Abstract
Objective Open angle glaucoma is one of the most common causes of blindness in industrialised nations. Treatments to lower ocular pressure are widely used in glaucoma prevention and treatment, despite conflicting evidence.
Design We performed meta-analyses to reassess the effectiveness of pressure lowering treatment to delay the development of glaucoma in ocular hypertension, as well as progression of manifest open angle glaucoma.
Data sources Medline, Embase, and the Cochrane Library.
Selection of studies Eligible studies were randomised controlled trials with a concurrent untreated control group and information on time to glaucomatous changes to visual field and optic disc. Trial reports were reviewed independently by two investigators in an unblinded standardised manner.
Results Meta-analysis of trials in ocular hypertension showed a significant preventive effect of reducing intraocular pressure on progression to glaucoma (hazard ratio 0.56, 95% confidence interval 0.39 to 0.81, P = 0.01; number needed to treat 12). Pooled data of studies in manifest glaucoma showed a significant delay of visual field deterioration (0.65, 0.49 to 0.87, P = 0.003; NNT = 7), with subgroup analysis showing a larger effect in patients with raised pressure and a reduced effect in normal tension glaucoma (subgroup comparison: not significant).
Conclusions Lowering intraocular pressure in patients with ocular hypertension or manifest glaucoma is beneficial in reducing the risk of visual field loss in the long term.
Introduction
Glaucoma is one of the most common causes of blindness in industrialised nations, with prevalences between 1% and 3%.1 This primary chronic disease is an optic neuropathy characterised by an acquired loss of retinal ganglion cells and atrophy of the optic nerve. As increased intraocular pressure may or may not be present (as seen in patients with normal tension glaucoma who represent about 15-40% of all patients with open angle glaucoma2), the definition of open angle glaucoma has changed so that the diagnosis is now based only on glaucomatous visual field defects or typical changes of the optic disc (table 1). However, raised intraocular pressure remains an important risk factor for the development or the progression of primary open angle glaucoma.3 Remarkably, patients in general do not have symptoms from glaucoma until large, irreversible visual field defects have occurred. Interventions at an early stage of the disease therefore promise to be most effective. Ideally, this would be at a presymptomatic stage—for example, in patients with ocular hypertension (increased intraocular pressure without any glaucomatous changes of the optic disc or visual field defects), with effective therapy preventing any progression to manifest glaucoma. However, because most people with ocular hypertension will not develop glaucoma4 and a prior meta-analysis was unable to show a significant effect,5 preventive therapy has been controversial. If early visual field loss has occurred or the optic disc has been classified as having typical glaucomatous changes then treatment to lower the intraocular pressure is initiated in virtually all patients. Since this approach includes patients with normal tension glaucoma, a relative, rather than absolute, reduction of intraocular pressure (for example, 20%) is the initial target.
Table 1.
Definitions of glaucoma and ocular hypertension
|
Open angle glaucoma
|
|||
|---|---|---|---|
| Pathology | Ocular hypertension | Primary open angle glaucoma | Normal tension glaucoma |
| Raised intraocular pressure | Yes | Yes | No |
| Optic disc changes or visual field defects, or both | No | Yes | Yes |
| Symptoms | No | <50% at diagnosis | <50% at diagnosis |
The primary objective was to review systematically the literature with regard to the effectiveness of treatment of ocular hypertension and open angle glaucoma (both primary open angle glaucoma and normal tension glaucoma).
Methods
Databases searched included the Cochrane Central Register of Controlled Trials (2004), Medline (1966-2004), and Embase (1974-2004). We searched other databases for guidelines and health technology assessment reports covering glaucoma. We also searched reference lists of relevant articles for additional trials and used the Science Citation Index to search for articles that cited the included studies. For relevant ongoing trials we contacted investigators and experts. The search was not restricted to specific languages or years of publication.
Search strategy
For the search in Medline (Ovid) we used the following search terms (the strategy was MESH term as well as textword based): “Glaucoma/pc, dt, su, th”; “exp Glaucoma, Open-Angle/pc, dt, su, th”; “ocular hypertension/pc, dt, su, th”; “randomised controlled trial.pt.”; “glaucoma$.tw”; “ocular hypertensi$.tw”; “rando$.tw”.
