Abstract
Chronic pain among older adults is common and often disabling. Pain-related formal social support (e.g., provided by staff at day-care centers, nursing homes), and the extent to which it promotes functional autonomy or dependence, plays a significant role in the promotion of older adults’ ability to engage in their daily activities. Assessing older adults’ preferences for pain-related social support for functional autonomy or dependence could contribute to increase formal social support responsiveness to individuals’ needs. Therefore, this study aimed at developing and validating the preferences for formal social support of autonomy and dependence in pain inventory (PFSSADI). One hundred and sixty-five older adults with chronic musculoskeletal pain (M age = 79.1, 67.3% women), attending day-care centers, completed the PFSSADI, the revised formal social support for autonomy and dependence in pain inventory, and a measure of desire for (in)dependence; the PFSSADI was filled out again 6 weeks later. Confirmatory factor analyses showed a structure of two correlated factors (r = .56): (a) preferences for autonomy support (α = .99) and (b) preferences for dependence support (α = .98). The scale showed good test–retest reliability, sensitivity and discriminant and concurrent validity; the higher the preferences for dependence support, the higher the desire for dependence (r = .33) and the lower the desire for independence (r = −.41). The PFSSADI is an innovative tool, which may contribute to explore the role of pain-related social support responsiveness on the promotion of older adults’ functional autonomy when in pain.
Keywords: Pain, Social support preferences, Functional autonomy/dependence, Older adults, Scale development and validation
Introduction
In 2050, individuals aged over 60 (i.e., older adults) will represent a third of the population living in developed countries (United Nations 2013). Considering current epidemiological data on pain and aging, over half of older adults will likely suffer from chronic (musculoskeletal) pain (Gibson 2007; Helme and Gibson 2001; Molton and Terrill 2014; Yamada and Thomas 2011), i.e., pain that persists beyond a “conventional” tissue healing time—3 months (Merskey and Bogduk 1994). Chronic pain is often highly disabling (Reyes-Gibby et al. 2002; Ferrel 1995; Helme and Gibson 1997) and one of the main obstacles to older adults’ ability to perform physical, cognitive and social activities independently—functional autonomy (Hébert et al. 2001; Stubbs et al. 2013)—and to an healthy aging process (Wilkie et al. 2013). In other words, population aging will most likely result in an increased prevalence of disabling chronic pain at the population level. Considering the huge social and economic burden of chronic pain in our current societies (e.g., Thomsen et al. 2002; Turk 2002), any efforts to understand and reduce the impact of pain on older adults’ aging processes are of paramount importance.
But how can we reduce pain-related disability, i.e., the extent to which chronic pain interferes in older adults’ daily lives? The negative relationship between physical and social activity engagement and chronic pain disability is central to current theoretical models and is widely empirically supported (e.g., Leeuw et al. 2007; Vlaeyen and Linton 2012). Although a great deal of research has been focusing on the cognitive and affective determinants of activity dis-/engagement and pain disability (e.g., catastrophizing, kinesiophobia, hypervigilance), there is also accumulating evidence supporting the role of social relations on chronic pain outcomes (e.g., Krahé et al. 2013; Leonard et al. 2006; Hadjistavropoulos et al. 2011).
Social support is one particular dimension of social relations that has been investigated in pain contexts. It refers to the support people report having received or that is available to them if needed within the context of informal (e.g., family, friends) or formal relationships (e.g., healthcare services/professionals; Cohen et al. 2000). Findings highlight the importance of social support in the experience of pain and pain-related outcomes such as disability (e.g., Campbell et al. 2011, 2013; Leonard et al. 2006; Newton-John 2002). Most of this literature, however, has been focusing on the role of informal social support (from spouses or co-workers) on middle-aged adults’ pain experiences. Considering that many older adults in western societies often live alone and/or need the support from institutions, such as day-care centers, nursing homes or home care services (European Union 2012; Harris-Kojetin et al. 2013; Phillip 2014), the role played by formal social support in reducing older adults’ pain-related disability and promoting their functional autonomy is an important gap in the present literature. This paper contributes to bridging this gap by aiming to develop and validate a measure of older adults’ preferences for pain-related formal social support for functional autonomy and dependence.
Formal social support for functional autonomy and dependence in pain
Pain-related formal social support, and the extent to which it promotes individuals’ functional autonomy and/or dependence, may play a significant role in the promotion of older adults’ ability to engage in their daily activities despite pain. Recent studies using a newly developed, reliable and valid measure—the (revised) formal social support for autonomy and dependence in pain inventory (FSSADI_PAIN)—have supported this contention (Matos and Bernardes 2013; Matos et al. 2015, 2016). This instrument measures older adults’ reports of how often employees at their institution (e.g., day-care center, nursing home) provided them support when they were in pain. Confirmatory factor analyses have shown that the revised FSSADI_PAIN assesses two functions of pain-related formal social support: (1) Perceived Promotion of Autonomy (4 items), i.e., the perceived frequency of employees’ instrumental and emotional/esteem support actions that reinforce older adults’ higher self-efficacy, motivation and/or ability to engage in life activities despite pain and (2) Perceived Promotion of Dependence (4 items), i.e., the perceived frequency of employees’ instrumental and emotional/esteem support actions that reinforce older adults’ lower self-efficacy and activity disengagement when in pain. Findings have shown that older adults’ higher perceived promotion of dependence is associated with higher pain disability; conversely, higher perceived promotion of autonomy is associated with lower pain disability (Matos and Bernardes 2013; Matos et al. 2015). Moreover, these relationships are partially mediated by older adults’ self-reported physical functioning (Matos et al. 2016). Taken together, these findings highlight: (1) the importance of distinguishing perceived promotion of dependence and of autonomy as two functions of formal social support that may play different roles in the promotion of older adults’ functional autonomy when in pain and (2) the theoretical and practical relevance of the FSSADI_PAIN, by assessing older adults’ perceptions of the frequency with which they are getting each kind of social support.
