Abstract
Background
Type II diabetes mellitus (T2DM) is complicated by multiple cardio-metabolic risk factors. Controlling these factors requires lifestyle modifications alongside utilisation of anti-diabetic medications. Different glucose lowering [(biguanides (BIGs), sulfonylureas (SUAs), thiazolidinediones (TNZ)], lipid lowering (statins), and anti-hypertensive medicines [angiotensin converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs), angiotensin II receptor blockers (ARBs) and central acting drugs (CADs)] have been approved for controlling hyperglycaemia, dyslipidaemia and hypertension respectively. Here, we examined factors that characterise T2DM and explored the response to medication therapy among T2DM patients.
Methods
This prospective cohort study recruited 241 T2DM patients reporting at a clinic in Ghana, from January through to August, 2016. Each patient’s demographic, medications and anthropometric data was obtained while information on medication adherence was captured using Morisky adherence scale-8 (MMAS-8). Fasting blood samples were collected for biochemical analysis.
Results
The mean age of participants was 57.82 years for baseline and six-month follow-up. Physical activity differed at baseline and follow up (p < 0.05) but not body mass index (BMI). BIG alone, or in combination with SUA and TNZ did not improve glycaemic status at follow up (p > 0.05). Many participants using either ACEI or ARB were able to control their blood pressures. Among dyslipidaemia patients under statin treatment, there was an improved lipid profile at follow-up.
Conclusions
Statin medications are effective for reducing dyslipidaemia in T2DM patients. However, control of modifiable risk factors, particularly blood glucose and to a lesser degree blood pressure is suboptimal. Addressing these will require concomitant interventions including education on medication adherence and correct dietary plans, lifestyle modifications and physical activity.
Electronic supplementary material
The online version of this article (doi:10.1186/s40169-017-0162-5) contains supplementary material, which is available to authorized users.
Keywords: Type II diabetes mellitus, Hypertension, Anti-diabetic medications, Risk factors, Ghana
Background
Despite substantial efforts, type II diabetes mellitus (T2DM) remains a major contributor to the world’s morbidity and mortality [1, 2]. In 2014 alone, more than 2.2 million people died from the disease and at approximately the same time, nearly 415 million adults were affected worldwide, representing a prevalence rate of ≈8.5% [2, 3]. This prevalence rate is expected to translate into 439 million T2DM cases by 2030 [3, 4]. Unfortunately, countries with less healthcare resources such as those in sub-Saharan Africa (SSA) are among the most affected with some 14.2 million people presently suffering from the disease [2]. For example, in Ghana, T2DM affected more than 266,200 individuals at a prevalence rate of 6% in 2015, and it is presently ranked among the top 10 causes of all adult deaths [2, 5].
People with T2DM have an increased risk of developing many health problems such as cardiovascular diseases [6, 7], amputations [8], depression [9, 10], and cognitive impairment [11–14]. Moreover, prolonged hyperglycaemia is strongly linked with many microvascular and, to a lesser extent, macrovascular complications and premature mortality [15]. In fact, just a 1% rise in glucose level will lead to an 18% increased risk for cardiovascular events [16], 37% increased risk for renal diseases [11] and 12–14% increased risk for premature mortality [11, 15, 16].
Additionally, the majority of T2DM patients are physically inactive which has led to dyslipidaemia, obesity and hypertension [17, 18]. These in turn lead to further consequences. Studies have shown that obesity accounts for 14% of all adult deaths while hypertension alone is an independent risk factor for cognitive decline [19], renal dysfunction [20, 21] and ultimately responsible for 45% of all deaths. Therefore, given these detrimental outcomes, controlling known modifiable factors should be a priority.
It has long been documented that achieving good glycaemic levels is pivotal to delaying T2DM complications. According to the American Diabetes Association (ADA), reduction of microvascular and macrovascular complications is possible at HbA1c <7% [22]. This could be achieved with single, combination or multiple glucose lowering medications [23, 24].
Alongside maintaining normal glycaemic levels, therapeutic interventions should be extended to other concomitant factors such as dyslipidaemia, hypertension and obesity [25, 26]. Different lipid lowering and anti-hypertensive medicines have been approved for controlling dyslipidaemia and hypertension respectively; majority of which are currently available in Ghana [5, 26]. Yet, the control of T2DM modifiable factors has been suboptimal, partly because studies to create awareness of T2DM are generally scarce in this region. Moreover, these studies have mainly been cross-sectional providing limited information on association or causality. Therefore, in this study, we explored the manifestations and the associated factors that characterise T2DM in a longitudinal design. Additionally, this study highlights the proportion of T2DM patients that have good glycaemic control, blood pressure and lipid levels and addresses the factors that contribute to poor management and control of these modifiable risk factors.
Methods
Study design
This prospective cohort study was conducted at the diabetic clinic of the Komfo Anokye Teaching Hospital (KATH) from January through to August 2016. In all, 241 participants with T2DM aged 35–70 years who reported to the clinic for review and medications were recruited. The study protocol was reviewed by the Committee on Human Research, Publication and Ethics (CHRPE), Kwame Nkrumah University of Science and Technology (KNUST), Kumasi and the Human Research Ethics Committee (HREC), Edith Cowan University (ECU), Australia. Written informed consent was obtained from each participant.
Inclusion and exclusion criteria
The study included only those who were diagnosed as having T2DM, based on the international classification of diabetes (ICD 10) criteria. Participants who were taking insulin injections were assumed to be suffering from type I diabetes mellitus and therefore were excluded. Additionally, among the original 260 T2DM participants recruited for the study, 19 were excluded, mainly because of missing clinical data.
Anthropometric and blood pressure measurements
After obtaining demographic data and information on the general health status from each participant, information of medication adherence was obtained using the validated Morisky Adherence Scale-8 (MMAS-8). This questionnaire comprises 8 items and responses for item 1 through 7 are either ‘yes’ or ‘no’ whereas item 8 comprises a 5-point Likert scale [27]. Following this, anthropometric measurements were taken. Weight (kg) and height (cm) were measured with a standard stadiometer (SECA, Hamburg, Germany). These were used to determine the body mass index (BMI), calculated as BMI = weight (kg)/height (m)2. Waist and hip circumference were measured in cm using a tape measure and waist-to-hip ratio (WHR) was calculated as WHR = waist (cm)/hip (cm). Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using a standard sphygmomanometer (Omron HEM711DLX, UK). To assess the level of physical activity, we asked basic questions such as 1) what is the level of physical activity during the last 7 days?, 2) on how many days did you walk for at least 10 min at a time in your leisure time?
Blood sample collection and biochemical assay
Venous fasting blood samples were collected from each participant into tubes containing EDTA (ethylene diamine tetraacetic acid), fluoride oxalate and gel separator. Fasting plasma glucose (FPG) in fluoride tubes and glycated haemoglobin (HbA1c) in EDTA tubes were measured on an automated chemistry analyser (Roche Diagnostics, COBAS INTEGRA 400 Plus, USA). Similarly, serum total cholesterol (TC), high density lipoprotein cholesterol (HDL-c), low density lipoprotein cholesterol (LDL-c), and triglycerides (TG) were measured on the automated chemistry analyser (Roche Diagnostics, COBAS INTEGRA 400 Plus, USA). Non-HDL was calculated as Non-HDL = total cholesterol-HDL. Coronary risk ratio and very low density lipoprotein (VLDL) cholesterol were calculated on the automated chemistry analyser. Various medications utilised by the T2DM patients at the clinic are shown in Fig. 1.