Study selection
According to the prespecified protocol, we included only randomised controlled trials of pressure lowering treatment (medical and surgical) with a concurrent untreated control group and appropriate end points, such as glaucomatous visual field defects or glaucomatous changes to the optic disc. We excluded inappropriate study designs, such as intraocular pressure reduction as the only end point or sole reliance on historical controls, as well as follow-up of less than one year.
Description of studies
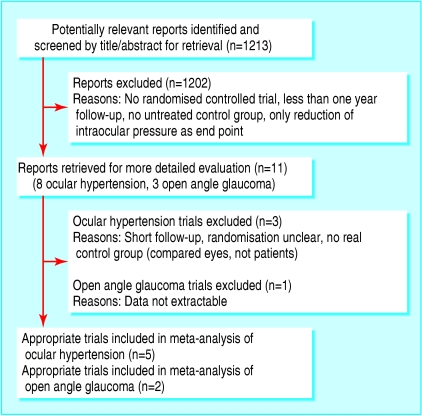
Literature searches of the bibliographic databases yielded 1213 reports, which consisted mostly of studies comparing one drug with another. Two authors (PCM and YTF-Y) reviewed retrieved abstracts independently in an unblinded standardised manner. We then obtained and critically appraised relevant articles and extracted data independently. We resolved disagreements by discussion. Five studies included a total of 2326 patients with ocular hypertension who were randomly assigned to various pressure lowering eye drops compared with placebo.6-10 Two studies in patients with manifest glaucoma (total: 400) used either eye drops or surgical approaches to lower intraocular pressure.11-13 We found no unpublished trials. Figure 1 gives further details on numbers of included and excluded studies. For details on study designs see table 2 for excluded studies, and tables 3 and 4 for studies included in the meta-analysis on ocular hypertension and glaucoma, respectively.
Fig 1.
Trial flow shows the number of trials screened, retrieved for evaluation, and included in the analysis
Table 2.
Trials excluded from meta-analysis, with reason for exclusion
| Study | Study design | Outcome | Comment | Reason |
|---|---|---|---|---|
| Shin et al 197618 | Randomised controlled trial, epinephrine treatment (1-2% twice daily) v observation in ocular hypertension Randomised: 38 eyes of patients Duration: 1-5 years End points: deterioration of visual field or optic disc | After 1-5 years follow-up, 2 treated v 11 control patients reached end points (P<0.01) | Significant treatment effect of reduction of intraocular pressure. Effect of epinephrine on control eye possible. No data about dropout rate, no definition of ocular hypertension, no analysis by intention to treat | No true control group (compared eyes and not patients) |
| Kitazawa et al 198119 | Controlled trial, timolol treatment (0.25-0.5% bid) v placebo in ocular hypertension Included: 52 patients Duration: 1 year Endpoints: deterioration of visual field | After 1 year follow-up, 1 treated v 2 control patients reached end points·(P>0.1) | Non-significant treatment effect. No analysis by intention to treat, no data about dropout rate | Probably no randomisation Short follow-up |
| Kass et al 198920 | Double blind randomised controlled trial, timolol (0.25% twice daily) in one eye v no treatment in the other in 62 patients with ocular hypertension Duration: 5 years End points: Visual field deterioration, disc haemorrhage, glaucomatous disc | After 5 years follow-up, 4 treated eyes v 10 untreated eyes reached end points (P<0.05) | Beneficial effect on deterioration of visual field. Effect of timolol on control eye possible. High dropout rate of >20% | No true control group (compared eyes and not patients) |
| Holmin et al 198821 | Randomised controlled trial, various medications v observation in primary open angle glaucoma. Randomised: 16 patients Duration: 3 years End point: Deterioration of visual field | Per protocol: regression analysis showed no significant difference between treated and untreated patients | Missing data on dropout rate and numbers of patients who reached end points | Necessary data could not be extracted for analysis |
Table 3.
