Abstract
Objective
To describe a rare case of moyamoya syndrome associated with systemic lupus erythematosus (SLE).
Presentation and Intervention
A 22-year-old woman presented with left-sided hemiparesis in addition to fever, fatigue and malar rash. Brain magnetic resonance imaging revealed acute infarction in the right middle cerebral artery territory. Cerebral angiography showed features of moyamoya syndrome. Brain biopsy showed evidence of vasculitis. She responded well to steroid therapy.
Conclusion
This case represented a rare co-occurrence of SLE-related vasculitis and moyamoya syndrome. Early vascular imaging is critical in patients with SLE and suspected ischemic stroke.
Key Words: Moyamoya syndrome, Systemic lupus erythematosus, Ischemic stroke, Angiography
Introduction
Moyamoya disease is a rare cerebrovascular disorder of unknown etiology characterized by bilateral progressive supraclinoidal stenosis or occlusion of the internal carotid arteries and development of collateral vessels (moyamoya vessels) [1]. Moyamoya syndrome is a cerebrovascular occlusive disorder with similar angiographic findings to moyamoya disease [1,2]. The causes of moyamoya syndrome include vasculitis, fibromuscular dysplasia, sickle cell disease, atherosclerosis and inflammatory diseases. The incidence of moyamoya syndrome in patients with systemic lupus erythematosus (SLE) is unclear due to a lack of sufficient data. Due to atypical clinical manifestations, diagnosis of moyamoya syndrome in patients with SLE may be difficult and is often delayed [1,2,3]. We report an unusual case of moyamoya syndrome, which was associated with SLE.
Case Report
A 22-year-old previously healthy right-handed woman presented with acute-onset left-sided weakness and slurred speech worsening over 5 days. She reported having been unwell for 3 weeks with fever and fatigue and she had noticed a rash over both cheeks 10 days before presentation. Physical examination revealed fever of up to 39°C, malar rash, pharyngeal erythema and diffuse cervical lymph node enlargement. Neurological examination showed dysarthria, left-sided hemiparesis and left-sided hemianesthesia.
She underwent extensive evaluation which showed: leukopenia (white cell count of 1,900/μl, normal range 3,500-9,000/μl), evidence of red blood cell casts in urine and proteinuria (640 mg/ 24 h). She had elevated liver enzymes and a high sedimentation rate (50 mm/h, normal range 0-20 mm/h). The autoimmune panel revealed a positive antinuclear antibody titer of 1:1,600 with a homogeneous pattern and positive anti-double-stranded DNA antibodies. She had positive rheumatoid factor antibodies and low levels of serum complements (C3 and C4). Antineutrophil cytoplasmic antibody and antiphospholipid antibody tests (lupus anticoagulant, anticardiolipin and anti-β2-glycoprotein antibodies) were negative. Extensive infectious workup was negative for cytomegalovirus, human immunodeficiency virus, herpes viruses, hepatitis virus panel and Epstein Barr virus. An urgent magnetic resonance imaging scan of the head revealed a large acute ischemic infarct in the right middle cerebral artery territory involving the parietotemporal region. Magnetic resonance angiography showed near occlusion of the right internal carotid artery and stenosis of the left internal carotid artery, with rich basal collaterals from the bilateral posterior cerebral arteries, which was indicative of the moyamoya syndrome. Digital subtraction angiogram revealed narrowing of the distal internal carotid arteries, proximal anterior and middle cerebral arteries, worse on the right, with the ‘puff of smoke’ appearance diagnostic of the moyamoya syndrome (fig. 1). Cerebrospinal fluid (CSF) examination showed normal opening pressure, no cells and normal protein and sugar level. The CSF examination was negative for an extensive panel of bacterial and viral etiologies. She underwent brain biopsy which showed T lymphocyte infiltrates (immune phenotyping CD3+ and CD20-) in the vessel wall and perivascular brain tissue (fig. 2). There was vascular endothelial cell swelling, and white matter tissue showed no evidence of demyelination or visible gliosis.
Fig. 1.
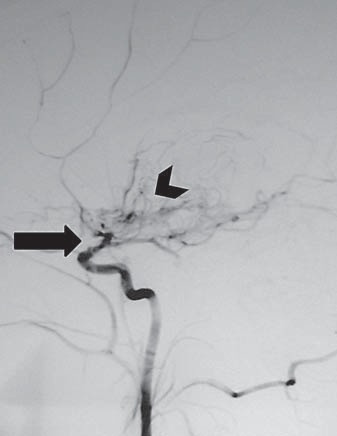
Cerebral angiogram showing occlusion of the distal internal carotid artery (arrow) and characteristic ‘puff of smoke’ appearance (arrowhead).
Fig. 2.
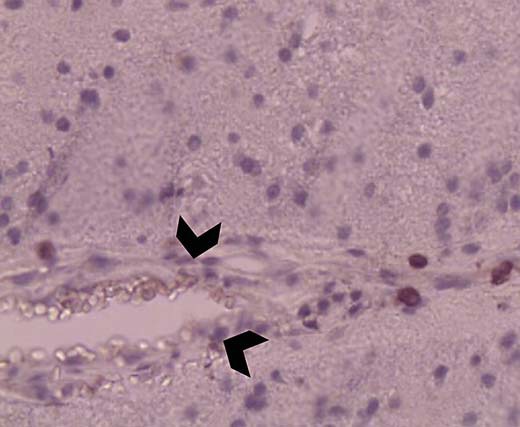
Brain biopsy (hematoxylin and eosin stain) showing lymphocytic infiltration of the vessel wall (arrowheads) and perivascular tissue, suggestive of vasculitis.
