Abstract
Normal adult mammary stem cells (AMSCs) are promising sources for breast reconstruction, particularly following the resection of breast tumors. However, carcinogenic events can potentially convert normal AMSCs to cancer stem cells, posing a safety concern for the use of AMSCs for clinical tissue regeneration. In the present study, AMSCs and autologous primary breast cancer cells were isolated and compared for their ability to differentiate, their gene expression profile, and their potential to form tumors in vivo. AMSCs were isolated from normal tissue surrounding primary breast tumors by immunomagnetic sorting. The pluripotency of these cells was investigated by differentiation analysis, and gene expression profiles were compared with microarrays. Differentially expressed candidate genes were confirmed by reverse transcription-polymerase chain reaction and western blot analyses. The in vivo tumorigenicity of these cells, compared with low-malignancy MCF-7 cells, was also investigated by xenograft tumor formation analysis. The results revealed that AMSCs isolated from normal tissues surrounding primary breast tumors were positive for the stem cell markers epithelial-specific antigen and keratin-19. When stimulated with basic fibroblast growth factor, a differentiation agent, these AMSCs formed lobuloalveolar structures with myoepithelia that were positive for common acute lymphoblastic leukemia antigen. The gene expression profiles revealed that, compared with cancer cells, AMSCs expressed low levels of oncogenes, including MYC, RAS and ErbB receptor tyrosine kinase 2, and high levels of tumor suppressor genes, including RB transcriptional corepressor 1, phosphatase and tensin homolog, and cyclin-dependent kinase inhibitor 2A. When injected into nude non-obese diabetic/severe combined immunodeficiency-type mice, the AMSCs did not form tumors, and regular mammary ductal structures were generated. The AMSCs isolated from normal tissue adjacent to primary breast tumors had the normal phenotype of mammary stem cells, and therefore may be promising candidates for mammary reconstruction subsequent to breast tumor resection.
Keywords: adult mammary stem cells, breast reconstruction, cancer stem cells, epithelial-specific antigen, mastectomy, sialomucin
Introduction
Mastectomy may negatively affect the quality of life for women with breast cancer (1). As the psychological benefits of breast reconstruction are increasingly acknowledged, reconstruction has become an important part of the management of breast cancer. (2) There are generally two options for breast cancer reconstruction: The autologous option involves the transfer of tissues from other regions (donor sites) of the body to the chest wall, whereas the prosthetic option involves the placement of synthetic implants under the chest wall (3). Both procedures have various advantages and disadvantages (4). Breast reconstruction with autologous tissue should contain no tumor cell infiltration. Recent advances in tissue engineering enable the use of composite tissues for breast reconstruction with stem cells and scaffolds, which has brought new hope that tissue regeneration can be achieved (5).
Adult mammary stem cells (AMSCs) are long-lived, generally quiescent, and capable of differentiating into any cell type associated with the mammary gland, depending on which signals are received (6). The first evidence for the presence of mammary stem cells emerged in 1959 when DeOme et al (7) demonstrated that the transplantation of small portions of normal mammary tissue from donor mice into epithelium-free fat pads of syngeneic recipient mice led to the development of fully functional mammary outgrowths, containing ductal, alveolar, and myoepithelial cells. The study also established the in vivo transplantation model, which remains the gold standard assay for testing stem or progenitor cell capacity. Since the DeOme study, significant understanding of AMSCs has been acquired, partially through the application of various markers to isolate and enrich these rare cells (8).
The longevity of mammary stem cells increases the chance that they could undergo tumorigenic changes and transform into cancer stem cells (CSCs). Although the origin of breast CSCs has yet to be identified, the similarity between CSCs and normal stem cells, including their self-renewal and differentiating capabilities, and evidence that differentiation is irreversible, strongly support the conclusion that normal stem cells are the source of CSCs (9).
As breast cancer is an acquired, multigenic disease that occurs primarily in middle-aged and older individuals, the application of prospectively isolated embryonic stem cells for breast reconstruction is not possible. Thus, AMSCs are a promising cell source; however, the close anatomical similarity between normal stem cells and CSCs poses an apparent safety issue if applying AMSCs for tissue regeneration (10). The majority of biomarkers used to isolate mammary stem cells cannot distinguish between normal and CSCs (11), inevitably leading to the question of whether AMSCs from breast cancer patients can safely be used as an autologous source in breast reconstruction.
In the present study, to address this question a population of AMSCs were isolated from the periphery of breast cancer tissues. These cells were characterized for their differentiation ability, their gene expression profile and their potential to form tumors in vivo. Gene expression profiles revealed the downregulation of a group of oncogenes and upregulation of tumor suppressor genes within the AMSCs relative to autologous cancer cells. The in vivo tumorigenesis assay demonstrated that the AMSCs were non-tumorigenic, suggesting that the AMSCs adjacent to breast cancer are likely to be suitable as cell sources for breast reconstruction.
Materials and methods
Human tissue samples
The Ethics Committee of Jilin University (Changchun, China) approved this study, and all patients provided informed written consent. A total of 9 female patients diagnosed with breast cancer were recruited for the study (Table I). Fresh mammary tissue samples, including cancerous and adjacent normal tissues, were obtained during surgical resection.
Table I.
Clinicopathological characteristics of the 9 female patients recruited into the present study.
