Abstract
Background
Health-related quality of life (HRQOL) is often prioritized over long-term survival in elderly patients. Although a longer dialysis session length (DSL) has been shown to reduce mortality, its effects on improving the HRQOL are unknown.
Methods
Using data from the Japan Dialysis Outcomes and Practice Patterns Study (J-DOPPS), patients aged ≥ 65 years on maintenance hemodialysis were enrolled. DSL was categorized as short (<210 minutes), medium (210–240 minutes), or long (>240 minutes). The primary outcomes were changes in mental health (ΔMH) and physical functioning (ΔPF) scores assessed using the Japanese version of SF-12, in one year. The differences in the ΔMH and ΔPF among the three groups were assessed via regression (beta) coefficients derived using a linear regression model.
Results
Of 1,187 patients at baseline, 319 (26.9%) had a short length, 686 (57.8%) a medium length, and 182 (15.3%) a long length. We assessed the ΔMH data from 793 patients and the ΔPF data from 738. No significant differences in the ΔMH were noted for the short or long groups compared with the medium group (score difference: 0.26, 95% confidence interval [CI]: -4.17 to 4.69 for short; score difference: -1.15, 95% CI: -6.17 to 3.86 for long). Similarly, no significant differences were noted for these groups versus the medium group in ΔPF either (score difference: -1.43, 95% CI: -6.73 to 3.87 for short; score difference: -1.71, 95% CI: -7.63 to 4.22 for long).
Conclusions
A shorter DSL might have no adverse effects on MH or PF for elderly patients.
Introduction
The mortality rates of hemodialysis (HD) patients continue to improve gradually, and Japanese HD patients in particular have the lowest mortality rates in the world [1]. With these improving mortality rates, the health-related quality of life (HRQOL) is gaining increasing importance as a relevant outcome [2]. However, the HRQOL in HD patients remains relatively low compared to that in the general population [3].
Among elderly HD patients, HRQOL is often prioritized over long-term survival. Although many previous reports have indicated that a longer dialysis session length is associated with a reduced mortality [4–9], dialysis session length in daily clinical practice is shortened in elderly patients for any of several reasons, such as reducing the physical burden. Indeed, the mean dialysis session length is shorter in elderly patients than in overall HD patients in Japan (231 minutes in elderly patients vs. 241 minutes in total HD patients; data provided by the Japanese Society for Dialysis Therapy) as well as in other countries [10, 11]. Therefore, the dialysis session length in elderly patients may be shortened not with respect to mortality but based on other determinants, such as HRQOL, provided the dialysis efficiency was sufficient.
Previous studies have reported that dialysis session length and treatment interval were associated with mental health (MH) and physical functioning (PF), but these findings are controversial [12–17]. Considering these results, the dialysis session length may ameliorate MH and PF through the improvement of dialysis efficiency, whereas the long restriction required for longer-duration treatment may deteriorate MH and PF in conventional HD patients. Therefore, the association of the MH and PF with dialysis session length in elderly patients needs to be examined.
Here, we evaluated the influence of the dialysis session length on the MH and PF in elderly HD patients as indicators of HRQOL. We hope these findings will guide clinicians on the optimum dialysis session length based not only on mortality but also HRQOL.
Materials and methods
Design, setting, and participants
We enrolled hemodialysis patients who participated in the third (2005–2008) and fourth (2009–2011) phase of the Japan Dialysis Outcomes and Practice Patterns Study (J-DOPPS). The design of the DOPPS is detailed in a previous report [18].
A total of 121 facilities were included in J-DOPPS phases 3 to 4. For this study, eligible participants were patients aged 65 years or older on maintenance HD for at least 120 days. We excluded participants with missing data on dialysis session length, MH and PF subdomain scores in the Japanese version of the SF-12, and vintage. J-DOPPS data, which included laboratory data, drug information, and dialysis conditions, were collected every four months. Our present study using these J-DOPPS data complied with the Declaration of Helsinki. All participants in J-DOPPS have provided written informed consent before study enrollment. Data collection was performed in a fashion that maintains patient anonymous at the cording center. This study’s conduct was approved by the Ethics Committee of Tokyo Women's Medical University (Approval Numbers 709, 1178, 1278, 1527, 1826, and 2143).
