Abstract
Previous data indicate that Tankyrase inhibitors exert anti-growth functions in many cancer cell lines due to their ability to inactivate the YAP protooncogene. In the present manuscript, we investigated the effect of Tankyrase inhibitors on the growth of hepatocellular carcinoma (HCC) cell lines and the molecular mechanisms involved. For this purpose, we performed cell proliferation assay by colony-forming ability in seven human HCC cells subjected to XAV-939 and G007-LK Tankyrase inhibitors. Noticeably, the two Tankyrase inhibitors suppressed the HCC cell growth in a dose-dependent manner. Furthermore, we found that Tankyrase inhibitors synergized with MEK and AKT inhibitors to suppress HCC cell proliferation. At the molecular level, Tankyrase inhibitors significantly decreased YAP protein levels, reduced the expression of YAP target genes, and inhibited YAP/TEAD luciferase reporter activity. In addition, Tankyrase inhibitors administration was accompanied by upregulation of Angiomotin-like 1 (AMOTL1) and Angiomotin-like 2 (AMOTL2) proteins, two major negative regulators of YAP. Altogether, the present data indicate that XAV-939 and G007-LK Tankyrase inhibitors could suppress proliferation of hepatocellular carcinoma cells and downregulate YAP/TAZ by stabilizing AMOTL1 and AMOTL2 proteins, thus representing new potential anticancer drugs against hepatocellular carcinoma.
Introduction
Liver cancer is one of the most common malignant tumors and the second leading lethal cancer worldwide. Hepatocellular carcinoma (HCC) accounts for 90% of primary liver cancer with approximately 850,000 new cases annually [1]. In the early stage of the disease, resection, liver transplantation and local ablation have curative possibilities, whereas only chemoembolization and sorafenib administration provide limited survival benefits in advanced HCC [2]. Thus, there is an urgent need for novel therapies to improve significantly the outcome of HCC patients.
Tankyrases belong to a family of enzymes called poly ADP ribosyl polymerases (PARPs) and take part in various cellular and molecular functions, such as Wnt/β-catenin signaling, telomere homeostasis, glucose metabolism, and cell cycle progression. Tankyrases play an important role in a variety of diseases including cancer, inflammation, infections, and obesity [3]. Tankyrase1 and Tankyrase 2 are the two main members of the family and share 82% sequence identity. Of note, tankyrases have been found to be significantly elevated in human HCC [4]. In this tumor type, the XAV-939 and G007-LK selective Tankyrase1/2 inhibitors effectively block the Wnt–β-catenin signaling and induce growth restraint of HCC cells [4, 5].
Yes-associated protein (YAP) is a major core effector of the Hippo pathway, whose deregulation can promote cancer development in various tissues and organs [6]. Once activated, YAP acts as transcriptional co-activator by binding to TEA domain (TEAD) DNA binding proteins in the nucleus to initiate the expression of target genes [6]. In particular, recent studies have found that YAP exerts multiple functions on normal and cancer cells via its ability to interact with multiple signaling pathways, such as Wnt/β-catenin [7], Notch [8], EGF [9], and TGFβ [10] cascades, involved in cell proliferation, tissue regeneration, and stem cell self-renewal [6–11]. Angiostatin binding proteins, including Angiomotin-like 1 (AMOTL1) and Angiomotin-like 2 (AMOTL2), are critical negative regulators of YAP, as they inhibit its nuclear translocation [12]. Importantly, it has been found that Tankyrase proteins are able to interact with Angiomotins and enhance their degradation through the RNF146b E3 ligase, with consequent YAP activation [13–15].
Mounting evidence indicates that YAP is expressed in the vast majority of human HCC specimens [16–18], where its elevated levels and nuclear accumulation represent an independent prognostic indicator [16–18]. Due to the concomitant activation of YAP and Tankyrases observed in HCC, it is tempting to speculate that suppression of YAP activity via inhibition of Tankyrases might be therapeutically relevant for the treatment of this deadly disease. In the present study, to test this hypothesis, we examined the effects of two Tankyrase inhibitors, XAV-939 and G007-LK, on the in vitro growth of 7 human HCC cell lines. In particular, we investigated the effects of Tankyrase inhibitors on the YAP pathway. Furthermore, we evaluated whether Tankyrase inhibitors synergize with AKT or MEK inhibitors to inhibit HCC cell growth. The data obtained strongly suggest that Tankyrase inhibitors might be potentially effective anticancer drugs against HCC.
Materials and methods
Cell lines and culture
SNU-475, SNU-449, and SNU-398 HCC cells were obtained from ATCC (Manassas, VA); HLE and Huh7 cells from JCRB Cell Bank (Osaka, Japan); MHCC97H and MHCC97L cells from Liver Center Research Institute, Fudan University (Shanghai, China). HLE, Huh7, MHCC97-L, and MHCC97-H HCC cell lines were cultured in Dulbecco’s modified Eagle medium (DMEM) supplemented with 10% FBS, penicillin (100 U/mL), and streptomycin (100 μg/mL). SNU-475, SNU-449, and SNU-398 HCC cells were instead cultured in Roswell Park Memorial Institute 1640 (RPMI 1640) medium supplemented with 10% FBS, penicillin (100 U/mL), and streptomycin (100 μg/mL) in a humidified 5% CO2 incubator at 37°C. All cell lines underwent validation before being used in the experiments (Genetica DNA Laboratories, Burlington, NC)
Clonogenic assay and assessment of proliferation and apoptosis
For clonogenic proliferation assay, the HCC cell lines were plated in triplicate at 1 X 103/well in 6-well plates (SNU-449 0.5 X 103/well). HCC cells were treated with 0.1% DMSO, or 2.5 μM, 5 μM, 10 μM, 20μM XAV-939 (ApexBio, Houston, TX) or G007-LK (ApexBio) until colonies became sufficiently large to be quantified. The medium with DMSO or inhibitors was replaced every 3 days. After 10–14 days, colonies were washed by PBS and dyed with crystal violet for at least 10 minutes at room temperature. Subsequently, the dye was washed off and colonies were counted. For cell proliferation or apoptosis assays, SNU-449 and HLE cells were grown in a 5% CO2 atmosphere, at 37°C, in RPMI Medium supplemented with 10% fetal bovine serum (FBS; Gibco, Grand Island, NY) and penicillin/streptomycin (Gibco). HCC cells were treated with 0.1% DMSO, or 2.5 μM, 5 μM, 10 μM, 20μM XAV-939 (ApexBio) or G007-LK (ApexBio), either alone or in combination with the MEK inhibitor U0126 (25 μM; Cell Signaling Technology Inc., Danvers, MA) or the AKT inhibitor MK-2206 (5 μM; ThermoFisher Scientific, Waltham, MA). Cell proliferation was analyzed using the BrdU Cell Proliferation Assay Kit (Cell Signaling Technology Inc.), while apoptosis was assessed with the Cell Death Detection Elisa Plus Kit (Roche Molecular Biochemicals, Indianapolis, IN), following the manufacturers’ protocols.
