During their professional career, most general practitioners will be consulted by various patients with an acute manifestation of ophthalmic herpes zoster. In addition to the diagnostic dilemma that doctors face in the initial phase of the disease, they may be uncertain about the course and treatment (when is referral indicated, who should be prescribed antiviral medication?). We present an evidence based policy.
Herpes zoster (shingles) is a commonly encountered disorder in general practice. One fifth of the population, mainly elderly people, will present with this neurocutaneous infection during their lifetime. Most immunocompetent patients will experience spontaneous and complete recovery within a few weeks. Some, however, will develop complications such as postherpetic neuralgia and, in cases of ophthalmic herpes zoster, sight threatening eye problems. We outline the main points that general practitioners should keep in mind when faced with a case of ophthalmic herpes zoster.
Methods
In February 2005, we searched the Cochrane Controlled Trial Register (keyword: “herpes zoster”), Embase, and Medline (MESH terms: “herpes zoster” and “therapy”) for clinical trials, randomised controlled trials, meta-analyses, practice guidelines, and reviews. We selected only articles written in English and disregarded any studies of immunocompromised patients.
Incidence and pathophysiology of herpes zoster
Herpes zoster is a commonly seen disorder; one fifth of the population will present with the disease during their lifetime. The reported incidence varies from 2.2 per 1000 to 3.4/1000 people per year. Herpes zoster develops mainly in elderly people: its incidence in people aged over 80 is about 10 in 1000/year.1,2 It is caused by reactivation of the varicella zoster virus (human herpes virus type 3). In temperate climates, primary infection with this virus usually occurs before the age of 10 and manifests itself clinically as chickenpox (varicella). The virus then becomes latent, nestling in the sensory ganglia. Later it may become active again, spread to the corresponding dermatome by means of a spinal or cerebral nerve (usually the trigeminal nerve), and generate the characteristic unilateral vesicular exanthema. The accompanying inflammation of the sensory nerve and skin damage are supposedly responsible for the acute pain.3 Reactivation of the virus is linked to a diminished virus specific and cell mediated immunity, which is related to age. Immunocompromised patients also run an increased risk of developing herpes zoster (especially patients with haematological malignancies or those receiving immunosuppressive drugs). In contrast to other herpes infections, recurrence of herpes zoster is relatively rare (6-14%).1 Since it has not yet been proved that herpes zoster is provoked by any serious underlying pathological condition (for example, a malignancy),4 a search for possible risk factors is not warranted in otherwise healthy patients in whom herpes zoster develops.
Summary points
One out of every 100 individuals will contract herpes zoster ophthalmicus during his or her lifetime
The risk of ocular complications in ophthalmic herpes zoster is not related to age or severity of the skin rash
Doctors should be alert for sight threatening eye complications if skin lesions are located in the dermatome of the nasociliary nerve. This area includes not only the tip of the nose, but also involves the skin at the inner corner of the eye, and the root and side of the nose (Hutchinson's sign)
All patients with ophthalmic zoster, irrespective of age or severity of symptoms, should be prescribed oral antiviral drugs at the first sign of disease. Moreover, they should be re-examined after at most one week
Hutchinson's sign in the early phase of ophthalmic zoster, visual complaints, or a red eye are indications for referral to an ophthalmologist
Because ophthalmic zoster can cause late complications, the disorder must be included in a patient's medical file
Box 1: A 70 year old woman tells her story
Figure 1.
Acute skin rash without involvement of the nasociliary
My complaints started as tender skin when I ran my hand through my hair—a stinging feeling as if my scalp were covered with glass splinters. Initially, I thought it was because I had driven with my car window open. In addition, I did not feel that well. I had a slight fever and a headache. After a few days, I noticed some red spots on the left side of my forehead. For this reason I consulted the general practitioner in attendance. Because my forehead hurt, he thought I had sinusitis. I have had that a few times in the past. The doctor diagnosed the red spots as eczema. I was prescribed nose spray and painkillers. The pain was worse the next day. I felt really sick and stayed in bed. I also noticed several blisters on my forehead and my left upper eyelid was swollen. My own doctor came to my house and diagnosed me as having shingles. He prescribed antiviral drugs. A day later, the eyelids of my left eye were so swollen that I could no longer see out of that eye. As a result, my doctor referred me to an ophthalmologist. Fortunately, only my eyelid was affected—there was no eye infection.
Now, three weeks after my complaints started, I am feeling better. I still have some scabs on my forehead, but I can see again with my left eye. The skin over my forehead, however, is still tender to the touch.