Main exposure
The main exposure was dialysis session length at baseline, categorized into three groups: (1) short length (≤ 210 minutes per session), (2) medium length as reference (210–240 minutes per session), and (3) long length (>240 minutes per session). In Japan, over half HD patients is prescribed 240 minutes dialysis session length and dialysis session length for the great majority of patients is at exactly 30 min intervals [11, 19, 20]. Therefore, we set the medium length group under the assumption of 240 minutes group as reference.
Main outcome
The primary outcomes were changes in mental health (ΔMH) and physical functioning (ΔPF), as assessed using the Japanese version of the SF-12 [21], at one year after study initiation.
The subdomain of MH was composed of the following questions:
Have you felt calm and peaceful?
Have you felt downhearted and blue?
The subdomain of PF was composed of the following questions:
Does your health now limit you in these activities? If so, how much?
Moderate activities, such as moving a table, pushing a vacuum cleaner, bowling, or playing golf
Climbing several flights of stairs
The scores of each subdomain were totaled and transformed to a scale of 0–100 points, with higher scores representing better health states.
Statistical analyses
Baseline characteristics of participants were categorized by dialysis session length and described respectively. Characteristics of continuous data with normal distribution were summarized as means (±standard deviation [SD]), continuous variables with skewed data as medians (inter-quartile range [IQR]), and dichotomous or categorical data as proportions.
We compared the unadjusted and multivariable-adjusted score differences to evaluate the association between each duration on HD and ΔMH or ΔPF at one year after study initiation.
The model was adjusted for potential confounders at baseline, including age, gender, smoking habit, dialysis vintage, calcium level, albumin level (Alb), ultrafiltration rates (UFR), presence of comorbidities (diabetes, cardiovascular disease, congestive heart failure, dysrhythmia, other cardiac diseases, cerebrovascular disease, peripheral vascular disease, gastrointestinal bleeding, liver disease, cancer, chronic obstructive pulmonary disease, and chronic hepatitis), soporific or antidepressant drugs (benzodiazepines, selective serotonin reuptake inhibitors, serotonin antagonist and reuptake inhibitors, selective melatonin receptors, noradrenergic and specific serotonergic antidepressant, tetracyclic antidepressants) and erythropoietin resistance index (ERI). The severity of comorbidities were presented as their Charlson Index, ranging from 0 to 21 [22]. The ERI was evaluated by dividing the average weekly erythropoiesis-stimulating agent dose by body weight (kg) per average hemoglobin value (g per dL). A diagnosis of depression was defined as Center for Epidemiologic Studies Depression Scale (CES-D) < 10%. Linear mixed effect models were developed to assess the score differences in ΔMH and ΔPF, taking into account cluster effects at the facility level.
Additionally, we performed multiple imputation using predictive mean matching (pmm) for complementation of missing covariates. The missing data were imputed 10 times to obtain 10 complete datasets. We then used Rubin’s rule with summary estimates to combine the results from multiple imputed datasets.
Further, as a sensitivity analysis, we assessed the influence of missing data for MH or PF in one year. We also performed multiple imputation using pmm with 10 repetitions for complementation of missing outcomes for participants censored for reasons other than death.
All statistical analyses were performed using STATA 14.0 (version 14.0; StataCorp, College Station, TX, USA), with 2-sided significance set at 0.05.
Results
Study flow diagram
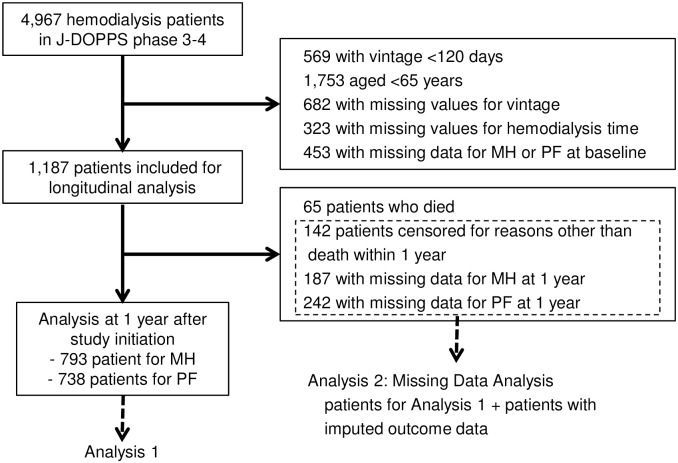
In accordance with pre-defined criteria, 1,187 patients were included in this study. After several dropouts, for reasons such as death, censoring other than death, and missing values of MH and PF at 1 year, 793 and 738 patients remained in the analysis of the score difference of MH and of PF at 1 year, respectively (Fig 1).