Quantitative real-time reverse-transcription polymerase chain reaction
mRNA was isolated from fresh SNU-449 and HLE cells after 48h with 0.1% DMSO, 10μM XAV-939 or 10μM G007-LK treatment using the Quick-RNA™ MiniPrep (Zymo Research, Irvine, CA). Reverse transcription was conducted according to the manufacturer's instructions (Invitrogen Carlsbad, CA). The human primers used for PCR analysis were synthesized by Integrated DNA Technologies (Coralville, IA). The sequences of the primers were as follows: Connective tissue growth factor (CTGF), 5′-CCAATGACAACGCCTCCTG-3′ (forward) and 5′-GAGCTTTCTGGCTGCACCA-3′ (reverse); Cysteine rich angiogenic inducer 61 (Cyr61), 5′- GGTCAAAGTTACCGGGCAGT-3′ (forward) and 5′- GGAGGCATCGAATCCCAG-3′ (reverse); YAP, 5′-TAGCCCTGCGTAGCCAGTTA -3′ (forward) and 5′-TCATGCTTAGTCCACTGTCTGT -3′ (reverse); Glyceraldehyde-3-phosphate dehydrogenase (GAPDH), 5′-ATGGGGAAGGTGAAGGTCG-3′ (forward) and 5′-GGGGTCATTGATGGCAACAATA-3′ (reverse). Quantitative real-time polymerase chain reaction was performed with 100 ng of cDNA, using an ABI Prism 7000 Sequence Detection System and TaqMan Universal PCR Master Mix (ThermoFisher Scientific). Cycling conditions were: 10 min of denaturation at 95°C and 40 cycles at 95°C for 15 s and at 52°C for 1 min. Quantitative values were calculated by using the PE Biosystems Analysis software and expressed as N target (NT). NT = 2-ΔCt, wherein the ΔCt value of each sample was calculated by subtracting the average Ct value of the target gene from the average Ct value of the GAPDH gene.
Dual-luciferase reporter assay
SNU-449 and HLE Cells were plated in triplicate in 24-well plate at 70–80% confluency and were co-transfected with 500ng of TEAD luciferase reporter plasmid (8xGTIIC-luciferase, Addgene plasmid #34615), 20ng of pRL-CMV Renilla luciferase plasmid (Promega, Madison, WI) and 1μL Lipofectamine 2000 per well (Invitrogen). The culture medium was replaced by Opti-MEM® Reduced Serum. After 4-hour incubation, the transfection mixture was replaced by culture medium with 0.1%DMSO, 10μM XAV-939, or 10μM G007-LK. At 48 hours, the cells were rinsed in 1X PBS and harvested with Passive Lysis Buffer in a new tube on ice. Luciferase activity was measured using the Dual-Luciferase® Reporter Assay System (Promega), according to the manufacturer’s protocol.
Western blot analysis
Cells were washed in PBS and lysed in M-PER™ Mammalian Protein Extraction Reagent (ThermoFisher Scientific) containing the Halt™ Protease Inhibitor Cocktail (ThermoFisher Scientific). Nuclear extraction was performed using NE-PER™ Nuclear and Cytoplasmic Extraction Reagents (ThermoFisher Scientific). Protein concentration was quantified using the Pierce™ Microplate BCA Protein Assay Kit (ThermoFisher Scientific). Membranes were blocked in in 5% non-fat milk for 1 hour and incubated with the following primary antibodies: YAP (1:1000; Cell Signaling Technology), YAP/TAZ (1:1000; Cell Signaling Technology), AMOTL1 (1:1000; Sigma-Aldrich, St. Louis, MO), AMOTL2 (1:1000, Sigma-Aldrich), p-YAP(Ser127) (1:1000; Cell Signaling Technology), Histone H3 (1:2000; Cell Signaling Technology), β-tubulin (1:1000; abcam), t-AKT (1:1000; Cell Signaling Technology), p-AKT (1:1000; Cell Signaling Technology), t-ERK (1:1000; Cell Signaling Technology), and p-ERK (1:1000; Cell Signaling Technology). β-actin (1:5000; Sigma-Aldrich, St. Louis, MO) and GAPDH (1:10000; EMD Millipore, Billerica, MA) were used as a loading controls. Each primary antibody was followed by incubation with secondary antibody (1:5000; Jackson ImmunoResearch Laboratories Inc. West Grove, PA) for 1 hour and bands were revealed with the Super Signal West Dura (ThermoFisher Scientific).
Statistical analysis
Statistical analysis was performed using Student’s t-test and Tukey-Kramer test. The data were expressed as the mean±SD of at least three independent experiments. P <0.05 was considered significant.