Fig. 1.
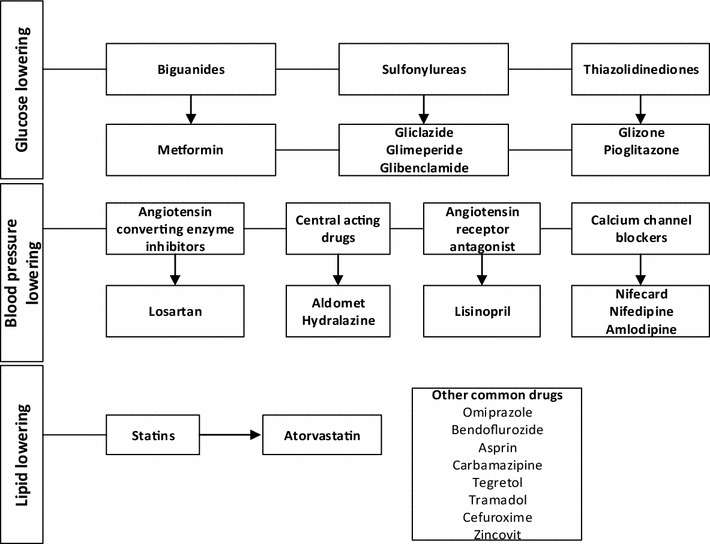
Category of medications utilised by T2DM patients
Definition of terms
High plasma glucose; FBG >7 mmol/L, HbA1c >7.2% [28].
Normal BP; 140/90 mmHg, high SBP >140 mmHg, high DBP >90 mmHg [29].
Dyslipidaemia: waist circumference ≥102 cm (males), ≥88 cm (females), WHR >90 (men) and 0.85 (female). High TG ≥1.7 mmol/l, HDL-C <1.0 (male), 1.03 (female), high LDL-C ≥2.59 mmol/l, high total cholesterol ≥5.18 mmol/l, high non-HDL ≥3.37 mmol/l [30].
Statistical analysis
Normality distribution was checked by the Shapiro–Wilk test. All continuous data was recorded as mean ± standard deviation and as frequency (percentages) for categorical variables. Between group comparisons for continuous variables were performed using student t-tests, and intergroup comparisons of categorical variables were performed using Chi square tests. Association between categorical variables and FBG or HbA1c were performed using logistic regression models and odds ratios (ORs) at 95% confidence intervals (95% CI) were recorded. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), version 22. A p < 0.05 was considered significant.
Results
Among the study population, the male to female ratio was 99/142 at baseline and 66/94 at follow up respectively. BMI and WHR of participants did not significantly differ from baseline to follow up [i.e. (p = 0.172) and (p = 0.276) respectively]. However, there was a significant difference in levels of physical activity from baseline to 6-month follow up (p = 0.0001) (Table 1).
Table 1.
Socio-demographic characteristics of study participants: Baseline and follow up
| Variable | Total | Baseline (n = 240) | Follow up (n = 160) | X2, df | p value |
|---|---|---|---|---|---|
| Age (years) | 57.80 ± 10.63 | 57.82 ± 10.88 | 57.79 ± 10.39 | 0.370t | 0.981 |
| Male:female ratio | 165/236 | 99/142 | 66/94 | ||
| BMI (Kg/m2) | 26.80 ± 9.44 | 26.13 ± 5.11 | 27.47 ± 13.78 | 1.367t | 0.172 |
| WHR | 0.93 ± 0.05 | 0.93 ± 0.06 | 0.92 ± 0.05 | 1.090t | 0.276 |
| Marital status | 17.5, 3 | 0.002 | |||
| Married | 269 (67.1) | 164 (68.0) | 105 (65.6) | ||
| Never married | 6 (1.5) | 4 (1.7) | 2 (1.3) | ||
| Divorced | 41 (10.2) | 25 (10.4) | 16 (10.0) | ||
| Widowed | 85 (21.2) | 48 (19.9) | 37 (23.1) | ||
| Education | 3.01, 4 | 0.55 | |||
| Tertiary | 58 (14.5) | 36 (14.9) | 22 (13.8) | ||
| Senior high school | 104 (25.9) | 57 (23.7) | 47 (29.4) | ||
| Junior high school | 133 (33.2) | 78 (32.4) | 55 (34.4) | ||
| Lower primary | 43 (10.7) | 28 (11.6) | 15 (9.4) | ||
| No formal education | 63 (15.7) | 42 (17.4) | 21 (13.1) | ||
| Occupation | 39.65, 3 | 0.0001 | |||
| Employed | 229 (57.1) | 133 (55.2) | 96 (60.0) | ||
| Retired | 85 (21.2) | 35 (14.5) | 50 (31.1) | ||
| Unemployed | 65 (16.2) | 51 (21.1) | 14 (8.8) | ||
| Informal employment | 22 (5.5) | 21 (9.0) | 1 (1) | ||
| Physical activity | 25.22, 1 | 0.0001 | |||
| Primarily sedentary | 101 (25.2) | 79 (32.8) | 22 (13.8) | ||
| Moderate activity | 300 (74.6) | 162 (67.2) | 138 (85.5) | ||
Values are presented as frequency (percentage); mean ± SD
tt-test value
The majority of the study participants were aged 51–60 years [81 (33.6%) vs 55 (34.4%)] while the lowest age range was 31–40 years [14 (5.8%) vs 10 (6.3%)] (Table 2). The severity and mean levels of the measured parameters were not significantly different from baseline to follow-up; [SBP (p = 0.474 and p = 0.600), DBP (p = 0.382 and p = 0.620), FBG (p = 0.364 and p = 0.940), TC (p = 0.328 and p = 0.160), non-HDL (p = 0.270 and p = 0.250) and LDL-c (p = 0.092 and p = 0.430)]. However, there was a difference in the severity and mean levels of HbA1c [(p = 0.004 and p = 0.0001)], TG [(p = 0.006 and p = 0.0001)] and HDL-c [(p < 0.0001 and p = 0.0001)] from baseline to follow up (Table 2).
Table 2.
