8.World Health Organization The Ottawa Charter for Health Promotion. 1st International Conference on Health Promotion, Ottawa, 1986. http://www.who.int/healthpromotion/conferences/previous/ottawa/en/ (accessed March 26, 2013).
- 9.Gebbie K, Rosenstock L, Hernandez LM. Educating Public Health Professionals for the 21st Century. Washington: National Academies Press; 2003. Who Will Keep the Public Healthy? http://www.nap.edu/openbook.php?record_id=10542&page=266 (accessed March 24, 2013). [PubMed] [Google Scholar]
- 10.World Health Organization Ottawa Charter for Health Promotion: 1st International Conference on Health Promotion Ottawa, 1986 – WHO/HPR/HEP/95.1. http://www.who.int/hpr2/archive/docs/ottawa.html (accessed February 28, 2012).
- 11.World Health Organization Bangkok Charter for Health Promotion in a Globalized World. 2005. http://www.who.int/healthpromotion/conferences/6gchp/bangkok_charter/en/ (accessed March 26, 2013).
- 12.de Leeuw E, Tang KC, Beaglehole R. Ottawa to Bangkok: health promotion's journey from principles to ‘glocal’ implementation. Health Promot Int. 2006;21(suppl 1):1–4. doi: 10.1093/heapro/dal057. [DOI] [PubMed] [Google Scholar]
- 13.McLuhan M. Letters of Marshall McLuhan. New York: Oxford UP; 1987. [Google Scholar]
- 14.White F. What's new in public health? Med Princ Pract. 2012;21:505–507. doi: 10.1159/000342566. [DOI] [PubMed] [Google Scholar]
- 15.Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Geneva: World Health Organization; 2008. http://whqlibdoc.who.int/publications/2008/9789241563703_eng_contents.pdf (accessed June 9, 2013). [DOI] [PubMed] [Google Scholar]
- 16.White F, Stallones L, Last JM. Global Public Health: Ecological Foundations. New York: Oxford UP; 2013. p. 131. chap 5: Assessing population health. [Google Scholar]
- 17.World Bank Group World Development Report 1993: investing in health. 1993. http://www-wds.worldbank.org/external/default/main?pagePK=64193027&piPK=64187937&theSitePK=523679&menuPK=64187510&searchMenuPK=64187283&siteName=WDS&entityID=000009265_3970716142319 (accessed February 10, 2012).
- 18.World Health Organization . Macroeconomics and health: investing in health for economic development. Geneva: World Health Organization; 2001. www.whqlibdoc.who.int/publications/2001/924154550x.pdf (accessed February 10, 2012). [Google Scholar]
- 19.John TJ, White F. Public health in South Asia. In: Beaglehole R, editor. Global Public Health: A New Era. Oxford: Oxford UP; 2003. pp. 172–190. [Google Scholar]
- 20.Jabbour S, Giacaman R, Khawaja M, et al. Public Health in the Arab World. Cambridge: Cambridge UP; 2012. [Google Scholar]
- 21.Wallace RB, editor. Maxcy-Rosenau-Last: Public Health and Preventive Medicine. ed 15. New York: McGraw Hill; 2008. [Google Scholar]
- 22.Detels R, Beaglehole R, Lansang MA, et al., editors. Oxford Textbook of Public Health. ed 5. Oxford: Oxford UP; 2009. [Google Scholar]
- 23.World Health Organization . International recruitment of health personnel: draft global code of practice. Geneva: Resolution 63rd World Health Assembly; 2010. http://apps.who.int/gb/e/e_wha63.html (accessed June 7, 2012). [Google Scholar]
- 24.Ministry of Health Services Public health renewal in British Columbia: an overview of core functions in public health. http://www.health.gov.bc.ca/public-health/pdf/phrenewal.pdf (accessed February 14, 2012).
- 25.Joint Task Group on Public Health Human Resources . Building the public health workforce for the 21st century: a pan-Canadian framework for public health human resources planning. Public Health Agency of Canada; 2005. [Google Scholar]
- 26.White F, Stallones L, Last JM. Global Public Health: Ecological Foundations. New York: Oxford UP; 2013. chap 8: Comparative organization and function of public health systems. [Google Scholar]
- 27.Council on Linkages between Academia and Public Health Practice Core competencies for public health professionals, adapted 2010. http://www.phf.org/programs/council/Pages/default.aspx (accessed January 16, 2012).
- 28.Association of Schools of Public Health MPH core competency model, updated 2010. http://www.asph.org/document.cfm?page=851 (accessed February 9, 2012).