Fig 1. Participant flow diagram and the study selection process.
Baseline characteristics of study participants
Dialysis session length showed a normal distribution, and the overall mean was 231.1 (29.4) minutes per session at baseline. With regard to each category, 319 (27.6%) subjects were categorized as short session length, 686 (57.8%) as medium, and 182 (15.3%) as long.
Table 1 shows the baseline characteristics of patients, categorized by time on HD per day. Mean age was 73.2 years (range 65 to 94 years), 62.9% of subjects were male, the median dialysis vintage was 6.6 years, and the mean Charlson Index was 4.1. Patients with longer time were more likely to be male and have a smoking habit, longer vintage, and lower ERI. Patients with shorter times were more likely to have lower MH and PF than those with a medium session length.
Table 1. Baseline characteristics of patients, categorized by dialysis session length.
| Characteristics | Total (n = 1,187) | Time≤210 (n = 319) | 210<Time≤ 240 (n = 686) | 240<Time (n = 182) |
|---|---|---|---|---|
| Age, years | 73.2 (6.3) | 74.7 (6.9) | 72.6 (6.0) | 72.4 (5.9) |
| Male, % | 62.9 | 58.2 | 62.8 | 71.4 |
| Time on hemodialysis, minutes | 231.1 (29.4) | 191.1 (16.1) | 239.7 (2.4) | 268.8 (25.6) |
| Dialysis time per week, times | 3.0 (0.20) | 2.9 (0.33) | 3.0 (0.11) | 3.0 (0.13) |
| Smoker (ever), % | 36.9 | 34.9 | 34.3 | 48.3 |
| Vintage, years | 6.6 (6.5) | 3.2 (3.4) | 7.8 (6.8) | 8.3 (7.3) |
| Charlson Index | 4.1 (3.5) | 4.0 (3.4) | 4.3 (3.6) | 3.9 (3.4) |
| CES-D < 10, % | 50.3 | 45.1 | 53.8 | 45.5 |
| Hemoglobin, g/dL | 10.3 (1.2) | 10.2 (1.2) | 10.3 (1.2) | 10.6 (1.2) |
| Calcium, mg/dL | 9.2 (0.79) | 9.1 (0.81) | 9.2 (0.77) | 9.4 (0.78) |
| Albumin, g/dL | 3.7 (0.37) | 3.7 (0.44) | 3.7 (0.35) | 3.7 (0.35) |
| Ultrafiltration Rates, ml/mmHg/h | 9.9 (5.5) | 10.5 (5.4) | 9.6 (5.4) | 10.3 (6.1) |
| ERI, U/week/kg/g/dL | 8.6 (7.7) | 9.0 (6.8) | 8.8 (8.2) | 7.5 (7.1) |
| Soporific, N (%) | 29.2 | 28.2 | 29.3 | 30.8 |
| Anti-depression medicine, N (%) | 3.4 | 2.2 | 4.2 | 2.2 |
| Mental health | 64.0 (23.9) | 61.1 (25.2) | 65.5 (23.2) | 63.1 (24.0) |
| Physical functioning | 50.1 (34.4) | 45.1 (33.5) | 52.1 (34.2) | 51.6 (35.9) |
Continuous data with a normal distribution are summarized as the mean (standard deviation), continuous variables with skewed data are summarized as the median (interquartile range), and dichotomous or categorical data are summarized as proportions.
Changes in MH
At 1 year after study initiation, the ΔMH of the 793 subjects (Fig 1, Analysis 1) was -1.42 (24.6). By category, the ΔMH in the short session length group was -0.35 (23.8), that in the medium session length group was -1.5 (25.4), and that in the long session length group was -2.5 (22.3).
As shown in Table 2, a short session length had no significant influence on the ΔMH versus a medium length as a reference during the 1-year observational period (score difference: 0.26, 95% confidence interval [CI]: -4.17 to 4.69, and p value: 0.91), nor did a long session length (score difference: -1.15, 95% CI: -6.17 to 3.86, and p value: 0.65).