However, more than assessing the amount of formal social support older adults report receiving (as measured by the FSSADI_PAIN), it is paramount knowing if what they are getting is satisfying their wants and needs. Indeed, research has shown that received social support that is not responsive to individuals’ basic and circumstantial needs is often associated with poorer health-related outcomes (Ibarra-Rovillard and Kuiper 2011; Maisel and Gable 2009; Selcuk and Ong 2013). Being able to assess whether older adults prefer receiving social support for functional autonomy or dependence when in pain would contribute to increase formal social support responsiveness. However, to the best of our knowledge, there is currently no instrument to assess older adults’ preferences for formal pain-related social support or, more specifically, their preferences for social support for functional autonomy and dependence. Therefore, in order to bridge this gap, this study specifically aimed at the development and validation of the preferences for formal social support for autonomy and dependence in pain inventory (PFSSADI).
The development and validation plan of the PFSSADI
In order to develop the items of the PFSSADI, we adapted the eight original items of the revised FSSADI_PAIN (Matos et al. 2015), by changing the general instructions, the initial wording of the items and their rating scale. More specifically, instead of asking older adults to assess the extent to which they received each type of support from the staff at their institution (i.e., frequency of received support), they were asked to rate the extent to which they liked receiving that kind of support when in pain (i.e., support preferences). Several procedures were undertaken to ensure the content validity of this set of items, i.e., its ability to properly reflect the two functions of support we aimed to assess (DeVellis 2012). Such procedures have been thoroughly described in previous articles (Matos and Bernardes 2013; Matos et al. 2015) and have included the development of a pool of 23 items based upon expert consultation and its assessment by several independent judges (e.g., directors of day-care centers or nursing homes, nurses, experts on older adults’ physical activity, laypeople). The final set of items of the revised FSSADI_PAIN showed very good content validity (Cohen’s K = .90; Matos et al. 2015). Since the PFSSADI shared a similar set of items, it was reasonable to expect that it would also show good content validity. However, the PFSSADI construct and criterion-related validity, reliability and sensitivity were yet to be determined (DeVellis 2012).
Our validation plan included the following steps. We aimed at investigating the measure’s construct validity, first, by testing its underlying factorial structure. Based on previous findings (Matos et al. 2015), we had reasons to believe that the underlying factorial structure of the preferences measure would mirror the twofold factor structure of the revised FSSADI_PAIN. However, because we were assessing individual preferences for support, we did not expect preferences for autonomy and dependence support to be entirely uncorrelated. In fact, we even raised the possibility of the presence of a general factor of preferences for support, with preferences for autonomy and dependence as sub-dimensions. Therefore, we tested the fit of three alternative models: (model 1) preferences for autonomy and dependence support as two correlated factors; (model 2) preferences for autonomy and dependence support as first-order factors and a general second-order factor of preferences for pain-related formal support; (model 3) a general factor of preferences for pain-related formal social support. We expected that models 1 or 2 would have a better fit to the data than model 3.
Second, we used the revised FSSADI_PAIN to assess the preferences scale discriminant validity. We expected weak associations between the sub-scales of the two instruments not only because they measured different constructs (received support vs. support preferences) but also because previous studies have suggested that older adults might not always get the support they want or need (Herr and Garand 2001; Makris et al. 2015).
In order to assess the PFSSADI criterion-related validity, namely its concurrent validity (DeVellis 2012), we first aimed to investigate the relationship between older adults’ preferences for support for autonomy/dependence and their desires for dependence and independence (Nagurney et al. 2004). We expected that older adults with higher desire to do things on their own without the support of others would report higher preferences for autonomy support and lower preferences for dependence support. Conversely, older adults’ with higher desire to do things with the support of others would report lower preferences for autonomy support and higher preferences for dependence support.
Finally, we also aimed to test the internal consistency, test–retest reliability and sensitivity of the PFSSADI.
Methods
Sampling criteria
The data presented in this study were collected as part of a broader longitudinal investigation on the effects of formal social support for autonomy and dependence on older adults’ chronic pain-related disability (Matos, Bernardes, Goubert & Beyers, under review). Since, in this investigation, observational measures of physical functioning were used, only older adults who were capable of performing several physical tasks were recruited, namely older adults attending day-care centers instead of residential long term care facilities. More specifically, participants were recruited from a convenience sample of nine day-care centers in Lisbon, which were all non-profitable organizations, had at least 50 daily attendants and offered social outings, occupational and organized physical activities, meal services and transportation.
Participants were recruited based on the following inclusion criteria: (1) being a day-care center user for at least 6 months; (2) reporting constant or intermittent musculoskeletal pain for at least three months; (3) being able to read and write autonomously; (4) not presenting cognitive impairments, as assessed by institutions’ clinical staff.
The sample size was previously calculated by aiming at the best established subjects-to-variable ratio of 20:1 (e.g., Hair et al. 1995).
Instruments
Preferences for formal social support for autonomy and dependence in pain.
The PFSSADI was developed to assess older adults’ preferences for pain-related formal social support for functional autonomy and dependence. As aforementioned, we have adapted the revised FSSADI_PAIN eight items by changing the instructions, the items initial wording and their rating scales. More specifically, participants were asked to rate the extent to which they agreed with eight sentences that started with When I am in pain, I like it when the employees at this institution… and ended by specifying the type of pain-related support action. Like in the revised FSSADI_PAIN, four items reflected pain-related support actions to promote functional autonomy (e.g., encourage me to be social) and four items reflected actions to promote functional dependence (e.g., advise me to stop doing whatever that I am doing). Participants rated their agreement using a Likert scale ranging from (1) totally disagree to (5) totally agree.
The Portuguese and English final versions of the PFSSADI are in “Appendix”. The translation of the instrument from Portuguese to English followed the same procedures proposed by Beaton et al. (2000), to ensure the semantic, idiomatic, experiential and conceptual equivalence between the two versions.
Formal social support for autonomy and dependence in pain.