Distribution of clinical characteristics among study participants
| Variables | Total | Baseline (n = 241) | Follow-up (n = 160) | X2, df | p value |
|---|---|---|---|---|---|
| Age | 0.909, 4 | 1.000 | |||
| 31–40 | 24 (6.0) | 14 (5.8) | 10 (6.3) | ||
| 41–50 | 76 (19.0) | 49 (20.3) | 27 (16.9) | ||
| 51–60 | 136 (33.9) | 81 (33.6) | 55 (34.4) | ||
| 61–70 | 118 (29.4) | 68 (28.2) | 50 (31.3) | ||
| 71–80 | 47 (11.7) | 29 (12.0) | 18 (11.3) | ||
| BMI | 3.386, 3 | 0.336 | |||
| Underweight | 11 (2.8) | 9 (3.80) | 2 (1.30) | ||
| Normal weight | 175 (43.9) | 170 (44.6) | 68 (42.8) | ||
| Overweight | 132 (33.10) | 80 (33.3) | 52 (32.7) | ||
| Obese | 81 (20.3) | 44 (18.3) | 37 (23.3) | ||
| SBP | 0.028, 1 | 0.474 | |||
| Normal | 121 (55.1) | 132 (54.8) | 89 (55.6) | ||
| High | 180 (44.9) | 109 (45.2) | 71 (44.4) | ||
| DBP | 0.178, 1 | 0.382 | |||
| Normal | 298 (74.5) | 177 (73.8) | 121 (75.6) | ||
| High | 102 (25.5) | 63 (26.3) | 39 (24.4) | ||
| HbA1c | 7.280, 1 | 0.004 | |||
| Normal | 104 (26.0) | 74 (30.8) | 30 (18.8) | ||
| High | 296 (74.0) | 166 (69.2) | 130 (81.3) | ||
| FPG | 0.202, 1 | 0.364 | |||
| Normal | 160 (39.9) | 94 (39.0) | 66 (41.3) | ||
| High | 241 (60.1) | 147 (61.0) | 94 (58.8) | ||
| TG | 6.679, 1 | 0.006 | |||
| Good | 343 (86.2) | 199 (82.6) | 144 (91.7) | ||
| High | 55 (13.8) | 42 (17.4) | 13 (8.3) | ||
| TC | 0.308, 1 | 0.328 | |||
| Good | 259 (65.2) | 154 (64.2) | 105 (66.9) | ||
| High | 138 (34.8) | 86 (35.8) | 52 (33.1) | ||
| HDL | 94.80, 1 | <0.0001 | |||
| Good | 235 (59.0) | 189 (78.4) | 46 (29.3) | ||
| Low | 163 (41.0) | 52 (21.6) | 111 (70.7) | ||
| NonHDL | 0.474, 1 | 0.270 | |||
| Normal | 188 (47.4) | 117 (48.8) | 71 (45.2) | ||
| High | 209 (52.6) | 123 (51.3) | 86 (54.8) | ||
| LDL | 2.040, 1 | 0.092 | |||
| Good | 164 (41.3) | 106 (44.2) | 58 (36.9) | ||
| High | 233 (58.7) | 134 (55.8) | 99 (63.1) | ||
| SBP (mmHg) | 140.06 ± 24.09 | 139.41 ± 24.31 | 140.71 ± 23.88 | 0.525t | 0.600 |
| DBP (mmHg) | 81.96 ± 13.18 | 81.63 ± 13.71 | 82.28 ± 12.65 | 0.484t | 0.620 |
| FBS (mmol/l) | 18.32 ± 4.31 | 9.18 ± 4.42 | 9.14 ± 4.20 | 0.082t | 0.940 |
| HbA1c (mmol/l) | 8.79 ± 2.49 | 8.27 ± 2.10 | 9.32 ± 2.88 | 4.201t | 0.0001 |
| TC (mmol/l) | 4.63 ± 1.27 | 4.73 ± 1.27 | 4.54 ± 1.27 | 1.406t | 0.160 |
| TG (mmol/l) | 1.17 ± 0.56 | 1.27 ± 0.57 | 1.07 ± 0.56 | 3.520t | 0.0001 |
| HDL-c (mmol/l) | 1.19 ± 1.19 | 1.35 ± 1.35 | 1.03 ± 1.03 | 9.960t | 0.0001 |
| Non-HDL-c (mmol/l) | 3.44 ± 1.22 | 3.37 ± 1.24 | 3.52 ± 1.20 | 1.142t | 0.250 |
| LDL-c (mmol/l) | 2.91 ± 0.57 | 2.79 ± 1.16 | 3.03 ± 1.13 | 2.029t | 0.430 |
| Coronary risk | 5.00 ± 2.7 | 4.97 ± 1.52 | 5.04 ± 3.88 | 0.232t | 0.820 |
| VLDL-c (mmol/l) | 0.54 ± 0.33 | 0.58 ± 0.26 | 0.51 ± 0.41 | 1.965t | 0.500 |
After adjusting for age and medication use, high BMI, SBP, DBP, TC, TG, HDL, non-HDL-c, and LDL-c status were not significant independent risk factors for high FBG in both baseline and follow up groups (p > 0.05) (Table 3). Similarly, in the logistic regression model, increased SBP, DBP, TC and non-HDL were slightly associated with high HbA1c levels at both baseline and follow up but not significantly (p > 0.05) (Table 4).
Table 3.
Association between metabolic risk factors and FBG levels at baseline and follow up
| Variables | FBG (baseline) | X2, df (p value) | p value | FBG (follow up) | X2, df (p value) | p value | ||
|---|---|---|---|---|---|---|---|---|
| High (n = 147) | Normal (n = 94) | aOR (95% CI) | High (n = 94) | Normal (n = 66) | aOR (95% CI) | |||
| Gender | 1.38, 1 (0.239) | 3.55, 1 (0.06) | ||||||
| Male | 56 (38.1) | 43 (45.7) | 1.0# | 33 (35.1) | 33 (50.0) | 1.0# | ||
| Female | 91 (61.9) | 51 (54.3) | 1.37 (0.81–2.32) | 0.283 | 61 (64.9) | 33 (50.0) | 1.85 (0.97–3.51) | 0.073 |
| BMI | 2.18, 3 (0.537) | 1.77, 3 (0.622) | ||||||
| Underweight | 6 (4.1) | 3 (3.2) | 1.05 (0.25–4.47) | 1.000 | 2 (2.1) | 1 (1.5) | 1.40 (0.12–16.21) | 1.000 |
| Normal | 70 (47.9) | 37 (39.4) | 1.0# | 40 (42.6) | 28 (43.1) | 1.0# | ||
| Overweight | 46 (31.5) | 34 (36.2) | 0.72 (0.39–1.29) | 0.289 | 29 (30.9) | 23 (35.4) | 0.88 (0.43–1.83) | 0.852 |
| Obese | 24 (16.4) | 20 (21.3) | 0.63 (0.31–1.30) | 0.268 | 23 (24.5) | 14 (21.5) | 1.15 (0.51–2.62) | 0.836 |
| SBP | 0.87, 1 (0.351) | 1.13, 1(0.288) | ||||||
| Normal | 77 (52.4) | 55 (58.5) | 1.0# | 49 (52.1) | 40 (60.6) | 1.0# | ||
| High | 70 (47.6) | 39 (41.5) | 1.28 (0.76–2.16) | 0.357 | 45 (47.9) | 26 (39.4) | 1.41 (0.75–2.68) | 0.333 |
| DBP | 0.02, 1 (0.901) | 2.34, 1(0.126) | ||||||
| Normal | 108 (73.5) | 69 (74.2) | 1.0# | 67 (73.1) | 54 (81.8) | 1.0# | ||
| High | 39 (26.5) | 24 (25.8) | 1.04 (0.57–1.88) | 1.000 | 27 (28.7) | 12 (18.2) | 1.81 (0.84–3.91) | 0.139 |
| TC | 0.22, 1 (0.642) | 0.09, 1 (0.764) | ||||||
| Good | 92 (63.0) | 62 (66.0) | 1.0# | 62 (66.0) | 43 (68.3) | 1.0# | ||
| High | 54 (37.0) | 32 (34.0) | 1.14 (0.67–1.96) | 0.681 | 32 (34.0) | 20 (31.7) | 1.11 (0.56–2.19) | 0.863 |
| TG | 0.23, 1(0.630) | 0.52,1 (0.472) | ||||||
| Good | 120 (81.6) | 79 (84.0) | 1.0# | 85 (90.4) | 59 (93.7) | 1.0# | ||
| High | 27 (18.4) | 15 (16.0) | 1.19 (0.59–2.37) | 0.729 | 9 (9.6) | 4 (6.3) | 1.56 (0.46–5.31) | 0.565 |
| HDL-c | 0.01, 1(0.928) | 0.83,1 (0.363) | ||||||
| Good | 115 (78.2) | 74 (78.7) | 1.0# | 25 (26.6) | 21 (33.3) | 1.0# | ||
| Low | 32 (21.8) | 20 (21.30) | 1.03(0.55–1.93) | 1.000 | 69 (73.4) | 42 (66.7) | 1.38 (0.69–2.77) | 0.377 |
| Non-HDL | 0.05, 1 (0.827) | 0.24,1 (0.621) | ||||||
| Normal | 72 (49.3) | 45 (47.5) | 1.0# | 41 (43.6) | 30 (47.6) | 1.0# | ||
| High | 74 (50.7) | 49 (52.1) | 0.94 (0.56–1.59) | 0.895 | 53 (56.4) | 33 (52.4) | 1.18 (0.62–2.23) | 0.628 |
| LDL-c | 0.88, 1 (0.349) | 0.84,1 (0.358) | ||||||
| Good | 68 (46.6) | 38 (40.4) | 1.0# | 32 (34.0) | 26 (41.3) | 1.0# | ||
| High | 78 (53.4) | 56 (59.6) | 0.78 (0.46–1.32) | 0.355 | 62 (66.0) | 37 (58.7) | 1.36 (0.71–2.63) | 0.401 |
Logistic regression model, adjusted for age and medication. 1.0#: reference point for odds ratio
X 2, df Chi square value, degrees of freedom, aOR adjusted odds ratio, CI confidence interval
Table 4.
