Abstract
Purpose
The aim of this study was to review the safety and stability of cornea cross-linking (CXL) for the treatment of keratectasia after Excimer Laser Refractive Surgery.
Methods
Eligible studies were identified by systematically searching PubMed, Embase, Web of Science and reference lists. Meta-analysis was performed using Stata 12.1 software. The primary outcome parameters included the changes of corrected distant visual acuity (CDVA), uncorrected visual acuity (UCVA), the maximum keratometry value (Kmax) and minimum keratometry value (Kmin), the surface regularity index (SRI), the surface asymmetry index (SAI), the keratoconus prediction index (KPI), corneal thickness, and endothelial cell count. Efficacy estimates were evaluated by weighted mean difference (WMD) and 95% confidence interval (CI) for absolute changes of the interested outcomes.
Results
Seven studies involving 118 patients treated with CXL for progressive ectasia after laser-assisted in situ keratomileusis (LASIK) or photorefractive keratectomy (PRK) (140 eyes; the follow-up time range from 12 to 62 months) were included in the meta-analysis. The pooled results showed that there were no significant differences in Kmax and Kmin values after CXL (WMD = 0.584; 95% CI: −0.289 to 1.458; P = 0.19; WMD = 0.466; 95% CI: −0.625 to 1.556; P = 0.403, respectively). The CDVA improved significantly after CXL (WMD = 0.045; 95% CI: 0.010 to 0.079; P = 0.011), whereas UCVA did not differ statistically (WMD = 0.011; 95% CI: −0.055 to 0.077; P = 0.746). The changes were not statistically significant in SRI, SAI, and KPI (WMD = 0.116; 95% CI: −0.090 to 0.322; P = 0.269; WMD = 0.240; 95% CI: −0.200 to 0.681; P = 0.285; WMD = 0.045; 95% CI: −0.001 to 0.090; P = 0.056, respectively). Endothelial cell count and corneal thickness did not deteriorate (WMD = 12.634; 95% CI: −29.460 to 54.729; P = 0.556; WMD = 0.657; 95% CI: −9.402 to 10.717; P = 0.898, respectively).
Conclusion
The study showed that CXL is a promising treatment to stabilize the keratectasia after Excimer Laser Refractive Surgery. Further long-term follow-up studies are necessary to assess the persistence of the effect of the CXL.
Keywords: Cross-linking, Keratectasia, Refractive surgery, Meta-analysis
Introduction
Iatrogenic keratectasia is a rare sight-threatening complication of the laser refractive surgery. It is associated with progressive corneal steepening, an increase in myopia and astigmatism, and a decrease in uncorrected and corrected visual acuity.1 Risk factors for its development are thin corneas, a thin residual stromal bed, deep ablations, and pre-existing abnormal corneal topography such as forme fruste keratoconus and pellucid marginal degeneration.2, 3 Until recently, treatment options were limited. In addition to rigid contact lenses, intrastromal corneal ring segments, penetrating or lamellar keratoplasty, and, more recently, cornea cross-linking (CXL) have been used to treat postrefractive surgery ectasia.4, 5, 6
CXL has emerged as an effective technique to slow or halt progression of keratoconus and postoperative ectasia. CXL is a new method to increase the biomechanical stability of the cornea by adding additional polymer bands between collagen fibers using a combination of riboflavin and ultraviolet A (UVA).7, 8, 9 Over the past 10 years, more and more studies and meta-analysis published the encouraging outcomes in advanced keratoconus throughout the world.
However, studies about CXL for postoperative ectasia are rare, the results were controversial, and the studies were less convincing because of the small sample sizes and other research design limitations. Therefore, a meta-analysis is imperative for summarizing results from different studies.
The main objectives of this systematic review and meta-analysis were to evaluate the safety and stability of CXL for the treatment of keratectasia after Excimer Laser Refractive Surgery.
Methods
Search strategy
The clinical studies were identified through a systematic search of PubMed, Embase, Web of Science, and reference lists (all searches with no limitation to specific languages or years of publication were used). The search terms included: “cross linking”, “crosslinking”, “cross-linking”,“keratectasia after laser-assisted in situ keratomileusis (LASIK)”, “post-LASIK keratectasia,” and “Postoperative Ectasia”. Different search strategies were used for database in order to meet the different requirements of each database. The citations of related articles were screened for additional publications. Two reviewers (D.W. and H.Y.) screened the titles and abstracts of the obtained publications and determined the trial eligibility independently. Then the full articles of the eligible publications were scrutinized.10 Only trials meeting the following criteria were used in present meta-analysis.