Studies included in the meta-analysis on ocular hypertension (reported data only)
| Study | Study design | Outcome | Comment |
|---|---|---|---|
| Epstein et al 19896 | Randomised controlled trial, timolol (0.5% twice daily) v no treatment in 107 patients with ocular hypertension Duration: 56 months End points: visual field defects, intraocular pressure >32 mm Hg, glaucomatous disc | Intention to treat analysis: 9 of 53 patients v 17 of 54 controls reached end point (P=0.07, log rank test); 6 v 10 failures owing to visual field defects or glaucomatous disc (P=0.24, log rank test) | Tendency of beneficial effect. Dropout rate >20% |
| Schulzer et al 19917 | Randomised controlled trial, timolol (0.25-0.5% twice daily) v no treatment in 143 patients with ocular hypertension Duration: 6 years End points: visual field defects or glaucomatous disc, disc haemorrhage | Intention to treat analysis: 20 of 67 patients v 22 of 70 controls reached end point (difference not significant) | No protective treatment effect observed with pressure reduction. Dropout rate >20% |
| Heijl et al 20008 | Double blind, randomised controlled trial, timolol (0.5% twice daily) v no treatment in 90 patients with ocular hypertension plus risk factors Duration: 1) years (post-study analysis after 17 years) End point: visual field defects or glaucomatous disc | Intention to treat analysis: 7 of 46 patients v 15 of 44 controls reached end point after 10 years (P=0.07, log rank test) | Tendency of beneficial effect. In the treatment group, intraocular pressure was higher in patients who reached the end point. Dropout rate >20% |
| Kass et al 20029 | Randomised controlled trial, various medications (titrated to lower intraocular pressure 20% or <24 mm Hg) v observation in ocular hypertension Duration: 5 years End points: visual field defects or glaucomatous disc | Intention to treat analysis: 36 of 817 treated v 89 of 819 control patients reached end point reached end point (hazard ratio 0.40, 95% Cl 0.27 to 0.59, P<0.0001) | Protective or preventive treatment effect of topical or medical reduction of intraocular pressure. 3328 patients screened, 1636 patients included. Dropout rate about 14% |
| Kamal et al 200310 | Randomised controlled trial, betaxolol twice daily v placebo in 356 patients with ocular hypertension Duration: 6 years End point: visual field defects | Intention to treat analysis: 15 of 182 treated v 18 of 174 control patients reached end point (P=0.25) | No significant preventive effect of topical reduction of intraocular pressure. Dropout rate 28% |
Table 4.
Studies included in meta-analysis on open angle glaucoma (both primary open angle glaucoma and normal tension glaucoma (reported data only)
| Study | Study design | Outcome | Comment |
|---|---|---|---|
| Heijl et al 200211,12 (early manifest glaucoma trial) | Randomised controlled trial, laser trabeculoplasty, betaxolol (5 mg/ml, twice daily) and latanoprost (50 μg/ml, once daily) when intraocular pressure >25 mm Hg in treated v observation in primary open angle glaucoma or normal tension glaucoma Randomised: 255 patients Duration: 6 years End point: deterioration of visual field or optic disc | Intention to treat analysis: 58 of 129 treated v 78 of 126 control patients reached end point (P=0.007, log rank test) | Significant protective treatment effect of reduction of intraocular pressure. Dropout rate about 11% |
| Collaborative Normal Tension Glaucoma Study Group 199813 | Randomised controlled trial, medication or surgery (to lower intraocular pressure 30%) v observation in normal tension glaucoma. Randomised: 145 patients Duration: 5 years End point: deterioration of visual. field or optic disc | Intention to treat analysis: 22 of 66 treated v 31 of 79 control patients reached end point (P=0.21, log rank test). When censored for cataracts, 10 treated v 29 control patients reached end point (P=0.0018, log rank test). | Significant only when analysis censored for newly developed cataracts. Dropout rate not clear |
Data extraction and analysis