| Patient no. | Age (years) | Histopathological classification | Tumor stage |
|---|---|---|---|
| 1 | 40 | Simple carcinoma | T1N1M0 |
| 2 | 36 | Invasive ductal carcinoma | T3N2M0 |
| 3 | 27 | Pupillary carcinoma | T2N1M0 |
| 4 | 36 | Mucinous carcinoma | T2N1M0 |
| 5 | 29 | Invasive lobular carcinoma | T3N1M0 |
| 6 | 33 | Intraductal carcinoma | T1N0M0 |
| 7 | 47 | Invasive ductal carcinoma | T2N1M0 |
| 8 | 36 | Simple carcinoma | T2N1M0 |
| 9 | 28 | Invasive ductal carcinoma | T1N1M0 |
Isolation of AMSCs and breast cancer cells
AMSCs were isolated as previously described (12), with modifications. Briefly, normal breast tissues, as confirmed by pathological examination, were dissected from ≥2 cm away from the periphery of breast tumors and digested with collagenase IV (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) overnight at 37°C. Collagenase solution was removed by centrifugation at 1,200 × g and 37°C for 5 min, and the cell pellet was cultured in a 1:1 mixture (v/v) of Dulbecco's modified Eagle's medium and Ham's F12 nutrient mixture (DMEM/F12; Invitrogen; Thermo Fisher Scientific, Inc.) containing 10% fetal calf serum (FCS; Hyclone; GE Healthcare Life Sciences, Logan, UT, USA); 50 µg/ml penicillin and 0.1 mg/ml streptomycin (Beyotime Institute of Biotechnology, Haimen, China); 2.5 µg/ml amphotericin-B, 1 µg/ml minocylin, 1 µg/ml insulin, 1 µg/ml hydrocortisone and 10 µg/ml transferrin (Shanghai HyperHeal Biology Co. Ltd., Shanghai, China); 11 µg/ml ethanolamine (Fusheng, Shanghai, China); 50 ng/ml cholera toxin (List Biological Laboratories, Inc., Campbell, CA, USA); and 10 ng/ml epithelial growth factor (Invitrogen; Thermo Fisher Scientific, Inc.). After 14 days, cells grown in primary culture were detached with trypsin and subjected to sequential immunomagnetic isolation with anti-epithelial specific antigen (anti-ESA; cat. no. MS-675-P; Invitrogen; Thermo Fisher Scientific, Inc.; dilution: 1:1,000; incubation at 4°C overnight) and anti-sialomucin (anti-MUC; cat. no. 35-4900; Invitrogen; Thermo Fisher Scientific, Inc.; dilution: 1:1,000; incubation at 4°C overnight) antibodies followed by goat anti-mouse IgG microbeads (cat. no. SC-53808; Miltenyi Biotec GmbH, Bergisch Gladbach, Germany; dilution: 1:1,000; incubation at 37°C for 2 h). ESA+/MUC− cells were collected and cultured in the aforementioned growth medium for future experiments.
To isolate breast cancer cells, the breast tumor tissue samples were minced into small pieces with a scalpel and digested with collagenase IV overnight at 37°C. The collagenase solution was then removed by centrifugation and the cell pellet was seeded in the same growth medium as for AMSC isolation. AMSCs grew as adherent cells and thus were isolated by removing the non-adherent cells. Upon culture in the aforementioned growth medium, adherent AMSCs between passages two and four were used for further experiments.
For treatment with basic fibroblast growth factor (bFGF; cat. no. CYT-557; ProSpec-Tany, Rehovot, Isreal), cells were cultured in M199 medium (Invitrogen; Thermo Fisher Scientific, Inc.) containing 15% fetal bovine serum, 100 U/ml penicillin, 100 µg/ml streptomycin, and 10 ng/ml bFGF at 37°C for 24 h.
Immunocytochemistry
Cells in the logarithmic growth phase were fixed with 10% neutral buffered formalin and stained with anti-ESA (cat. no. MS-675-P, Invitrogen, Thermo Fisher Scientific, Inc.; dilution: 1:1,000; incubation at 4°C overnight), anti-common acute lymphoblastic leukemia antigen (anti-CALLA; cat. no. SC46656, Santa Cruz Biotechnology, Santa Cruz, CA, USA; dilution: 1:100; incubation at 4°C overnight), and anti-keratin-19 antibodies (anti-K-19; cat. no. SC6278, Santa Cruz Biotechnology, Santa Cruz, CA, USA; dilution: 1:100; incubation at 4°C overnight) using an indirect immunoperoxidase avidin-biotinylated enzyme complex method that involved the avidin/biotin blocking kit (cat. no. SP-2001; Vector Laboratories, Burlingame, CA, USA;), followed by species-specific biotinylated secondary antibodies targeting the corresponding primary antibodies (dilution: 1:100; incubation at 37°C for 1 h), and detected using the Vectastain Elite ABC HRP reagent (cat. no. PK-7100) in accordance with the manufacturer's protocol.
Microarray analysis
The gene expression profiles of the isolated AMSCs and breast cancer cells of the 9 patients were determined using a CapitalBio Human Genome Oligo Array (22 K) (cat. no. 400010; CapitalBio Corporation, Beijing, China) of 21,552 human genes, according to the manufacturer's instructions. Briefly, total RNA was extracted from isolated cells using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.) in accordance with the manufacturer's protocol. Total RNA was reversed transcribed into the first-strand cDNA using the First Strand Enzyme Mix and Buffer Mix included in the kit at 42°C for 2 h. Subsequently, the synthesis of second-strand cDNA was achieved using the Second Strand Master Mix at 16°C for 1 h followed by 65°C for 10 min. cDNA was then transcribed into cRNA in a reaction mixture containing 4 µl nuclease water, 20 µl T7 Buffer Mix (cat. no. HZ101-975; Shanghai Wei Zhen Industrial Co., Ltd., Shanghai, China) and 6 µl T7 enzyme mix (cat. no. AM2719G1; TideRadar Technology Co., Ltd., Beijing, China) and allowed to interact at 40°C for 8–14 h. cRNA (5 µg in 7.5 µl nuclease free water) was hybridized to random primers (4 µl) at 65°C for 5 min, followed by incubation on ice for 5 min, and reversed transcribed into cDNA in a Master Mix containing 5 µl of 4xCbcScriptII Buffer (CapitalBio Corporation, Beijing, China), 2 µl 0.1 M DTT, 1.5 µl CbcScriptII at 25°C for 10 min followed by at 37°C for 1.5 h. Following the addition of Termination Buffer (cat. no. BTN130614; Beijing Baiaolaibo Science and Technology Ltd., Beijing, China) at 65°C for 10 min and, Neutralization Solution (cat. no. A7132; Promega Corporation, Madison, WI, USA) was added to the reaction mixture at room temperature for 5 min. cDNA was then purified and labeled with Cy5-dCTP (for breast cancer cells) or Cy3-dCTP (for AMSCs; GE Healthcare Life Sciences) in a reaction mixture containing 4 µl random primers, 5 µl 5X Klenow Buffer, 1 µl Cy5-dCTP (PA55031; GE Healthcare Life Sciences) or Cy3-dCTP (cat. no. PA55031; GE Healthcare Life Sciences) and 1.2 µl Klenow Fragment (cat. no. D7035; Beyotime Institute of Biotechnology) at 37°C for 1.5 h, followed by 70°C for 5 min.