Inclusion criteria and outcomes
We included studies that compared: (1) research design: randomized or non-randomized clinical studies; (2) population: patients with keratectasia after Excimer Laser Refractive; (3) intervention: CXL (4) outcome parameters: the end points of topographic parameters, corrected distant visual acuity (CDVA), uncorrected visual acuity (UCVA), endothelial cell count, and corneal thickness.
Data extraction
Two reviewers (D.W. and H.Y.) evaluated the quality of the citations and extracted data independently. Any disagreement was resolved by discussion.10 The following information was extracted: the name of the first author, the year of publication, the trial location, the research design, the number of eyes, the mean age of patient, the sex proportion, the follow-up durations, and the sort of refractive Surgery.
Quality assessment
The Newcastle-Ottawa Scale (NOS) scoring methods of quality literature assessment was used for the prospective and retrospective studies that were selected for this analysis.9 The quality assessment scale is composed of three main sections (Selection, Comparability, and Outcome). A study can be awarded a maximum of one star for each numbered item within the Selection and Outcome categories. A maximum of two stars can be given for Comparability. Studies with stars ≥5 were considered to have adequate quality.
Statistical analysis
Analyses were carried out using Stata SE software package (Version 12.1; Stata Corp, College Station, TX). For continuous outcomes, the weighted mean difference (WMD) and 95% confidence interval (CI) calculated for absolute changes of the interested outcomes. The outcomes were measured as mean ± standard deviation (SD). Heterogeneity across studies was estimated by using χ2 and I2 test (I2> 50% indicating significant heterogeneity).11, 12 The overall effect was determined to be statistically significant with P < 0.05. Additionally, if significant heterogeneity existed among trials, a random model was used, and sensitivity analysis was conducted. Alternatively, results were combined using a fixed effect model.13 Potential publication bias was assessed visually with a funnel plot and statistically with the Egger's and Begg's tests.10, 14, 15
Result
Characteristics of trials
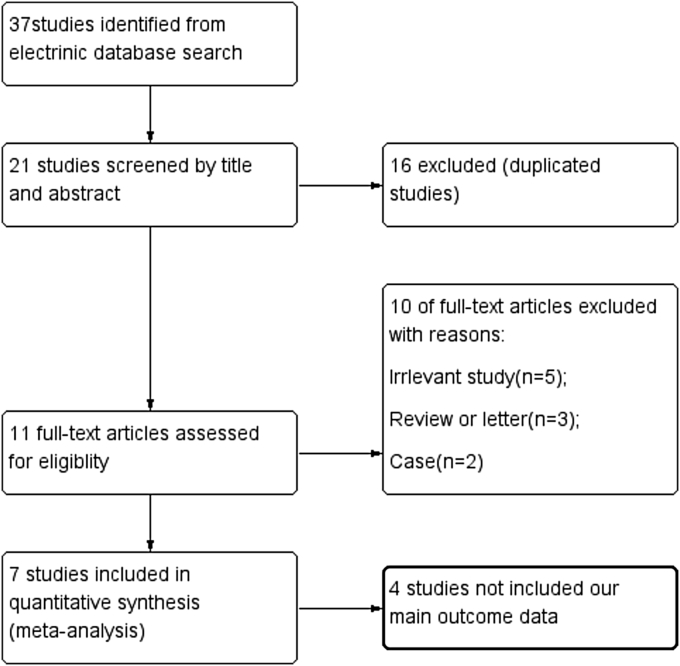
The detailed steps of the study selection process and exclusion reasons are summarized in Fig. 1. Finally, this meta-analysis was based on seven studies2, 16, 17, 18, 19, 20, 21 that met our inclusion criteria. Among these, 5 were prospective studies, and 2 were retrospective studies (Table 1). There were altogether 118 patients (with 140 eyes) diagnosed with post-lasercorneal ectasia, 134 eyes after LASIK and 6 eyes after photorefractive keratectomy (PRK), included in this meta-analysis. The sample sizes of these trials ranged from 10 to 40. These trials were performed in 6 countries (2 each in Switzerland; 1 each in Italy, Germany, China, Turkey, and Brazil). Three trials reported that their patients were followed up for 12 months after post-CXL. Four trials reported follow-up outcomes after more than 1 year.
Fig. 1.
Flow diagram of study selection.
Table 1.