- 29.Association of Schools of Public Health Global health competency model. 2011. http://www.asph.org/document.cfm?page=1084 (accessed June 9, 2013).
- 30.Public Health Agency of Canada Core competency statements. 2013. http://www.phac-aspc.gc.ca/php-psp/ccph-cesp/stmts-enon-eng.php (accessed April 19, 2013).
- 31.Public Health Agency of Canada Core competencies for public health in Canada, release 1.0 (reference card). http://www.phac-aspc.gc.ca/php-psp/ccph-cesp/pdfs/zcard-eng.pdf (accessed April 19, 2013).
- 32.Birt C, Foldspang A. Public health capacity building: not only the property of the medical profession. Eur J Public Health. 2009;19:232–235. doi: 10.1093/eurpub/ckp069. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization Regional Office for the Western Pacific . Essential Public Health Functions: A Three-Country Study in the Western Pacific Region. Manila: World Health Organization; 2003. [Google Scholar]
- 34.World Health Organization Accreditation guidelines for educational/training institutions and programmes in public health: report of the regional consultation, Chennai, India, 30 January to 1 February 2002. New Delhi, 2002. http://whqlibdoc.who.int/searo/2002/SEA_HMD_213.pdf (accessed April 22, 2013).
- 35.Pan American Health Organization 42nd Directing Council Essential public health functions, CD42/15 (in English). 2000. http://www1.paho.org/english/gov/cd/cd42_15-e.pdf (accessed April 22, 2013).
- 36.Pan American Health Organization . PAHO launches course on Essential Public Health Functions on the virtual campus. Washington: Pan American Health Organization/World Health Organization; 2013. http://www.paho.org/hq/index.php?option=com_content&view=article&id=8423%3Aops-lanza-curso-sobre-funciones-esenciales-de-salud-publica-en-el-campus-virtual&catid=1443%3Anews-front-page-items&Itemid=223&lang=en (accessed April 22, 2013). [Google Scholar]
- 37.Bjegovic-Mikanovic V, Czabanowska K, Flahault A, et al. Policy summary: addressing needs in the public health workforce in Europe. Association of Schools of Public Health in the European Region; 2012. http://2011.aspher.org/old/pg/file/read/10084/policy-summary-addressing-needs-in-the-public-health-workforce-in-europe-draft-for-consultation (accessed April 21, 2013). [Google Scholar]
- 38.White F. Community medicine: a specialty whose time has come. J Coll Physicians Surg Pak. 2001;11:733–735. [Google Scholar]
- 39.Riegelman RK, Albertine S. Undergraduate public health at 4-year institutions: it's here to stay. Am J Prev Med. 2011;40:226–231. doi: 10.1016/j.amepre.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 40.Tulchinsky TH, Goodman J. The role of schools of public health in capacity building. J Public Health (Oxf) 2012;34:462–464. doi: 10.1093/pubmed/fds045. [DOI] [PubMed] [Google Scholar]
- 41.Fraser DW. Epidemiology as a liberal art. N Engl J Med. 1987;316:309–314. doi: 10.1056/NEJM198702053160605. [DOI] [PubMed] [Google Scholar]
- 42.Gebbie K, Rosenstock L, Hernandez LM. Educating Public Health Professionals for the 21st Century. Washington: National Academies Press; 2003. Who Will Keep the Public Healthy? p. 144. [PubMed] [Google Scholar]
- 43.Association of American Colleges and Universities The educated citizen and public health. 2008. http://www.aacu.org/public_health/index.cfm (accessed February, 2012).
- 44.White F. A voluntary perspective on health promotion. Health Promot. 1986;1:429–436. [PubMed] [Google Scholar]
- 45.Council on Education for Public Health. http://www.ceph.org/ (accessed February 19, 2012).
- 46.University of Alberta School of Public Health Accreditation. http://www.publichealth.ualberta.ca/about_us/accreditation.aspx (accessed April 3, 2013).
- 47.Association of Schools of Public Health Members. http://www.asph.org/document.cfm?page=200 (accessed February 19, 2012).
- 48.Otok R, Levin I, Sitko S, et al. European accreditation of public health education. Public Health Rev. 2011;33:30–38. [Google Scholar]
- 49.Agency for Public Health Education Accreditation London School of Hygiene and Tropical Medicine: first School of Public Health to undergo accreditation by APHEA. 2012. http://2011.aspher.org/old/pg/blog/read/11778/london-school-of-hygiene-and-tropical-medicine-first-school-of-public-health-to-undergo-accreditation-by-aphea (accessed March 23, 2013).