The labeled cDNA was then hybridized to the microarray chip in 81.6-µl hybridization mixture containing 40 µl of fluorescently labeled cDNA and 41.6 µl of hybridization buffer [25% formamide, 3X saline sodium citrate buffer, 5X Denhardt's solution (Beijing Dingguo Changsheng Biotechnology Co., Ltd., Beijing, China), 0.2X SDS]. After a 3-min incubation at 95°C, the chip containing the hybridization mixture was placed on ice, sealed with Lifterslip Coverslip (Thermo Fisher Scientific) and incubated at 42°C overnight, scanned using a LuxScan 10KA scanner, and processed using LuxScan 3.0 imaging analysis software (CapitalBio). Following background subtraction and normalization, genes exhibiting an experiment/control signal ratio of <0.5 were considered to be downregulated, and those with a ratio of >2.0 were considered to be upregulated.
Semi-quantitative reverse-transcription PCR (RT-PCR)
Total RNA was extracted using a TriPure™ reagent (Boehringer; Roche Applied Science, Mannheim, Germany) in accordance with the manufacturer's protocol. The extracted RNA was treated with DNase I and further purified with phenol chloroform. Total RNA (1 µg) was reversed transcribed using Superscript II reverse transcriptase (cat. no. 18064071, Invitrogen; Thermo Fisher Scientific, Inc.), according to the manufacturer's instructions.
The following primers were used for PCR: MYC forward, 5′-CCC AGC GAG GAC ATC TGG AAG AA-3′; MYC reverse, 5′-GAG AAG CCG CTC CAC ATG CAG TC-3′ (amplicon size, 268 bp); H-RAS forward, 5′-AAG CTT GTG GTG GTG GGC GCT AAA GGC-3′; H-RAS reverse, 5′-CTT TCA CCC GCT TGA TCT GCT CCC TGT ACT-3′ (amplicon size, 300 bp); ErbB receptor tyrosine kinase 2 (ERBB2, forward, 5′-GCC CTG GAC ACC TAC AAC AC-3′; ERBB2 reverse, 5′-TCC GGC AGA AAT GCC AGG CT-3′ (amplicon size, 329 bp); β-actin (ACTB) forward, 5′-CCT GTA CGC CTC TGG CCG TAC CAC T-3′; and ACTB reverse, 5′- CTG TAG CCG CGC TCG GTG AGG ATC T-3′ (amplicon size, 174 bp).
The PCR conditions for the amplification of MYC were 28 cycles of 94°C for 1 min, 60°C for 1 min and 72°C for 1 min, followed by a 5-min final extension at 72°C. PCR amplification of H-RAS comprised denaturation at 94°C for 4 min; 30 cycles of 94°C for 1 min, 62°C for 1 min and 72°C for 1 min; followed by an elongation 72°C for 10 min. PCR amplification of ERBB2 consisted of denaturation at 94°C for 2 min; then 35 cycles at 94°C for 45 sec, 55°C for 45 sec and 72°C for 1 min; followed by a 5-min final extension at 72°C. PCR amplification of ACTB included denaturation at 95°C for 3 min; followed by 40 cycles at 95°C for 30 sec, 57°C for 40 sec and 72°C for 45 sec; followed by a 6-min final extension at 72°C. The PCR products were loaded onto ethidium bromide-stained 1% agarose gel and imaged using a Gel Doc XR+ System (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The band density was quantified using Quantity One software (version 4.52, Bio-Rad Laboratories, Inc.) and presented as a ratio of target gene to β-actin (internal control).
Western blot analysis
Whole cell extracts from AMSCs and breast CSCs were prepared by lysing cells in lysis buffers [300 mM NaCl, 50 mM Tris-HCl (pH 8.0), 25 mM EDTA, 20% (v/v) SDS, and 0.2 mg/ml proteinase K]. Insoluble debris was removed by centrifugation at 16,000 × g for 2 min. Protein concentration in whole cell extracts was determined using a Bio-Rad Protein Assay (Bio-Rad Laboratories, Inc.). From each sample, 20–30 µg of whole cell extract was resolved by SDS-PAGE, transferred to an Immobilon-P polyvinylidene fluoride membrane (EMD Millipore, Billerica, MA, USA) and probed with the following primary antibodies: anti-ErbB2 (cat. no. 2244S; dilution: 1:1,000; incubation at 4°C overnight), anti-Ras (cat. no. 3339S; dilution: 1:1,000; incubation at 4°C overnight), anti-PTEN (cat. no. 9549L; dilution: 1:1,000; incubation at 4°C overnight), and anti-β-actin (internal control; cat. no. 8844S; dilution: 1:500; incubation at 4°C overnight) antibodies (all from Cell Signaling Technology, Inc., Danvers, MA, USA) followed by horseradish peroxidase (HRP)-conjugated species-specific secondary antibodies targeting the corresponding primary antibodies at room temperature for 2 h. Protein bands were visualized using an Amersham ECL Western Blotting Detection kit (GE Healthcare Bio-Sciences, Pittsburgh, PA, USA).
Culture of MCF-7 cells
MCF-7 cells were purchased from the Cell Bank of Type Culture of Chinese Academy of Sciences (Shanghai, China) and cultured in DMEM containing 10% FCS, 50 µg/ml penicillin, 0.1 mg/ml streptomycin, 1.0 µg/ml sodium pyruvate, 10 µg/ml insulin, 0.1 mM non-essential amino acids, and 1.5 g/l sodium bicarbonate at 37°C in a sterile atmosphere containing 5% CO2.
In vivo tumorigenesis assay
The Institutional Animal Care and Use Committee of Jilin University approved all animal experiments. A total of 28 female non-obese diabetic/severe combined immunodeficiency (NOD/SCID) mice (age, 4–6 weeks; weight, 19–22 g) were purchased from the Shanghai Laboratory Animal Center (Shanghai, China) and housed in a pathogen-free facility, with water and food provided ad libitum.