Characteristics of the studies included in this review.
| Author | Year | Country | Design | Eyes/NO. | Mean age (years) | Male/female | Duration (months) | (PRK/LASIK) | NOS score |
|---|---|---|---|---|---|---|---|---|---|
| Farhad et al. | 2007 | Switzerland | Prospective, nonrandomized | 10/10 | 36.2 (27–43) | 4/6 | 18 ± 5 month | 0/10 | **** |
| Paolo et al. | 2010 | Italy | Prospective, nonrandomized | 13/9 | 42 (30–59) | 3/6 | 12 month | 3/10 | ***** |
| Salgado JP et al. | 2011 | Germany | Prospective, nonrandomized | 20/15 | 38.4 (27–51) | 9/6 | 12 month | 0/20 | ***** |
| Li G et al. | 2012 | China | Prospective, nonrandomized | 11/20 | 27.4 (20–36). | 5/6 | 12 month | 0/11 | ***** |
| Olivier et al. | 2013 | Switzerland | Retrospective | 26/26 | 35 (23–46) | 18/8 | 25 ± 13 month | 3/23 | ***** |
| Aydin et al. | 2014 | Turkiye | Retrospective | 20/14 | 34 (25–45) | 7/7 | 42 ± 7 month | 0/20 | ***** |
| Gustavo K et al. | 2015 | Brazil | Prospective, nonrandomized | 40/24 | 33.8 (24–52) | 15/9 | 24 month | 0/40 | ***** |
NOS: Newcastle-Ottawa Scale; LASIK: Laser-assisted in situ keratomileusis; PRK: Photorefractive keratectomy.
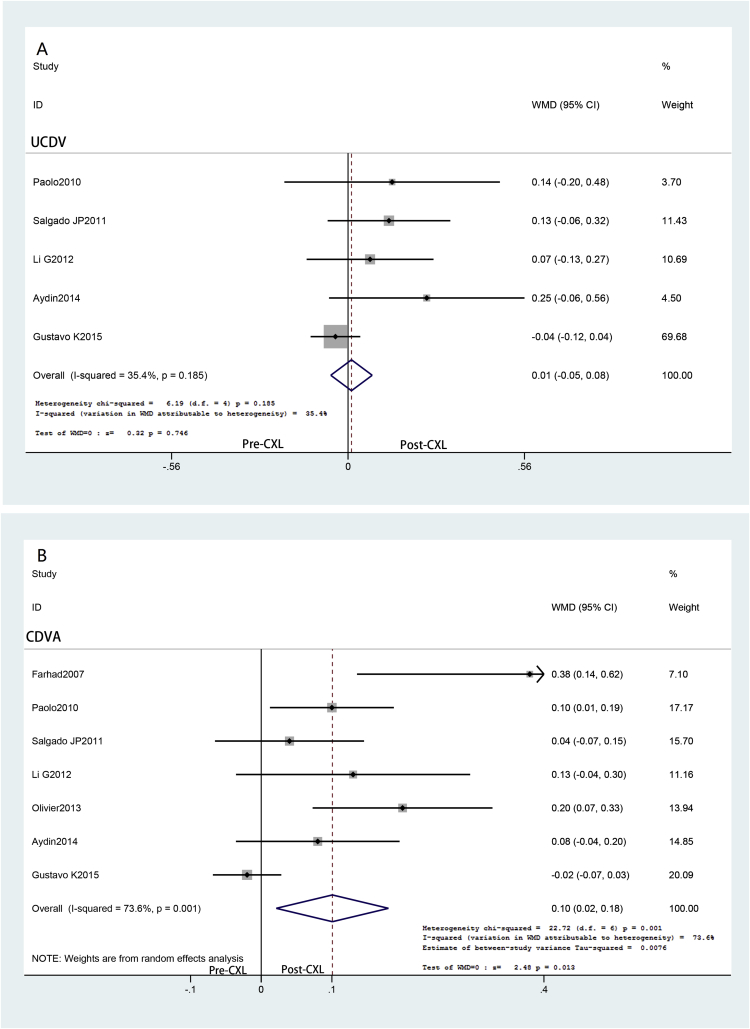
Visual acuity outcomes
The outcomes of UCVA and CDVA are shown in Fig. 2. Visual acuity was recorded and analyzed as the logarithm of the minimum angle of resolution (logMAR) value. In comparison with the preoperation baseline, there was no significantly different in UCVA after CXL operation (WMD = 0.011; 95% CI: −0.055 to 0.077; P = 0.746) (Fig. 2A), and no statistically significant heterogeneity between studies was identified (P = 0.746, I2 = 35.4%). However, compared with the preoperation, the CDVA significantly improved in post-CXL (WMD = 0.045; 95% CI: 0.010 to 0.079; P = 0.011) (Fig. 2B), while heterogeneity was observed there (P = 0.001, I2 = 73.6%). Then a leave-one-out analysis was conducted.12, 22 When Gustavo K 2015 was removed, it improved significantly in patients undergoing CXL surgery compared with preoperation (WMD = 0.123; 95% CI: 0.054 to 0.191; P = 0.000) and no significant heterogeneity existed (P = 0.124, I2 = 42.4%). There was no significant publication bias by Begg's test (P = 0.452) or Egger's test (P = 0.622).