Results
XAV-939 and G007-LK restrain HCC cell growth in vitro
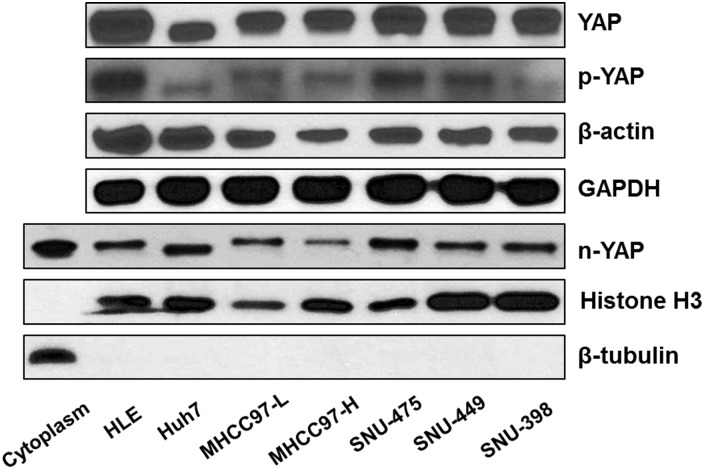
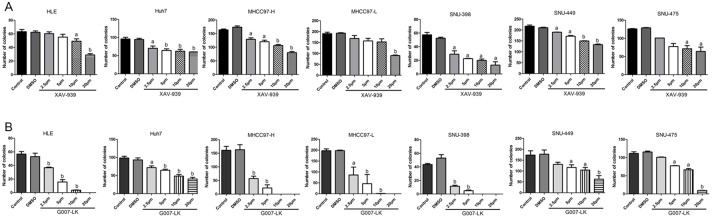
First, we determined YAP expression in a panel of 7 human HCC cell lines, including HLE, Huh7, MHCC97-L, MHCC97-H, SNU-475, SNU-449, and SNU-398 cells. We found that all 7 cells express YAP as well as phosphorylated YAP (p-YAP) (Fig 1 and S4 Fig). Importantly, analysis of nuclear protein extracts showed that YAP is localized in the nucleus of all HCC cell lines tested, thus indicating the ubiquitous activation of YAP in these cells (Fig 1 and S4 Fig). As Tankyrase inhibitors have been shown to suppress tumor cell growth via inhibiting YAP [13–15], we investigated the effect of two Tankyrase inhibitors, XAV-939 and G007-LK, in regulating HCC cell growth. Both XAV-939 and G007-LK displayed a dose-dependent growth inhibitory effect on all 7 HCC cell lines tested, as assessed by colony formation assay (Fig 2A and 2B). In general, G007-LK exhibited a higher growth inhibitory activity than that of XAV-939 (Fig 2A and 2B).
Fig 1. YAP expression in human HCC cell lines.
Total YAP, phosphorylated (p-)YAP as well as nuclear YAP (n-YAP) protein levels were analyzed in a panel of 7 human HCC cell lines by Western blotting. β-actin and GAPDH were used as loading controls for total cell lysate. Histone H3 and β-tubulin were used as controls for nuclear and cytoplasmic extraction, respectively. The experiments were repeated twice.
Fig 2. The XAV-939 and G007-LK Tankyrase inhibitors suppress HCC cell growth.
Colony formation assay was used to determine the growth inhibitory effects of XAV-939 (A) and G007-LK (B) in the panel of 7 HCC cell lines. Student’s t-test: (a) p<0.05 vs DMSO; (b) p<0.01 vs DMSO. Colony formation assay was repeated three times for each drug in each cell line.
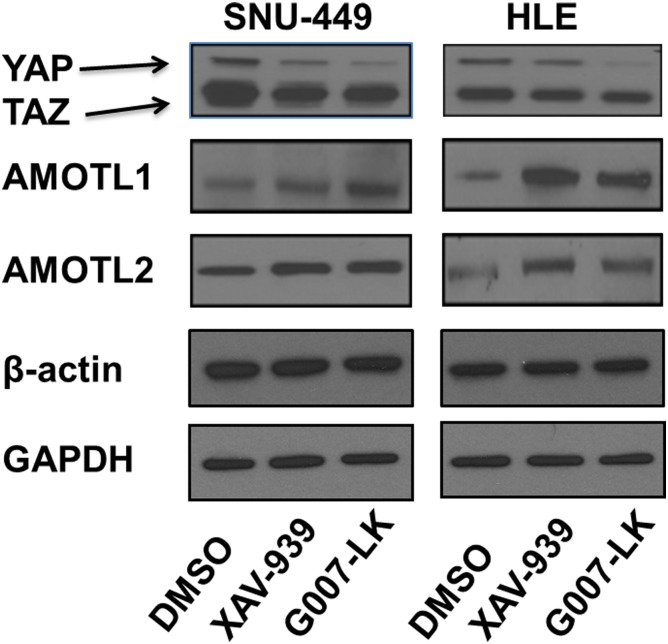
XAV-939 and G007-LK downregulate the levels of YAP and its targets by upregulating AMOTL1 and AMOTL2
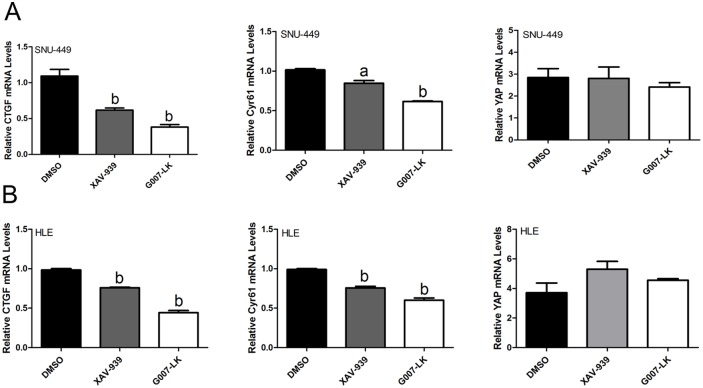
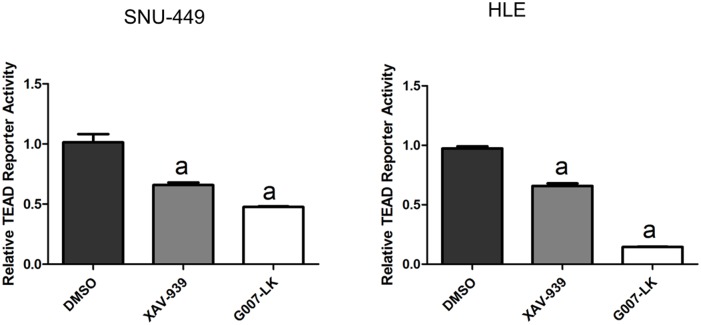
Next, we investigated whether the XAV-939 and G007-LK Tankyrase inhibitors suppress YAP signaling in HCC cells. For this purpose, initially we assessed the mRNA expression of YAP and its downstream effectors CTGF and Cyr61 by qRT-PCR. We found that the mRNA levels of CTGF and Cyr61, but not YAP, were significantly decreased in SNU-449 and HLE cells following the treatment with XAV-939 and G007-LK (Fig 3). In addition, YAP/TEAD luciferase reporter activity was significantly inhibited following the administration of XAV-939 and G007-LK (Fig 4), supporting the notion that Tankyrase inhibitors constrain the transcriptional activity of YAP. Consistent with the stronger growth inhibitory effects by G007-LK, this drug exhibited a more pronounced inhibitory activity towards YAP target gene expression and TEAD luciferase activity than that following XAV-939 administration (Figs 3 and 4). At the protein level, a decline in YAP amount and an increase in AMOTL1 and AMOTL2 expression were detected in cells treated XAV-939 or G007-LK when compared with control DMSO treated cells (Fig 5 and S5 Fig). Protein levels of TAZ, a paralog of YAP, were instead not affected by treatment with Tankyrase inhibitors (Fig 5 and S5 Fig).