The mice were randomly divided into an experimental group (n=14) and a control group (n=14), and were individually injected subcutaneously with AMSCs (2×106) or MCF-7 cells (2×106), respectively, in the right dorsolateral area. The growth of subcutaneous tumors was monitored by evaluating the length (L) and width (W) of the tumors using a caliper every two days. The tumor volume (V) was calculated as V=1/2 xL xW2. At 30 days after the injection for the experimental group and 14 days for the control group, all mice were sacrificed by cervical dislocation and tissues from the injected region were isolated. The isolated tissues were fixed in formalin, embedded in paraffin, stained with hematoxylin and eosin, and observed under a microscope.
Results
AMSCs isolated from normal tumor-adjacent mammary tissue exhibit stem cell features
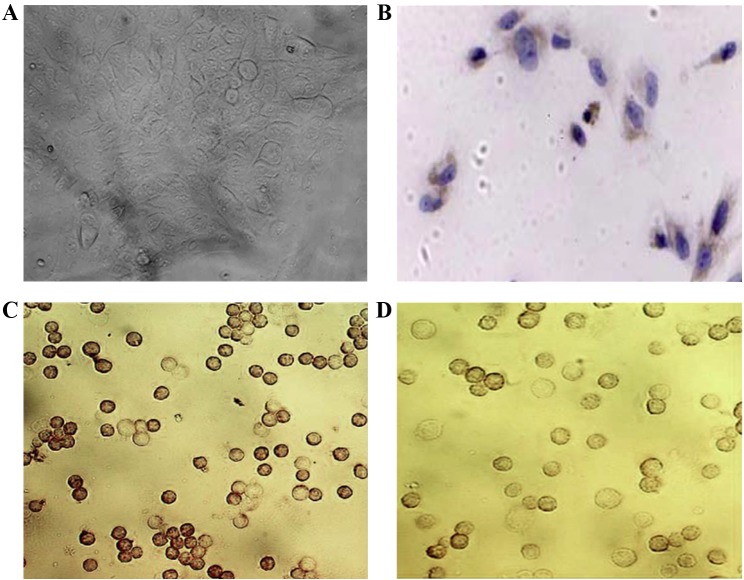
To characterize AMSCs from breast cancer patients, tumor-free mammary tissue was extracted from ≥2 cm away from the tumor periphery in patients with breast cancer, and confirmed by pathological examination. ESA+/MUC− cells were purified through immunomagnetic isolation, which has been demonstrated to separate a cell population into luminal and myoepithelial cells (13). Under non-differentiating conditions, these cells attached to the plate and became round or polygonal, with an indistinct cell boundary (Fig. 1A). Using immunocytochemical staining, these cells were identified as positive for ESA on the cellular membrane and partially in the cytoplasm (Fig. 1B) and for K-19 (Fig. 1C), and were positive for CALLA following bFGF treatment (Fig. 1D).
Figure 1.
AMSCs isolated from normal tissues adjacent to breast cancer exhibit stem cell features (magnification, ×400). (A) A phase-contrast microscope image of an AMSC colony in non-differentiating conditions. The individual cells have a diffuse phenotype and are round or cuboidal in shape, with indistinct cell boundaries. The cell colony had a clear boundary, with a number of cells on the periphery exhibiting an elongated phenotype. The AMSCs upon bFGF treatment were subjected to immunohistochemical staining with antibodies specific for (B) epithelial specific antigen, (C) keratin-19, and (D) common acute lymphoblastic leukemia antigen. Positive staining for ESA was observed on the cellular membrane and within the cytoplasm. AMSC, adult mammary stem cell.
AMSCs exhibit low expression levels of oncogenes and high expression levels of tumor suppressor genes
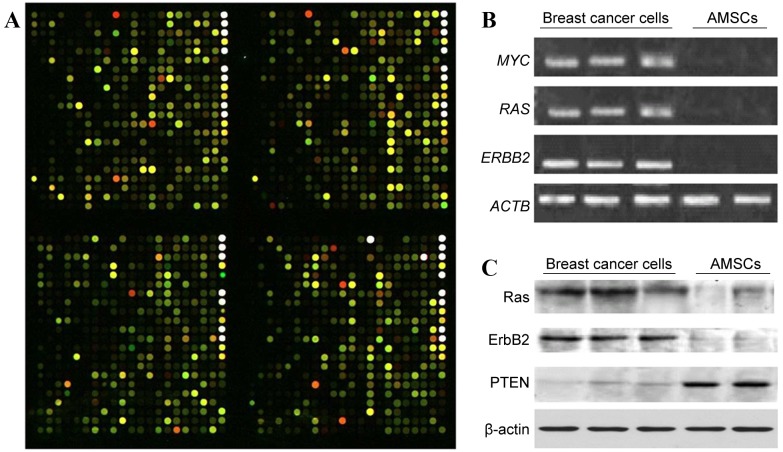
To characterize the molecular features associated with the isolated AMSCs, we performed a gene microarray analysis and compared the gene expression profiles of paired AMSCs and cancer cells extracted from patients (Fig. 2A). From a total of 21,522 genes examined, 798 differed >2.5-fold between the groups, with 174 downregulated and 624 upregulated in AMSCs compared with cancer cells. From those differentially expressed genes, 16 have a clearly demonstrated clinical association with human breast cancer (as defined by the CapitalBio Gene Ontology Database (www.capitalbio.com); Table II), including 10 upregulated tumor suppressor genes and 6 downregulated oncogenes.
Figure 2.
AMSCs exhibit differential gene expression compared with autologous breast cancer cells. (A) Representative image of four blocks following the hybridization of Cy3-labeled AMSC sample (green signal) and Cy5-labeled breast cancer sample (red signal). The CapitalBio Human Genome Oligo Array (22K) includes 21,522 70-mer oligo probes spotted on a 75×25-mm, chemically modified glass slide. The green color indicates a stronger signal from the AMSC sample, whereas red indicates a stronger signal from the breast cancer sample, and yellow indicates a similar signal from the two tissue types. (B) Gel electrophoretic analyses of RT-PCR products. Total RNA was extracted from isolated breast cancer cell samples and AMSC samples selected at random from the 9 patients with breast cancer, and was reverse transcribed. The relative gene expression levels of MYC, RAS, and ERBB2 were examined by semi-quantitative PCR, with ACTB used as an internal control. (C) Western blot analysis of Ras, ErbB2 and PTEN in breast cancer cell samples and AMSC samples with β-actin used as internal control. AMSC, adult mammary stem cell; RT-PCR, reverse transcription-polymerase chain reaction; ErbB2, ErbB receptor tyrosine kinase 2; ACTB, β-actin; PTEN, phosphatase and tensin homolog.