Table 2. Association between dialysis session length and change in mental health or physical functioning at one year after study initiation.
| Unadjusted β | Adjusted β | |
|---|---|---|
| Mental Health | ||
| Time≤210 | 1.21 (-3.04 to 5.47) | 0.26 (-4.17 to 4.69) |
| 210<Time≤ 240 | Reference | Reference |
| 240<Time | -0.97 (-5.95 to 4.02) | -1.15 (-6.17 to 3.86) |
| Physical Functioning | ||
| Time≤210 | -2.37 (- 7.41 to 2.68) | -1.43 (-6.73 to 3.87) |
| 210<Time≤240 | Reference | Reference |
| 240<Time | -1.32 (-7.19 to 4.55) | -1.71 (-7.63 to 4.22) |
Results shown are coefficients (95% confidence intervals).
Adjusted for age, gender, HD duration, smoking, Ca, Alb, UFR, Charlson index, ERI, and medication (soporific, antidepressant). Additionally, dialysis session length was not associated with ΔMH among all-aged participants of this study (S1 Table).
Changes in PF
At 1 year after study initiation, the ΔPF of the 738 patients (Fig 1, Analysis 1) was -1.9 (28.1). By category, the ΔPF in the short session length group was -3.6 (28.3), that in the medium session length group was -1.1 (28.2), and that in the long session length group was -2.7 (27.7).
As found for MH, in Table 2, a short session length had no significant influence on the ΔPF versus a medium length as a reference during the 1-year observational period (score difference: -1.43, 95% CI: -6.73 to 3.87, and p value: 0.60), nor did a long session length (score difference: -1.71, 95% CI: -7.63 to 4.22, and p value: 0.57). Additionally, dialysis session length was not associated with ΔPF among all-aged participants of this study (S1 Table).
Sensitivity analysis of missing data
Of the 1,187 patients at baseline, about 40% dropped out within 1 year from study initiation. Sixty-five patients were censored due to death (20 patients with short session length [6.3% of the short session length group], 33 patients with medium session length [4.8% of the group], and 12 patients with long session length [6.6% of the group]), 142 were censored for reasons other than death, and 277 had missing values for MH or PF at 1 year (187 patients with missing data for MH and 242 patients with missing data for PF). We performed multiple imputation using pmm for 1,122 participants with missing values of MH or PF due to reasons other than death (Fig 1, Analysis 2). The findings were consistent with the original results, and we confirmed that the missing data didn’t affect the overall study results.
Discussion
This is the first report to investigate the relationships between the dialysis session length and MH and PF as indicators of HRQOL, which is a particularly relevant outcome for elderly patients. Dialysis session length was not significantly associated with MH or PF in the present study. We used a subdomain of the SF-12 to measure MH and PF. The SF-12 is constructed from the SF-36 and vigorously and concisely predicts the SF-36 Physical and Mental Component Summary scores [23–26]. Further, ΔMH and ΔPF have been evaluated as predictors of mortality in previous studies [26, 27].
In this study, aged HD patients with short dialysis sessions were more likely to be female and have a higher ERI. A previous study similarly reported that a shorter dialysis session was associated with older age and a higher prevalence of female patients [10, 11]. Given that other studies have reported an association between a shorter dialysis session and a higher ultrafiltration rate, a short dialysis session may be sufficient in elderly female patients because of their overall smaller stature than male patients [11]. However, ERI, which is associated with mortality, is known to be improved by increased intensity of dialysis including a longer dialysis session [28]. Taken together, these present and previous findings indicate that patients unlikely to survive long-term might receive a shorter dialysis session.
No session length-dependent factors influencing the ΔMH in aged HD patients were noted in the present study. Although only one cross sectional study reported no association between dialysis session length and MH in conventional HD patients [29], the ΔMH versus the dialysis session length has never before been evaluated. While previous reports have shown that daily short-session dialysis tended to improve the MH [12, 13], the effects of daily long-session dialysis are controversial [30]. In the present study, dialysis session length did not influence the ΔMH in elderly conventional HD patients. Therefore, in terms of MH, a short session length might be the better option in elderly patients, as these patients are more likely to have back pain and experience a burden due to inactivity than younger patients.
