Abstract
Cardiac arrest victims who present with pulseless electrical activity (PEA) usually have a grave prognosis. Several conditions, however, have cause-specific treatments which, if applied immediately, can lead to quick and sustained recovery. Current teaching focuses on recollection of numerous conditions that start with the letters H or T as potential causes of PEA. This teaching method is too complex, difficult to recall during resuscitation, and does not provide guidance to the most effective initial interventions. This review proposes a structured algorithm that is based on the differentiation of the PEA rhythm into narrow- or wide-complex subcategories, which simplifies the working differential and initial treatment approach. This, in conjunction with bedside ultrasound, can quickly point towards the most likely cause of PEA and thus guide resuscitation.
Key Words: Pulseless electrical activity, Cardiopulmonary resuscitation, Electrocardiogram, Echocardiogram
Introduction
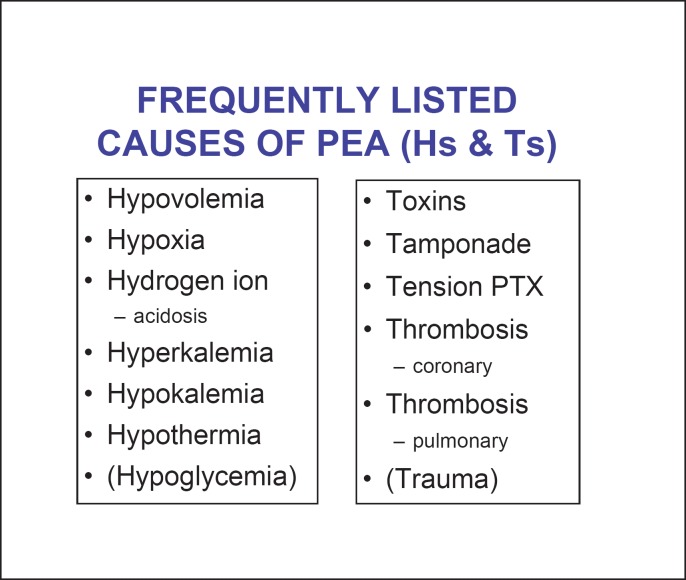
Patients with pulseless electrical activity (PEA) account for up to 30% of cardiac arrest victims [1,2]. The survival rate of patients with PEA is much worse than that of cardiac arrest patients with shockable rhythms [1,3]. Studies suggest that cause-specific treatment of PEA is more effective than general treatments offered by advanced cardiac life support (ACLS) guidelines such as cardiac massage, epinephrine and vasopressin [4]. Higher-dose epinephrine has actually been shown to be associated with worse outcomes [5]. Both the European and American ACLS guidelines, therefore, stress the significance of quickly finding and addressing the cause of PEA [6,7]. Memory aids list numerous conditions whose English names start with the letters H or T as potentially treatable causes of PEA (fig. 1) [6,7]. Studies, however, have shown that during cardiopulmonary resuscitation it is difficult to recall up to 13 causes of PEA [8]. Moreover, even if such a list can be generated, the ACLS does not provide guidance on the relative likelihood of the specific causes, nor does it offer suggestions on how to individualize treatments based on simple initial findings.
Fig. 1.
Causes of PEA listed by European and American guidelines. Hypoglycemia and trauma have been removed from the most recent ACLS guidelines [6,7]. PTX = Pneumothorax.
These limitations of current ACLS guidelines have been recognized and attempts have been made to simplify the evaluation of patients who present with cardiac arrest due to PEA [9,10]. There were also attempts to use the electrocardiogram (ECG) and bedside echocardiogram to guide the diagnosis and management of PEA [10,11,12,13,14,15,16]. Over the last few years we have developed a teaching tool that simplifies the diagnostic approach by differentiating narrow- and wide-complex rhythms on initial telemetry (QRS duration <0.12 and ≥0.12 s, respectively), and by eliminating those diagnoses which rarely if ever cause PEA. Our algorithm does not apply in the specific trauma setting. This algorithm has not been systematically tested but is supported by scientific and clinical principles and by a thorough review of the literature.