Ophthalmic herpes zoster
Ophthalmic herpes zoster represents 10-20% of all zoster cases.5 In other words, one out of every 100 individuals will develop ophthalmic zoster during his or her lifetime. The disease is potentially serious and may result in severe and lasting pain, particularly in elderly patients. Moreover, without antiviral treatment, about half of all patients will develop various eye disorders. Conjunctivitis, for example, is seen in nearly all of ophthalmic zoster patients with ocular involvement. More severe disorders include keratitis, uveitis, and optic neuritis of the affected eye. If these latter disorders are not diagnosed and treated adequately the patient's sight may become permanently affected. The cornea may lose optical quality because of clouding and surface irregularities. Moreover, a decreased corneal sensitivity combined with inadequate blinking may lead to severe problems with dry eyes with subsequent corneal complications (neurotrophic ulceration and exposure keratopathy, secondary bacterial infection). The risk of corneal ulceration is particularly enhanced in patients with a substantial loss of corneal sensitivity. The risk of ophthalmic complications is not related to age or severity of the skin rash.
Symptoms and signs of ophthalmic zoster
Herpes zoster can present with extraocular and ocular features (table), sometimes simultaneously.
Table 1.
Ocular complications in immunocompetent patients with ophthalmic zoster
| Part of eye affected | Acute phase | Late phase |
|---|---|---|
| Eyelids |
Swelling, vesicular rash |
Ptosis, eyelid retraction |
| Conjunctiva |
Conjunctivitis |
Self limiting |
| Episclera or sclera |
Episcleritis |
Self limiting |
| Scleritis |
Focal scleral atrophy |
|
| Cornea |
Epithelial keratitis |
Neurotrophic or exposure keratopathy |
| Stromal keratitis |
Corneal neovascularisation, deposition |
|
| Anterior chamber |
Uveitis |
Focal iris atrophy |
| Ocular hypertension |
Usually self limiting |
|
| Rare complications |
Extraocular muscle palsies |
Self limiting |
| Optic neuritis |
Optic atrophy |
|
| Retinal vasculitis, retinitis | Retinal atrophy |
In box 1, a patient shares her experiences with the condition, and in box 2, a close family member, a son, reports how he was affected by his father's illness.
Extraocular features
In the prodromal phase, patients may report malaise, pain, itching photophobia, and low grade fever up to one week before the skin rash appears. The rash usually starts with progressive pain sensations that are accompanied by hypersensitive areas on the forehead.6 Then erythematous macules appear that progress to form clusters of papules and clear vesicles in the affected dermatome. In most patients, new skin lesions usually continue to appear for three to five days; the rash then evolves through stages of pustulation and crusting. Patients with deeper involvement of the dermis may develop permanent scars with loss of normal pigmentation. Rash in the dermatome of the nasociliary nerve may indicate ophthalmic complications. Although ophthalmic zoster is usually characterised by this typical rash, a minority of patients have only ophthalmic symptoms.7,8 With typical ophthalmic zoster, the skin rash usually precedes the ocular lesions by some days. Several studies have proposed a greater risk of protracted pain in patients with ophthalmic zoster, but this relation has not been found consistently.9
Ocular features
A wide range of symptoms affecting the eye may occur during the various phases of ophthalmic zoster.
Eyelids
The skin of the forehead and upper eyelid is commonly affected and may give rise to substantial periorbital oedema in the early phase of the disease. In patients with severe dermal inflammation, late phase contraction scars may lead to incomplete eyelid closure and corneal exposure.
Conjunctiva
Conjunctivitis is a common finding in ophthalmic zoster with involvement of the eye. The conjunctiva appears oedematous and injected, sometimes with petechial haemorrhages. These signs usually resolve within a week.
Episclera, sclera
Episcleritis and scleritis may be diagnosed when a localised redness with dilatation of the deeper vessels appears. The presence of pain, however, is not helpful in differentiating between these complications, as ocular sensitivity is invariably affected. After the inflammation has resolved completely, patchy scleral atrophy may become apparent.
Cornea
Small corneal epithelial defects may be visible during the acute phase, but those microdendritic lesions will disappear within days. In patients with a red eye, corneal sensitivity is often substantially and irreversibly reduced. Although corneal hyposensitivity is the norm, hypersensitivity can sometimes occur.10 In prolonged keratitis, regular eye examinations by an ophthalmologist are necessary to evaluate and treat surface problems and deep corneal inflammation and to prevent subsequent neovascularisation. In a minority of patients, topical steroids are indicated on the advice of an ophthalmologist to control inflammation and to maintain corneal transparency.