Association between metabolic risk factors and HbA1c levels at baseline and follow up
| Variables | HbA1c (baseline) | X2, df (p value) | p value | HbA1c (follow-up) | X2, df (p value) | p value | ||
|---|---|---|---|---|---|---|---|---|
| Poor (n = 167) | Good (n = 74) | aOR (95% CI) | Poor (n = 130) | Good (n = 30) | aOR (95% CI) | |||
| Gender | 0.18, 1 (0.675) | 0.96, 1 (0.328) | ||||||
| Male | 67 (40.4) | 32 (43.2) | 1.0# | 56 (43.1) | 10 (33.3) | 1.0# | ||
| Female | 99 (59.6) | 42 (56.8) | 1.13 (0.65–1.96) | 0.673 | 74 (56.9) | 20 (66.7) | 0.66 (0.29–1.52) | 0.413 |
| BMI | 1.35, 3 (0.718) | 4.38, 3 (0.224) | ||||||
| Underweight | 5 (3.0) | 4 (5.4) | 0.49 (0.12–1.94) | 0.445 | 2 (1.6) | 0 (0.0) | ||
| Normal | 77 (46.7) | 30 (40.5) | 1.0# | 56 (43.4) | 12 (40.0) | 1.0# | ||
| Overweight | 53 (32.1) | 26 (35.1) | 0.79 (0.42–1.49) | 0.519 | 45 (34.90 | 7 (23.3) | 1.38 (0.50–3.78) | 0.619 |
| Obese | 30 (18.2) | 14 (18.9) | 0.83 (0.39–1.79) | 0.695 | 26 (20.2) | 11 (36.7) | 0.50 (0.19–1.29) | 0.216 |
| SBP | 2.22,1 (0.136) | 0.47, 1(0.491) | ||||||
| Normal | 86 (51.8) | 46 (62.2) | 1.0# | 74 (56.9) | 15 (50.0) | 1.0# | ||
| High SBP | 80 (48.2) | 28 (37.8) | 1.53 (0.87–2.68) | 0.161 | 56 (43.1) | 15 (50.0) | 0.76 (0.34–1.68) | 0.544 |
| DBP | 0.16, 1 (0.692) | 0.022, 1 (0.883) | ||||||
| Normal | 121 (72.9) | 55 (75.3) | 1.0# | 98 (75.4) | 23 (76.7) | 1.0# | ||
| High DBP | 45 (27.1) | 18 (24.7) | 1.14 (0.60–2.14) | 0.752 | 32 (24.6) | 7 (23.3) | 1.07 (0.42–2.73) | 1.000 |
| TC | 2.42, 1 (0.12) | 0.49, 1 (0.483) | ||||||
| Good | 101 (61.2) | 53 (71.6) | 1.0# | 84 (65.6) | 21 (72.4) | 1.0# | ||
| High | 64 (38.8) | 21 (28.4) | 1.60 (0.88–2.89) | 0.144 | 44 (34.4) | 8 (27.6) | 1.38 (0.56–3.36) | 0.522 |
| TG | 0.00, 1 (0.985) | 1.42, 1 (0.233) | ||||||
| Good | 137 (82.5) | 61 (82.4) | 1.0# | 119 (93.0) | 25 (86.2) | 1.0# | ||
| High | 29 (17.5) | 13 (17.6) | 0.99 (0.48–2.04) | 1.000 | 9 (7.0) | 4 (13.8) | 0.47 (0.14–1.68) | 0.262 |
| HDL-c | 0.11, 1 (0.743) | 0.46, 1 (0.499) | ||||||
| Good | 132 (79.0) | 57 (77.0) | 1.0# | 39 (30.5) | 7 (24.1) | 1.0# | ||
| Low | 35 (21.0) | 17 (23.0) | 0.90 (0.46–1.73) | 0.737 | 89 (69.5) | 22 (75.9) | 0.73 (0.29–1.84) | 0.652 |
| Non-HDL | 0.25, 1 (0.620) | 0.002, 1 (0.962) | ||||||
| Normal | 79 (47.9) | 38 (51.4) | 1.0# | 58 (45.3) | 13 (44.8) | 1.0# | ||
| High | 86 (52.1) | 36 (48.6) | 1.15 (0.66–1.99) | 0.675 | 70 (54.7) | 16 (55.2) | 0.98 (0.44–2.21) | 1.000 |
| LDL-c | 0.05,1 (0.817) | 0.53,1 (0.465) | ||||||
| Good | 74 (44.8) | 32 (43.2) | 1.0# | 49 (38.3) | 9 (31.0) | 1.0# | ||
| High | 91 (55.2) | 42 (56.8) | 0.94 (0.54–1.630 | 0.888 | 79 (61.7) | 20 (69.0) | 0.73 (0.31–1.72) | 0.528 |
Logistic regression model, adjusted for age and medication. 1.0#: reference point for odds ratio
X 2, df Chi square value, degrees of freedom, aOR adjusted odds ratio, CI confidence interval
From baseline to follow up, FBG levels increased by 25.0% when (BIG) was administered alone. In a combination therapy with either SUA or TNZ, there was only a decrease in FBG levels by 1% (p = 0.9924) and 1.6% (p = 0.1098) respectively. However, FBG levels decreased by 15.8% when all three medications; BIG, SUA and TNZ were administered (p = 0.216). Meanwhile, levels of HbA1c were increased by 29.6% after BIG treatment alone (p = 0.0094), increased by 19.2% and 16.7% when BIG was combined with SUA (p = 0.0175) and TNZ (p = 0.0903) respectively. However, a multiple therapy of BIG, SUA and TNZ resulted in only a 1.3% increase of HbA1c levels (p = 0.8308) (Table 5).