Table II.
Summary of 16 differentially expressed genes between AMSCs and cancer cells that have demonstrated an association with human breast cancer.
| A, Genes upregulated in AMSCs relative to cancer cells | ||||
|---|---|---|---|---|
| Gene symbol | Gene locus | Gene name and general functions in breast cancer | Ratio (AMSCs/cancer cells) | (Refs.) |
| RB1 | 13q14.2 | RB transcriptional corepressor 1; regulates cell cycle progression | 19.1491 | (25) |
| PTEN | 10q23.3 | Phosphatase and tensin homolog; phosphatase involved in multiple signaling pathways, including phosphoinositide 3-kinase/protein kinase B, cyclin D1 and p53 signaling | 2.0883 | (26) |
| ADRB2 | 5q31-q32 | Adrenoceptor β 2; regulates growth and migration of breast cancer cells | 2.1505 | (27) |
| CDKN2A | 9p21 | Cyclin-dependent kinase inhibitor 2A; controls cell cycle progression and senescence | 2.6221 | (28) |
| CLCA2 | 1p31-p22 | Chloride channel accessory 2; induced by p53 to inhibit breast cancer cell proliferation | 25.5938 | (29) |
| SOD2 | 6q25.3 | Superoxide dismutase 2, mitochondrial; neutralizes reactive oxygen species and may be epigenetically silenced in breast cancer cells | 4.6025 | (30) |
| NFKBIA | 14q13 | NFκB inhibitor α; regulates NFκB signaling in breast cancer | 2.6952 | (31) |
| MMP12 | 11q22.3 | Matrix metalloproteinase 12; inhibits tumor vascularization | 13.0442 | (32) |
| ITGB3 | 17q21.32 | Integrin subunit β 3; regulates tumor progression, metastasis and stem cell properties | 5.6503 | (33) |
| IL1B | 2q14 | Interleukin 1 β; pro-inflammatory cytokine regulating breast cancer progression | 10.4994 | (34) |
| B, Genes downregulated in AMSCs relative to cancer cells | ||||
| Gene symbol | Gene locus | Gene name and general functions in breast cancer | Ratio (AMSCs/cancer cells) | (Refs.) |
| ERBB2 | 17q21 | Erb-B2 receptor tyrosine kinase 2; regulates multiple functions, including apoptosis, proliferation, adhesion, motility and vascularization, to promote breast cancer progression. | 0.3866 | (35) |
| HRAS | 11p15.1-p15.4 | HRas proto-oncogene, GTPase; proto-oncogene regulating intracellular signaling pathways to promote tumorigenesis. | 0.4989 | (36) |
| MYC | 8q24.12-q24.13 | V-Myc avian myelocytomatosis viral oncogene homolog; proto-oncogene regulating cell proliferation, apoptosis and stem/progenitor cell function. | 0.3921 | (37,38) |
| GHR | 5p13-p12 | Growth hormone receptor; mediates growth hormone signaling. | 0.3815 | (39) |
| H19 | 11p15.5 | H19, imprinted maternally expressed transcript (non-protein coding); encodes an untranslated RNA that is overexpressed in breast cancer and promotes cellular transformation/in vivo tumorigenesis. | 0.3125 | (40) |
| ADAMTSL1 | 9p22.1-p22.2 | ADAMTS-like 1; a secreted molecule resembling members of the ADAMTS family of proteases with important functions regulating extracellular matrix. | 0.4506 | (41) |
AMSC, adult mammary stem cell; NFκB, nuclear factor κB; ADAMTS, a disintegrin and metalloproteinase with thrombospondin motifs.
To validate the microarray data, semi-quantitative RT-PCR was performed on certain targets identified by microarray, including MYC, RAS and ERBB2. Consistent with the microarray analysis, there were higher mRNA levels of all three of these genes in the isolated cancer cells than in the AMSCs (Fig. 2B). The levels of RAS, ERBB2, and phosphatase and tensin homolog (PTEN) proteins in these cells were also evaluated. As presented in Fig. 2C, the levels of RAS and ERBB2 were higher in breast cancer cells than in the AMSCs, whereas AMSCs had a higher level of PTEN than the cancer cells.
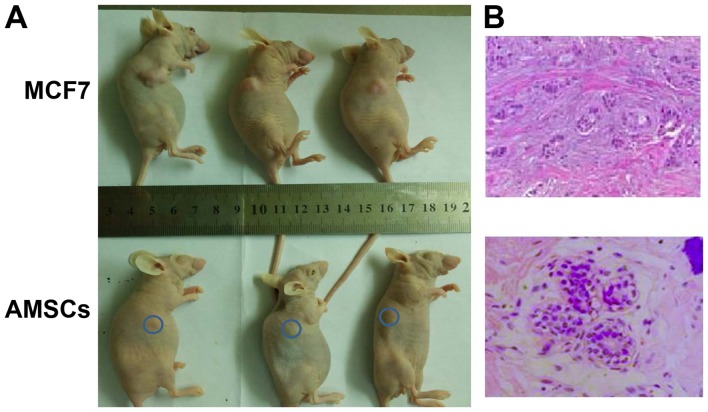
AMSCs do not generate tumors in nude NOD/SCID mice, and form regularly arranged duct-like structures
To assess the properties and tumorigenic nature of the isolated AMSCs, an in vivo analysis was conducted by injecting the AMSCs into immunodeficient mice, then monitoring the growth of tumors in vivo and histologically. As a control, MCF-7 cells were used, which are breast cancer cells of low malignancy that exhibit an early-stage cancer phenotype. In the AMSC-injected mice, over the 30-day observation period, the lump under the skin resulting from subcutaneous injection did not increase in size, while injection with MCF-7 cells led to prominent outgrowth following 14 days (Fig. 3A). Histological examination revealed that the subcutaneous lump from AMSC injection contained duct-like structures composed of an inner layer of cuboidal luminal epithelial cells with an outer layer of squamous cells (Fig. 3B, left). By contrast, the outgrowth from MCF-7 cells exhibited a glandular-like arrangement of hyperplastic cells of various sizes (Fig. 3B, right).