Fig 3. Tankyrase inhibitors decrease mRNA expression of YAP target genes in HCC cell lines.
qRT-PCR analysis of mRNA expression of CTGF, Cyr61, and YAP in SNU-449 (A) and HLE (B) HCC cell lines upon treatment with XAV-939 and G007-LK inhibitors. Student’s t-test: (a) p<0.05 vs. DMSO; (b) p<0.01 vs. DMSO. qRT-PCR experiments were repeated three times.
Fig 4. Tankyrase inhibitors suppress TEAD-luciferase activity in HCC cell lines.
Relative TEAD reporter activity in SNU-449 and HLE HCC cells upon XAV-939 and G007-LK treatment is shown. Student’s t-test: (a) p<0.05 vs. DMSO; (b) p<0.01 vs. DMSO. Experiments were repeated three times.
Fig 5. Tankyrase inhibitors reduce YAP protein levels and increase AMOTL1 and AMOTL2 protein expression in HCC cell lines.
Western blot analysis of YAP, AMOTL1, and AMOTL2 in SNU-449 and HLE HCC cells upon XAV-939 or G007-LK treatment. β-actin and GAPDH were used as loading controls. Experiments were repeated twice.
In summary, our study demonstrates that Tankyrase inhibitors suppress YAP protein expression and activity via upregulation of AMOTL1 and AMOTL2 in HCC cells.
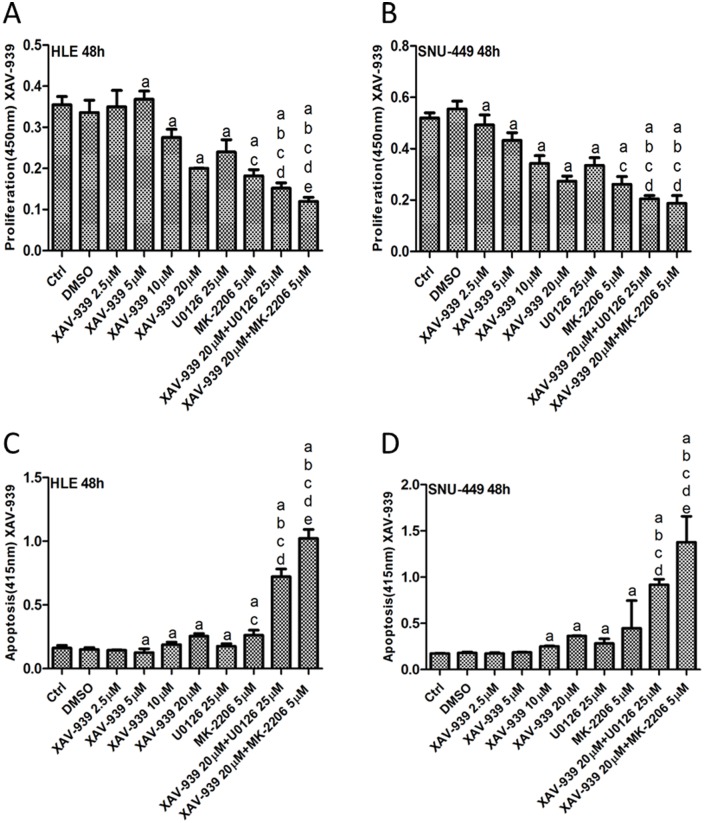
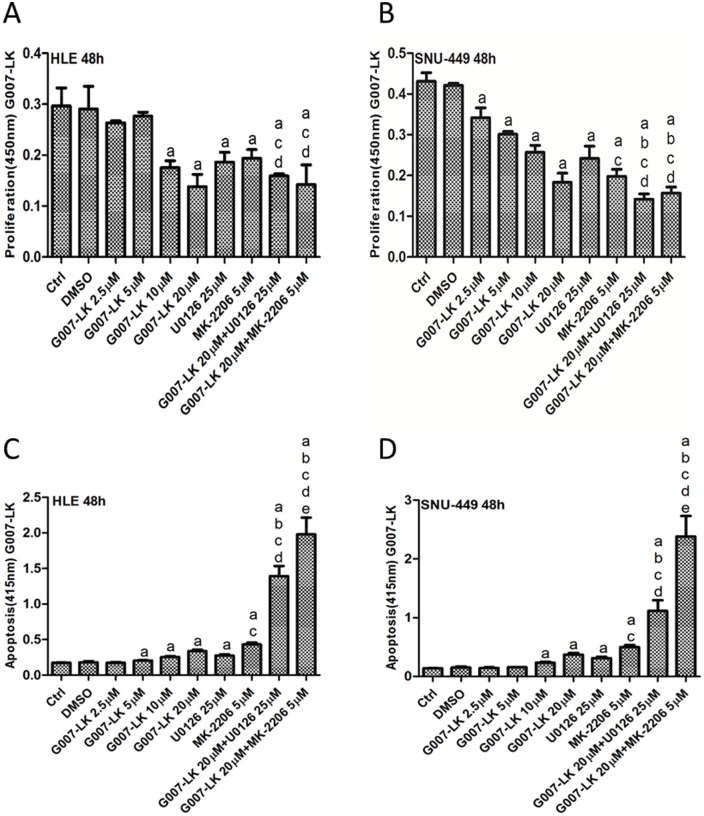
XAV-939 and G007-LK synergize with MEK and AKT inhibitors to suppress HCC cell proliferation in vitro
As Ras/MAPK and AKT/mTOR signaling cascades are critical pathways for tumor cell growth, MEK and AKT inhibitors have been developed. In human HCC, frequent activation of Ras/MAPK and AKT/mTOR pathways has been previously detected [19–22]. Thus, it is not surprising that MEK and AKT inhibitors are effective in restraining the growth of HCC cells [23–25]. In the light of these previous findings, we hypothesized that combined inhibition of YAP and MEK or AKT pathways will lead to increased growth restraint of HCC cells. To test this hypothesis, we treated SNU-449 and HLE cell lines with XAV-939 or G007-LK Tankyrase inhibitors, either alone or in combination with MEK inhibitor U0126 or AKT inhibitor MK-2206. We found that treating cells with XAV-939, G007-LK, U0126 or MK-2206 alone led to decreased HCC cell proliferation and increased apoptosis. Importantly, XAV-939 or G007-LK synergized with U0126 and MK-2206 to further constrain HCC cell growth and promote massive apoptotic cell death (Figs 6 and 7, S1 and S2 Figs). At the biochemical level, XAV-939/G007-LK, U0126 or MK-2206 effectively inhibited YAP, phosphorylated/activated (p)-ERK and p-AKT levels, respectively, in SNU-449 and HLE cells (S3 and S6 Figs). The results suggest that combining Tankyrase inhibitors with MEK or AKT inhibitors might be a novel, effective therapeutic strategy for the treatment of HCC.