She was diagnosed with active SLE with secondary moyamoya syndrome. The cerebral vasculopathy was attributed to vascular inflammation due to SLE. Steroids were administered as a pulse of methylprednisolone 1 g/day for 3 days followed by oral prednisone. She was also started on aspirin. Her symptoms improved over the next 4 weeks. Follow-up CT angiography (at 6 months) revealed stenosis and occlusion at the terminus of the internal carotid arteries and extensive collateral formation (fig. 3). She did not have more strokes in the next 2 years during the follow-up.
Fig. 3.
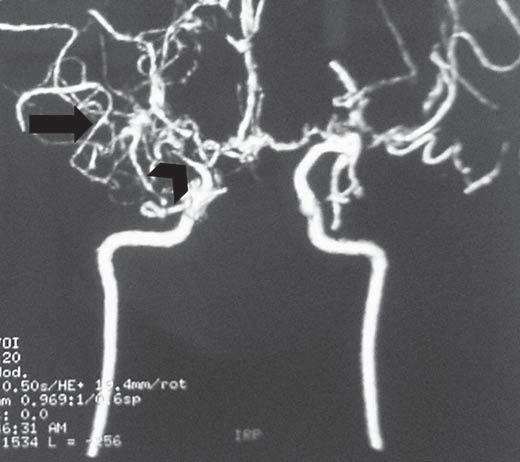
Follow-up CT angiography at 6 months showing stenosis and occlusion at the terminus of the internal carotid arteries (arrowhead) and extensive collateral formation (arrow).
Discussion
Our case has several uncommon features. The CNS vasculitis was largely confined to the perivascular region and there was no pleocytosis or elevated protein in the CSF. Our patient presented with fever and rash followed by cerebral infarction and blood tests confirmed the diagnosis of SLE. Large-vessel stroke due to moyamoya syndrome as a presenting manifestation of SLE was unique in this patient.
Transient ischemic attacks or seizures are the usual presentation of moyamoya disease in children, whereas cerebral ischemia and cerebral hemorrhage are the most common manifestations in adults as in our case [2]. SLE is an autoimmune disease of unknown etiology with multisystem organ manifestations [4]. CNS manifestations of SLE include neuropsychiatric symptoms, seizures or aseptic meningitis [4,5]. Stroke caused by occlusion of large cerebral vessels is distinctly uncommon in lupus and results from cardiogenic embolus (including Libman-Sacks endocarditis) or antibody-mediated hypercoagulable state such as antiphospholipid syndrome [5]. CNS vasculitis in the setting of lupus leading to large cerebral vessel occlusions and producing moyamoya syndrome is extremely rare and the data are limited to a handful of case reports in the literature [6,7,8]. Our case represents a rare occurrence of CNS vasculitis, secondary to lupus. The radiological findings supported the diagnosis of moyamoya syndrome. Various forms of immunosuppressive therapies have been tried. Steroids are the most commonly used first-line therapy as in this case. Other agents such as cyclophosphamide in pulse doses have been shown to be effective in some cases [7,8,9,10] as was in our patient.
Conclusion
This case showed that SLE should be considered in young patients, especially women who present with stroke as early vascular imaging is of paramount importance. Such early imaging could facilitate early diagnosis and treatment with steroids and thus improve outcome, as in our patient.
References
- 1.Suzuki J, Takaku A. Cerebrovascular ‘moyamoya’ disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:288–299. doi: 10.1001/archneur.1969.00480090076012. [DOI] [PubMed] [Google Scholar]
- 2.Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226–1237. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- 3.Matsuki Y, Kawakami M, Ishizuka T, et al. SLE and Sjögren's syndrome associated with unilateral moyamoya vessels in cerebral arteries. Scand J Rheumatol. 1997;26:392–394. doi: 10.3109/03009749709065707. [DOI] [PubMed] [Google Scholar]
- 4.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 5.Tsokos GC, Tsokos M, Le Riche NG, et al. A clinical and pathologic study of cerebrovascular disease in patients with systemic lupus erythematosus. Semin Arthritis Rheum. 1986;16:70–78. doi: 10.1016/0049-0172(86)90041-7. [DOI] [PubMed] [Google Scholar]
- 6.Jeong HC, Kim YJ, Yoon W, et al. Moyamoya syndrome associated with systemic lupus erythematosus. Lupus. 2008;17:679–682. doi: 10.1177/0961203307087375. [DOI] [PubMed] [Google Scholar]
- 7.El Ramahi KM, Al Rayes HM. Systemic lupus erythematosus associated with moyamoya syndrome. Lupus. 2000;9:632–636. doi: 10.1191/096120300678828686. [DOI] [PubMed] [Google Scholar]
- 8.Ramos-Casals M, Nardi N, Lagrutta M, et al. Vasculitis in systemic lupus erythematosus: prevalence and clinical characteristics in 670 patients. Medicine (Baltimore) 2006;85:95–104. doi: 10.1097/01.md.0000216817.35937.70. [DOI] [PubMed] [Google Scholar]
- 9.Wang R, Xu Y, Lv R, et al. Systemic lupus erythematosus associated with moyamoya syndrome: a case report and literature review. Lupus. 2013;22:629–633. doi: 10.1177/0961203313485828. [DOI] [PubMed] [Google Scholar]
- 10.Prelipcean V, Koch AE. Systemic lupus erythematosus associated with moyamoya disease case report and review of the literature. J Clin Rheumatol. 1998;4:328–332. doi: 10.1097/00124743-199812000-00008. [DOI] [PubMed] [Google Scholar]