We used a standardised form to extract the following data from the methodologically adequate randomised controlled trials: randomisation procedure, allocation concealment, masking, type of interventions, participant flow, sample size, length of follow-up, numbers of patients randomised, numbers analysed, outcome data and estimation, and loss to follow-up. For the meta-analysis we reassessed the numbers of patients originally described as developing the outcome “glaucoma” to include only patients with unequivocal glaucomatous changes to the visual field or optic disc, according to current definition of glaucoma. We ignored older outcome definitions, such as disc haemorrhage, “very high” but asymptomatic intraocular pressure elevation alone, which yielded a more conservative estimate since such pressure readings were more common in the control groups. We extracted information on the time to definite visual field deteriorations and optic disc changes compatible with open angle glaucoma, rather than binary data at one or two fixed points in time. This allowed us to use the study data to the fullest by performing meta-analyses of time to event data using the hazard ratio. The hazard ratio then represents the relative risk of development or worsening of glaucoma during treatment compared with the control group. If the hazard ratio was not reported and data on individual patients were not available we calculated the hazard ratio by using methods described by Parmar et al.14 We performed separate meta-analyses for ocular hypertension and for open angle glaucoma, using the DerSimonian and Laird random effects model in R,15 as well as predefined subgroup analysis of normal tension glaucoma compared with increased pressure glaucoma. We assessed heterogeneity by inspecting the forest plot, the χ2 test as well as the I2 statistic16 for heterogeneity. Sensitivity analysis included using the random and fixed effects model as well as a pre-defined subgroup analysis of elevated and normal tension glaucoma. We used methods described by Altman et al17 to calculate the number needed to treat to prevent the first glaucomatous visual field defect in patients with ocular hypertension and glaucoma progression in patients with open angle glaucoma within five years after treatment onset.17
Results
When we looked at the treatment of patients with ocular hypertension alone, we found earlier trials of treatment for intraocular pressure reduction difficult to interpret because of poor study design (for example, an inadequate control group), small sample size, and short follow-up.18,19 Six studies6-10,20 showed major improvements in study design, but we had to exclude one of these from the meta-analysis because a true control group was missing (table 2).20
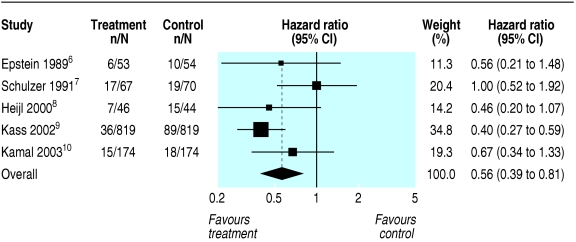
Combining the results of the remaining five trials (table 3) in a meta-analysis to estimate overall efficacy of pressure lowering treatment in ocular hypertension showed a beneficial treatment effect (hazard ratio 0.56, 95% confidence interval 0.39 to 0.81, P = 0.01; fig 2). To estimate the hazard ratio of Schulzer et al,7 we assumed from the completely overlapping Kaplan-Meier curves a P value of 1.00 (stated as non-significant in the publication). We could not observe significant heterogeneity of the included studies (χ2 = 6.2, P = 0.185; I2 = 35.4%, 95% confidence interval 0 to 75.8%).
Fig 2.
Visual field loss or deterioration of optic disc, or both, among patients randomised to pressure lowering treatment v no treatment in ocular hypertension. Hazard ratios of less than 1.0 favour pressure lowering treatment. Boxed area is proportional to weight given to each trial in the statistical model. Heterogeneity: χ2 = 6.2 (P=0.185); I2 = 35.4% (95% confidence interval 0 to 75.8%)
To illustrate the baseline risk, Kaplan-Meier estimates in the control group for remaining free of glaucomatous visual field defects within five years after treatment onset ranged from approximately 63% to 91% in the five trials. We therefore used the 80% mark as a realistic, but conservative assumption to calculate the number needed to treat as an example of absolute effect. When this information and the estimated hazard ratio of 0.56 are used, 12 patients with ocular hypertension alone need to be treated to prevent the first glaucomatous visual field defect or definite glaucomatous disc change within five years of treatment (95% confidence interval for number needed to treat 9 to 29).