The New PEA Algorithm: Diagnostic Aspects
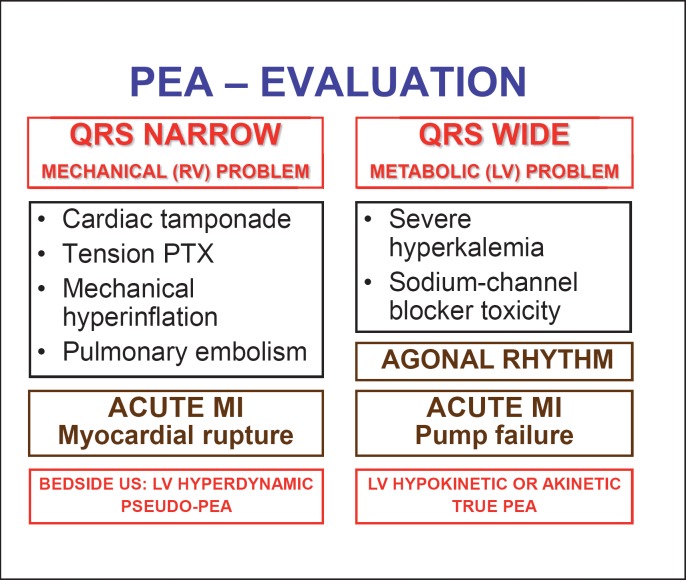
The multiple Hs and Ts that are frequently quoted as possible causes of PEA are listed in figure 1. It seems obvious that recollection of these can be near impossible in the acute setting. Our simplified algorithm that focuses on differentiation between narrow or wide QRS complexes is shown in figure 2. This should be an easy distinction that can be discerned by simply looking at the telemetry monitor during resuscitation. The general assumption is that narrow-complex PEA is generally due to a mechanical problem frequently caused by right ventricular inflow or outflow obstruction, whereas wide-complex PEA is typically due to a metabolic problem or ischemia and left ventricular failure. Wide-complex PEA may also indicate agonal rhythm.
Fig. 2.
New classification of PEA based on its initial electrocardiographic manifestation. LV = Left ventricular; PTX = pneumothorax; US = ultrasound; RV = right ventricular.
The four most common mechanical causes of PEA arrest include cardiac tamponade, tension pneumothorax, mechanical hyperinflation and pulmonary embolism (fig. 2). The clinical scenario can usually help navigate between these causes. Jugular venous distension and muffled heart sounds suggest tamponade. Rib fracture, severe emphysema, positive pressure ventilation and hyperexpanded chest indicate pneumothorax, mechanical hyperinflation or auto-PEEP [17,18]. Cancer history and deep venous thrombosis suggest pulmonary embolism. In all of these cases cardiac ultrasound usually shows preserved or even hyperdynamic left ventricular function indicative of pseudo-PEA (fig. 2) [10,11,12,13,14]. A collapsed right ventricle suggests inflow obstruction from tamponade, pneumothorax or hyperinflation. A dilated right ventricle, on the other hand, indicates possible pulmonary embolism. Thoracic ultrasonography may also help in direct pleural assessment and in the diagnosis of pneumothorax.
Wide-complex PEA usually suggests a metabolic problem such as severe hyperkalemia with or without metabolic acidosis, or sodium channel blocker toxicity (fig. 2) [19,20]. Again, the clinical scenario is usually helpful: in patients with critical illness, sepsis, shock or renal failure, the diagnosis of wide-complex PEA is usually hyperkalemia. Identification of an arteriovenous fistula or dialysis catheter also suggests hyperkalemia. In patients who were ‘found down’ or who present following ingestion or suicide attempt, the cause of wide-complex PEA is almost always sodium channel blocker toxicity [21]. In wide-complex PEA, a metabolic or ischemic cause is supported by the echocardiographic observation of left ventricular hypokinesis or standstill (fig. 2). Other possible causes of wide-complex PEA include a mechanical etiology with preexisting aberrancy or pulmonary embolism – a mechanical cause that can be associated with complete right bundle branch block. In these cases too, bedside ultrasound can quickly point to a mechanical cause.