Anterior chamber
Inflammatory cells may be observed in the anterior chamber when a biomicroscope is used. In most patients, the inflammatory signs will gradually disappear within weeks to months without topical steroid treatment. The release of viral antigens in the iris and ciliary body initiates a mild uveitis often accompanied by temporary elevation of the intraocular pressure. Chronic uveitis, possibly related to an insufficient immune response and prolonged viral activity, is a rare finding in patients who have not been treated with steroids.
Rare complications
Acute ophthalmic zoster may be complicated by involvement of another cranial nerve—for example, the oculomotor nerve. This is probably related to secondary vasculitis within the orbital apex (orbital apex syndrome)11 and may give rise to transient eye motility disorders with diplopia.12 Delayed contralateral hemiparesis may develop as a late complication.13 Acute optic neuritis is a major form of morbidity, because it may lead to a permanent loss of vision.14 Problems with perfusion of the retina and virus induced necrosis of the retina as a result of ophthalmic herpes zoster have been reported, but these complications are rare in immunocompetent patients.15
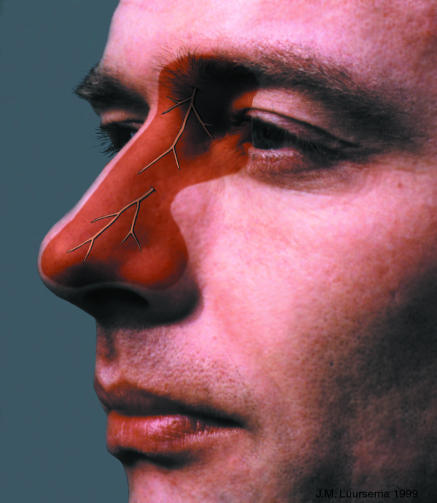
Examination by the general practitioner
In ophthalmic zoster, diagnostics in general practice is restricted to history taking and a physical examination. The diagnostic possibilities during the prodromal phase are manifold until the typical skin signs become manifest. Doctors should always be on the alert for involvement of the eye. The appearance of skin lesions along the side of the nose, which represents the dermatome of the nasociliary nerve, is a useful prognostic factor for subsequent ocular inflammation in patients with acute ophthalmic zoster (Hutchinson's sign).16 General practitioners are often advised to focus their attention only on the tip of the nose—the dermatome of the external branch. The nasociliary dermatome, however, is more extensive and also affects the skin at the inner corner of the eye and the root and side of the nose (figure next page).17
Figure 4.
Visual representation of the nasociliary dermatome
In the acute phase, profound swelling of the eyelids may hinder examination of the eye. Although often difficult to detect (even with the aid of a slit lamp), small corneal epithelial lesions may be visible when the ocular surface is stained with fluoresceine. Corneal sensation of the inflamed eye is often affected, and corneal sensitivity of both eyes should be tested with a cotton wool fibre to assess the risk of future ocular complications. A painful response to light combined with blurred vision may be a symptom of uveitis.
Box 2: A 70 year old man, talking about his late father
Figure 2.
Severe acute skin rash with haemorrhagic ulcerative lesions
Figure 3.

Permanent depigmented scars on the forehead
These are two photographs of my late father, one taken during the acute phase of shingles and the other several months later. I can still vividly remember the horrible skin rash and the agony of his pain when his shingles started. He was 70 years old at that time and already had pulmonary emphysema. I do not know to what extent the pain or itching sensations influenced his daily life or night's sleep, because my father didn't complain about his health problems. The disease, however, affected his appearance permanently, and he sometimes couldn't stop rubbing the eye because of severe itching. His inability to sleep—he slept only a few hours a night—may also be related to his shingles.
Since the onset of shingles, my father had regular check ups for dry eye disease. Until his death at age 84, his right eye was treated with a lubricating eye gel during the day (three times daily) and an ophthalmic ointment before sleep. An ophthalmologist had prescribed this treatment because eyelid closure remained insufficient despite corrective surgery.
During the last years of his life, my father's vision gradually deteriorated because of macular degeneration. His inability to read, even with the aid of a low vision device, was dramatic for him personally. Fortunately, he could still recognise his close relatives with his poorly functioning, herpes zoster affected right eye.