Treatment of open angle glaucoma with and without raised intraocular pressure
Until recently only a very small trial had been conducted,21 which did not show a significant effect in the treatment group. Because we could not extract data as information on the number of end points was missing, we excluded this study from the analysis (table 2). Table 4 shows a summary of two more recent randomised controlled trials in manifest open angle glaucoma that we included in the analysis.11-13
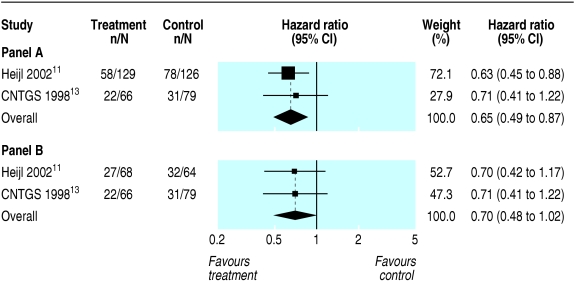
Combining the results from the early manifest glaucoma trial11,12 and the Collaborative Normal-Tension Glaucoma Study Group13 showed a significant pooled treatment effect of lowering intraocular pressure to effectively prevent glaucoma progression (hazard ratio 0.65, 95% confidence interval 0.49 to 0.87, P = 0.003; fig 3). The included studies were not significantly heterogeneous (χ2 = 0.13, P = 0.72).
Fig 3.
Visual field loss or deterioration of optic disc, or both, among patients randomised to pressure lowering treatment v no treatment in open angle glaucoma (panel A). Panel B shows subgroup analysis of data in normal tension glaucoma. Hazard ratios of less than 1.0 favour pressure lowering treatment. Boxed area is proportional to weight given to each trial in the statistical model. Heterogeneity: χ2 = 0.13 (P=0.72) for open angle glaucoma and χ2 = 0.001 (P=0.97) for normal tension glaucoma
The Kaplan-Meier estimate in the control group for remaining free of glaucoma progression within five years after treatment onset was 42% and 43% in the early manifest glaucoma trial and the Collaborative Normal-Tension Glaucoma Study Group, respectively. Accordingly, when using the 40% mark and the estimated hazard ratio of 0.65, seven patients with glaucoma need to be treated to prevent one patient with glaucoma progression within five years of treatment (95% confidence interval for number needed to treat 4 to 20).
Sensitivity and subgroup analysis
Changing our meta-analysis model from random to fixed effects did not change the results in either meta-analysis. The subgroup of patients with elevated ocular pressure glaucoma responded well to pressure lowering treatment, as seen in a subgroup analysis of these patients in the early manifest glaucoma trial (hazard ratio 0.57, 95% confidence interval 0.37 to 0.89, P = 0.013; data not presented in a figure).11,12 However, to investigate whether patients with normal tension glaucoma would fare equally well as all patients with open angle glaucoma patients, we extracted the subset of data from the early manifest glaucoma trial11,12 accordingly and combined this with the uncensored data set from the collaborative normal-tension glaucoma study.13 Although fewer end points were reached in the treatment group (hazard ratio 0.70, 95% confidence interval 0.48 to 1.02, P = 0.06; fig 3), the confidence interval remained wide, indicating remaining uncertainty about the true treatment effect. However, when we used methods described by Altman and Bland,22 to compare these two subgroups we found no significant difference.
Discussion
Primary prevention of glaucomatous visual field defects in patients with ocular hypertension by using topical pressure lowering agents seems to be effective, as shown in this meta-analysis of five methodologically adequate trials. The overall positive effect, as seen in the ocular hypertension treatment study9 remained robust, even when combined with all the other non-significant trials to date.
In comparison, a 1993 meta-analysis of randomised controlled trials by Rossetti et al5 identified only three appropriate randomised controlled trials out of a total of 102 trials.6,7,20 Although the pooled treatment effect showed a reduced risk for progression to glaucoma (odds ratio 0.75), the 95% confidence interval was wide (0.42 to 1.35), indicating that worsening of visual field defects could not be excluded in the intervention group.
The recent ocular hypertension treatment study had to exclude 1692 of 3328 patients screened for inclusion in the study for various reasons.9 The overall effectiveness of treatment may therefore be different in real practice. Moreover, the effectiveness of the investigators' treatment strategy in patients with mildly raised intraocular pressure (above 21 mm Hg, but below 24 mm Hg) remains unanswered.