Patients with acute myocardial infarction (MI) can also present with PEA. Patients who undergo prehospital resuscitation for MI and PEA typically have a dismal prognosis, despite aggressive management including thrombolytics [22,23]. In hospitalized patients with acute MI, PEA is usually a relatively late manifestation. Here too, the ECG is crucial in distinguishing a mechanical cause such as myocardial rupture from pump failure [24,25]. The former is usually associated with narrow QRS complexes, whereas the latter is associated with widened QRS complexes (fig. 2). Immediate recognition of possible myocardial rupture can be life-saving as with emergent surgical intervention some patients may survive for decades [25]. Wide-complex PEA associated with acute MI or with other agonal rhythms, on the other hand, has dismal prognosis with no effective treatments.
An important question is whether this simplified algorithm covers all important causes of PEA? We believe that it does. A recent thorough review of the PEA literature by Desbiens [9] and our independent review did not find any evidence that hypoxemia, hypokalemia or hypoglycemia presents primarily with PEA. Hypothermia is not listed in our new algorithm, but there the clinical picture is usually quite obvious. Of ‘toxins’, the initial presentation of β-blocker, calcium channel blocker and digitalis toxicity is almost always hypotension, sinus bradycardia, sinus arrest or atrioventricular block [26,27]. Some of these do progress to PEA but by that time the diagnosis is usually well established [28,29,30]. Standard treatments are available for these conditions [26,31]. Of the other possible ‘Ts’, we have excluded trauma, as have the newest guidelines [6,7], because traumatic arrests have unique management strategies separate from current ACLS guidelines [32], and signs are usually apparent on exam.
The New PEA Algorithm: Therapeutic Considerations
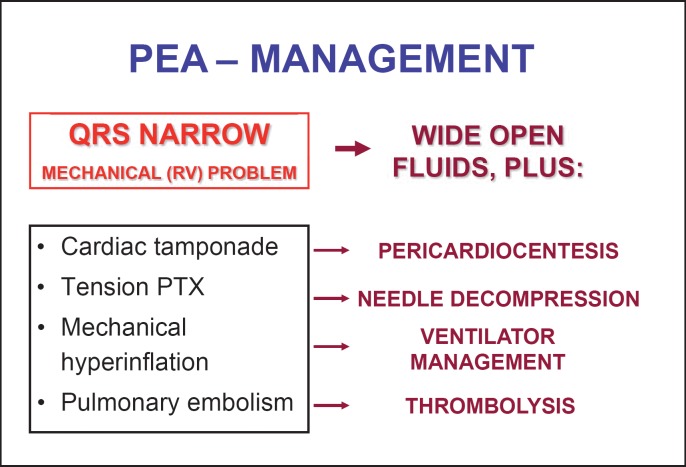
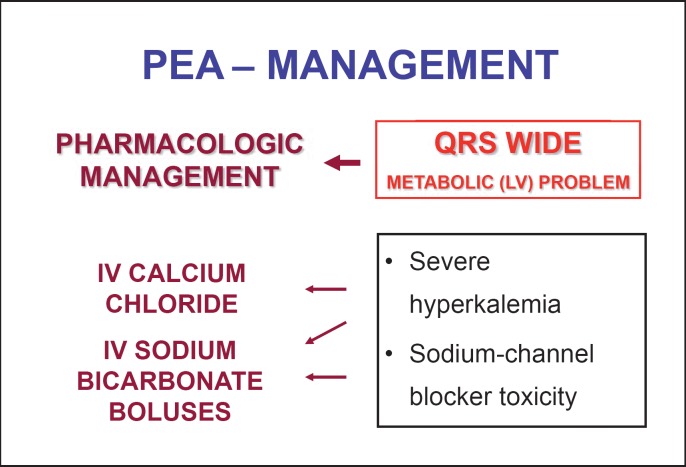
How this simplified and structured approach to PEA can guide initial treatment is shown in figures 3 and 4. For patients with narrow-complex PEA from a suspected mechanical etiology, aggressive intravenous fluid administration should be initiated as these causes are potentially fluid responsive. After that, based on the most likely clinical scenario or results of bedside ultrasonography, pericardiocentesis, needle decompression, adjustment of ventilation or thrombolytic therapy should be considered (fig. 3). For wide-complex PEA intravenous calcium chloride and sodium bicarbonate should be administered if the clinical picture indicates hyperkalemia. Intravenous sodium bicarbonate boluses should be given if the clinical picture suggests sodium channel blocker toxicity (fig. 4) [33]. Neither calcium nor bicarbonate is likely to have any effect on narrow-complex PEA.