Fig. 2.
Change in visual acuity after cornea cross-linking (CXL) treatment: the corrected distant visual acuity (CDVA) change (A) and the uncorrected visual acuity (UCVA) change (B). WMD: Weighted mean difference.
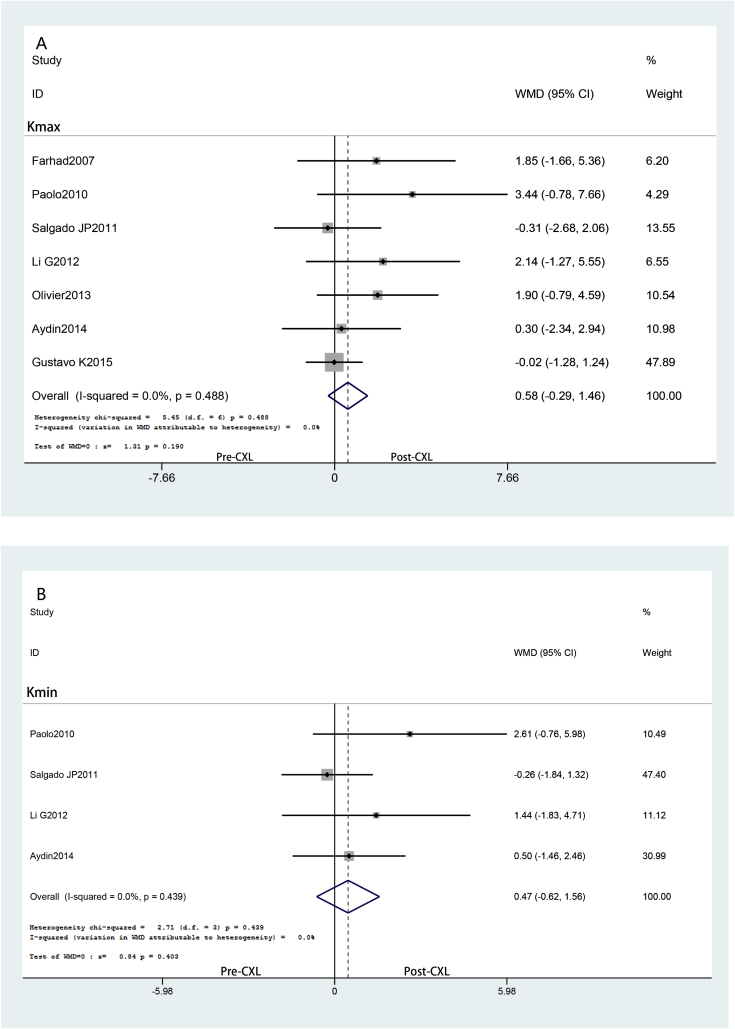
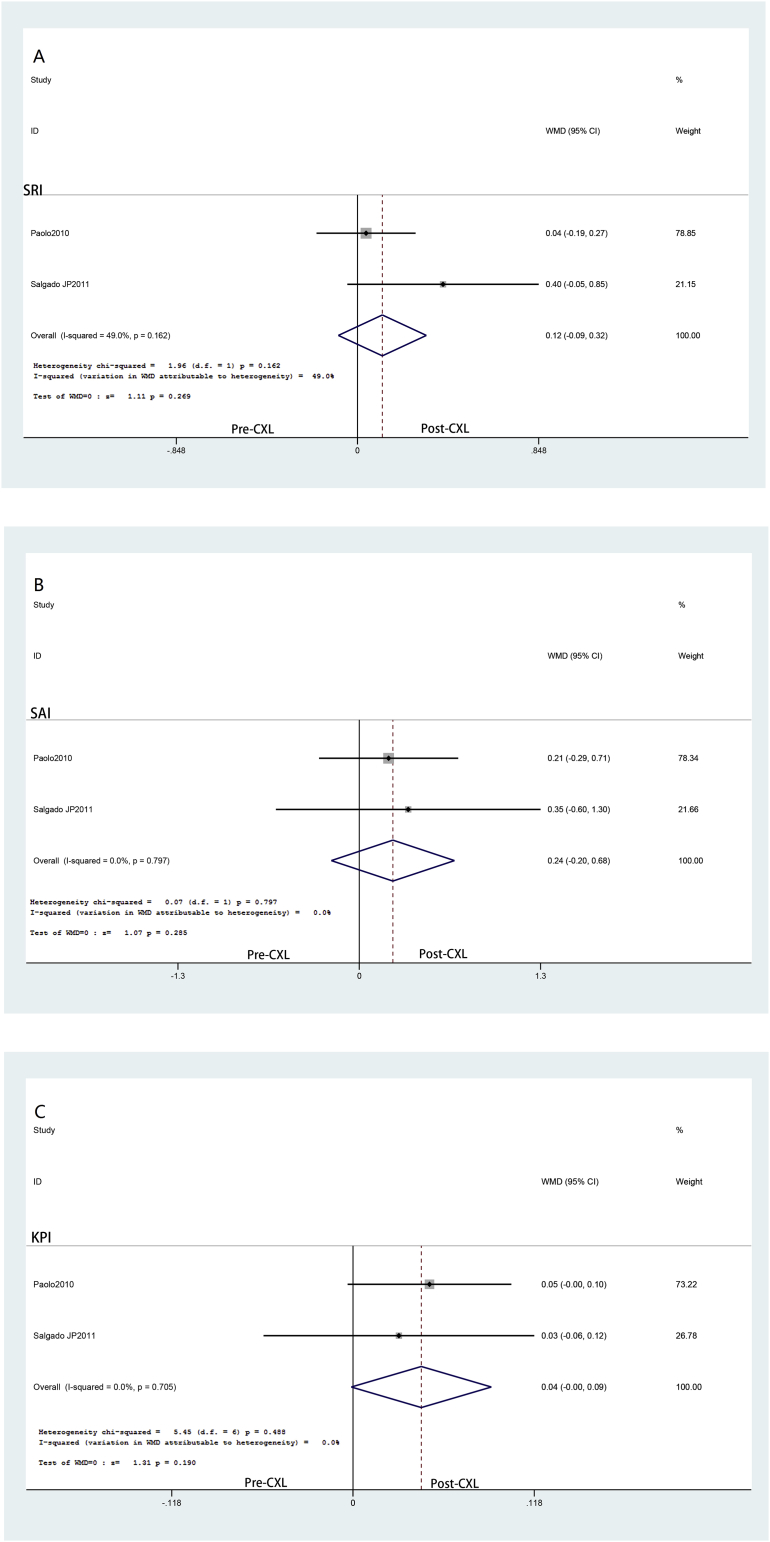
Topographic results
The results of Kmax and Kmin are shown in Fig. 3, indicating that both Kmax (WMD = 0.584; 95% CI: −0.289 to 1.458; P = 0.19) (Fig. 3A) and Kmin (WMD = 0.466; 95% CI: −0.625 to 1.556; P = 0.403) (Fig. 3B) had no statistically significant differences. Meanwhile, there was no heterogeneity found (P = 0.488, I2 = 0%; P = 0.439, I2 = 0%, respectively). Only two studies provided the following topographic parameters: the surface regularity index (SRI), the surface asymmetry index (SAI) and the keratoconus prediction index (KPI). The analysis of these data showed (in Fig. 4) that the pre-post value had no changes in SRI (WMD = 0.116; 95% CI: −0.090 to 0.322; P = 0.269) (Fig. 4A), SAI (WMD = 0.240; 95% CI: −0.200 to 0.681; P = 0.285) (Fig. 4B), and KPI (WMD = 0.045; 95% CI: −0.001 to 0.090; P = 0.056) (Fig. 4C). No heterogeneity was found (P = 0.162, I2 = 49%; P = 0.797, I2 = 0%; P = 0.705, I2 = 0%, respectively).
Fig. 3.
Change in maximum keratometry (Kmax) (A) and minimum keratometry (Kmin) (B) after cornea cross-linking (CXL) treatment. WMD: Weighted mean difference.
Fig. 4.
The primary outcomes in the surface regularity index (SRI) (A), the surface asymmetry index (SAI) (B) and the keratoconus prediction index (KPI) (C) after cornea cross-linking (CXL) treatment. WMD: Weighted mean difference.