Until now, only few adequate trials have been completed to address the issue of effective secondary prevention of visual field deterioration with pressure lowering treatment in patients with manifest primary open angle glaucoma, most probably because of ethical concerns of including an untreated control group. However, the results of our meta-analysis, as well as the early manifest glaucoma trial,11,12 show that reducing the intraocular pressure in patients with open angle glaucoma leads to a significant delay of visual field loss, particularly for those patients with increased intraocular pressure, as seen in the subgroup analysis of these patients.
In normal tension glaucoma, lowering the intraocular pressure may be beneficial as seen in the normal tension glaucoma study,13 but this has to be confirmed by larger trials and newer treatment modalities, because in this study, the development of excess cases of cataracts may have offset the treatment effect. In addition, we were not able to show a significant treatment effect convincingly when combining the data for patients with normal tension glaucoma in our subgroup analysis. This was mainly due to low power because of the small number of patients with normal tension glaucoma enrolled in these two studies.
Limitations
Our analysis may have some limitations. Firstly, we cannot fully exclude publication bias; we did not perform a statistical test for the detection of publication bias, since these tests have very low power in meta-analysis of only five trials. However, we did not impose restrictions by language or year of publication, and the search results were complemented by hand searching of relevant journals, yielding more than 1000 reports that we assessed for inclusion in this review. Secondly, since our meta-analysis would lose significance (confidence interval 0.47 to 1.01) by excluding the ocular hypertension treatment study,9 the overall beneficial effect can only be safely assumed in patients with intraocular pressure of 24 mm Hg or more. Four of five included studies on ocular hypertension had high dropout rates, and therefore the magnitude of effect may have been biased.
Although the more recent trials discussed in our report seem methodologically sound, some general questions remain. In particular, it is not entirely clear why some patients may experience disease progression much faster than others (with and without treatment), even if they do not differ in terms of their risk factor profile: The results of the early manifest glaucoma trial11,12 showed that the visual fields of many treated patients deteriorated and those of many untreated patients did not. Therefore, more research is needed to identify subgroups that may be particularly susceptible to pressure reduction strategies. Conversely, some patients, especially those with only borderline elevated intraocular pressure or particular genetic traits, may or may not need immediate intervention.
Conclusions
Although lowering the intraocular pressure in patients with ocular hypertension of 24 mm Hg or more to prevent progression to primary open angle glaucoma seems to be beneficial, uncertainty prevails about the optimal treatment for patients with slightly raised intraocular pressure of 22 mm Hg or 23 mm Hg. In general, patients with manifest open angle glaucoma showed a significant delay in progression of visual field deterioration when treated with a pressure lowering strategy. More research is needed in the subgroup of patients without increased intraocular pressure to determine which patients with normal tension glaucoma will benefit most, since our analysis was unable to show a consistent beneficial effect in these patients.
What is already known on this topic
Primary open angle glaucoma is a leading cause of blindness in industrialised countries
Lowering intraocular pressure is generally used to prevent and to treat primary open angle glaucoma, although a meta-analysis of trials on ocular hypertension did not show a significant preventive treatment effect
What this study adds
Medical reduction of ocular pressure seems to be beneficial for the primary prevention of glaucomatous visual field defects
Only one adequate trial has shown effective secondary prevention of visual field deterioration with topical treatment or surgery in patients with manifest primary open angle glaucoma
A meta-analysis summarising data on normal tension glaucoma was inconclusive
We thank Edith Motschall for her support with the search strategies. Contributors: PCM had the idea for the meta-analysis and participated in conception and design, analysis and interpretation of data, critical appraisal of studies, drafting the article, and final approval of the version to be published. He is the guarantor. GS performed statistical analysis of data, revised the article critically for important intellectual content, and gave final approval of the version to be published. JF was involved in interpreting data, revising the article critically for important intellectual content, and giving final approval of the version to be published. GA was involved in interpreting data, revising them critically for important intellectual content, and giving final approval of the version to be published. YTF-Y had the idea for the meta-analysis and participated in conception and design, critical appraisal of studies, revising the article critically for important intellectual content, and giving final approval of the version to be published. Edith Motschall helped with the literature search.