We also noted no association between dialysis session length and ΔPF. The above-referenced cross-sectional study reported an association between short dialysis session length and better PF in conventional HD patients [29]. However, a randomized controlled trial revealed that daily short-session dialysis did not improve the objective PF but did improve the subjective PF, while daily long-session dialysis did not improve either the objective or subjective PF [17]. As with MH, a short dialysis session length may not adversely affect the PF in elderly HD patients. Additionally, dialysis session length were not associated with both ΔMH and ΔPF among all-aged participants of this study (S1 Table). Further, we considered the influence of missing values of both ΔMH and ΔPF through sensitivity analyses. Although the point estimates of the coefficients were slightly deviated, we concluded that the differences in the ΔMH and ΔPF among the HD session length groups did not meet the minimum clinically important difference in comparison with the original results [31–33] (Table 3), and the findings were essentially the same as those obtained in the primary analyses.
Table 3. Multiple imputation using predictive mean matching (pmm) for censoring during study follow-up.
| Unadjusted β | Adjusted β | |
|---|---|---|
| Mental Health | ||
| Time≤210 | 1.75 (-2.28 to 5.78) | 0.96 (-3.15 to 5.08) |
| 210<Time≤ 240 | Reference | Reference |
| 240<Time | -0.52 (-5.48 to 4.44) | -0.67 (-5.67 to 4.34) |
| Physical Functioning | ||
| Time≤210 | -1.04 (-5.72 to 3.63) | -0.14 (-5.16 to 4.88) |
| 210<Time≤240 | Reference | Reference |
| 240<Time | -0.71 (-6.47 to 5.05) | -0.51 (-6.23 to 5.20) |
Results shown are coefficients (95% confidence intervals).
Adjusted for age, gender, HD duration, smoking, Ca, Alb, UFR, Charlson index, ERI, and medication (soporific, antidepressant).
Several limitations to the present study warrant mention. First, we conducted our evaluation using the dialysis session length at baseline. Dialysis session length can often fluctuate, but we did not evaluate the influence of such fluctuation during the observational period. Second, the model in this study wasn’t adjusted for unmeasured confounding factors, such as treatment principles depended on physicians, residual renal function, residual urine output, or urea clearance, because of the observational nature of the study. These limitations may have obscured the influence of dialysis session length on MH and PF. Third, our study excluded patients who could not respond to the questionnaire for MH or PF due to physical or intellectual disability. Baseline characteristics among participants with missing values of MH or PF were similar to the total means of those without missing outcomes (S1 Table), but any interpretation of the findings should be conducted with caution. Fourth, the SF-12 was validated using Japanese representative samples, and also validated internationally in dialysis patients [24, 34]. We can calculate norm-based scores based on the study. Actually, there are many reports using the SF-12 in Japanese patients with other various diseases [35–39]. In the recent report using DOPPS data, the SF-12 is used for measurement of health-related quality of life including Japanese HD patients [40].
In conclusion, the present results suggest that a shorter dialysis session length had no adverse effects on MH or PF in elderly patients.
Supporting information
Results shown are coefficients (95% confidence intervals). Adjusted for age, gender, HD duration, smoking, Ca, Alb, UFR, Charlson index, ERI, and medication (soporific, antidepressant). Of 2,610 all aged participants, 1,882 patients had the results of ΔMH and 1,725 patients had the results of ΔPF.
(DOCX)
Acknowledgments
The JDOPPS is Japanese part of The DOPPS. The DOPPS is administered by the Arbor Research Collaborative for Health and is supported by scientific research grants from Amgen (since 1996), Kyowa Hakko Kirin (since 1999, in Japan), Sanofi/Genzyme (since 2009), Abbott (since 2009), Baxter (since 2011), and Vifor Fresenius Renal Pharma (since 2011), without restrictions on publications. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The present study is supported by scientific research grants from Kyowa Hakko Kirin without restrictions.
Data Availability
Data requests can be sent to Arbor Research via their website (http://www.arborresearch.org/AboutUs/ContactUs.aspx). If the requests are accepted, the data can be made available to other researchers.