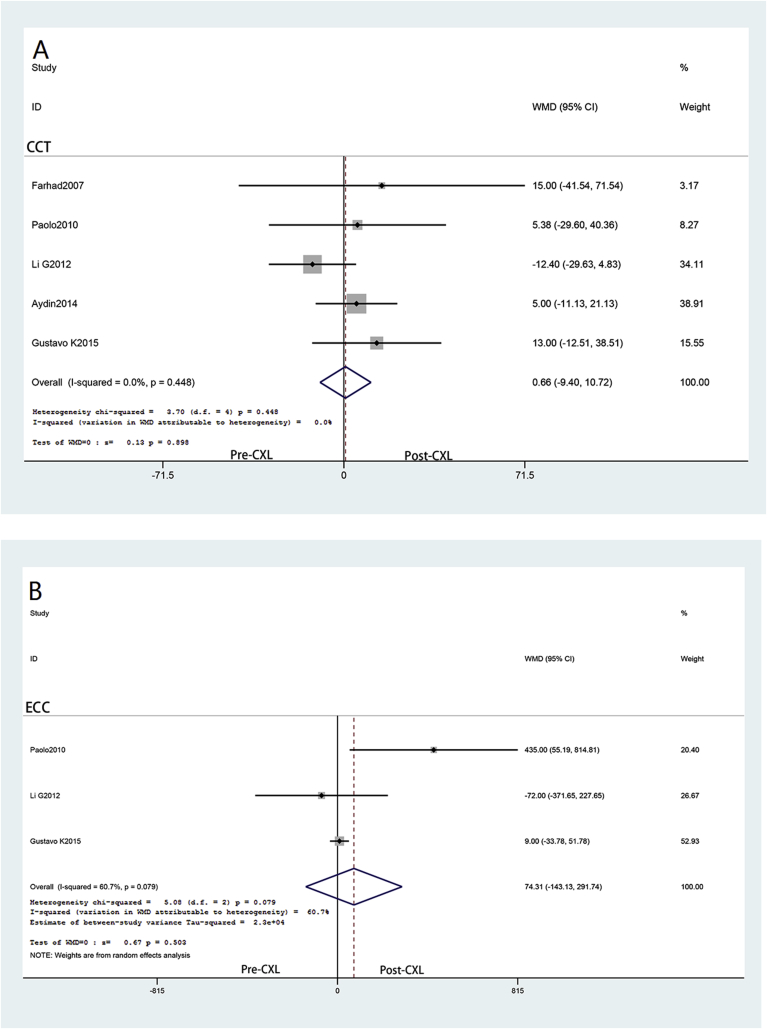
Central corneal thickness and endothelial cell count
Five studies reported corneal thickness data and three studies provided endothelial cell count (shown in Fig. 5). The analysis of these data manifested that the pre- and post-CXL value differences in corneal thickness, and endothelial cell count was not statistically significant (WMD = 0.657; 95% CI: −9.402 to 10.717; P = 0.898 (Fig. 5A); WMD = 12.634; 95% CI: −29.460 to 54.729; P = 0.556; (Fig. 5B), respectively). Additionally, no statistically significant heterogeneity between studies was identified in comparison of corneal thickness (P = 0.448, I2 = 0), but existed in endothelial cell count (P = 0.079, I2 = 60.7%).
Fig. 5.
Change in corneal thickness (CCT) (A) and endothelial cell count (ECC) (B) after cornea cross-linking (CXL) treatment. WMD: Weighted mean difference.
Discussion
Although laser refractive surgery has become increasingly safe and predictable in the past 20 years, more and more complications were reported. Post-refractive-surgery keratectasia, first described by Seiler and Quurke in 1998, was recognized as a rare but major sight-threatening complication of corneal refractive laser surgery.23, 24 Traditional treatment for ectasia after laser refractive surgery follows the keratoconus scheme. The use of CXL has shown the potential for slowing or eliminating the progression of keratoconus.7 Recently, several studies with variable outcomes about CXL treatment for post-refractive-surgery ectasia have been published. According to what we know, this is the first meta-analysis about CXL study for post-refractive-surgery corneal ectasia. The pooled results manifested that CXL was effective in stabilizing keratectasia after refractive surgery.