Table 5.
Utilisation of glucose lowering medications among T2DM patients
| Baseline | Follow up | Mean difference (95% CI) | p value | % effect | |
|---|---|---|---|---|---|
| Treatment | |||||
| FBG (mmol/l) | |||||
| BIG only | 8.02 ± 0.65 | 10.08 ± 1.12 | 2.05 (−1.25 to 5.36) | 0.2162 | 25.00 |
| BIG + SUA | 8.45 ± 0.49 | 8.441 ± 0.82 | −0.01 (−1.83 to 1.82) | 0.9924 | −0.10 |
| BIG + TNZ | 9.63 ± 0.59 | 11.88 ± 1.47 | 2.25 (−0.52 to 5.02) | 0.1098 | 23.40 |
| BIG + SUA + TNZ | 9.921 ± 0.66 | 8.36 ± 1.04 | −1.57 (−4.06 to 0.93) | 0.216 | −15.80 |
| HbA1c (%) | |||||
| BIG only | 7.34 ± 0.28 | 9.51 ± 1.10 | 2.17 (0.57 to 3.78) | 0.0094 | 29.60 |
| BIG + SUA | 8.11 ± 0.32 | 9.67 ± 0.65 | 1.55 (0.28 to 2.83) | 0.0175 | 19.20 |
| BIG + TNZ | 8.68 ± 0.33 | 10.12 ± 1.04 | 1.45 (−0.23 to 3.14) | 0.0903 | 16.70 |
| BIG + Sul + TNZ | 8.46 ± 0.26 | 8.57 ± 0.47 | 0.11 (−0.91 to 1.12) | 0.8308 | 1.30 |
BIG Biguanide, SUA Sulfonylurea, TNZ Thiazolidinedione
p < 0.05 is considered significant
There was a mean percentage decrease effect in levels of HDL-c (p < 0.0001), TG (p = 0.0259) and VLDL-c (p = 0.0237) by 22.8%, 18.4% and 17.3% respectively, after atorvastatin treatment alone. Conversely, there was an increased effect in levels of TC (p = 0.743) by 1.7%, non-HDL-c (p = 0.075) by 14.5%, LDL-c (p = 0.022) by 21.5% and CR (p = 0.955) by 0.5% after atorvastatin treatment (Table 6).
Table 6.
Utilisation of lipid lowering medications among T2DM patients
| Variable | Baseline | Follow up | Mean difference (95% CI) | p value | % difference |
|---|---|---|---|---|---|
| TC (mmol/l) | |||||
| No statin | 5.03 ± 0.12 | 4.95 ± 0.13 | −0.07 (−0.42 to 0.28) | 0.6817 | 1.39 |
| Atorvastatin | 4.06 ± 0.16 | 4.13 ± 0.16 | 0.07 (−0.37 to 0.51) | 0.7434 | 1.72 |
| TG (mmol/l) | |||||
| No statin | 1.32 ± 0.06 | 1.19 ± 0.06 | −0.13 (−0.30 to 0.04) | 0.1322 | 9.85 |
| Atorvastatin | 1.14 ± 0.06 | 0.93 ± 0.06 | −0.21 (−0.39 to −0.03) | 0.0259 | 18.42 |
| HDL-c (mmol/l) | |||||
| No statin | 1.36 ± 0.03 | 1.05 ± 0.03 | −0.30 (−0.39 to −0.21) | <0.0001 | 22.06 |
| Atorvastatin | 1.36 ± 0.04 | 1.04 ± 0.04 | −0.31 (−0.42 to −0.19) | <0.0001 | 22.79 |
| Non-HDL (mmol/l) | |||||
| No statin | 3.67 ± 0.11 | 3.89 ± 0.12 | 0.23 (−0.09 to 0.55) | 0.1617 | 6.27 |
| Atorvastatin | 2.69 ± 0.15 | 3.09 ± 0.15 | 0.39 (−0.04 to 0.81) | 0.0754 | 14.50 |
| LDL-c (mmol/l) | |||||
| No statin | 3.06 ± 0.11 | 3.36 ± 0.11 | 0.30 (−0.01 to 0.60) | 0.058 | 9.80 |
| Atorvastatin | 2.19 ± 0.15 | 2.68 ± 0.14 | 0.47 (0.06 to 0.87) | 0.022 | 21.46 |
| CR | |||||
| No statin | 5.24 ± 0.15 | 5.57 ± 0.49 | 0.33 (−0.68 to 1.34) | 0.5202 | 6.29 |
| Atorvastatin | 4.31 ± 0.19 | 4.32 ± 0.20 | 0.02 (−0.53 to 0.57) | 0.9547 | 0.46 |
| VLDL-c (mmol/l) | |||||
| No statin | 0.60 ± 0.03 | 0.58 ± 0.05 | −0.01 (−0.12 to 0.09) | 0.8181 | 1.67 |
| Atorvastatin | 0.52 ± 0.03 | 0.42 ± 0.03 | −0.09 (−0.18 to −0.01) | 0.0237 | 17.3 |
CI confidence interval
p < 0.05 is considered significant
For non-hypertensive T2DM participants, there was no significant change in SBP and DBP from baseline to follow up (Table 7). SBP levels were reduced by 0.1% after CCB + ACEI treatment (p = 0.969). Levels of both SBP and DBP were reduced by 1.9% (p = 0.644) and 5.8% (p = 0.128) respectively after ACEI treatment alone and decreased by 1.0% (p = 0.835) and 0.1% (p = 0.912) respectively after CCB + ARB combination therapies. However, levels of both SBP and DBP increased by 3.0% (p = 0.683) and 0.4% (p = 0.942) respectively after CCB treatment alone and increased by 17.3% (p = 0.061) and 11.3% (p = 0.086) respectively after CAD treatment alone, while a combination therapy of CCB + ACEI increased DBP by 1.9% (p = 0.666) (Table 7).
Table 7.