Fig 6. XAV-939 synergizes with U0126 and MK-2206 to inhibit HCC cell growth.
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with XAV-939, U0126 or MK-2206, either alone or in combination, for 48 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM XAV-939 alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. XAV-939+U0126. Experiments were repeated three times in triplicate.
Fig 7. G007-LK synergizes with U0126 or MK-2206 to inhibit HCC cell growth.
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with G007-LK, U0126 or MK-2206, either alone or in combination for 48 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM G007-LK alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. G007-LK+U0126. Experiments were repeated three times in triplicate.
Discussion
Deregulation of Hippo signaling pathway leading to the increased expression and activation of YAP has been found in multiple tumor types [6, 26], including HCC [16–18, 27, 28]. In this tumor type, inactivation of Hippo and high nuclear YAP expression has been associated with poor prognosis of the patients [16–18, 29, 30]. The pro-oncogenic role of YAP in hepatocarcinogenesis has been demonstrated both in vitro and in vivo. Indeed, overexpression of activated forms of YAP promotes HCC cell proliferation and migration [17], whereas silencing of YAP inhibits HCC cell growth and induces apoptosis [17, 31]. YAP has also been identified as a key survival factor mediating the resistance to chemotherapeutic drugs [32] in various tumor types, including HCC [33, 34]. Importantly, in animal studies, it was found that inhibiting YAP expression triggers regression of advanced stage HCC and drive hepatocyte differentiation [35]. Also, overexpression of an activated form of YAP together with a mutant form of phosphatidylinositol-4,5-bisphosphate 3-Kinase catalytic subunit alpha (PIK3CA) induced the development of HCC and cholangiocarcinomas in the mouse liver [36]. Taken together, this body of evidence strongly supports the development of anti-YAP based therapeutic strategies for the treatment of HCC.
Currently, drugs which can directly target the Hippo/YAP cascade are still very limited [6, 37]. Verteporfin, a photosensitizer that is clinically used for the treatment of macular degeneration, is the only small molecule that is able to directly target YAP mediated transcriptional activity [38]. In HCC, it has been found that Verteporfin is able to effectively inhibit HCC cell growth both in vitro [36, 38] and in vivo [38]. Verteporfin treatment also decreased liver preneoplastic foci formation in mice [18]. However, studies have also demonstrated that Verteporfin has multiple targets, and its in vivo efficacy is very limited. Therefore, Verteporfin is not an ideal YAP targeting drug [39]. An alternative approach for inhibiting YAP is to use YAP RNAi-lipid nanoparticles (siYAP-LNP). For instance, Fitamant J. et al. showed that siYAP-LNP can efficiently induce HCC regression in liver specific Mst1/Mst2 knockout mice [35]. siYAP-LNP can also reverse liver enlargement in mice induced by Hippo inactivation [40]. However, the delivery efficacy of RNAi-lipid nanoparticles to human HCC and their effectiveness in the treatment of liver cancer remain to be determined. Clearly, it is imperative to identify additional approaches to successfully target YAP in the treatment of HCC.
Tankyrases are poly(ADP-ribose) polymerases that can induce the poly-ADP ribosylation of their substrates, leading to the change of subcellular localization or degradation of these substrates. Tankyrase substrates include a growing number of tumor suppressors, whose inactivation is implicated in cancer development and progression [13–15]. Therefore, Tankyrases have become attractive drug targets, and numerous small molecules able to inhibit Tankyrase activity have been developed, including G007-LK, NVP-TNKS656, WIKI4, and XAV-939 [41, 42]. In vitro and in vivo studies have demonstrated the excellent efficacy of these Tankyrase inhibitors for cancer treatment [43, 44]. Mechanistically, studies of Tankyrase inhibitors have been largely focusing on their ability to target and reactivate Axin proteins, thus leading to the inactivation of the Wnt/β-catenin signaling cascade [45, 46]. Recently, several studies suggest that Angiostatin binding protein family members (AMOT), which are involved in the negative regulation of YAP activity, are substrates of Tankyrases [13–15]. Tankyrase inhibitors, therefore, may inhibit YAP pathway by targeting AMOT proteins. However, whether Tankyrase inhibitors target YAP in HCC has not been investigated before. In the present study, we tested the hypothesis that Tankyrase inhibitors suppresses HCC cell growth via targeting the YAP pathway. For this purpose, we have chosen a panel of 7 HCC cell lines with high expression of YAP. Our findings indicate that the Tankyrase inhibitors G007-LK and XAV-939 are effective in inducing growth restraint in these cells. In addition, we show that G007-LK and XAV-939 cooperate with MEK and AKT inhibitors to further suppress HCC cell growth. Mechanistically, we demonstrated that, in HCC cells, administration of Tankyrase inhibitors increases AMOTL1 and AMOTL2 protein expression, leading to decreased YAP protein levels and transcriptional activity. Tankyrase treatment did not result in consistent changes of Ras/MAPK and AKT/mTOR pathways, two critical signaling cascades regulating HCC cell growth and survival (S3 Fig). This finding was expected as Tankyrases do not directly target these pathways. Importantly, the concomitant treatment of HCC cells with Tankyrase inhibitors and MEK or AKT inhibitors led to increased cell growth suppression (Figs 6 and 7). The precise mechanism(s) underlying this synergistic anti-growth effect remains to be defined. Nonetheless, our results strongly support further investigation on these combined therapies for HCC treatment.