Visual acuity maybe one of most important criteria that reflects the efficacy of CXL treatment. Based on this meta-analysis, the impact of CXL on visual acuity is remarkable. Although the uncorrected distant visual acuity (UDVA) remained stable, significant improvement in CDVA was observed. From the studies included in our meta-analysis, Hafezi et al. reported that CDVA increased by one more lines in 9 (90%) eyes. Gustavo et al. reported that CDVA was stable or improved in 72.5% of all patients after 2 years, and Richoz et al. reported that CDVA improved (gain of ≥1 line) in 19 cases and remained stable in 7 patients. No patient showed deterioration of visual acuity (loss of ≥1 line). The possible reasons for improvement in CDVA (not UDVA) is that corneal CXL may cause a tendency towards improvement of the ectatic cornea, with possible partial recentration of the optical Zone. The same result was also found in keratoconus after crosslinking.25
In the present analysis, topographic indices were investigated because they are important parameters for determining whether a keratoconic or postoperative ectasia has worsened. An examination of the forest plot showed that both keratometric readings and topographic parameters (SRI, SAI, and KPI) were still maintaining stability and not improving as reported in studies involving keratoconic eyes.19, 26 These results indicate that post-laser refractive surgery ectatic corneas may have a less positive response to CXL compared with keratoconic corneas. The reason perhaps is that CXL preferentially strengthens the anterior stroma, which is weakened by flap generation and tissue ablation. Also, for post-lasik corneal ectasia, the riboflavin diffusion may be reduced due to the flap interface, affecting the CXL result. This distinct responses also reported by Greenstein et al.27
Endothelial cell count and corneal thickness were also included in the current analysis to assess the safety of CXL procedure. Endothelial cell count and corneal thickness remained unchanged during post-CXL, with the longest follow-up more than 62 months after CXL. Almost all studies reported that there were no serious complications, such as epithelial ingrowth, elevations of the flap margin, infectious keratitis, cataract formation, or retinal damage. The most common complication was an early corneal haze, which is short-lived and does not affect vision.
The present study has limitations and biases that result from the quality of the individual trials and the methods of the meta-analysis. First, the number of included clinical trials was relatively small. Some outcomes such as intraocular pressure or corneal bio-mechanics changes can not be analyzed due to a lack of data. Second, the included trials varied with population, participant age, clinical measurement, follow-up period, and quality. Third, the previously published studies are almost all non-randomized trials. No randomized clinical trials are available for cross-linking because of the lack of ethics of such studies,12, 13 thus, increasing the risk of diverse bias and decreasing reliability. However, the results are promising and indicate that it would be worthy to further investigate this treatment in iatrogenic ectasia after corneal refractive surgery.
In conclusion, in this systematic review and meta-analysis, CXL is a safe and effective approach in halting the progression of iatrogenic ectasia after corneal refractive surgery. The effect of CXL on CDVA improvement is remarkable. Further larger and longer studies are needed to confirm the results.
Footnotes
Ethics: Not applicable.
Consent to publish: Not applicable.
Competing interests: All authors declare that they have no competing interests.
Availability of data and materials: All data supporting findings in our article can be found.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Comaish I.F., Lawless M.A. Progressive post-LASIK keratectasia: biomechanical instability or chronic disease process? J Cataract Refract Surg. 2002;28(12):2206–2213. doi: 10.1016/s0886-3350(02)01698-x. [DOI] [PubMed] [Google Scholar]
- 2.Hafezi F., Kanellopoulos J., Wiltfang R., Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33(12):2035–2040. doi: 10.1016/j.jcrs.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 3.Binder P.S. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29(12):2419–2429. doi: 10.1016/j.jcrs.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Tan D.T., Por Y.M. Current treatment options for corneal ectasia. Curr Opin Ophthalmol. 2007;18(4):284–289. doi: 10.1097/ICU.0b013e3281a7ecaa. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez L.A., Guillen P.B., Benavides M.A., Garcia L., Porras D., Daqui-Garay R.M. Penetrating keratoplasty versus intrastromal corneal ring segments to correct bilateral corneal ectasia: preliminary study. J Cataract Refract Surg. 2007;33(3):488–496. doi: 10.1016/j.jcrs.2006.09.048. [DOI] [PubMed] [Google Scholar]