Utilisation of anti-hypertensive medicines among T2DM patients
| Anti-hypertensive drugs | Baseline | Follow up | Mean difference (95%CI) | p value | %effect |
|---|---|---|---|---|---|
| SBP (mmHg) | |||||
| DM only (n = 38) | 127.1 ± 4.09 | 130.5 ± 3.45 | 3.34 (−7.33 to 14.01) | 0.534 | 2.63 |
| DM + HPT | |||||
| CCB (n = 11) | 150.2 ± 7.99 | 154.6 ± 7.21 | 4.46 (−18.02 to 26.92) | 0.683 | 2.96 |
| ARB (n = 22) | 130.1 ± 3.04 | 130.0 ± 4.36 | 0.01 (−10.74 to 10.74) | >0.999 | 0.00 |
| ACEI (n = 30) | 130.4 ± 3.93 | 128.0 ± 3.59 | −2.47 (−13.12 to 8.19) | 0.644 | −1.90 |
| CAD (n = 8) | 150.6 ± 9.07 | 176.6 ± 8.33 | 26.0 (−2.43 to 54.43) | 0.061 | 17.30 |
| CCB + ARB (n = 24) | 153.3 ± 5.74 | 151.7 ± 4.98 | −1.58 (−16.88 to 13.72) | 0.835 | 1.03 |
| CCB + ACEI (n = 27) | 143.1 ± 3.33 | 142.9 ± 3.46 | −0.19 (−9.83 to 9.46) | 0.969 | 0.13 |
| DBP (mmHg) | |||||
| DM only (n = 38) | 74.87 ± 2.25 | 77.87 ± 1.80 | 3.00 (−2.75 to 8.74) | 0.301 | 4.00 |
| DM + HPT | |||||
| CCB (n = 11) | 83.18 ± 3.74 | 83.55 ± 3.23 | 0.36 (−9.95 to 10.68) | 0.942 | 0.43 |
| ARB (n = 22) | 80.00 ± 2.31 | 80.02 ± 2.09 | 1.00 (−5.29 to 7.30) | 0.750 | 1.25 |
| ACEI (n = 30) | 80.01 ± 1.89 | 76.43 ± 2.37 | −4.67 (−10.73 to 1.40) | 0.128 | 5.76 |
| CAD (n = 8) | 93.80 ± 5.23 | 104.4 ± 7.22 | 10.6 (−9.96 to 31.16) | 0.086 | 11.30 |
| CCB + ARB (n = 24) | 86.13 ± 3.33 | 86.08 ± 2.62 | −0.04 (−8.58 to 8.50) | 0.992 | 0.05 |
| CCB + ACEI (n = 27) | 82.81 ± 2.78 | 84.41 ± 2.40 | 1.59 (−5.78 to 8.96) | 0.666 | 1.92 |
CCB calcium channel blockers, ACEI angiotensin converting enzyme inhibitors, ARB angiotensin II receptor blockers, CADcentral acting drugs
Discussion
The prevalence of T2DM has increased tremendously in the past few decades among different countries worldwide [2, 3, 31–34]. SSA remains one of the most affected regions due to rapid urbanisation and increased adoption of a westernised diet with less physical activity [5, 30–34].
In this hospital-based study, we examined the major factors that characterise T2DM and how these factors influence anti-diabetes medication response. As reported by Danquah et al. [5], the majority of T2DM patients in urban Ghana are middle aged, of low socio-economic status and their lifestyle is primarily sedentary [5]. Moreover, our findings on clinical parameters such as SBP, DBP, HDL-c, LDL-c, TG, TC and FBG are similar to those reported in their study [5].
Overall, several of these biomarkers are higher than the recommended threshold for T2DM as suggested by the WHO and the ADA [35, 36]. For example, approximately 60 and 69.2% of the participants were not able to achieve the desired FBG and HbA1c targets respectively. This is in fact disturbing given the direct association between abnormal plasma glucose levels and macrovascular or microvascular complications. Efforts to control glucose levels are necessary and could be achieved in several ways. After diagnosis, medical nutrition therapy (MNT) is necessary to reduce weight and normalise glucose levels [37].
However, it has been established that MNT alone is not sufficient for improving plasma glucose levels. As such, the use of medications becomes the next phase of action [37].
In Ghana, several glucose lowering medications have been approved for the treatment of hyperglycaemia including SUAs, TNZs and biguanides, the latter being the first line anti-diabetic medicine [5]. Like many other countries, its popularity is because: (1) it is less expensive, (2) it is effective for weight reduction and plasma glucose levels, and (3) it has a reduced risk for hypoglycaemia [38]. Not surprisingly, a high proportion of our participants (>80%) were on this medication, most of whom had used this drug for a period long before the start of this study. However, the majority of those who used BIG (metformin) alone could not achieve the desired glycaemic level even at follow up although there seems to be a minimal percentage effect (29.6%, p = 0.0094) on HbA1c level (Tables 3, 4, 5). This emphasises the failure of metformin as a monotherapy to achieve glucose control. At this point, the focus shifts towards individuals undergoing combination and multiple therapies.
SUAs and TNZs have been recognised as second line anti-diabetic medications and their efficacy is similar to metformin [25, 38]. However, it was apparent after six months that even with multiple therapies, the majority of the patients could not attain the desired glucose target levels. Only a minimal percentage effect of BIG + SUA (19.2%, p = 0.0175) on HbA1c was observed (Table 5). Several reasons can be attributed to this:
Firstly, there is a possibility of poor adherence to oral medications, especially among those taking combination and multiple therapies, not only for hyperglycaemia but also for other comorbidities [26, 38, 39]. Moreover, many of these drugs are associated with side effects and hence it is possible that some participants will be selective in their choice of medicine (Additional file 1: Table S1). In a study among 2849 T2DM patients in the UK, it was shown that only 13% of the patients adhered strictly to the drug regimen [40]. This could possibly be the case in our study as some participants may have become bored with swallowing different medications daily. Efforts to simplify treatment regimens should therefore be intensified. For example, instead of multiple medications, single-dose combination pills with minimal side effects could be administered. Secondly, ensuring adequate control of glycaemic status requires a paradigm shift from sedentary behaviour to a more physically active lifestyle. One study has shown that moderate-intensity physical activity such as brisk walking and reducing time spent watching television to less than 30 min per day could reduce several modifiable T2DM risk factors including plasma LDL-c and TG while increasing HDL-c [41]. A meta-analysis also showed that physical activity is inversely associated with risk for T2DM [42].
Moreover, intense exercise is necessary to stimulate 5-adenosine monophosphate-activated kinase (5-AMPK) causing the release of glucose to the muscles rather than it accumulating in the plasma [4]. In our study however, we were unable to assess the level or intensity of physical activity by the individuals. Therefore, an effective physical assessment tool such as the international physical activity questionnaire (IPAQ) could be useful [43].
Thirdly, poor dietary preferences may have been a contributory factor. Studies have shown that healthy diets or consumption of vegetables, low calorie diets, low trans fats, legumes, fruits, poultry, whole grains and cereal fibre is linked to a reduced risk of metabolic syndrome and T2DM [44, 45]. Conversely, consumption of red and processed meat, sugar-sweetened beverages, desserts and fried foods is associated with an increased risk of T2DM [44, 45]. However, whether or not the majority of the study participants utilised a particular food was unverified and therefore, a validated food frequency questionnaire would also have been useful.
Despite the increasing use of anti-hypertensives, BP control was suboptimal in our study population. With an attrition rate of nearly 40%, only 52 T2DM participants who took anti-hypertensive medications were able to maintain a target BP (both SBP and DBP) at follow up (Table 7). Majority were unable to achieve a desired target although they took more than one antihypertensive drug. This is disturbing given that high BP is by far the most critical risk factor for cardiovascular disease (CVD) and stroke [46]. Other studies that have explored the role of intensive BP control in preventing CVD have produced conflicting results. One study showed that a DBP of ≤80 mmHg could reduce the risk of CVD by 50% [47]. However, another study reported that SBP ≤120 mmHg was not associated with a reduced risk for CVD [48]. Notwithstanding this, our findings agree with several other studies that BP is poorly controlled among T2DM patients worldwide [49, 50].