Funding: None.
Competing interests: None declared.
References
- 1.Quigley HA. Number of people with glaucoma worldwide. Br J Ophthalmol 1996;80: 389-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dielemans I, Vingerling JR, Wolfs RC, Hofman A, Grobbee DE, de Jong PT. The prevalence of primary open-angle glaucoma in a population-based study in the Netherlands. The Rotterdam study. Ophthalmology 1994;101: 1851-5. [DOI] [PubMed] [Google Scholar]
- 3.Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120: 714-20. [DOI] [PubMed] [Google Scholar]
- 4.Kitazawa Y, Horie T, Aoki S, Suzuki M, Nishioka K. Untreated ocular hypertension. A long-term prospective study. Arch Ophthalmol 1977;95: 1180-4. [DOI] [PubMed] [Google Scholar]
- 5.Rossetti L, Marchetti I, Orzalesi N, Scorpiglione N, Torri V, Liberati A. Randomized clinical trials on medical treatment of glaucoma. Are they appropriate to guide clinical practice? Arch Ophthalmol 1993;111: 96-103. [DOI] [PubMed] [Google Scholar]
- 6.Epstein DL, Krug JH, Jr., Hertzmark E, Remis LL, Edelstein DJ. A long-term clinical trial of timolol therapy versus no treatment in the management of glaucoma suspects. Ophthalmology 1989;96: 1460-7. [DOI] [PubMed] [Google Scholar]
- 7.Schulzer M, Drance SM, Douglas GR. A comparison of treated and untreated glaucoma suspects. Ophthalmology 1991;98: 301-7. [DOI] [PubMed] [Google Scholar]
- 8.Heijl A, Bengtsson B. Long-term effects of timolol therapy in ocular hypertension: a double-masked, randomised trial. Graefes Arch Clin Exp Ophthalmol 2000;238: 877-83. [DOI] [PubMed] [Google Scholar]
- 9.Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120: 701-13. [DOI] [PubMed] [Google Scholar]
- 10.Kamal D, Garway-Heath D, Ruben S, O'Sullivan F, Bunce C, Viswanathan A, et al. Results of the betaxolol versus placebo treatment trial in ocular hypertension. Graefes Arch Clin Exp Ophthalmol 2003;241: 196-203. [DOI] [PubMed] [Google Scholar]
- 11.Heijl A, Leske MC, Bengtsson B, Hyman L, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol 2002;120: 1268-79. [DOI] [PubMed] [Google Scholar]
- 12.Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 2003;121: 48-56. [DOI] [PubMed] [Google Scholar]
- 13.The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol 1998;126: 498-505. [DOI] [PubMed] [Google Scholar]
- 14.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17: 2815-34. [DOI] [PubMed] [Google Scholar]
- 15.Ihaka RG, Gentlemen R. “R”: a language for data analysis and graphics. J Computational Graphical Stat 1996;5: 299-314. [Google Scholar]
- 16.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327: 557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Altman DG, Andersen PK. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ 1999;319: 1492-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shin DH, Kolker AE, Kass MA, Kaback MB, Becker B. Long-term epinephrine therapy of ocular hypertension. Arch Ophthalmol 1976;94: 2059-60. [DOI] [PubMed] [Google Scholar]
- 19.Kitazawa Y. Prophylactic therapy of ocular hypertension. A prospective study. Trans Ophthalmol Soc N Z 1981;33: 30-2. [PubMed] [Google Scholar]
- 20.Kass MA, Gordon MO, Hoff MR, Parkinson JM, Kolker AE, Hart WM, Jr., et al. Topical timolol administration reduces the incidence of glaucomatous damage in ocular hypertensive individuals. A randomized, double-masked, long-term clinical trial. Arch Ophthalmol 1989;107: 1590-8. [DOI] [PubMed] [Google Scholar]
- 21.Holmin C, Thorburn W, Krakau CE. Treatment versus no treatment in chronic open angle glaucoma. Acta Ophthalmol (Copenh) 1988;66: 170-3. [DOI] [PubMed] [Google Scholar]
- 22.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]