The revised FSSADI_PAIN (Matos et al. 2015) was used to test the discriminant validity of the preference scale. It assessed older adults’ perceptions of the frequency with which they have received pain-related social support from staff at their institution. As mentioned in the introduction, it was composed by two four-item sub-scales: (1) Perceived promotion of autonomy (e.g., When I am in pain, the employees at this institution…: … Encourage me to trust in my ability to keep on going … Help me to deal with practical aspects so I can participate in activities/social outings) and (2) Perceived promotion of dependence (e.g., When I am in pain, the employees at this institution…: …Bring me everything so that I don’t need to move; … Tell me not to push myself when I feel unable of handling certain issues). Participants were asked to rate each item on a 5-point Likert scale ranging from (1) not at all frequent to (5) extremely frequent. Both scales had very high levels of internal consistency in the present sample (α > .90). Each sub-scale score was calculated by averaging the respective four items. Higher scores represented higher perceived promotion of autonomy or dependence.
Desire for (in)dependence
The Portuguese version of Nagurney et al.’s measure (2004) of individual differences in the desire for functional (in)dependence was used to test the concurrent validity of the PFSSADI. A confirmatory factor analysis of the original scale (Nagurney et al. 2004) showed that it was composed by two items measuring desire for independence (e.g., It’s very important for me to retain my independence) and three items measuring desire for dependence (e.g., I would rather have others take care of things for me because it’s easier). Items were rated on a 5-point Likert scale, ranging from 1(strongly disagree) to 5 (strongly agree).
The original items were translated and culturally adapted for the Portuguese population based on Beaton et al.’s (2000) guidelines for the process of cross-cultural adaptation of self-report measures. Afterward, we ran a confirmatory factor analysis of the Portuguese version of the measure in the present sample. The variance of latent variables was constraint to 1, errors were kept fixed, observed variables were free, and the degrees of freedom were greater than 0. Results showed an acceptable fit to the data of a structure of two correlated factors (r = −.36; CFI = .992; NFI = .989; IFI = .992; RMSEA = .122; χ 2(4) = 13.83, p = .008): (1) desire for independence (n = 2 items, α = .98) and (2) desire for dependence (n = 3, α = .82). Each sub-scale score was calculated by averaging the respective items; higher scores represented higher desire for (in)dependence.
Procedure
This study followed the Ethics Guidelines issued in 2013 by the Scientific Commission of the hosting institution (CIS-IUL) and the American Psychological Association Ethical Principles of Psychologists and Code of Conduct (APA 2010). This study was also approved by the boards of the participating day-care centers.
As previously mentioned, the data presented in this paper were collected within a larger prospective study (Matos et al., under review), with assessments at three moments in time, each separated by 6 weeks. A 6-week lag was considered long enough to allow testing the specific hypotheses of the longitudinal study but short enough to avoid a large dropout rate, especially considering participants’ health status. At time 1 (T1), the director of each institution (a psychologist or social worker) helped us identify older adults who were able to read and write autonomously and attended the institution for more than 6 months. Also, based on their knowledge of the institutions’ clinical files on each user, directors could also help us identify older adults with no cognitive impairments. Afterward, potential participants were approached for further screening by the second author (MM), who is a female psychologist in her mid-thirties, with expertise in the provision of formal care to older adults. The researcher asked participants for the presence of current chronic musculoskeletal pain (i.e., on bones, muscles, ligaments and/or tendons) by adapting a methodological strategy used in several pain epidemiological studies (e.g., Breivik et al. 2006; Torrance et al. 2006). More specifically, participants were asked three yes-or-no questions: (1) “Have you had constant or intermittent pain for more than three consecutive months?” (2) “Did you feel this pain during last week?” and (3) “Was the pain located in your bones, muscles, ligaments and/or tendons?” Older adults who answered affirmatively to all three questions we invited to participate in a study on pain-related social support. Questionnaires were administered by face-to-face structured interviews, all conducted by MM in quiet rooms inside the respective institutions. This procedure was often explicitly requested by older adults, facilitating the participation of people with low levels of education and visual impairments. Furthermore, the anonymity and confidentiality of their data were guaranteed. After obtaining informed consent, participants filled out the PFSSADI, the revised FSSADI_PAIN and the Portuguese version of the desire for (in)dependence scale. In order to assess their pain location(s), pain severity and disability, participants were administered the Portuguese version of the Brief Pain Inventory (Azevedo et al. 2007). Participants were also administered the Portuguese version of the physical functioning scale of the Medical Outcomes Study—Short Form 36v2 (SF-36v2; Ferreira 2000a, b). Afterward, participants’ sociodemographic characteristics were collected. Finally, all participants and staff were thanked and debriefed.
In order to assess PFSSADI test–retest reliability and construct validity, after 6 weeks (Time 2) the same researcher (MM) approached the older adults who had participated at Time 1 and administered them a protocol that again included the PFSSADI, the Brief Pain Inventory and the physical functioning scale of the SF-36v2. As in Time 1, questionnaires were administered by face-to-face structured interviews in quiet rooms inside the respective institutions. At this time, two participants refused to collaborate and sixteen were unreachable due to disease, resulting in a total sample of 149 participants. The sample at T2 did not differ from the sample at T1, both in terms of sociodemographic, clinical and pain-related characteristics and levels of self-reported physical functioning.
Data analyses
First, using SPSS (version 20 IBM Corp, Armonk, NY), we verified the absence of missing data and analyzed item distribution for the total sample at T1 (n = 165). Then, a principal axis factoring analysis (oblique rotation) was conducted with participant responses of the preferences scale at T1. Afterward, a confirmatory factor analysis (CFA) was performed with participant responses at T2 (n = 149), with no missing data, using maximum likelihood (ML) estimation, with the support of AMOS v20 (IBM Corp). CFA was ran to test the fit of three alternative models: (1) preferences for autonomy and dependence support as correlated factors; (2) general pain-related social support preferences as a second-order factor with preferences for autonomy and dependence support as first-order factor; and (3) one general factor of preferences for pain-related social support that included all items. Criteria for good fit were established by CFI > .90; NFI > .90; IFI > .90; RMSEA < .05 (e.g., Hu and Bentler 1999). Given that item distributions deviated from the normal curve, CFA was also run using a nonparametric method (bootstrap) with 5000 subsamples in order to confirm the results obtained with the parametric method (ML). Next, using SPSS v20, we explored the relationship between the pain-related social support preferences and participants’ clinical, pain-related and sociodemographic characteristics, using t-tests, Chi-squares or Spearman correlations. Given the considerable amount of tested relations, we reduced our critical p value to .01 to prevent an inflated type I error. Social support preferences were not significantly associated with any of the sociodemographic (age, sex and educational level), clinical and pain-related variables (duration, intensity and interference) or with self-reported physical functioning. Finally, we used Spearman correlations to investigate the association between support preferences and desires for (in)dependence, pain-related received support and to assess the test–retest reliability of preferences for autonomy and dependence support.