Funding Statement
The JDOPPS is Japanese part of The DOPPS. The DOPPS is administered by the Arbor Research Collaborative for Health and is supported by scientific research grants from Amgen (since 1996), Kyowa Hakko Kirin (since 1999, in Japan), Sanofi/Genzyme (since 2009), Abbott (since 2009), Baxter (since 2011), and Vifor Fresenius Renal Pharma (since 2011), without restrictions on publications. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The present study is supported by scientific research grants from Kyowa Hakko Kirin without restrictions.
References
- 1.Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T, Andreucci VE, et al. Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan, and the United States: the Dialysis Outcomes and Practice Patterns Study (DOPPS). J Am Soc Nephrol. 2003;14(12):3270–7. Epub 2003/11/26. . [DOI] [PubMed] [Google Scholar]
- 2.Davison SN, Levin A, Moss AH, Jha V, Brown EA, Brennan F, et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney Int. 2015;88(3):447–59. Epub 2015/04/30. doi: 10.1038/ki.2015.110 . [DOI] [PubMed] [Google Scholar]
- 3.Fukuhara S, Lopes AA, Bragg-Gresham JL, Kurokawa K, Mapes DL, Akizawa T, et al. Health-related quality of life among dialysis patients on three continents: the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2003;64(5):1903–10. Epub 2003/10/09. doi: 10.1046/j.1523-1755.2003.00289.x . [DOI] [PubMed] [Google Scholar]
- 4.Shinzato T, Nakai S, Akiba T, Yamazaki C, Sasaki R, Kitaoka T, et al. Survival in long-term haemodialysis patients: results from the annual survey of the Japanese Society for Dialysis Therapy. Nephrol Dial Transplant. 1997;12(5):884–8. Epub 1997/05/01. . [DOI] [PubMed] [Google Scholar]
- 5.Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, et al. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the DOPPS. Kidney Int. 2006;69(7):1222–8. Epub 2006/04/13. doi: 10.1038/sj.ki.5000186 . [DOI] [PubMed] [Google Scholar]
- 6.Tentori F, Zhang J, Li Y, Karaboyas A, Kerr P, Saran R, et al. Longer dialysis session length is associated with better intermediate outcomes and survival among patients on in-center three times per week hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2012;27(11):4180–8. Epub 2012/03/21. doi: 10.1093/ndt/gfs021 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Held PJ, Levin NW, Bovbjerg RR, Pauly MV, Diamond LH. Mortality and duration of hemodialysis treatment. Jama. 1991;265(7):871–5. Epub 1991/02/20. . [PubMed] [Google Scholar]
- 8.Marshall MR, Song Q, Ma TM, MacDonell SG, Kasabov NK. Evolving connectionist system versus algebraic formulas for prediction of renal function from serum creatinine. Kidney Int. 2005;67(5):1944–54. Epub 2005/04/21. doi: 10.1111/j.1523-1755.2005.00293.x . [DOI] [PubMed] [Google Scholar]
- 9.Brunelli SM, Chertow GM, Ankers ED, Lowrie EG, Thadhani R. Shorter dialysis times are associated with higher mortality among incident hemodialysis patients. Kidney Int. 2010;77(7):630–6. Epub 2010/01/22. doi: 10.1038/ki.2009.523 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flythe JE, Curhan GC, Brunelli SM. Shorter length dialysis sessions are associated with increased mortality, independent of body weight. Kidney Int. 2013;83(1):104–13. doi: 10.1038/ki.2012.346 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tentori F, Zhang J, Li Y, Karaboyas A, Kerr P, Saran R, et al. Longer dialysis session length is associated with better intermediate outcomes and survival among patients on in-center three times per week hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2012;27(11):4180–8. doi: 10.1093/ndt/gfs021 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Unruh ML, Larive B, Chertow GM, Eggers PW, Garg AX, Gassman J, et al. Effects of 6-times-weekly versus 3-times-weekly hemodialysis on depressive symptoms and self-reported mental health: Frequent Hemodialysis Network (FHN) Trials. Am J Kidney Dis. 2013;61(5):748–58. doi: 10.1053/j.ajkd.2012.11.047 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaber BL, Lee Y, Collins AJ, Hull AR, Kraus MA, McCarthy J, et al. Effect of daily hemodialysis on depressive symptoms and postdialysis recovery time: interim report from the FREEDOM (Following Rehabilitation, Economics and Everyday-Dialysis Outcome Measurements) Study. Am J Kidney Dis. 2010;56(3):531–9. doi: 10.1053/j.ajkd.2010.04.019 . [DOI] [PubMed] [Google Scholar]