It is interesting to note that activation of YAP and Wnt/β-catenin pathways characterizes two distinct molecular classes of human HCC. Recent studies have shown that co-activation of YAP and β-catenin frequently occurs in hepatoblastoma, a pediatric form of liver tumor, but rarely in HCC [47]. HCCs with activated β-catenin tend to be chromosomal stable [48], whereas YAP activation has recently been linked to chromosomal instability in HCCs [49]. Most importantly, inhibition of YAP in mouse liver tumors induced Wnt/β-catenin pathway activation and hepatocyte differentiation [35]. As Tankyrase inhibitors can target both YAP and Wnt/β-catenin cascades, these drugs may have rather broad anti-HCC efficacy. Furthermore, in HCCs with high YAP activity, Tankyrase inhibitors may prevent Wnt activation induced by YAP suppression.
Altogether, our study supports the hypothesis that Tankyrase inhibitors may represent novel and effective small molecules targeting YAP for HCC treatment. Obviously, additional experiments in vivo are required to evaluate the effectiveness of Tankyrase inhibitors for HCC treatment. For this purpose, appropriate preclinical models such as genetically engineered mouse (GEM) models and patient derived xenograft (PDX) models of liver cancer should be subjected to administration of Tankyrase inhibitors. In addition, it would be crucial to identify biomarkers, such as YAP nuclear localization or AMOTL1/2 downregulation, which can predict Tankyrase inhibitors’ therapeutic efficacy against HCC. Finally, the combined treatment of Tankyrase inhibitors with other drugs, including novel targeted therapy drugs or immunotherapy drugs, should be explored in detail in vitro and in vivo for HCC treatment.
Supporting information
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with XAV-939, U0126 or MK-2206, either alone or in combination for 72 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM XAV-939 alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. XAV-939+U0126. Experiments were repeated three times in triplicate.
(TIF)
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with G007-LK, U0126 or MK-2206, either alone or in combination for 72 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM G007-LK alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. G007-LK+U0126. Experiments were repeated three times in triplicate.
(TIF)
Western blot analysis of YAP, phosphorylated (p)-AKT and p-ERK levels in SNU-449 and HLE HCC cells upon treatment with XAV-939 and G007-LK, either alone or in combination with U0126 or MK-2206. Total (t-) AKT, ERK, and GAPDH were used as loading controls. Experiments were repeated twice.
(TIF)
(TIF)
(TIF)
(TIF)
Acknowledgments
We would like to thank Dr. Li Che for the technical and administrative support.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by NIH grants R01CA136606 to XC; P30DK026743 for UCSF Liver Center. This work was also supported by China Scholarship Council (201506175181) to JJ.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. doi: 10.1002/ijc.29210 . [DOI] [PubMed] [Google Scholar]
- 2.Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2016;2:16018 doi: 10.1038/nrdp.2016.18 . [DOI] [PubMed] [Google Scholar]
- 3.Haikarainen T, Krauss S, Lehtio L. Tankyrases: structure, function and therapeutic implications in cancer. Curr Pharm Des. 2014;20(41):6472–88. doi: 10.2174/1381612820666140630101525 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma L, Wang X, Jia T, Wei W, Chua MS, So S. Tankyrase inhibitors attenuate WNT/beta-catenin signaling and inhibit growth of hepatocellular carcinoma cells. Oncotarget. 2015;6(28):25390–401. doi: 10.18632/oncotarget.4455 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voronkov A, Holsworth DD, Waaler J, Wilson SR, Ekblad B, Perdreau-Dahl H, et al. Structural basis and SAR for G007-LK, a lead stage 1,2,4-triazole based specific tankyrase 1/2 inhibitor. J Med Chem. 2013;56(7):3012–23. doi: 10.1021/jm4000566 . [DOI] [PubMed] [Google Scholar]
- 6.Bae JS, Kim SM, Lee H. The Hippo signaling pathway provides novel anti-cancer drug targets. Oncotarget. 2017. Epub 2016/12/31. doi: 10.18632/oncotarget.14306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim W, Khan SK, Yang Y. Interacting network of Hippo, Wnt/beta-catenin and Notch signaling represses liver tumor formation. BMB Rep. 2016. doi: 10.5483/BMBRep.2017.50.1.196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy BV, Irvine KD. Regulation of Hippo signaling by EGFR-MAPK signaling through Ajuba family proteins. Dev Cell. 2013;24(5):459–71. doi: 10.1016/j.devcel.2013.01.020 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varelas X, Sakuma R, Samavarchi-Tehrani P, Peerani R, Rao BM, Dembowy J, et al. TAZ controls Smad nucleocytoplasmic shuttling and regulates human embryonic stem-cell self-renewal. Nat Cell Biol. 2008;10(7):837–48. doi: 10.1038/ncb1748 . [DOI] [PubMed] [Google Scholar]
- 10.Abylkassov R, Xie Y. Role of Yes-associated protein in cancer: An update. Oncol Lett. 2016;12(4):2277–82. doi: 10.3892/ol.2016.4955 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azzolin L, Zanconato F, Bresolin S, Forcato M, Basso G, Bicciato S, et al. Role of TAZ as mediator of Wnt signaling. Cell. 2012;151(7):1443–56. Epub 2012/12/19. doi: 10.1016/j.cell.2012.11.027 . [DOI] [PubMed] [Google Scholar]