Results
Participant characteristics
One hundred and sixty-five older adults (67.3% women) were invited and agreed to participate in this study. Table 1 summarizes participants’ sociodemographic, pain-related characteristics and physical functioning levels. All participants were aged 60 or above and had, on average, around 5 years of formal education. Most participants had elementary school degrees (81.8%), 13.0% had middle school degrees, and a minority had high school (3.5%) or higher education degrees (1.8%). Regarding participants’ marital status, 60.6% were widowed, 22.4% married, 11.8% divorced and 5.3% single.
Table 1.
Participants’ sociodemographics, pain-related characteristics and physical functioning levels (n = 165)
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age | 60 | 99 | 79.01 | 7.8 |
| Years of education | 2 | 20 | 4.9 | 2.6 |
| Pain-related characteristics | ||||
| Pain duration (years) | 0.25 | 52 | 7.13 | 9.9 |
| Number of pain locations | 1 | 5 | 1.4 | .77 |
| Pain intensity | 0 | 10 | 3.0 | 2.0 |
| Pain interference | 0 | 10 | 3.6 | 3.3 |
| Physical functioning | ||||
| 0 | 100 | 36.4 | 34.4 | |
Pain intensity/interference scores ranged from 0 (no pain/does not interfere) to 10 (pain as bad as you can imagine/completely interferes). Physical functioning scores ranged from 0 (lowest ability) to 100 (highest ability) to perform daily physical activities
All participants suffered from chronic musculoskeletal pain. Pain duration ranged from 3 months to 52 years and, on average, participants reported relatively low levels of pain intensity and interference. Most participants reported pain in only one location (68.8%), 21.2% in two locations and the remaining in three or more locations. Lower limbs (60.6%) and back (49.9%) were the most prevalent pain locations, followed by upper limbs (15.9%) and hips (5.9%). Furthermore, several health conditions were present in this sample—spine diseases (31.8%), rheumatoid arthritis (9.4%), osteoporosis (7.1%), osteoarthritis (2.9%) and fibromyalgia (1.2%). Also 19.7% had hypertension and 44.7% reported frequent dizziness and/or chest pain. On average, participants reported a relatively low level of physical functioning despite the low levels of pain intensity and pain interference (Table 1).
Item descriptive analysis and sensitivity
The analysis of item distribution on the total sample at T1 (n = 165) showed that participants’ answers covered the scale range for every item (min = 1; max = 5). Means ranged from 2.62 to 3.48 and standard deviations ranged from 1.25 to 1.44 (Table 2). In general, preferences for autonomy support items showed averages above the central point of the rating scale (>3), while preferences for dependence support items showed averages below this point (<3). Preferences for autonomy support items showed higher levels of skewness (skewness/SEskewness > |1.96|), i.e., participants rated these items mostly using the right end of the scale, which showed consistent preferences toward autonomy promotion. Preferences for dependence support items showed higher standard deviations and levels of kurtosis (kurtosis/SEkurtosis > |1.96|), namely platykurtic distributions. None of the items followed a normal distribution (Table 2).
Table 2.
Descriptive statistics and principal axis factor analysis with oblique rotation of the items of the PFSSADI (Time 1)
| Items | Descriptives | Factor loadings | ||||
|---|---|---|---|---|---|---|
| When I am in pain, I like it when the employees at this institution… | M | SD | Kurtosis/SE | Skewness/SE | PAS | PDS |
| …encourage me to participate in leisure activities | 3.46 | 1.26 | −0.44 | −4.99 | 1.007 | −.015 |
| …encourage me to trust in my ability to keep on going | 3.48 | 1.25 | −0.19 | −5.14 | .993 | −.020 |
| …help me to deal with practical aspects (e.g., transportation, reservations, tickets) so I can participate in activities/social outings | 3.42 | 1.26 | −0.57 | −4.96 | .945 | −.041 |
| …tell me not to push myself when I feel unable of handling certain issues | 2.63 | 1.40 | −3.94 | 0.27 | −.020 | 1.002 |
| …bring me everything so that I don’t need to move | 2.62 | 1.43 | −4.10 | 0.31 | −.033 | 1.000 |
| …advise me to stop doing whatever I am doing | 2.70 | 1.43 | −3.97 | −0.08 | .063 | .908 |
| …tell me that I need help from others to cope with my pain (PDS) | 2.63 | 1.44 | −4.01 | 0.20 | – | – |
| …encourage me to socialize (PAS) | 3.48 | 1.25 | −0.19 | −5.14 | – | – |
| Cronbach’ α | .988 | .980 | ||||
Values in bold refer to item loadings in the respective factor
PAS Preferences for Autonomy Support, PDS Preferences for Dependence Support
Construct validity and reliability
Principal axis factor analysis
First, two items (one per sub-scale; see Table 2) were eliminated given their extreme communalities (above .98). Then, a principal axis factor analysis (oblique rotation) was performed (KMO = .802; Bartlett’s χ 2 (15) = 1865.57, p < .001). Two factors were extracted, based on the Kaiser criterion, accounting for 95.6% of the total variance: (a) Preferences for Autonomy Support (n = 3 items) and (b) Preferences for Dependence Support (n = 3 items). Factors showed very high internal consistency and a moderate positive correlation (r = .51, p < .001).