- 14.McPhatter LL, Lockridge RS Jr., Albert J, Anderson H, Craft V, Jennings FM, et al. Nightly home hemodialysis: improvement in nutrition and quality of life. Adv Ren Replace Ther. 1999;6(4):358–65. . [DOI] [PubMed] [Google Scholar]
- 15.Heidenheim AP, Muirhead N, Moist L, Lindsay RM. Patient quality of life on quotidian hemodialysis. American Journal of Kidney Diseases. 2003;42(1):S36–S41. doi: 10.1016/S0272-6386(03)00536-5 WOS:000184034300008. [DOI] [PubMed] [Google Scholar]
- 16.Manns BJ, Walsh MW, Culleton BF, Hemmelgarn B, Tonelli M, Schorr M, et al. Nocturnal hemodialysis does not improve overall measures of quality of life compared to conventional hemodialysis. Kidney Int. 2009;75(5):542–9. doi: 10.1038/ki.2008.639 . [DOI] [PubMed] [Google Scholar]
- 17.Hall YN, Larive B, Painter P, Kaysen GA, Lindsay RM, Nissenson AR, et al. Effects of six versus three times per week hemodialysis on physical performance, health, and functioning: Frequent Hemodialysis Network (FHN) randomized trials. Clin J Am Soc Nephrol. 2012;7(5):782–94. doi: 10.2215/CJN.10601011 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pisoni RL, Gillespie BW, Dickinson DM, Chen K, Kutner MH, Wolfe RA. The Dialysis Outcomes and Practice Patterns Study (DOPPS): design, data elements, and methodology. Am J Kidney Dis. 2004;44(5 Suppl 2):7–15. . [DOI] [PubMed] [Google Scholar]
- 19.Brunelli SM, Chertow GM, Ankers ED, Lowrie EG, Thadhani R. Shorter dialysis times are associated with higher mortality among incident hemodialysis patients. Kidney Int. 2010;77(7):630–6. doi: 10.1038/ki.2009.523 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, et al. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the DOPPS. Kidney Int. 2006;69(7):1222–8. doi: 10.1038/sj.ki.5000186 . [DOI] [PubMed] [Google Scholar]
- 21.Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3(5):329–38. . [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010;77(2):141–51. doi: 10.1038/ki.2009.413 . [DOI] [PubMed] [Google Scholar]
- 23.Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34(3):220–33. . [DOI] [PubMed] [Google Scholar]
- 24.Osthus TB, Preljevic VT, Sandvik L, Leivestad T, Nordhus IH, Dammen T, et al. Mortality and health-related quality of life in prevalent dialysis patients: Comparison between 12-items and 36-items short-form health survey. Health Qual Life Outcomes. 2012;10:46 doi: 10.1186/1477-7525-10-46 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lacson E Jr., Xu J, Lin SF, Dean SG, Lazarus JM, Hakim RM. A comparison of SF-36 and SF-12 composite scores and subsequent hospitalization and mortality risks in long-term dialysis patients. Clin J Am Soc Nephrol. 2010;5(2):252–60. doi: 10.2215/CJN.07231009 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loosman WL, Hoekstra T, van Dijk S, Terwee CB, Honig A, Siegert CE, et al. Short-Form 12 or Short-Form 36 to measure quality-of-life changes in dialysis patients? Nephrol Dial Transplant. 2015;30(7):1170–6. doi: 10.1093/ndt/gfv066 . [DOI] [PubMed] [Google Scholar]
- 27.Perl J, Karaboyas A, Morgenstern H, Sen A, Rayner HC, Vanholder RC, et al. Association between changes in quality of life and mortality in hemodialysis patients: results from the DOPPS. Nephrol Dial Transplant. 2016. doi: 10.1093/ndt/gfw233 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ifudu O, Feldman J, Friedman EA. The intensity of hemodialysis and the response to erythropoietin in patients with end-stage renal disease. N Engl J Med. 1996;334(7):420–5. doi: 10.1056/NEJM199602153340702 . [DOI] [PubMed] [Google Scholar]