Fig. 3.
Treatment recommendations for narrow-complex PEA. PTX = Pneumothorax: RV = right ventricular.
Fig. 4.
Treatment recommendations for wide-complex PEA. IV = Intravenous; LV = left ventricular.
Discussion
There is considerable debate surrounding the most appropriate approach to cardiac arrest due to PEA [4,5,6,7,8,9,10,11,12]. Our simplified and structured approach offers three new elements compared to official European and American guidelines. First, rather than randomly listing 10-13 causes of PEA with terms starting with the letters H or T, our algorithm categorizes the possible causes based on the easy finding of QRS complexes being narrow or wide in a simple telemetry or rhythm strip (fig. 2). Narrow-complex PEA is usually due to a mechanical cause, whereas wide-complex PEA is usually due to a metabolic cause. Second, within each category we have markedly reduced the number of listings to those diagnoses that have the highest likelihood and clinical relevance. Among the mechanical causes we have listed cardiac tamponade, tension pneumothorax, mechanical hyperinflation and pulmonary embolism. The clinical scenario and, if available, bedside ultrasonography should quickly distinguish among these. When the presentation is wide-complex PEA or nonshockable pulseless wide-complex tachycardia, the most likely causes include severe hyperkalemia or sodium channel blocker toxicity. Metabolic acidosis without hyperkalemia is usually the consequence rather than the cause of PEA. Third, our algorithm provides specific treatment recommendations that are based on the initial QRS morphology on telemetry (fig. 3, 4). In narrow-complex PEA, wide-open fluids should be started. It is important to remember that the problem is frequently right ventricular inflow obstruction where overzealous mechanical ventilation and vigorous external cardiac compression may actually be harmful [18,34]. Consideration should be given to perform immediate needle decompression or pericardiocentesis, or to administer thrombolytic therapy. The use of intravenous calcium or sodium bicarbonate as initial management should be discouraged, and the use of epinephrine should be limited. Several studies have shown that routine, indiscriminate use of these agents is ineffective or harmful in PEA [5,35,36,37,38]. With wide-complex PEA or nonshockable pulseless wide-complex tachycardia, the initial treatment of choice is intravenous calcium and/or sodium bicarbonate [6,7,33]. Needle decompression, pericardiocentesis and thrombolytic administration should be entertained only if a mechanical cause is suggested by history or bedside ultrasound.
There is strong physiological basis behind these recommendations. In PEA the heart usually produces some mechanical action but it generates such a low blood pressure that it does not result in a palpable pulse [39]. The main mechanisms of PEA include mechanical obstruction to right ventricular filling or outflow, or severe pump failure. The mechanical causes are not directly related to abnormal myocardial performance (pseudo-PEA) and therefore are almost always associated with narrow QRS complexes. Pump failure resulting in PEA, on the other hand, is usually due to blockade of the cardiac sodium channels either directly by sodium channel blocker toxicity or by extracellular hyperkalemia [40]. Severe ischemia may also be associated with potassium accumulation and reduced sodium transport [41,42]. At the cellular level sodium channel blockade causes flattening of phase zero of the cardiac action potential; in the surface ECG this is reflected by widening of the QRS complexes [43]. Decreased sodium influx results in diminished release of calcium from the sarcoplasmic reticulum and reduced activation of the tropomyosin complex [44]. In both hyperkalemia and sodium channel blocker toxicity, therefore, the width of the QRS complex is a good indicator of clinical severity [19,20,21].