Factor descriptive analysis and sensitivity
Participants’ scores on preferences for autonomy support covered the entire scale range (min = 1; max = 5). The preferences for autonomy support factor presented a mean value suggesting moderate to high preference for autonomy support (M = 3.45, SD = 1.24). This factor did not present a normal distribution; it showed a high level of skewness (skewness/SE = −5.08) and an acceptable level of kurtosis (kurtosis/SE = −.31). Participants’ scores on preferences for dependence support also covered the entire scale range (min = 1; max = 5). The Preferences for dependence support factor presented a mean value (M = 2.65, SD = 1.39) suggesting moderate to low preferences for dependence promotion. This factor did not present a normal distribution; it showed an acceptable level of skewness (skewness/SE = .15) but a flatter than normal distribution (kurtosis/SE = −3.85).
Confirmatory factor analyses
The first tested model was the one obtained from the exploratory factor analysis—two correlated factors (model 1; Fig. 1). Variance of latent variables was constrained to 1, errors were kept fixed, observed variables were free, and the degrees of freedom were greater than 0. The observation of several ML-based fit indexes (CFI = 1; NFI = .996; IFI = 1; RMSEA = .023) that were within the established cutoffs (e.g., Hu and Bentler 1999) indicated a good fit. Moreover, a good fit was found between the model and the observed data (χ 2 (8) = 8.602, p = .377).
Fig. 1.
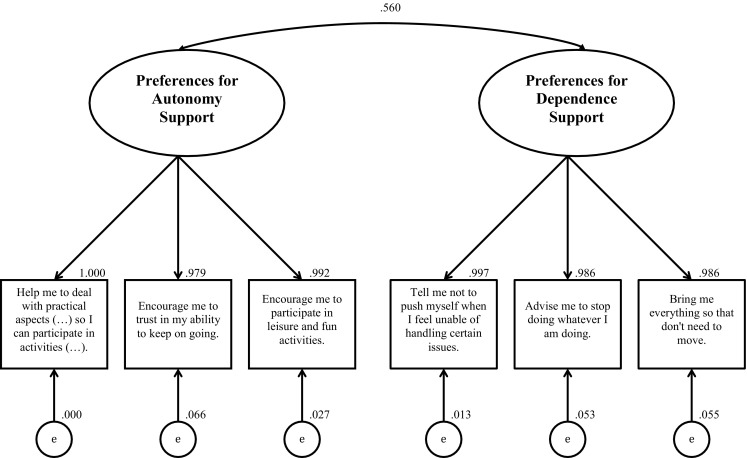
Confirmatory factor analysis of the PFSSADI
Then, model 2 was tested—pain-related social support preferences as a second-order factor with preferences for autonomy and dependence support as first-order factors. This model presented a poor fit to the data and, as compared to model 1 [χ 2 (9) = 886.091, p < .001; CFI = .583; NFI = .581; IFI = .584; RMSEA = .817].
Afterward, model 3 was tested—one general factor of preferences for pain-related social support that included all items, also showing a poor fit to the data [CFI = .583; NFI = .582; IFI = .584; RMSEA = .817; χ 2 (9) = 886.091, p < .000].
Finally, the results obtained by the parametric method (ML) were replicated with a nonparametric method (bootstrap); there was no bias between the estimates for every item.
Discriminant validity
No significant correlations were found between preferences for autonomy support and perceived promotion of autonomy (r = .141, p = .106) and with perceived promotion of dependence (r = .028, p = .747). No significant correlations were found between preferences for dependence support and perceived promotion of autonomy (r = −.035, p = .688) or perceived promotion of dependence (r = .019, p = .832).
Test–retest reliability
Both preferences for autonomy support (r = .679, p < .001) and dependence support (r = .703, p < .001) sub-scales showed high test–retest reliability.
Criterion-related validity
Preferences for autonomy support showed no significant correlations with desires for dependence or independence. Preferences for dependence support were positively correlated with desires for dependence (r = .329, p < .001) and negatively correlated with desires for independence (r = −.412, p < .001).
Discussion
This paper aimed at the development and validation of the preferences for formal social support for autonomy and dependence in pain inventory (PFSSADI), which assesses older adults’ preferences for formal social support for functional autonomy and dependence in pain. Generally, our findings showed that the PFSSADI is a new measure that, in the present sample, showed good psychometric properties; it presented good construct and criterion-related validity and proved to be a reliable and sensitive tool. A detailed discussion of the instrument’s psychometric properties now follows.
Construct validity
With regard to its construct validity, exploratory and confirmatory factor analyses supported our predictions for a twofold underlying structure: (1) preferences for support that promotes functional autonomy when in pain and (2) preferences for support that promotes functional dependence when in pain. This structure mirrors the revised FSSADI_PAIN underlying structure (Matos et al. 2015), which also included two factors, namely perceived promotion of autonomy and perceived promotion of dependence. The PFSSADI sub-scales, however, are one-item shorter than the sub-scales of the revised FSSADI-PAIN, given the extreme redundancies of these items. Despite being shorter, the twofold structure of the PFSSADI accounted for almost 96% of the variance, showing that it is a short and parsimonious measure with very good construct validity. Also, as predicted, preferences for autonomy and dependence support showed a moderate correlation; the higher the preferences for autonomy support, the higher the preferences for dependence support. This was supported by the good fit to the data of model 1—Preferences for autonomy and dependence support as correlated factors. This correlation, however, is not being accounted for by a second-order factor—preferences for formal pain-related social support—given the poor fit of model 2 to the data.
As for PFSSADI discriminant validity, no significant associations were found between older adults’ preferences for support and received support. Therefore, despite the similarity of the set of items and the fact that they were administered in tandem, older adults’ still discriminated support preferences (“what I like”) from received support (“what I usually get”). However, this also suggests that pain-related social support received from the staff is not being responsive to older adults’ preferences, reflecting a generalized tendency for undervaluing and disregarding older adults’ pain experiences (Herr and Garand 2001; Makris et al. 2015).