- 29.Bohlke M, Nunes DL, Marini SS, Kitamura C, Andrade M, Von-Gysel MP. Predictors of quality of life among patients on dialysis in southern Brazil. Sao Paulo Med J. 2008;126(5):252–6. Epub 2008/12/23. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walsh M, Culleton B, Tonelli M, Manns B. A systematic review of the effect of nocturnal hemodialysis on blood pressure, left ventricular hypertrophy, anemia, mineral metabolism, and health-related quality of life. Kidney Int. 2005;67(4):1500–8. Epub 2005/03/23. doi: 10.1111/j.1523-1755.2005.00228.x . [DOI] [PubMed] [Google Scholar]
- 31.Vilagut G, Forero CG, Pinto-Meza A, Haro JM, de Graaf R, Bruffaerts R, et al. The mental component of the short-form 12 health survey (SF-12) as a measure of depressive disorders in the general population: results with three alternative scoring methods. Value Health. 2013;16(4):564–73. doi: 10.1016/j.jval.2013.01.006 . [DOI] [PubMed] [Google Scholar]
- 32.Parker SL, Mendenhall SK, Shau D, Adogwa O, Cheng JS, Anderson WN, et al. Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. J Neurosurg Spine. 2012;16(1):61–7. doi: 10.3171/2011.8.SPINE1194 . [DOI] [PubMed] [Google Scholar]
- 33.Singh J, Sloan JA, Johanson NA. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18(2):72–82. ; [PMC free article] [PubMed] [Google Scholar]
- 34.Fukuhara S, Suzukamo Y. Manual of the SF-36v2 Japanese version.: Institute for Health Outcomes & Process Evaluation Research, Kyoto: 2004. [Google Scholar]
- 35.Inoue M, Shiozawa K, Yoshihara R, Yamane T, Shima Y, Hirano T, et al. Predictors of poor sleep quality in patients with systemic lupus erythematosus. Clin Rheumatol. 2017;36(5):1053–62. doi: 10.1007/s10067-017-3545-5 . [DOI] [PubMed] [Google Scholar]
- 36.Yoshida M, Igawa Y, Higashimura S, Suzuki M, Niimi A, Sanada H. Translation and reliability and validity testing of a Japanese version of the Intermittent Self-Catheterization Questionnaire among disposable and reusable catheter users. Neurourol Urodyn. 2016. doi: 10.1002/nau.23111 . [DOI] [PubMed] [Google Scholar]
- 37.Hamuro A, Tachibana D, Wang H, Hayashi M, Yanai S, Kurihara Y, et al. Combined reconstructive surgery involving uterosacral colpopexy and anterior vaginal mesh implantation for pelvic organ prolapse. J Obstet Gynaecol Res. 2016;42(6):707–15. doi: 10.1111/jog.12952 . [DOI] [PubMed] [Google Scholar]
- 38.Honda M, Wakita T, Onishi Y, Nunobe S, Miura A, Nishigori T, et al. Development and Validation of a Disease-Specific Instrument to Measure Diet-Targeted Quality of Life for Postoperative Patients with Esophagogastric Cancer. Ann Surg Oncol. 2015;22 Suppl 3:S848–54. doi: 10.1245/s10434-015-4696-8 . [DOI] [PubMed] [Google Scholar]
- 39.Kato S, Oshima Y, Oka H, Chikuda H, Takeshita Y, Miyoshi K, et al. Comparison of the Japanese Orthopaedic Association (JOA) score and modified JOA (mJOA) score for the assessment of cervical myelopathy: a multicenter observational study. PLoS One. 2015;10(4):e0123022 doi: 10.1371/journal.pone.0123022 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perl J, Karaboyas A, Morgenstern H, Sen A, Rayner HC, Vanholder RC, et al. Association between changes in quality of life and mortality in hemodialysis patients: results from the DOPPS. Nephrol Dial Transplant. 2017;32(3):521–7. doi: 10.1093/ndt/gfw233 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Results shown are coefficients (95% confidence intervals). Adjusted for age, gender, HD duration, smoking, Ca, Alb, UFR, Charlson index, ERI, and medication (soporific, antidepressant). Of 2,610 all aged participants, 1,882 patients had the results of ΔMH and 1,725 patients had the results of ΔPF.
(DOCX)
Data Availability Statement
Data requests can be sent to Arbor Research via their website (http://www.arborresearch.org/AboutUs/ContactUs.aspx). If the requests are accepted, the data can be made available to other researchers.