Limitations
Whereas a presentation with narrow-complex PEA almost always indicates a mechanical cause, mechanical causes can occasionally present with wide QRS complexes. Examples include patients with preexisting bundle branch blocks, cases of massive pulmonary embolism causing right bundle branch block, and the rare combination of acute MI – new left bundle branch block and myocardial rupture. Following a prolonged downtime or prolonged resuscitation all mechanical causes of PEA may eventually result in wide QRS complexes but by that time the rhythm is typically agonal with minimal or no chance of survival.
Our new algorithm has not been systematically tested for inclusiveness or resuscitation outcome. Of note, neither the American or European ACLS guidelines nor any of the newer proposals have ever been tested in the clinical setting [6,7,9,10,11,12,13,14]. It may actually be quite difficult to perform a randomized trial comparing the new algorithm with the official ACLS guidelines because instruction on the new algorithm can introduce bias. A more realistic approach would be to systematically teach the new algorithm to all house staff within an institution and then collect outcome data of consecutive cases of resuscitation for PEA and compare those with historic data.
Conclusion
Using the presenting ECG from a simple telemetry recording can quickly direct evaluation of PEA towards the most likely etiology. Narrow-complex PEA usually signifies pseudo-PEA that is due to a mechanical cause. If confirmed by bedside ultrasound, treatment can be directed at relieving the mechanical obstruction. Wide-complex PEA suggests a metabolic cause; early administration of intravenous calcium or sodium bicarbonate may be life-saving.
References
- 1.Engdahl J, Bång A, Lindqvist J, et al. Factors affecting short- and long-term prognosis among 1,069 patients with out-of-hospital cardiac arrest and pulseless electrical activity. Resuscitation. 2001;51:17–25. doi: 10.1016/s0300-9572(01)00377-x. [DOI] [PubMed] [Google Scholar]
- 2.Cobb LA, Fahrenbruch CE, Olsufka M, et al. Changing incidence of out-of-hospital ventricular fibrillation, 1980-2000. JAMA. 2002;288:3008–3013. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 3.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 4.Saarinen S, Nurmi J, Toivio T, et al. Does appropriate treatment of the primary underlying cause of PEA during resuscitation improve patients' survival? Resuscitation. 2012;83:819–822. doi: 10.1016/j.resuscitation.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 5.Arrich J, Sterz F, Herkner H, et al. Total epinephrine dose during asystole and pulseless electrical activity cardiac arrest is associated with unfavourable functional outcome and increased in-hospital mortality. Resuscitation. 2012;83:333–337. doi: 10.1016/j.resuscitation.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 6.Deakin CD, Nolan JP, Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–1352. doi: 10.1016/j.resuscitation.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Neumar RW, Otto CW, Link MS, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S729–S767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 8.Morgan R, Westmoreland C. Survey of junior hospital doctors' attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78:413–415. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desbiens NA. Simplifying the diagnosis and management of pulseless electrical activity in adults: a qualitative review. Crit Care Med. 2008;36:391–396. doi: 10.1097/CCM.0b013e318161f504. [DOI] [PubMed] [Google Scholar]