Criterion-related validity
As for its criterion-related validity, namely its concurrent validity, our results partially supported our hypotheses; although preferences for autonomy support did not show any significant relationships with desires for dependence and independence, older adults who preferred more support for dependence also reported higher desire for dependence and lower desire for independence. These findings may shed some light on Nagurney et al.’s (2004) results, which show that individuals’ desires for (in)dependence influence their (un)favorable responses to socially supportive interactions. Social support preferences may indeed be a mediator of this relationship, but this remains to be tested. The reason as to why preferences for autonomy support did not show any significant relation with desires for (in)dependence may be due to the fact that preferences for autonomy support scores were more skewed toward a ceiling effect. In fact, preferences for autonomy support presented a lower dispersion of participants’ scores than preferences for dependence support; most participants reported high preferences for autonomy support. It may also be noted that, on average, older adults’ seemed to prefer more support for autonomy than for dependence, which is in line with previous findings that have suggested that solicitous responses to pain behaviors may not always be desired or positive reinforcers of pain behaviors (e.g., Newton-John and Williams 2006).
Reliability and sensitivity
Finally, our findings suggest that the PFSSADI is a reliable measure in the present sample. First, preferences for autonomy and dependence support presented high internal consistency indices, showing that random error has little influence on participants’ answers. Second, both sub-scales showed good temporal stability, suggesting that preferences for pain-related formal social support are relatively stable across time. Also, the PFSSADI also seems to be a sensitive measure as it was able to differentiate several levels of older adults’ preferences for autonomy and dependence support based on their global scores (DeVellis 2012).
Limitations and implications for further research
Like every piece of research, the present study has limitations that bear direct implications for future research. First, and regarding the study’s external validity, the fact we have only included in our sample Portuguese older adults with musculoskeletal chronic pain, low levels of formal education and attending day-care centers hampers the generalization of our findings. Further studies investigating the psychometric qualities of the PFSSADI with other samples (e.g., older adults with acute pain) in other settings (e.g., nursing homes, residential care) and cultures are warranted. Indeed, to facilitate the adaptation of the PFSSADI to other cultures we provide in “Appendix” its English version. Its psychometric properties, however, should still be assessed in an English speaking country.
Second, more evidence on the scale’s content, discriminant and convergent validity is needed. As for its content validity, as in many well-known and validated pain-related measures (e.g., Pain Catastrophizing Scale; Sullivan et al. 1995), the initial unspecific wording of the items when I am in pain was meant to stimulate responses anchored on an overall representation of individuals’ pain experiences, instead of a specific pain level (e.g., at its maximum). We cannot guarantee that this was the case for every participant. Hence, a linguistic validation of the items would be useful to empirically support our assumption. Even so, inter- and intra-individual differences in participants’ “overall pain experiences” would be expected, which could influence their preferences for pain-related support for autonomy and dependence. Although our findings did not show significant associations between pain severity/interference and preferences for support for autonomy/dependence, further studies on the relationship between pain-related characteristics and support preferences are needed.
Our choice of the FSSADI_PAIN to assess the discriminant validity could have backfired if we had found strong positive correlations between the sub-scales. Indeed, such correlations wouldn’t necessarily have spoken against the discriminant validity of the scale but, instead, reflect an ideal association between older adults’ preferences for support and received support. Therefore, future studies should use measures of constructs that, regardless of the circumstances, have no theoretical relationship with preferences for autonomy/dependence support.
Information on the scale’s convergent validity is also lacking. A recent measure—the Pain Response Preference Questionnaire (PRPQ; McWilliams et al. 2009)—could be used in future studies. It assesses the extent to which three types of responses to pain are desired from a significant other—Solicitude, Encouragement and Suppression. If suppression (e.g., ignore or stop pain talk) may not be considered a social support response, solicitude and encouragement can and may be associated with our concepts of preferences for dependence and autonomy support, respectively.
Third, the selection of participants with no cognitive impairments was exclusively based on institutions’ clinical staff assessments. Although this was done to avoid adding another instrument to an already long data collection protocol, it is a limitation of the present study. Indeed, we did not know which criteria or procedures were used to make such clinical assessment or if the files were updated at the time of the data collection. This means that we cannot preclude the possibility of having included in our sample older adults with mild cognitive impairments. If this was indeed the case, it does not seem to have affected the instruments’ reliability, validity and sensitivity for the present sample. However, in future studies it would be interesting to explicitly include older adults with mild/moderate cognitive impairments, given their high prevalence in the older population (e.g., Kiejna et al. 2011).
Finally, it would have been interesting to have collected information on care facilities’ characteristics (e.g., staff/attendants ratio), as they may influence the degree to which older adults’ preferences of support are met.
Despite its limitations, this study has several current theoretical, methodological and practical contributions. First, the present instrument is, currently, one of only a few valid measures of pain-related social support preferences. As such, it may contribute to future research on the role of pain-related social support preferences, and social support responsiveness to such preferences, on older individuals’ pain experiences. Second, the PFSSADI, used in tandem with the revised FSSADI_PAIN, may stimulate future systematic research on the role of two clearly distinct functions of social support on the promotion of older adults’ healthy aging. This clearly bridges a gap in the current literature, where most research has been focusing on informal social support in early or middle adulthood. Hopefully, by bridging this gap, our findings may stimulate more research on a segment of the population that will exponentially grow in the next few years in western societies.
As for practical contributions, like the revised FSSADI_PAIN, the PFSSADI is very short and user-friendly. Both instruments, used simultaneously, may provide healthcare practitioners and staff at support institutions a fast, accurate and reliable way to assess the extent to which older adults with chronic pain perceive the support they are receiving as being responsive to their needs. This information may be useful to promote a better adjustment of social support provided by formal care institutions to individuals’ needs and/or preferences. These measures may also be easily integrated in the assessment of intervention programs aiming at promoting older adults’ functional autonomy and quality of life despite pain.
Acknowledgements
We would like to thank Prof. Helena Carvalho for her help with statistics. This study was partially funded by Fundação para a Ciência e Tecnologia (SFRH/BD/79145/2011). We declare that there were no financial or other relationships that lead to conflicts of interest in the development of this research.
Appendix: PFSSADI
Portuguese version
Durante toda a vida, a maior parte das pessoas sente dor de vez em quando. A dor pode ser uma experiência que dificulta o nosso dia-a-dia e a realização de várias tarefas quotidianas. Nestas circunstâncias, o apoio recebido nas instituições, como os Lares e Centros de Dia, pelas pessoas que aí trabalham pode ter um papel muito relevante no auxílio aos utentes com dores.