Figure 3.
To assess whether AMSCs are tumorigenic in vivo, AMSCs or MCF-7 breast cancer cells were subcutaneously injected into the dorsolateral area of nude non-obese diabetic/severe combined immunodeficiency-type mice (n=14 per group). (A) Representative mice from the AMSC group and the MCF-7 group were randomly selected at 30 and 14 days after injection, respectively, and photographed (blue circle: injection site in AMSC group). (B) Tissues from the injection site were isolated at 30 days (AMSC group) and 14 days (MCF-7 group) after injection and stained with hematoxylin and eosin. In the AMSC-injected tissue (magnification, ×400), normal mammary glandular structure was detected, in which the duct is lined with an inner layer of cuboidal luminal epithelial cells with an outer layer of squamous cells. MCF-7-injected breast tissue is shown on the right (magnification, ×200). AMSC, adult mammary stem cell.
Discussion
In the present study, the phenotype of AMSCs was characterized, AMSC gene expression profiles were compared with breast cancer cells, and tumorigenic potential in vivo was assessed. It was demonstrated that AMSCs exhibited the characteristics of normal, non-malignant stem cells, in that they presented the morphology of luminal epithelial cells in non-differentiating culture, exhibited downregulated expression of oncogenes and upregulated expression of tumor suppressor genes, and formed normal mammary structures upon xenograft injection into nude mice.
In 2006, two groups independently reported the generation of functional mammary glands from a single AMSC isolated from mice (14,15). In the same year, Proia and Kuperwasser (16) published a detailed protocol for reconstructing human mammary tissues in a mouse model. These studies may contribute advancements towards the use of AMSCs for breast reconstruction subsequent to mastectomy, as is typically performed on female patients with breast cancer.
Multiple markers, individually or combined, have been applied to isolate AMSCs (17). In the current study, the results confirmed those of Gudjonsson et al (18), who demonstrated that there were generally two luminal epithelial cell populations: A major population co-expressing MUC and ESA (MUC+/ESA+), and a minor population positive only for ESA (MUC−/ESA+). MUC+/ESA+ cells are differentiated, acinar and restricted to the luminal epithelium, without stem cell properties. MUC−/ESA+ cells are suprabasally localized in situ, retain the potential to differentiate into MUC+/ESA+ luminal epithelial cells or Thy-1+/α-smooth muscle actin+ myoepithelial cells, and give rise to elaborate terminal ductal lobular units in three-dimensional cultures (18). Consistent with that study, it was identified that the MUC−/ESA+ cells isolated by immunomagnetic sorting exhibited the morphology of luminal epithelial cells in non-differentiating culture in the present study.
Due to their inherent ability to differentiate into a variety of cell types, AMSCs have become a key component in regenerative medicine. Their longevity, however, also makes them candidates for CSC generation, by increasing the likelihood that they will acquire all the changes necessary for tumorigenesis. To characterize the potential cancerous nature of AMSCs, two assays were performed. Initially, the gene expression profiles of AMSCs were compared with breast cancer cells isolated from the same patients. From the 798 differentially expressed genes, ≥16 genes were previously associated with breast cancer. Of these, genes with tumor-inhibitory functions, including RB transcriptional corepressor 1, PTEN, adrenoceptor β2, cyclin-dependent kinase inhibitor 2A, NFκB inhibitor α, calcium-activated chloride channel-2, and mitochondrial superoxide dismutase, were present at enhanced levels in AMSCs compared with cancer cells. By contrast, several oncogenes, including ERBB2, MYC, RAS, and growth hormone receptor were upregulated in cancer cells relative to the AMSCs. This suggests that isolated AMSCs have not undergone oncogenic transformation to the same extent as cancer cells from the same source.
This conclusion is consistent with the concept of field cancerization proposed by Slaughter et al (19) in 1953 when, through extensive histological examinations, they identified histologically abnormal, though not cancerous, tissue surrounding oral squamous cell carcinoma. This phenomenon has also been observed in other human cancers, including breast cancer (20). Therefore, although the tissues used for AMSC isolation may be confirmed by pathological examination to be tumor-free and exhibit a gene expression profile corresponding to a normal phenotype, AMSCs may still contain oncogenic changes that are not detected by microarray analysis which, nonetheless, indicate the early events of carcinogenesis. To address this possibility, these cells were further characterized with functional assays.
An in vivo tumorigenesis assay was employed to assess the AMSCs, since this is considered the gold standard for the analysis of normal cells and CSCs. When compared with the low-malignancy MCF-7 cells, even a high number of injected AMSCs (2×106) did not form any tumors; however, over a 12-week observation period, the AMSCs formed ductal structures containing luminal epithelial and myoepithelial cells resembling normal mammary parenchyma. By contrast, the MCF-7 cells readily formed well-differentiated tumors with glandular structures. This data further corroborated the multipotency of AMSCs; although they exhibited a luminal epithelial phenotype in vitro, they differentiated into luminal and myoepithelial cells in vivo.
Although microarray analysis revealed marked differences between AMSCs and autologous breast cancer cells, it is desirable to compare the gene expression profile between AMSCs and autologous CSCs. A recent study has demonstrated that CSCs share major somatic mutations with bulk cancer cells (21); it would be interesting and potentially more accurate for future studies to compare the genetic mutations between AMSCs and autologous CSCs or cancer cells for any underlying carcinogenic potential of the AMSCs.
Besides the potential stem cells residing in the mammary epithelial compartment, the mesenchymal compartment within or outside the mammary gland may also contain stem cells that can be transdifferentiated into mammary epithelial components. Using the Cre-LoxP recombination system, Morroni et al (22) observed a reversible transdifferentiation between mammary adipocytes and epithelium in adult mice during pregnancy and lactation. Furthermore, De Matteis et al (23) observed that white adipose tissue from the dorso-lumbar fat depot in the fourth right mammary glands of Rosa26 mice (males or virgin females) gave rise to epithelial lobuloalveolar glands that tested positive for immunocytochemical markers of milk-secreting glandular cells, following implantation under the capsule of the fourth right mammary gland of pregnant and lactating wild-type females.