- 10.Hernandez C, Shuler K, Hannan H, et al. CAUSE: cardiac arrest ultra-sound exam – a better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation. 2008;76:198–206. doi: 10.1016/j.resuscitation.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 11.Querellou E, Leyral J, Brun C, et al. In and out-of-hospital cardiac arrest and echocardiography: a review. Ann Fr Anesth Reanim. 2009;28:769–778. doi: 10.1016/j.annfar.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 12.Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225–1230. doi: 10.1016/j.echo.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Testa A, Cibinel GA, Portale G, et al. The proposal of an integrated ultrasonographic approach into ALS algorithm for cardiac arrest: the PEA protocol. Eur Rev Med Pharmacol Sci. 2010;14:77–88. [PubMed] [Google Scholar]
- 14.Lanctôt JF, Valois M, Beaulieu Y. EGLS: echo-guided life support. Crit Ultrasound J. 2011;3:123–129. [Google Scholar]
- 15.Aufderheide TP, Thakur RK, Stueven HA, et al. Electrocardiographic characteristics in EMD. Resuscitation. 1989;17:183–193. doi: 10.1016/0300-9572(89)90070-1. [DOI] [PubMed] [Google Scholar]
- 16.Mehta C, Brady W. Pulseless electrical activity in cardiac arrest: electrocardiographic presentations and management considerations based on the electrocardiogram. Am J Emerg Med. 2012;30:236–239. doi: 10.1016/j.ajem.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Lapinsky SE, Leung RS. Auto-PEEP and electromechanical dissociation. N Engl J Med. 1996;335:674. doi: 10.1056/NEJM199608293350916. [DOI] [PubMed] [Google Scholar]
- 18.Conacher ID. Dynamic hyperinflation – the anaesthetist applying a tourniquet to the right heart. Br J Anaesth. 1998;81:116–117. doi: 10.1093/bja/81.2.116. [DOI] [PubMed] [Google Scholar]
- 19.Delk C, Holstege CP, Brady WJ. Electrocardiographic abnormalities associated with poisoning. Am J Emerg Med. 2007;25:672–687. doi: 10.1016/j.ajem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 20.Littmann L, Monroe MH, Taylor L III, et al. The hyperkalemic Brugada sign. J Electrocardiol. 2007;40:53–59. doi: 10.1016/j.jelectrocard.2006.10.057. [DOI] [PubMed] [Google Scholar]
- 21.Harrigan RA, Brady WJ. ECG abnormalities in tricyclic antidepressant ingestion. Am J Emerg Med. 1999;17:387–393. doi: 10.1016/s0735-6757(99)90094-3. [DOI] [PubMed] [Google Scholar]
- 22.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance: Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005 – December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 23.Koeth O, Nibbe L, Arntz HR, et al. Fate of patients with prehospital resuscitation for ST-elevation myocardial infarction and a high rate of early reperfusion therapy (results from PREMIR, Prehospital Myocardial Infarction Registry) Am J Cardiol. 2012;109:1733–1737. doi: 10.1016/j.amjcard.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 24.López-Sendón J, González A, López de Sá E, et al. Diagnosis of subacute ventricular wall rupture after acute myocardial infarction: sensitivity and specificity of clinical, hemodynamic and echocardiographic criteria. J Am Coll Cardiol. 1992;19:1145–1153. doi: 10.1016/0735-1097(92)90315-e. [DOI] [PubMed] [Google Scholar]
- 25.Pink E, Foot CL, Garlick B, et al. Survival following ventricular free wall rupture: a case series. Crit Care Resusc. 2006;8:43–45. [PubMed] [Google Scholar]
- 26.DeWitt CR, Waksman JC. Pharmacology, pathophysiology and management of calcium channel blocker and β-blocker toxicity. Toxicol Rev. 2004;23:223–238. doi: 10.2165/00139709-200423040-00003. [DOI] [PubMed] [Google Scholar]
- 27.Ramoska EA, Spiller HA, Winter M, et al. A one-year evaluation of calcium channel blocker overdoses: toxicity and treatment. Ann Emerg Med. 1993;22:196–200. doi: 10.1016/s0196-0644(05)80202-1. [DOI] [PubMed] [Google Scholar]