Antiviral therapy
Early treatment with aciclovir (within 72 hours after rash onset) reduces the percentage of eye disorders in ophthalmic zoster patients from 50% to 20-30%.18 This early treatment also lessens acute pain.19 Valaciclovir and famciclovir seem to be as effective as aciclovir in reducing pain associated with zoster,20,21 but their efficacy in reducing eye disorders associated with zoster has not been studied. In clinical practice, however, these second generation antiviral agents may be more effective than aciclovir because patients are more likely to comply with the treatment regimen (three, rather than five, daily doses). Since the course of disease is unpredictable, all patients with ophthalmic zoster, irrespective of their age and the severity of symptoms, should be prescribed oral antiviral drugs at the first signs of infection. Moreover, they should be re-examined after one week at the most. The efficacy of antiviral medication more than 72 hours after the onset of skin rash has never been confirmed. Nevertheless, prescription of these drugs after this timespan should be considered in elderly patients with ophthalmic zoster, because their immune response is usually delayed and, consequently, viral shedding may last longer.22 Although the additional effectiveness of aciclovir eye ointments has never been established, topical aciclovir can be considered in cases of severe eye infection since much higher concentrations of the drug in the anterior eye segment will be effected by this route. Monotherapy with antiviral eye ointment is, however, insufficient and should be adjuvant to oral treatment.23
Additional therapy
When the natural blinking reflex and eyelid function are affected, long term application of a lubricating eye ointment or eye gel is indicated to prevent corneal epithelial damage. Anaesthesia based interventions, such as stellate ganglion block, may produce short term pain relief24 but are not done on a regular basis. In addition, no evidence exists for their effectiveness in reducing the risk of protracted pain.25
When should patients be referred to an ophthalmologist?
Hutchinson's sign in the early phase of ophthalmic zoster, visual complaints, or an unexplained red eye are indications for referral to an ophthalmologist. Immediate consultation, however, is usually not required, since vision threatening ophthalmic complications that require specific treatment usually do not develop during the first week after onset of skin rash. Importantly, the patient should start taking antiviral medication as soon as possible, independent of the ophthalmic condition.
Long term prognosis
Once an eye has been affected by herpes zoster it will always remain vulnerable. Complications can develop even months or years after the acute phase. The cornea, for example, may be damaged because epithelial regeneration is delayed, particularly in eyes with corneal anaesthesia. Doctors should, therefore, remain alert when the natural defensive mechanisms of the eyes of patients with “cured” ophthalmic zoster are affected, as in the state of decreased consciousness and after ophthalmic surgery. Accordingly, we recommend that a past infection with ophthalmic zoster should be registered in the patient's medical file.
Additional educational resources
Review papers
Guidelines for the management of shingles. Report of a working group of the British Society for the Study of Infection (BSSI). J Infect 1995;30: 193-200.
Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med 2002;347: 340-6.
Shaikh S, Ta CN. Evaluation and management of herpes zoster ophthalmicus. Am Fam Physician 2002;66: 1723-30.
Gross G, Schöfer H, Wassilew S, Friese K, Timm A, Guthoff R, et al. Herpes zoster guideline of the German Dermatological Society (DDG). J Clin Virol 2003;26: 277-89.
Liesegang TJ. Herpes zoster virus infection. Curr Opin Ophthalmol 2004;15: 531-6.
Websites
International Herpes Management Forum (IHMF, www.ihmf.org)
Varicella Zoster Virus Research Foundation (VZVRF, www.vzvfoundation.org)
Both websites offer information to both healthcare professionals and the public
Information for patients
www.familydoctor.org—website from the American Academy of Family Physicians offering health information for patients
Contributors: WO and MJWZ collected the data. WO wrote the initial draft document and both authors jointly produced the final article. WO is guarantor.
Funding: None.
Competing interests: None declared.
References
- 1.Hope-Simpson RE, MRCS. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med 1965;58: 9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chapman RS, Cross KW, Fleming DM. The incidence of shingles and its implications for vaccination policy. Vaccine 2003;21: 2541-7. [DOI] [PubMed] [Google Scholar]