- 12.Moleirinho S, Guerrant W, Kissil JL. The Angiomotins—from discovery to function. FEBS Lett. 2014;588(16):2693–703. doi: 10.1016/j.febslet.2014.02.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang W, Li N, Li X, Tran MK, Han X, Chen J. Tankyrase Inhibitors Target YAP by Stabilizing Angiomotin Family Proteins. Cell Rep. 2015;13(3):524–32. doi: 10.1016/j.celrep.2015.09.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang H, Lu B, Castillo J, Zhang Y, Yang Z, McAllister G, et al. Tankyrase Inhibitor Sensitizes Lung Cancer Cells to Endothelial Growth Factor Receptor (EGFR) Inhibition via Stabilizing Angiomotins and Inhibiting YAP Signaling. The Journal of biological chemistry. 2016;291(29):15256–66. doi: 10.1074/jbc.M116.722967 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Troilo A, Benson EK, Esposito D, Garibsingh RA, Reddy EP, Mungamuri SK, et al. Angiomotin stabilization by tankyrase inhibitors antagonizes constitutive TEAD-dependent transcription and proliferation of human tumor cells with Hippo pathway core component mutations. Oncotarget. 2016;7(20):28765–82. doi: 10.18632/oncotarget.9117 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han SX, Bai E, Jin GH, He CC, Guo XJ, Wang LJ, et al. Expression and clinical significance of YAP, TAZ, and AREG in hepatocellular carcinoma. J Immunol Res. 2014;2014:261365 Epub 2014/05/27. doi: 10.1155/2014/261365 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tschaharganeh DF, Chen X, Latzko P, Malz M, Gaida MM, Felix K, et al. Yes-associated protein up-regulates Jagged-1 and activates the Notch pathway in human hepatocellular carcinoma. Gastroenterology. 2013;144(7):1530–42 e12. doi: 10.1053/j.gastro.2013.02.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perra A, Kowalik MA, Ghiso E, Ledda-Columbano GM, Di Tommaso L, Angioni MM, et al. YAP activation is an early event and a potential therapeutic target in liver cancer development. J Hepatol. 2014;61(5):1088–96. doi: 10.1016/j.jhep.2014.06.033 . [DOI] [PubMed] [Google Scholar]
- 19.Calvisi DF, Ladu S, Gorden A, Farina M, Conner EA, Lee JS, et al. Ubiquitous activation of Ras and Jak/Stat pathways in human HCC. Gastroenterology. 2006;130(4):1117–28. doi: 10.1053/j.gastro.2006.01.006 . [DOI] [PubMed] [Google Scholar]
- 20.Calvisi DF, Wang C, Ho C, Ladu S, Lee SA, Mattu S, et al. Increased lipogenesis, induced by AKT-mTORC1-RPS6 signaling, promotes development of human hepatocellular carcinoma. Gastroenterology. 2011;140(3):1071–83. doi: 10.1053/j.gastro.2010.12.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ladu S, Calvisi DF, Conner EA, Farina M, Factor VM, Thorgeirsson SS. E2F1 inhibits c-Myc-driven apoptosis via PIK3CA/Akt/mTOR and COX-2 in a mouse model of human liver cancer. Gastroenterology. 2008;135(4):1322–32. doi: 10.1053/j.gastro.2008.07.012 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villanueva A, Chiang DY, Newell P, Peix J, Thung S, Alsinet C, et al. Pivotal role of mTOR signaling in hepatocellular carcinoma. Gastroenterology. 2008;135(6):1972–83, 83 e1–11. doi: 10.1053/j.gastro.2008.08.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ewald F, Norz D, Grottke A, Bach J, Herzberger C, Hofmann BT, et al. Vertical Targeting of AKT and mTOR as Well as Dual Targeting of AKT and MEK Signaling Is Synergistic in Hepatocellular Carcinoma. Journal of Cancer. 2015;6(12):1195–205. doi: 10.7150/jca.12452 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klein PJ, Schmidt CM, Wiesenauer CA, Choi JN, Gage EA, Yip-Schneider MT, et al. The effects of a novel MEK inhibitor PD184161 on MEK-ERK signaling and growth in human liver cancer. Neoplasia. 2006;8(1):1–8. doi: 10.1593/neo.05373 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson JM, Kunnimalaiyaan S, Gamblin TC, Kunnimalaiyaan M. MK2206 inhibits hepatocellular carcinoma cellular proliferation via induction of apoptosis and cell cycle arrest. The Journal of surgical research. 2014;191(2):280–5. doi: 10.1016/j.jss.2014.05.083 . [DOI] [PubMed] [Google Scholar]
- 26.Yu FX, Zhao B, Guan KL. Hippo Pathway in Organ Size Control, Tissue Homeostasis, and Cancer. Cell. 2015;163(4):811–28. doi: 10.1016/j.cell.2015.10.044 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patel SH, Camargo FD, Yimlamai D. Hippo Signaling in the Liver Regulates Organ Size, Cell Fate, and Carcinogenesis. Gastroenterology. 2017;152(3):533–45. doi: 10.1053/j.gastro.2016.10.047 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yimlamai D, Fowl BH, Camargo FD. Emerging evidence on the role of the Hippo/YAP pathway in liver physiology and cancer. J Hepatol. 2015;63(6):1491–501. doi: 10.1016/j.jhep.2015.07.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reis H, Bertram S, Pott L, Canbay A, Gallinat A, Baba HA. Markers of Hippo-Pathway Activity in Tumor Forming Liver Lesions. Pathol Oncol Res. 2017;23(1):33–9. doi: 10.1007/s12253-016-0079-0 . [DOI] [PubMed] [Google Scholar]