- 28.Hendren WG, Schieber RS, Garrettson LK. Extracorporeal bypass for the treatment of verapamil poisoning. Ann Emerg Med. 1989;18:984–987. doi: 10.1016/s0196-0644(89)80465-2. [DOI] [PubMed] [Google Scholar]
- 29.Pertoldi F, D'Orlando L, Mercante WP. Electromechanical dissociation 48 h after atenolol overdose: usefulness of calcium chloride. Ann Emerg Med. 1998;31:777–781. doi: 10.1016/s0196-0644(98)70241-0. [DOI] [PubMed] [Google Scholar]
- 30.Behringer W, Sterz F, Domanovits H, et al. Percutaneous cardiopulmonary bypass for therapy resistant cardiac arrest from digoxin overdose. Resuscitation. 1998;37:47–50. doi: 10.1016/s0300-9572(98)00025-2. [DOI] [PubMed] [Google Scholar]
- 31.Kerns W., II Management of β-adrenergic blocker and calcium channel antagonist toxicity. Emerg Med Clin North Am. 2007;25:309–331. doi: 10.1016/j.emc.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Kortbeek JB, Al Turki SA, Ali J, et al. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008;64:1638–1650. doi: 10.1097/TA.0b013e3181744b03. [DOI] [PubMed] [Google Scholar]
- 33.Kolecki PF, Curry SC. Poisoning by sodium channel blocking agents. Crit Care Clin. 1997;13:829–848. doi: 10.1016/s0749-0704(05)70371-7. [DOI] [PubMed] [Google Scholar]
- 34.Hogan TS. External cardiac compression may be harmful in some scenarios of pulseless electrical activity. Med Hypotheses. 2012;79:445–447. doi: 10.1016/j.mehy.2012.06.018. [DOI] [PubMed] [Google Scholar]
- 35.Spöhr F, Wenzel V, Böttiger BW. Drug treatment and thrombolytics during cardiopulmonary resuscitation. Curr Opin Anaesthesiol. 2006;19:157–165. doi: 10.1097/01.aco.0000192797.10420.a1. [DOI] [PubMed] [Google Scholar]
- 36.Williamson K, Breed M, Alibertis K, et al. The impact of the code drugs: cardioactive medications in cardiac arrest resuscitation. Emerg Med Clin North Am. 2012;30:65–75. doi: 10.1016/j.emc.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 37.Stueven HA, Thompson B, Aprahamian C, et al. The effectiveness of calcium chloride in refractory electromechanical dissociation. Ann Emerg Med. 1985;14:626–629. doi: 10.1016/s0196-0644(85)80874-x. [DOI] [PubMed] [Google Scholar]
- 38.Väyrynen T, Kuisma M, Määttä T, et al. Who survives from out-of-hospital pulseless electrical activity? Resuscitation. 2008;76:207–213. doi: 10.1016/j.resuscitation.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 39.Paradis NA, Martin GB, Goetting MG, et al. Aortic pressure during human cardiac arrest: identification of pseudo-electromechanical dissociation. Chest. 1992;101:123–128. doi: 10.1378/chest.101.1.123. [DOI] [PubMed] [Google Scholar]
- 40.Ballantyne F III, Davis LD, Reynolds EW., Jr Cellular basis for reversal of hyperkalemic electrocardiographic changes by sodium. Am J Physiol. 1975;229:935–940. doi: 10.1152/ajplegacy.1975.229.4.935. [DOI] [PubMed] [Google Scholar]
- 41.Kléber AG. Resting membrane potential, extracellular potassium activity, and intracellular sodium activity during acute global ischemia in isolated perfused guinea pig hearts. Circ Res. 1983;52:442–450. doi: 10.1161/01.res.52.4.442. [DOI] [PubMed] [Google Scholar]
- 42.Carmeliet E. Cardiac ionic currents and acute ischemia: from channels to arrhythmias. Physiol Rev. 1999;79:917–1017. doi: 10.1152/physrev.1999.79.3.917. [DOI] [PubMed] [Google Scholar]
- 43.Shinozaki T, Satoh S, Miura M, et al. The rise time of the monophasic action potential: a new index of local use-dependent conductivity by sodium channel blockers in human myocardium. Jpn Circ J. 1997;61:979–987. doi: 10.1253/jcj.61.979. [DOI] [PubMed] [Google Scholar]
- 44.Bers DM. Cardiac excitation-contraction coupling. Nature. 2002;415:198–205. doi: 10.1038/415198a. [DOI] [PubMed] [Google Scholar]