- 3.Haanpaa M, Dastidar P, Weinberg A, Levin M, Miettinen A, Lapinlampi A, et al. CSF and MRI findings in patients with acute herpes zoster. Neurology 1998;51: 1405-11. [DOI] [PubMed] [Google Scholar]
- 4.Ragozzino MW, Melton LJ 3rd, Kurland LT, Chu CP, Perry HO. Risk of cancer after herpes zoster: a population-based study. N Engl J Med 1982;307: 393-7. [DOI] [PubMed] [Google Scholar]
- 5.Ragozzino MW, Melton LJ 3rd, Kurland LT, Chu CP, Perry HO. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore) 1982;61: 310-6. [DOI] [PubMed] [Google Scholar]
- 6.Cobo M, Foulks GN, Liesegang T, Lass J, Sutphin J, Wilhelmus K, et al. Observations on the natural history of herpes zoster ophthalmicus. Curr Eye Res 1987;6: 195-9. [DOI] [PubMed] [Google Scholar]
- 7.Silverstein BE, Chandler D, Neger R, Margolis TP. Disciform keratitis: a case of herpes zoster sine herpete. Am J Ophthalmol 1997;123: 254-5. [DOI] [PubMed] [Google Scholar]
- 8.Van der Lelij A, Ooijman FM, Kijlstra A, Rothova A. Anterior uveitis with sectoral iris atrophy in the absence of keratitis: a distinct clinical entity among herpetic eye diseases. Ophthalmology 2000;107: 1164-70. [DOI] [PubMed] [Google Scholar]
- 9.Jung BF, Johnson RW, Griffin DRJ, Dworkin RH. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology 2004;62: 1545-51. [DOI] [PubMed] [Google Scholar]
- 10.Tullo AB, Milodot M, Johnson RW, Easty DL. Corneal hyperaesthesia after herpes zoster ophthalmicus. Cornea 1983;2: 115-7. [Google Scholar]
- 11.Kattah JC, Kennerdell JS. Orbital apex syndrome secondary to herpes zoster ophthalmicus. Am J Ophthalmol 1978;85: 378-82. [DOI] [PubMed] [Google Scholar]
- 12.Marsh RJ, Dulley B, Kelly V. External ocular motor palsies in ophthalmic zoster: a review. Br J Ophthalmol 1977;61: 677-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hilt DC, Buchholz D, Krumholz A, Weiss H, Wolinsky JS. Herpes zoster ophthalmicus and delayed contralateral hemiparesis caused by cerebral angiitis: diagnosis and management approaches. Ann Neurol 1983;14: 543-53. [DOI] [PubMed] [Google Scholar]
- 14.Zaal MJ, Volker-Dieben HJ, D'Amaro J. Visual prognosis in immunocompetent patients with herpes zoster ophthalmicus. Acta Ophthalmol Scand 2003;81: 216-20. [DOI] [PubMed] [Google Scholar]
- 15.Liesegang TJ. The varicella-zoster virus: systemic and ocular features. J Am Acad Dermatol 1984;11(2 Pt 1): 165-91. [DOI] [PubMed] [Google Scholar]
- 16.Hutchinson J. A clinical report on herpes zoster frontalis seu ophthalmicus (shingles affecting the forehead and the nose). R London Ophthalmic Hospital Rep 1865;5: 191-15. [Google Scholar]
- 17.Zaal MJ, Volker-Dieben HJ, D'Amaro J. Prognostic value of Hutchinson's sign in acute herpes zoster ophthalmicus. Graefes Arch Clin Exp Ophthalmol 2003;241: 187-91. [DOI] [PubMed] [Google Scholar]
- 18.Cobo LM, Foulks GN, Liesegang T, Lass J, Sutphin JE, Wilhelmus K, et al. Oral acyclovir in the treatment of acute herpes zoster ophthalmicus. Ophthalmology 1986;93: 763-70. [DOI] [PubMed] [Google Scholar]
- 19.Harding SP, Porter SM. Oral acyclovir in herpes zoster ophthalmicus. Curr Eye Res 1991;(10 suppl): 177-82. [DOI] [PubMed]
- 20.Colin J, Prisant O, Cochener B, Lescale O, Rolland B, Hoang-Xuan T. Comparison of the efficacy and safety of valaciclovir and acyclovir for the treatment of herpes zoster ophthalmicus. Ophthalmology 2000;107: 1507-11. [DOI] [PubMed] [Google Scholar]
- 21.Tyring S, Engst R, Corriveau C, Robillard N, Trottier S, Van Slycken S, et al. Famciclovir for ophthalmic zoster: a randomised aciclovir controlled study. Br J Ophthalmol 2001;85: 576-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zaal MJ, Volker-Dieben HJ, Wienesen M, D'Amaro J, Kijlstra A. Longitudinal analysis of varicella-zoster virus DNA on the ocular surface associated with herpes zoster ophthalmicus. Am J Ophthalmol 2001;131: 25-9. [DOI] [PubMed] [Google Scholar]
- 23.Neoh C, Harding SP, Saunders D, Wallis S, Tullo AB, Nylander A, et al. Comparison of topical and oral acyclovir in early herpes zoster ophthalmicus. Eye 1994;8 (Pt 6): 688-91. [DOI] [PubMed] [Google Scholar]
- 24.Harding SP, Lipton JR, Wells JC, Campbell JA. Relief of acute pain in herpes zoster ophthalmicus by stellate ganglion block. BMJ (Clin Res Ed) 1986;292: 1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Opstelten W, van Wijck AJ, Stolker RJ. Interventions to prevent postherpetic neuralgia: cutaneous and percutaneous techniques. Pain 2004;107: 202-6. [DOI] [PubMed] [Google Scholar]