Statins are well-known lipid lowering medications and the common one used by participants in this study is atorvastatin. More than half of the participants taking atorvastatin had good lipid profiles and this is consistent with the findings by Wong et al. [39]. Moreover, our study showed that there was a significant improvement in several lipid markers such as TG, LDL-c, HDL-c and VDL-c at follow up (Table 6). Whether atorvastatin interfered with glucose homeostasis is yet to be determined but our study confirms that atorvastatin is a potent drug for treating dyslipidaemia.
The present study does have some limitations. Firstly, because it was an observational longitudinal study, it was limited by confounding factors such as differences in dosage regimen. Dosage regimen refers to the modality of drug administration/doses per unit of time to reach a therapeutic objective. This comprises the time or frequency when the drug should be administered, the time between doses and the amount or unit dose of medicine to be administered at a specific time [51–53]. However, given the number of participants, each with a different medication dosage at a point in time, it was difficult to take into consideration the dosage regimen. At the same time, certain tests especially FBG are influenced by biological variation even when fluoride tubes are used. For example, stressful situations in the hours preceding FBG test could increase FBG levels [54]. Thus, we were unable to provide a full explanation on the poor drug response among some participants. Secondly, a clinical randomised control trial would have eliminated potential confounding factors, and also shed further light on the effect of the various medications in lowering modifiable risk factors. Thirdly, the sample size of the study was small and therefore cannot be representative of the entire T2DM population. Finally, over 40% of the participants were lost to follow up and this may have had an effect on our assessments.
Conclusion
Our study showed that the use of statins is effective for improving lipid profiles and can be regarded as a potent medication for treating dyslipidaemia. However, utilisation of oral hypoglycaemic agents whether as a monotherapy, combination or polytherapy was not effective for achieving plasma glucose targets of <7%. This is alarming and therefore, alternative approaches including a less sedentary lifestyle while engaging in vigorous exercise may reduce weight and obesity; enforcing healthy eating practices and administration of single/fixed-dose combination tablets or pills with minimal side effects may improve medication adherence (Additional file 1: Table S1).
Authors’ contributions
EA and WW conceived the study; the latter designed the questionnaire. EA was involved in data collection, design and drafted the manuscript. KF and WW participated in the design and coordination of the study. EA, SAS, FAY, AD and EOA were involved in biochemical analysis. EOA and EA performed the statistical analysis. PR revised the manuscript for intellectual content. All authors read and approved the final manuscript.
Acknowledgements
The authors wish to thank the laboratory personnel at the Department of Biochemistry at KATH for allowing the use of their automated chemistry machine for analysing the clinical data.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All relevant data on which conclusions were made are included in the manuscripts.
Ethics approval and consent to participate
The Committee on Human Research, Publication and Ethics (CHRPE), Kwame Nkrumah University of Science and Technology (KNUST), Kumasi and the Human Research Ethics Committee (HREC), Edith Cowan University (ECU), Australia granted ethical approval for this study. Written informed consent was obtained from each participant.
Funding
This work was partially supported by Australia-China International Collaborative Grant (NH&MRC-APP1112767-NSFC81561128020).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- BIG
biguanide
- SUA
sulfonylurea
- TNZ
thiazolidinedione
- ACEI
angiotensin converting enzyme inhibitor
- CCB
calcium channel blocker
- ARB
angiotensin II receptor blocker
- CAD
central acting drug
- T2DM
type II diabetes mellitus
Additional file
Additional file 1: Table S1. Morisky adherence scale-8 (MMAS-8).
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s40169-017-0162-5) contains supplementary material, which is available to authorized users.
Contributor Information
Eric Adua, Email: eadua@our.ecu.edu.au.
Peter Roberts, Email: p.roberts@ecu.edu.au.
Samuel Asamoah Sakyi, Email: sasakyi.chs@knust.edu.gh.
Francis Agyemang Yeboah, Email: fayeboah.sms@knust.edu.gh.
Albert Dompreh, Email: adompreh@gmail.com.
Kwasi Frimpong, Email: frimpongk@hotmail.com.
Enoch Odame Anto, Email: eanto@our.ecu.edu.au.
Wei Wang, Phone: +61 (0) 418469913, Email: wei.wang@ecu.edu.au.
References
- 1.Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, Rastas M. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation: IDF Diabetes Atlas 2015. http://www.diabetesatlas.org/resources/2015-atlas.html. Accessed 04 Oct 2016
- 3.The World Health Organisation: The Diabetes epidemiology 2014. http://www.who.int/mediacentre/factsheets/fs312/en/accessed. Accessed 14 Feb 2015
- 4.Epstein FH, Shepherd PR, Kahn BB. Glucose transporters and insulin action—implications for insulin resistance and diabetes mellitus. N Engl J Med. 1999;341(4):248–257. doi: 10.1056/NEJM199907223410406. [DOI] [PubMed] [Google Scholar]
- 5.Danquah I, Bedu-Addo G, Terpe KJ, Micah F, Amoako YA, Awuku YA, Mockenhaupt FP. Diabetes mellitus type 2 in urban Ghana: characteristics and associated factors. BMC Public Health. 2012;12(210):1–8. doi: 10.1186/1471-2458-12-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herder C, Karakas M, Koenig W. Biomarkers for the prediction of type 2 diabetes and cardiovascular disease. Clin Pharmacol Ther. 2011;90(1):52–66. doi: 10.1038/clpt.2011.93. [DOI] [PubMed] [Google Scholar]
- 7.Resnick HE, Howard BV. Diabetes and cardiovascular disease. Ann Rev Med. 2002;53(1):245–267. doi: 10.1146/annurev.med.53.082901.103904. [DOI] [PubMed] [Google Scholar]
- 8.Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ. Diabetic foot syndrome. Diabetes Care. 2003;26(5):1435–1438. doi: 10.2337/diacare.26.5.1435. [DOI] [PubMed] [Google Scholar]
- 9.Holt RI, De Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 2014;14(6):1–9. doi: 10.1007/s11892-014-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campayo A, Gómez-Biel CH, Lobo A. Diabetes and depression. Curr Psychiatry Rep. 2011;13(1):26–30. doi: 10.1007/s11920-010-0165-z. [DOI] [PubMed] [Google Scholar]
- 11.Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biessels GJ, Koffeman A, Scheltens P. Diabetes and cognitive impairment. J Neurol. 2006;253(4):477–482. doi: 10.1007/s00415-005-0036-4. [DOI] [PubMed] [Google Scholar]
- 13.Zilliox LA, Chadrasekaran K, Kwan JY, Russell JW. Diabetes and cognitive impairment. Curr Diab Rep. 2016;16(9):87. doi: 10.1007/s11892-016-0775-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luchsinger JA. Type 2 diabetes and cognitive impairment: linking mechanisms. J Alzheimers Dis. 2012;30(s2):S185–S198. doi: 10.3233/JAD-2012-111433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerstein H, Pogue J, Mann J, Lonn E, Dagenais G, McQueen M, Yusuf S. The relationship between dysglycaemia and cardiovascular and renal risk in diabetic and non-diabetic participants in the HOPE study: a prospective epidemiological analysis. Diabetologia. 2005;48(9):1749–1755. doi: 10.1007/s00125-005-1858-4. [DOI] [PubMed] [Google Scholar]