Com este questionário gostaríamos de conhecer as suas preferências face à ajuda que recebe quando tem dores. Por favor, faça um círculo num dos números de 1 a 5, mostrando em que medida concorda com cada uma das seguintes afirmações.
Muito obrigada pela sua colaboração.
Quando eu estou com dores, gosto que os/as funcionários/as desta instituição…
| Discordo totalmente | Discordo | Não concordo nem discordo | Concordo | Concordo totalmente | |
|---|---|---|---|---|---|
| 1. …me ajudem a tratar de aspetos práticos (ex., transporte, reservas, bilhetes) para que consiga participar em actividades/saídas sociais | 1 | 2 | 3 | 4 | 5 |
| 2. …me incentivem a confiar na minha capacidade para continuar a funcionar | 1 | 2 | 3 | 4 | 5 |
| 3. …me incentivem a participar nas actividades de lazer e diversão | 1 | 2 | 3 | 4 | 5 |
| 4. …me digam para não insistir quando não me sinto capaz de tratar de alguns problemas | 1 | 2 | 3 | 4 | 5 |
| 5. …me aconselhem a parar tudo o que estou a fazer | 1 | 2 | 3 | 4 | 5 |
| 6. …me tragam tudo o que eu necessito para que não precise de me mexer | 1 | 2 | 3 | 4 | 5 |
English version
Throughout life, most people feel pain from time to time. Pain can be a difficult experience that challenges our day-to-day and the performance of various daily tasks. In these circumstances, the support received in institutions, such as Nursing Homes and Day Centers, by the people who work there can have a very important role in helping clients with pain.
This questionnaire is designed to gather information about your preferences regarding the support received when experiencing pain. Please circle one of the numbers between 1 and 5, indicating the extent to which you agree or disagree with each of the following statements.
Thank you for your collaboration.
When I am in pain, I like it when the employees at this institution…
| Totally disagree | Disagree | Neither agree nor disagree | Agree | Totally agree | |
|---|---|---|---|---|---|
| 1. … help me to deal with practical aspects (e.g., transportation, reservations, tickets) so I can participate in activities/social outings | 1 | 2 | 3 | 4 | 5 |
| 2. …encourage me to trust in my ability to keep on going | 1 | 2 | 3 | 4 | 5 |
| 3. …encourage me to participate in leisure and fun activities | 1 | 2 | 3 | 4 | 5 |
| 4. … tell me not to push myself when I feel unable of handling certain issues | 1 | 2 | 3 | 4 | 5 |
| 5. … advise me to stop doing whatever I am doing | 1 | 2 | 3 | 4 | 5 |
| 6. … bring me everything so that I don’t need to move | 1 | 2 | 3 | 4 | 5 |
Footnotes
Responsible editor: H.-W. Wahl.
References
- American Psychological Association (2010) Ethical principles of psychologists and code of conduct: including 2010 Amendments. American Psychological Association website http://www.apa.org/ethics/code/index.aspx. Accessed Jan 2014
- Azevedo LF, Pereira AC, Dias C, Agualusa L, Lemos L, Romão J, Castro-Lopes JM. Tradução, adaptação cultural e estudo multicêntrico de validação de instrumentos para rastreio e avaliação do impacto da dor crónica. Dor. 2007;15:6–56. [Google Scholar]
- Beaton D, Bombardier C, Guillemin F, Ferraz M. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Campbell P, Wynne-Jones G, Dunn KM. The influence of informal social support on risk and prognosis in spinal pain: a systematic review. Eur J Pain. 2011;15:444.e1–444.e14. doi: 10.1016/j.ejpain.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell P, Wynne-Jones G, Muller S, Dunn KM. The influence of employment social support for risk prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Archiv Occup Environ Health. 2013;86:119–137. doi: 10.1007/s00420-012-0804-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CIS-IUL (2013) Ethical guidelines. http://www.cis.iscte-iul.pt/files/Research/LAPSO/ethicsguidelines2013.pdf
- Cohen S, Underwood L, Gottlieb B. Social support measurement and intervention: a guide for health and social scientists. Oxford: Oxford University Press; 2000. [Google Scholar]
- DeVellis RF. Scale development: theory and applications. 3. Thousand Oaks: SAGE Publications; 2012. [Google Scholar]
- Ferreira PL. Criação da versão portuguesa do MOS SF-36. Parte I—Adaptação cultural e linguística. Acta Med Port. 2000;13:55–66. [PubMed] [Google Scholar]
- Ferreira PL. Criação da versão portuguesa do MOS SF-36. Parte II—testes de validação. Act Med Port. 2000;13:119–127. [PubMed] [Google Scholar]
- Ferrel BA. Pain evaluation and management in the nursing home. Ann Intern Med. 1995;123:681–687. doi: 10.7326/0003-4819-123-9-199511010-00007. [DOI] [PubMed] [Google Scholar]
- Gibson SJ. IASP global year against pain in older persons: highlighting the current status and future perspectives in geriatric pain. Expert Rev Neurother. 2007;7:627–635. doi: 10.1586/14737175.7.6.627. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos T, Craig KD, Duck S, Cano AM, Goubert L, Jackson P, Mogil J, Rainville P, Sullivan M, de Williams AC, Vervoort T, Fitzgerald T. A biopsychosocial formulation of pain communication. Psychol Bull. 2011;137:910–939. doi: 10.1037/a0023876. [DOI] [PubMed] [Google Scholar]
- Hair JRJF, Anderson RE, Tatham RL, Black WC. Multivariate date analysis with readings. New Jersey: Prentice Hall; 1995. [Google Scholar]
- Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R. Long-term care services in the United States: 2013 overview. National Center for Health Statistics. Vital Health Stat. 2013;3:37. [PubMed] [Google Scholar]
- Hébert R, Guilbault J, Desrosiers J, Dubuc N. The functional autonomy measurement system (SMAF): a clinical-based instrument for measuring disabilities and handicaps in older people. Geriatr Today. 2001;4:141–147. [Google Scholar]
- Helme RD, Gibson SJ. Pain in the elderly. In: Jensen TS, Turner JA, editors. Proceedings of the 8th world congress on pain. Seattle: IASP Press; 1997. pp. 919–944. [Google Scholar]
- Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17:417–431. doi: 10.1016/S0749-0690(05)70078-1. [DOI] [PubMed] [Google Scholar]
- Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17:457–463. doi: 10.1016/S0749-0690(05)70080-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Ibarra-Rovillard MS, Kuiper N. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin Psychol Rev. 2011;31:342–352. doi: 10.1016/j.cpr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Kiejna A, Frydecka D, Adamowski T, Bickel H, Reynish E, Prince M, Caracciolo B, Fratiliglioni L, Geoges J. Epidemiological studies of cognitive impairment and dementia across Eastern and Middle European countries. Int J Geriatr Psychiatry. 2011;26:111–117. doi: 10.1002/gps.2511. [DOI] [PubMed] [Google Scholar]
- Krahé C, Springer A, Weinman JA, Fotopoulou A. The social modulation of pain: others as predictive signals of salience—a systematic review. Front Hum Neurosci. 2013;386:1–21. doi: 10.3389/fnhum.2013.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: a review and integration of theoretical models and empirical evidence. J Pain. 2006;7:377–390. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisel NC, Gabel SL. The paradox of received social support: the importance of responsiveness. Psychol Sci. 2009;20:928–932. doi: 10.1111/j.1467-9280.2009.02388.x. [DOI] [PubMed] [Google Scholar]
- Makris UE, Higashi RT, Marks EG, Fraenkel L, Sale JE, Gill TM, Reid MC. Ageism, negative attitudes, and competing co-morbidities: why older adults may not seek care for restricting back pain—a qualitative study. BMC Geriatr. 2015;15(39):1–9. doi: 10.1186/s12877-015-0042-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matos M, Bernardes SF. The Portuguese formal social support for autonomy and dependence in pain inventory (FSSADI_PAIN): a preliminary validation study. Br J Health Psychol. 2013;18:593–609. doi: 10.1111/bjhp.12006. [DOI] [PubMed] [Google Scholar]
- Matos M, Bernardes SF, Goubert L, Carvalho H. The revised formal social support for autonomy and dependence in pain inventory (FSSADI_PAIN): confirmatory factor analysis and validity. J Pain. 2015;16:508–517. doi: 10.1016/j.jpain.2015.02.006. [DOI] [PubMed] [Google Scholar]
- Matos M, Bernardes SF, Goubert L. The relationship between perceived promotion of autonomy/dependence and pain-related disability in older adults with chronic pain: the mediating role of self-reported physical functioning. J Behav Med. 2016;39:704–715. doi: 10.1007/s10865-016-9726-x. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Saldanha KM, Dick BD, Watt MC. Development and psychometric evaluation of a new measure of pain-related support preferences: the Pain Response Preference Questionnaire. Pain Res Manage. 2009;14:461–469. doi: 10.1155/2009/429767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2. Seattle: IASP Press; 1994. [Google Scholar]
- Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. 2014;69:197–207. doi: 10.1037/a0035794. [DOI] [PubMed] [Google Scholar]
- Nagurney A, Reich JW, Newsom JT. Gender moderates the effects of independence and dependence desires during the social support process. Psychol Aging. 2004;19:215–218. doi: 10.1037/0882-7974.19.1.215. [DOI] [PubMed] [Google Scholar]
- Newton-John TRO. Solicitousness and chronic pain: a critical review. Pain Rev. 2002;9:7–27. doi: 10.1191/0968130202pr186ra. [DOI] [Google Scholar]
- Newton-John TR, Williams AC. Chronic pain couples: perceived marital interactions and pain behaviors. Pain. 2006;123:53–63. doi: 10.1016/j.pain.2006.02.009. [DOI] [PubMed] [Google Scholar]
- Philip LJ. Social isolation and the perceived importance of in-person care amongst rural older adults with chronic pain: a review and emerging research agenda. J Pain Manag. 2014;7:13–21. [Google Scholar]
- IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp
- Reyes-Gibby CC, Aday LA, Cleeland CS. Impact of pain on self-related health in the community-dwelling older adults. Pain. 2002;95:75–82. doi: 10.1016/S0304-3959(01)00375-X. [DOI] [PubMed] [Google Scholar]
- Selcuk E, Ong AD. Perceived partner responsiveness moderates the association between received emotional support and all-cause mortality. Health Psychol. 2013;32:231–235. doi: 10.1037/a0028276. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Binnekade TT, Soundy A, Schofield P, Huijnen IP, Eggermont LH. Are older adults with chronic musculoskeletal pain less active than older adults without pain? A systematic review and meta-analysis. Pain Med. 2013;14:1316–1331. doi: 10.1111/pme.12154. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. doi: 10.1037/1040-3590.7.4.524. [DOI] [Google Scholar]
- Thomsen AB, Sorensen J, Sjogren P, Eriksen J. Chronic non-malignant pain patients and health economic consequences. Eur J Pain. 2002;6:341–352. doi: 10.1016/S1090-3801(02)00023-X. [DOI] [PubMed] [Google Scholar]
- Torrance N, Smith BH, Bennett MI, Lee AJ. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain. 2006;7:281–289. doi: 10.1016/j.jpain.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Turk DC. Chronic non-malignant pain patients and health economic consequences. Eur J Pain. 2002;6:353–355. doi: 10.1016/S1090-3801(02)00024-1. [DOI] [PubMed] [Google Scholar]
- Union European. Long-term care for the elderly: provisions and providers in 33 European countries. Luxembourg: Publications Office of the European Union; 2012. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Ageing 2013. ST/ESA/SER.A/348
- Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153:1144–1147. doi: 10.1016/j.pain.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Wilkie R, Tajar A, McBeth J. The onset of widespread musculoskeletal pain is associated with a decrease in healthy ageing in older people: a population-based prospective study. PLoS ONE. 2013;8:e59858. doi: 10.1371/journal.pone.0059858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada E, Thomas DC. Common musculoskeletal diagnoses of upper and lower extremities in older patients. Mt Sinai J Med. 2011;78:546–557. doi: 10.1002/msj.20274. [DOI] [PubMed] [Google Scholar]