Compared with mesenchymal stem or precursor cells, mammary epithelial stem cells are more readily differentiated to other epithelial components. However, their ability to differentiate into stromal components, which are important for mammary structure and function, may be limited (24). Consistently, the present study demonstrated that isolated AMSCs primarily formed epithelial ductal structures, which were distinct from the mesenchymal compartment, suggesting that the further characterization of mesenchymal stem cells may have great significance with regard to constructing a more functionally intact mammary gland.
In summary, in the present study preliminary evidence that AMSCs isolated from normal tissue adjacent to breast cancer have the phenotypes of normal stem cells, rather than CSCs, is provided. Therefore, AMSCs are a potential cell source for autologous breast reconstruction.
Acknowledgements
The authors would like to thank Medjaden Bioscience Limited (Hong Kong, China) for assisting in the preparation of this manuscript. This study was supported by National Natural Science Foundation of China (grant no. 30300336), the Jilin Provincial Science and Technology Department of China (grant no. 200705134) and Bethune Project B of Jilin University (grant no. 2012217).
References
- 1.Thomas-MacLean R. Beyond dichotomies of health and illness: Life after breast cancer. Nurs Inq. 2005;12:200–209. doi: 10.1111/j.1440-1800.2005.00268.x. [DOI] [PubMed] [Google Scholar]
- 2.Roje Z, Roje Z, Janković S, Ninković M. Breast reconstruction after mastectomy. Coll Antropol. 2010;34(Suppl 1):S113–S123. [PubMed] [Google Scholar]
- 3.Rozen WM, Rajkomar AK, Anavekar NS, Ashton MW. Post-mastectomy breast reconstruction: A history in evolution. Clin Breast Cancer. 2009;9:145–154. doi: 10.3816/CBC.2009.n.024. [DOI] [PubMed] [Google Scholar]
- 4.Djohan R, Gage E, Bernard S. Breast reconstruction options following mastectomy. Cleve Clin J Med. 2008;75(Suppl 1):S17–S23. doi: 10.3949/ccjm.75.Suppl_1.S17. [DOI] [PubMed] [Google Scholar]
- 5.Techanukul T, Lohsiriwat V. Stem cell and tissue engineering in breast reconstruction. Gland Surg. 2014;3:55–61. doi: 10.3978/j.issn.2227-684X.2014.02.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holland MS, Holland RE. The cellular perspective on mammary gland development: Stem/progenitor cells and beyond. J Dairy Sci. 2005;88(Suppl 1):E1–E8. doi: 10.3168/jds.S0022-0302(05)73132-5. [DOI] [PubMed] [Google Scholar]
- 7.Deome KB, Faulkin LJ, Jr, Bern HA, Blair PB. Development of mammary tumors from hyperplastic alveolar nodules transplanted into gland-free mammary fat pads of female C3H mice. Cancer Res. 1959;19:515–520. [PubMed] [Google Scholar]
- 8.Ercan C, van Diest PJ, Vooijs M. Mammary development and breast cancer: The role of stem cells. Curr Mol Med. 2011;11:270–285. doi: 10.2174/156652411795678007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta PB, Chaffer CL, Weinberg RA. Cancer stem cells: Mirage or reality? Nat Med. 2009;15:1010–1012. doi: 10.1038/nm0909-1010. [DOI] [PubMed] [Google Scholar]
- 10.Li L, Neaves WB. Normal stem cells and cancer stem cells: The niche matters. Cancer Res. 2006;66:4553–4557. doi: 10.1158/0008-5472.CAN-05-3986. [DOI] [PubMed] [Google Scholar]
- 11.Chen X, Liu Q, Song E. Mammary stem cells: Angels or demons in mammary gland? Signal Transduction Targeted Therapy. 2017;2:16038. doi: 10.1038/sigtrans.2016.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kao CY, Nomata K, Oakley CS, Welsch CW, Chang CC. Two types of normal human breast epithelial cells derived from reduction mammoplasty: Phenotypic characterization and response to SV40 transfection. Carcinogenesis. 1995;16:531–538. doi: 10.1093/carcin/16.3.531. [DOI] [PubMed] [Google Scholar]
- 13.Ponti D, Zaffaroni N, Capelli C, Daidone MG. Breast cancer stem cells: An overview. Eur J Cancer. 2006;42:1219–1224. doi: 10.1016/j.ejca.2006.01.031. [DOI] [PubMed] [Google Scholar]
- 14.Shackleton M, Vaillant F, Simpson KJ, Stingl J, Smyth GK, Asselin-Labat ML, Wu L, Lindeman GJ, Visvader JE. Generation of a functional mammary gland from a single stem cell. Nature. 2006;439:84–88. doi: 10.1038/nature04372. [DOI] [PubMed] [Google Scholar]
- 15.Stingl J, Eirew P, Ricketson I, Shackleton M, Vaillant F, Choi D, Li HI, Eaves CJ. Purification and unique properties of mammary epithelial stem cells. Nature. 2006;439:993–997. doi: 10.1038/nature04496. [DOI] [PubMed] [Google Scholar]
- 16.Proia DA, Kuperwasser C. Reconstruction of human mammary tissues in a mouse model. Nat Protoc. 2006;1:206–214. doi: 10.1038/nprot.2006.31. [DOI] [PubMed] [Google Scholar]
- 17.Kalirai H, Clarke RB. Human breast epithelial stem cells and their regulation. J Pathol. 2006;208:7–16. doi: 10.1002/path.1881. [DOI] [PubMed] [Google Scholar]
- 18.Gudjonsson T, Villadsen R, Nielsen HL, Ronnov-Jessen L, Bissell MJ, Petersen OW. Isolation, immortalization, and characterization of a human breast epithelial cell line with stem cell properties. Genes Dev. 2002;16:693–706. doi: 10.1101/gad.952602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer. 1953;6:963–968. doi: 10.1002/1097-0142(195309)6:5<963::AID-CNCR2820060515>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 20.Försti A, Louhelainen J, Söderberg M, Wijkström H, Hemminki K. Loss of heterozygosity in tumour-adjacent normal tissue of breast and bladder cancer. Eur J Cancer. 2001;37:1372–1380. doi: 10.1016/S0959-8049(01)00118-6. [DOI] [PubMed] [Google Scholar]