- 50.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 51.World Health Organization . The World Health Report 2006: working together for health. Geneva: World Health Organization; 2006. http://www.who.int/whr/2006 (accessed June 7, 2012). [Google Scholar]
- 52.White F, Stallones L, Last JM. Global Public Health: Ecological Foundations. New York: Oxford UP; 2013. chap 8: Comparative organization and function of public health systems, pp 234–274. [Google Scholar]
- 53.Berger N.Needs assessment in human resource development in Berger N (ed): Human Resources and Their Development. http://www.eolss.net/Sample-Chapters/C11/E1-10-02-01.pdf (accessed November 14, 2012).
- 54.White F. Capacity-building for health research in developing countries: a manager's approach. Pan Am J Public Health. 2002;12:165–172. doi: 10.1590/s1020-49892002000900004. [DOI] [PubMed] [Google Scholar]
- 55.Pierre-Louis AM, Akala FA, Karam HS. Public Health in the Middle East and North Africa: Meeting the Challenges of the Twenty-First Century. Washington: World Bank; 2004. [Google Scholar]
- 56.Akala FA, El-Saharty S. Public-health challenges in the Middle East and North Africa. Lancet. 2006;367:961–964. doi: 10.1016/S0140-6736(06)68402-X. [DOI] [PubMed] [Google Scholar]
- 57.PhD's Public Health Schools Master's and PhD programs in Public Health. http://graduate-school.phds.org/find/programs/public-health (accessed November 20, 2012).
- 58.University of the West Indies UWI Launches Master of Public Health (MPH) programme. News Releases, Oct 28, 2009. http://sta.uwi.edu/news/releases/release.asp?id=396 (accessed April 24, 2013).
- 59.Massé R, Moloughney B. New era for schools and programs of public health in Canada. Public Health Rev. 2011;33:277–288. [Google Scholar]
- 60.TEPHINET: Training Programs in Epidemiology and Public Health Interventions Network. http://www.tephinet.org/ (accessed October 9, 2012). [DOI] [PMC free article] [PubMed]
- 61.Peerson A, Saunders M. Health literacy revisited: what do we mean and why does it matter? Health Promot Int. 2009;24:285–296. doi: 10.1093/heapro/dap014. [DOI] [PubMed] [Google Scholar]
- 62.Bunker J, Frazier HS, Mosteller F. Improving health: measuring effects of medical care. Milbank Q. 1994;72:225–258. [PubMed] [Google Scholar]
- 63.Schroeder SA. We can do better: improving the health of the American people. N Engl J Med. 2007;357:1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 64.Centers for Disease Control and Prevention Ten great public health achievements: United States, 1900–1999. MMWR. 1999;48:241–243. http://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm (accessed February 11, 2012). [Google Scholar]
- 65.Canadian Public Health Association The future of public health in Canada (Board of Directors Discussion Paper). 2001. http://www.cpha.ca/uploads/policy/future_e.pdf (accessed February 11, 2012).
- 66.Gray S, Pilkington D, Pencheon D, et al. Public health in the UK: success or failure? J R Soc Med. 2006;99:107–111. doi: 10.1258/jrsm.99.3.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Commission on Health Research for Development . Health Research: Essential Link to Equity in Development. New York: Oxford UP; 1990. [Google Scholar]
- 68.Okello D, Chongtrakul P, COHRED Working Group on Priority Setting . A manual for research priority setting using the ENHR strategy. Geneva: Council on Health Research for Development; 2000. [Google Scholar]
- 69.White F. De la evidencia al desempeño: cómo fijar prioridades y tomar buenas decisiones. Pan Am J Public Health. 1998;4:69–74. [Google Scholar]
- 70.Stephenson R, Hennink M. Moving beyond research to inform policy: barriers and strategies in developing countries. Southampton: University of Southampton; 2002. http://www.socstats.soton.ac.uk/choices/moving%20beyond%20research.pdf. [DOI] [PubMed] [Google Scholar]
- 71.Weiss CH. Policy research as advocacy: pro and con. Knowledge Technol Policy. 1991;4:37–55. [Google Scholar]
- 72.National Council for Voluntary Organizations http://www.ncvo-vol.org.uk/ (accessed October 10, 2012).
- 73.World Federation of Public Health Associations http://www.wfpha.org/ (accessed October 10, 2012).
- 74.IANPHI Public Health Institutes of the World http://www.ianphi.org/ (accessed May 13, 2012).