- 30.Sohn BH, Shim JJ, Kim SB, Jang KY, Kim SM, Kim JH, et al. Inactivation of Hippo Pathway Is Significantly Associated with Poor Prognosis in Hepatocellular Carcinoma. Clin Cancer Res. 2016;22(5):1256–64. doi: 10.1158/1078-0432.CCR-15-1447 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang C, Zhu ZM, Liu CL, He XJ, Zhang HY, Dong JH. Knockdown of yes-associated protein inhibits proliferation and downregulates large tumor suppressor 1 expression in MHCC97H human hepatocellular carcinoma cells. Mol Med Rep. 2015;11(6):4101–8. doi: 10.3892/mmr.2015.3257 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim MH, Kim J. Role of YAP/TAZ transcriptional regulators in resistance to anti-cancer therapies. Cell Mol Life Sci. 2017;74(8):1457–74. doi: 10.1007/s00018-016-2412-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dai XY, Zhuang LH, Wang DD, Zhou TY, Chang LL, Gai RH, et al. Nuclear translocation and activation of YAP by hypoxia contributes to the chemoresistance of SN38 in hepatocellular carcinoma cells. Oncotarget. 2016;7(6):6933–47. doi: 10.18632/oncotarget.6903 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huo X, Zhang Q, Liu AM, Tang C, Gong Y, Bian J, et al. Overexpression of Yes-associated protein confers doxorubicin resistance in hepatocellullar carcinoma. Oncol Rep. 2013;29(2):840–6. doi: 10.3892/or.2012.2176 . [DOI] [PubMed] [Google Scholar]
- 35.Fitamant J, Kottakis F, Benhamouche S, Tian HS, Chuvin N, Parachoniak CA, et al. YAP Inhibition Restores Hepatocyte Differentiation in Advanced HCC, Leading to Tumor Regression. Cell Rep. 2015. doi: 10.1016/j.celrep.2015.02.027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li X, Tao J, Cigliano A, Sini M, Calderaro J, Azoulay D, et al. Co-activation of PIK3CA and Yap promotes development of hepatocellular and cholangiocellular tumors in mouse and human liver. Oncotarget. 2015;6(12):10102–15. doi: 10.18632/oncotarget.3546 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zanconato F, Battilana G, Cordenonsi M, Piccolo S. YAP/TAZ as therapeutic targets in cancer. Curr Opin Pharmacol. 2016;29:26–33. doi: 10.1016/j.coph.2016.05.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu-Chittenden Y, Huang B, Shim JS, Chen Q, Lee SJ, Anders RA, et al. Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev. 2012;26(12):1300–5. doi: 10.1101/gad.192856.112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gibault F, Corvaisier M, Bailly F, Huet G, Melnyk P, Cotelle P. Non-Photoinduced Biological Properties of Verteporfin. Curr Med Chem. 2016;23(11):1171–84. . [DOI] [PubMed] [Google Scholar]
- 40.Yin H, Bogorad RL, Barnes C, Walsh S, Zhuang I, Nonaka H, et al. RNAi-nanoparticulate manipulation of gene expression as a new functional genomics tool in the liver. J Hepatol. 2016;64(4):899–907. doi: 10.1016/j.jhep.2015.11.028 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhan P, Song Y, Itoh Y, Suzuki T, Liu X. Recent advances in the structure-based rational design of TNKSIs. Mol Biosyst. 2014;10(11):2783–99. doi: 10.1039/c4mb00385c . [DOI] [PubMed] [Google Scholar]
- 42.Lehtio L, Chi NW, Krauss S. Tankyrases as drug targets. FEBS J. 2013;280(15):3576–93. doi: 10.1111/febs.12320 . [DOI] [PubMed] [Google Scholar]
- 43.Tiruveedi VL, Bale S, Khurana A, Godugu C. Tankyrase as a Novel Molecular Target in Cancer and Fibrotic Diseases. Current drug targets. 2016. doi: 10.2174/1389450117666160715152503 . [DOI] [PubMed] [Google Scholar]
- 44.Thorvaldsen TE. Targeting Tankyrase to Fight WNT-dependent Tumours. Basic & clinical pharmacology & toxicology. 2017;121(2):81–8. doi: 10.1111/bcpt.12786 . [DOI] [PubMed] [Google Scholar]
- 45.Tran FH, Zheng JJ. Modulating the wnt signaling pathway with small molecules. Protein Sci. 2017;26(4):650–61. doi: 10.1002/pro.3122 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lum L, Chen C. Chemical Disruption of Wnt-dependent Cell Fate Decision-making Mechanisms in Cancer and Regenerative Medicine. Curr Med Chem. 2015;22(35):4091–103. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tao J, Calvisi DF, Ranganathan S, Cigliano A, Zhou L, Singh S, et al. Activation of beta-catenin and Yap1 in human hepatoblastoma and induction of hepatocarcinogenesis in mice. Gastroenterology. 2014;147(3):690–701. doi: 10.1053/j.gastro.2014.05.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Laurent-Puig P, Legoix P, Bluteau O, Belghiti J, Franco D, Binot F, et al. Genetic alterations associated with hepatocellular carcinomas define distinct pathways of hepatocarcinogenesis. Gastroenterology. 2001;120(7):1763–73. . [DOI] [PubMed] [Google Scholar]
- 49.Weiler SM, Pinna F, Wolf T, Lutz T, Geldiyev A, Sticht C, et al. Induction of Chromosome Instability by Activation of Yes Associated Protein and Forkhead box M1 in Liver Cancer. Gastroenterology. 2017. doi: 10.1053/j.gastro.2017.02.018 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with XAV-939, U0126 or MK-2206, either alone or in combination for 72 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM XAV-939 alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. XAV-939+U0126. Experiments were repeated three times in triplicate.
(TIF)
Cell proliferation (A and B) and apoptosis (C and D) assays of HLE (A and C) and SNU-449 (B and D) cells treated with G007-LK, U0126 or MK-2206, either alone or in combination for 72 hours. Tukey-Kramer test: p<0.05 (a) vs. DMSO; (b) vs. 20μM G007-LK alone; (c) vs. 25μM U0126 alone; (d) vs. 5μM MK-2206 alone; (e) vs. G007-LK+U0126. Experiments were repeated three times in triplicate.
(TIF)
Western blot analysis of YAP, phosphorylated (p)-AKT and p-ERK levels in SNU-449 and HLE HCC cells upon treatment with XAV-939 and G007-LK, either alone or in combination with U0126 or MK-2206. Total (t-) AKT, ERK, and GAPDH were used as loading controls. Experiments were repeated twice.
(TIF)
(TIF)
(TIF)
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.