- 21.Klevebring D, Rosin G, Ma R, Lindberg J, Czene K, Kere J, Fredriksson I, Bergh J, Hartman J. Sequencing of breast cancer stem cell populations indicates a dynamic conversion between differentiation states in vivo. Breast Cancer Res. 2014;16:R72. doi: 10.1186/bcr3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morroni M, Giordano A, Zingaretti MC, Boiani R, De Matteis R, Kahn BB, Nisoli E, Tonello C, Pisoschi C, Luchetti MM, et al. Reversible transdifferentiation of secretory epithelial cells into adipocytes in the mammary gland; Proc Natl Acad Sci USA; 2004; pp. 16801–16806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Matteis R, Zingaretti MC, Murano I, Vitali A, Frontini A, Giannulis I, Barbatelli G, Marcucci F, Bordicchia M, Sarzani R, et al. In vivo physiological transdifferentiation of adult adipose cells. Stem Cells. 2009;27:2761–2768. doi: 10.1002/stem.197. [DOI] [PubMed] [Google Scholar]
- 24.Mammary stem cells and the differentiation hierarchy: Current status and perspectives. Genes Dev. 2014;28:1143–1158. doi: 10.1101/gad.242511.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burkhart DL, Sage J. Cellular mechanisms of tumour suppression by the retinoblastoma gene. Nat Rev Cancer. 2008;8:671–682. doi: 10.1038/nrc2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blanco-Aparicio C, Renner O, Leal JF, Carnero A. PTEN, more than the AKT pathway. Carcinogenesis. 2007;28:1379–1386. doi: 10.1093/carcin/bgm052. [DOI] [PubMed] [Google Scholar]
- 27.Luthy IA, Bruzzone A, Piñero CP, Castillo LF, Chiesa IJ, Vázquez SM, Sarappa MG. Adrenoceptors: Non conventional target for breast cancer? Curr Med Chem. 2009;16:1850–1862. doi: 10.2174/092986709788186048. [DOI] [PubMed] [Google Scholar]
- 28.Caldon CE, Daly RJ, Sutherland RL, Musgrove EA. Cell cycle control in breast cancer cells. J Cell Biochem. 2006;97:261–274. doi: 10.1002/jcb.20690. [DOI] [PubMed] [Google Scholar]
- 29.Walia V, Ding M, Kumar S, Nie D, Premkumar LS, Elble RC. hCLCA2 Is a p53-Inducible Inhibitor of Breast Cancer Cell Proliferation. Cancer Res. 2009;69:6624–6632. doi: 10.1158/0008-5472.CAN-08-4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hitchler MJ, Oberley LW, Domann FE. Epigenetic silencing of SOD2 by histone modifications in human breast cancer cells. Free Radic Biol Med. 2008;45:1573–1580. doi: 10.1016/j.freeradbiomed.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pratt MA, Tibbo E, Robertson SJ, Jansson D, Hurst K, Perez-Iratxeta C, Lau R, Niu MY. The canonical NF-kappaB pathway is required for formation of luminal mammary neoplasias and is activated in the mammary progenitor population. Oncogene. 2009;28:2710–2722. doi: 10.1038/onc.2009.131. [DOI] [PubMed] [Google Scholar]
- 32.Margheri F, Serrati S, Lapucci A, Anastasia C, Giusti B, Pucci M, Torre E, Bianchini F, Calorini L, Albini A, et al. Systemic sclerosis-endothelial cell antiangiogenic pentraxin 3 and matrix metalloprotease 12 control human breast cancer tumor vascularization and development in mice. Neoplasia. 2009;11:1106–1115. doi: 10.1593/neo.09934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pontier SM, Muller WJ. Integrins in mammary-stem-cell biology and breast-cancer progression-a role in cancer stem cells? J Cell Sci. 2009;122:207–214. doi: 10.1242/jcs.040394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin L, Yuan RQ, Fuchs A, Yao Y, Joseph A, Schwall R, Schnitt SJ, Guida A, Hastings HM, Andres J, et al. Expression of interleukin-1beta in human breast carcinoma. Cancer. 1997;80:421–434. doi: 10.1002/(SICI)1097-0142(19970801)80:3<421::AID-CNCR10>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 35.Freudenberg JA, Wang Q, Katsumata M, Drebin J, Nagatomo I, Greene MI. The role of HER2 in early breast cancer metastasis and the origins of resistance to HER2-targeted therapies. Exp Mol Pathol. 2009;87:1–11. doi: 10.1016/j.yexmp.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moon A. Differential functions of Ras for malignant phenotypic conversion. Arch Pharm Res. 2006;29:113–122. doi: 10.1007/BF02974271. [DOI] [PubMed] [Google Scholar]
- 37.Jamerson MH, Johnson MD, Dickson RB. Of mice and Myc: c-Myc and mammary tumorigenesis. J Mammary Gland Biol Neoplasia. 2004;9:27–37. doi: 10.1023/B:JOMG.0000023586.69263.0b. [DOI] [PubMed] [Google Scholar]
- 38.Stoelzle T, Schwarb P, Trumpp A, Hynes NE. c-Myc affects mRNA translation, cell proliferation and progenitor cell function in the mammary gland. BMC Biol. 2009;7:63. doi: 10.1186/1741-7007-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Garderen E, Schalken JA. Morphogenic and tumorigenic potentials of the mammary growth hormone/growth hormone receptor system. Mol Cell Endocrinol. 2002;197:153–165. doi: 10.1016/S0303-7207(02)00259-9. [DOI] [PubMed] [Google Scholar]
- 40.Lottin S, Adriaenssens E, Dupressoir T, Berteaux N, Montpellier C, Coll J, Dugimont T, Curgy JJ. Overexpression of an ectopic H19 gene enhances the tumorigenic properties of breast cancer cells. Carcinogenesis. 2002;23:1885–1895. doi: 10.1093/carcin/23.11.1885. [DOI] [PubMed] [Google Scholar]
- 41.Hirohata S, Wang LW, Miyagi M, Yan L, Seldin MF, Keene DR, Crabb JW, Apte SS. Punctin, a novel ADAMTS-like molecule, ADAMTSL-1, in extracellular matrix. J Biol Chem. 2002;277:12182–12189. doi: 10.1074/jbc.M109665200. [DOI] [PubMed] [Google Scholar]