- 17.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441–447. doi: 10.1016/j.pcad.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myers J, McAuley P, Lavie CJ, Despres JP, Arena R, Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog Cardiovasc Dis. 2015;57(4):306–314. doi: 10.1016/j.pcad.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Reitz C, Tang MX, Manly J, Mayeux R, Luchsinger JA. Hypertension and the risk of mild cognitive impairment. Arch Neurol. 2007;64(12):1734–1740. doi: 10.1001/archneur.64.12.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaes B, Beke E, Truyers C, Elli S, Buntinx F, Verbakel JY, Van Pottelbergh G. The correlation between blood pressure and kidney function decline in older people: a registry-based cohort study. BMJ. 2015;5(6):e007571. doi: 10.1136/bmjopen-2015-007571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agarwal R, Andersen MJ. Correlates of systolic hypertension in patients with chronic kidney disease. Hypertension. 2005;46(3):514–520. doi: 10.1161/01.HYP.0000178102.85718.66. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Supplement 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B. Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy. Diabetologia. 2009;52(1):17–30. doi: 10.1007/s00125-008-1157-y. [DOI] [PubMed] [Google Scholar]
- 24.DeFronzo RA, Abdul-Ghani M. Type 2 diabetes can be prevented with early pharmacological intervention. Diabetes Care. 2011;34(Supplement 2):S202–S209. doi: 10.2337/dc11-s221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cox ME, Feinglos MN. Risk vs benefit in diabetes pharmacotherapy: a rational approach to choosing pharmacotherapy in type 2 diabetes. Curr Diab Rep. 2013;13(3):319–328. doi: 10.1007/s11892-013-0374-z. [DOI] [PubMed] [Google Scholar]
- 26.Wright EAS, Cuddihy R. In support of an early polypharmacy approach to the treatment of type 2 diabetes. Diabetes Obes Metab. 2010;12(11):929–940. doi: 10.1111/j.1463-1326.2010.01255.x. [DOI] [PubMed] [Google Scholar]
- 27.Okello S, Nasasira B, Muiru AN, Muyingo A. Validity and reliability of a self-reported measure of antihypertensive medication adherence in Uganda. PLoS ONE. 2016;11(7):e0158499. doi: 10.1371/journal.pone.0158499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. Report of a WHO consultation. 1999. http://www.staff.ncl.ac.uk/philip.home/who_dmg.pdf. Accessed 01 May 2017
- 29.World Health Organization Guidelines for the management of hypertension. Guidelines Subcommittee. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 30.Expert Panel on Detection. Treatment of High Blood Cholesterol In Adults Executive summary of the third report of The National Cholesterol Education Program. JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 31.Wang W. The global reach of family medicine and community health. Fam Med Community Health. 2016;4(3):2–3. doi: 10.15212/FMCH.2016.0116. [DOI] [Google Scholar]
- 32.Adua E, Frimpong K, Li X, Wang W. Emerging issues in public health: a perspective 5 on Ghana’s healthcare expenditure, policies and outcomes. EPMA J. 2017 doi: 10.1007/s13167-017-0109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Asweto CO, Alzain MA, Andrea S, Alexander R, Wang W. Integration of community health workers into health systems in developing countries: opportunities and challenges. Fam Med Community Health. 2016;14:37–45. doi: 10.15212/FMCH.2016.0102. [DOI] [Google Scholar]
- 34.Wang W. West meets east: Chinese and US doctors addressing the medical ecology and disease management from both countries’ perspectives. Fam Med Community Health. 2011;3:1–3. [Google Scholar]
- 35.American Diabetes Association Standards of medical care in diabetes-2015 summary of revisions. Diabetes Care. 2015;38:S11–S66. doi: 10.2337/dc14-2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organisation 2006. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. http://apps.who.int/iris/bitstream/10665/43588/1/9241594934_eng.pdf
- 37.Esposito K, Ciotola M, Maiorino MI, Giugliano D. Lifestyle approach for type 2 diabetes and metabolic syndrome. Curr Atheroscler Rep. 2008;10(6):523–528. doi: 10.1007/s11883-008-0081-4. [DOI] [PubMed] [Google Scholar]
- 38.Emslie-Smith A, Dowall J, Morris A. The problem of polypharmacy in type 2 diabetes. Br Diab Vasc Dis Res. 2003;3(1):54–56. doi: 10.1177/14746514030030010901. [DOI] [Google Scholar]
- 39.Wong HK, Ong KL, Cheung CL, Cheung BM. Utilization of glucose, blood pressure, and lipid lowering medications among people with type II diabetes in the United States, 1999–2010. Ann Epidemiol. 2014;24(7):516–521. doi: 10.1016/j.annepidem.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 40.Donnan P, MacDonald T, Morris A. Adherence to prescribed oral hypoglycaemic medication in a population of patients with Type 2 diabetes: a retrospective cohort study. Diab Med. 2002;19(4):279–284. doi: 10.1046/j.1464-5491.2002.00689.x. [DOI] [PubMed] [Google Scholar]
- 41.Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care. 2002;25(9):1612–1618. doi: 10.2337/diacare.25.9.1612. [DOI] [PubMed] [Google Scholar]
- 42.Aune D, Norat T, Leitzmann M, Tonstad S, Vatten LJ. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Epidemiol. 2015;30(7):529–542. doi: 10.1007/s10654-015-0056-z. [DOI] [PubMed] [Google Scholar]
- 43.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8(1):115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frank LK, Kröger J, Schulze MB, Bedu-Addo G, Mockenhaupt FP, Danquah I. Dietary patterns in urban Ghana and risk of type 2 diabetes. Br J Nutr. 2014;112(1):89–98. doi: 10.1017/S000711451400052X. [DOI] [PubMed] [Google Scholar]
- 45.InterAct Consortium Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetol. 2015;58(7):1394–1408. doi: 10.1007/s00125-015-3585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu JG, Zhou RR, Cai GJ. From hypertension to stroke: mechanisms and potential prevention strategies. CNS Neurosci Ther. 2011;17(5):577–584. doi: 10.1111/j.1755-5949.2011.00264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755–1762. doi: 10.1016/S0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 48.Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304(1):61–68. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Amer J Med. 2009;122(5):443–453. doi: 10.1016/j.amjmed.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 50.Kuznik A, Mardekian J. Trends in utilization of lipid-and blood pressure-lowering agents and goal attainment among the US diabetic population, 1999–2008. Cardiovasc Diabetol. 2011;10(1):31. doi: 10.1186/1475-2840-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23(8):1296–1310. doi: 10.1016/S0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 52.Patrick GL. An introduction to medicinal chemistry. 5. Oxford: Oxford University Press; 2013. pp. 153–178. [Google Scholar]
- 53.Ritschel WA, Kearns GL. Handbook of basic pharmacokinetics—including clinical applications. 5. Washington: American Pharmacists Association; 2009. pp. 9–89. [Google Scholar]
- 54.Bonora E, Tuomilehto J. The pros and cons of diagnosing diabetes with A1C. Diabetes Care. 2011;34(Supplement 2):S184–S190. doi: 10.2337/dc11-s216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data on which conclusions were made are included in the manuscripts.