- 6.Bilgihan K., Ozdek S.C., Sari A., Hasanreisoğlu B. Excimer laser-assisted anterior lamellar keratoplasty for keratoconus, corneal problems after laser in situ keratomileusis, and corneal stromal opacities. J Cataract Refract Surg. 2006;32(8):1264–1269. doi: 10.1016/j.jcrs.2006.02.056. [DOI] [PubMed] [Google Scholar]
- 7.Wollensak G., Spoerl E., Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 8.Spoerl E., Huhle M., Seiler T. Induction of cross-links in corneal tissue. Exp eye Res. 1998;66(1):97–103. doi: 10.1006/exer.1997.0410. [DOI] [PubMed] [Google Scholar]
- 9.Chunyu T., Xiujun P., Zhengjun F., Xia Z., Feihu Z. Corneal collagen cross-linking in keratoconus: a systematic review and meta-analysis. Sci Rep. 2014;4:5652. doi: 10.1038/srep05652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He M., Huang W., Zhong X. Central corneal sensitivity after small incision lenticule extraction versus femtosecond laser-assisted LASIK for myopia: a meta-analysis of comparative studies. BMC Ophthalmol. 2015;15:141. doi: 10.1186/s12886-015-0129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J., Ji P., Lin X. Efficacy of corneal collagen cross-linking for treatment of keratoconus: a meta-analysis of randomized controlled trials. PLoS One. 2015;10(5):e0127079. doi: 10.1371/journal.pone.0127079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meiri Z., Keren S., Rosenblatt A., Sarig T., Shenhav L., Varssano D. Efficacy of corneal collagen cross-linking for the treatment of keratoconus: a systematic review and meta-analysis. Cornea. 2016;35(3):417–428. doi: 10.1097/ICO.0000000000000723. [DOI] [PubMed] [Google Scholar]
- 14.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. [PubMed] [Google Scholar]
- 16.Yildirim A., Cakir H., Kara N. Corneal collagen crosslinking for ectasia after laser in situ keratomileusis: long-term results. J Cataract Refract Surg. 2014;40(10):1591–1596. doi: 10.1016/j.jcrs.2014.01.042. [DOI] [PubMed] [Google Scholar]
- 17.Vinciguerra P., Camesasca F.I., Albe E., Trazza S. Corneal collagen cross-linking for ectasia after excimer laser refractive surgery: 1-year results. J Refract Surg. 2010;26(7):486–497. doi: 10.3928/1081597X-20090910-02. [DOI] [PubMed] [Google Scholar]
- 18.Salgado J.P., Khoramnia R., Lohmann C.P., Winkler von Mohrenfels C. Corneal collagen crosslinking in post-LASIK keratectasia. Br J Ophthalmol. 2011;95(4):493–497. doi: 10.1136/bjo.2010.179424. [DOI] [PubMed] [Google Scholar]
- 19.Richoz O., Mavrakanas N., Pajic B., Hafezi F. Corneal collagen cross-linking for ectasia after LASIK and photorefractive keratectomy: long-term results. Ophthalmology. 2013;120(7):1354–1359. doi: 10.1016/j.ophtha.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 20.Marino G.K., Torricelli A.A., Giacomin N., Santhiago M.R., Espindola R., Netto M.V. Accelerated corneal collagen cross-linking for postoperative LASIK ectasia: two-year outcomes. J Refract Surg. 2015;31(6):380–384. doi: 10.3928/1081597X-20150521-04. [DOI] [PubMed] [Google Scholar]
- 21.Li G., Fan Z.J., Peng X.J. Corneal collagen crosslinking for corneal ectasia of post-LASIK: one-year results. Int J Ophthalmol. 2012;5(2):190–195. doi: 10.3980/j.issn.2222-3959.2012.02.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang W., Zhou M., Huang W., Zhang X. Ex-PRESS implantation versus trabeculectomy in uncontrolled glaucoma: a meta-analysis. PLoS One. 2013;8(5):e63591. doi: 10.1371/journal.pone.0063591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seiler T., Quurke A.W. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998;24(7):1007–1009. doi: 10.1016/s0886-3350(98)80057-6. [DOI] [PubMed] [Google Scholar]
- 24.Seiler T., Koufala K., Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14(3):312–317. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 25.Caporossi A., Baiocchi S., Mazzotta C., Traversi C., Caporossi T. Parasurgical therapy for keratoconus by riboflavin-ultraviolet type A rays induced cross-linking of corneal collagen: preliminary refractive results in an Italian study. J Cataract Refract Surg. 2006;32(5):837–845. doi: 10.1016/j.jcrs.2006.01.091. [DOI] [PubMed] [Google Scholar]
- 26.Tomita M., Mita M., Huseynova T. Accelerated versus conventional corneal collagen crosslinking. J Cataract Refract Surg. 2014;40(6):1013–1020. doi: 10.1016/j.jcrs.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 27.Greenstein S.A., Fry K.L., Hersh P.S. Corneal topography indices after corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37(7):1282–1290. doi: 10.1016/j.jcrs.2011.01.029. [DOI] [PubMed] [Google Scholar]