Abstract
Objectives
To investigate the determinants of the length of hospitalization (LOH) due to acute odontogenic maxillofacial infections (AOMIs) from 2009 to 2013.
Materials and Methods
Dental records of adult patients with AOMIs and related data were retrieved from the Vilnius University's dental hospital. The LOH was related to several determinants in each of the following domains: outpatient primary care, severity of AOMIs, lifestyle and disease domains. Determinants were also associated with the LOH using multivariate analysis.
Results
A total of 285 patients were hospitalized with AOMIs, of which 166 (58.2s%) were males and 119 (41.8s%) were females. The mean LOH was 8.3 ± 4.9 days. The bivariate analysis did not reveal any statistically significant differences in LOH between patients with AOMIs who received urgent outpatient primary care and those who did not receive such care prior to hospitalization. All AOMI severity-related determinants were associated with the LOH. The LOH was related to coexisting systemic conditions but not to the higher severity of dental or periodontal diseases. Both bivariate and multivariate analyses revealed similar trends, where the most significant determinants of a longer LOH were related to the severity of AOMIs.
Conclusion
The most important determinants regarding longer hospitalization were indicators of infection severity such as an extension of the odontogenic infection and the need for an extraoral incision to drain the infection.
Key Words: Length of hospitalization, Odontogenic infections, Determinants
Introduction
Acute odontogenic maxillofacial infections (AOMIs) develop due to untreated dental diseases [1]. Most AOMIs need intraoral or extraoral incisions to drain the infection [2]. While less severe AOMIs can be treated in outpatient treatment facilities, treatment of the most severe AOMIs requires costly hospitalization [3]. The length of hospitalization (LOH) has been associated with the severity of AOMIs [4,5] and the presence of coexisting systemic conditions [3], among which diabetes has been identified as one of the most common medical conditions that increases a patient's overall susceptibility to infections [6]. Among patient-related risk determinants, poor oral hygiene, self-medication, inadequate use of medications and delayed hospitalization have been associated with the spread of acute odontogenic infections [1]. Most importantly, severe forms of AOMIs as well as delayed or unsuccessful treatment of AOMIs may lead to life-threatening complications such as mediastinitis or sepsis [7].
Given that the costs of dental care have been identified as a barrier to regular dental checkups, easily accessible and affordable primary dental care is necessary to meet the treatment needs of the most vulnerable population groups [8,9]. Thus, free or subsidized public dental clinics are vital to meet the health care needs of underserved population groups and patients at high risk of dental diseases [10].
To improve access to urgent primary care for patients with acute medical conditions including AOMIs, the Lithuanian National Health Care Insurance Fund has contracted multiple treatment facilities to provide such care in different locations of the country. This infrastructure allows patients with AOMIs to receive free or partly subsidized primary medical care at a dental treatment facility of their choice.
The Lithuanian health care model for the provision of urgent primary care is useful to study how the presence of free or partially subsidized access to urgent primary care in both outpatient and hospital settings impacts the LOH of patients treated for AOMIs. Hence, the present study investigated the determinants of the LOH of patients with severe AOMIs in both the outpatient and hospital settings.
Materials and Methods
The study was approved by the National Lithuanian Ethics Board. The present comprehensive retrospective study focused on the period from 2009 to 2013 and on patients with severe AOMIs hospitalized at the University Hospital. Dental records and clinical related information of adult patients, who agreed to participate in the study, were investigated.
Study Variables
The present study examined how different clinical and nonclinical determinants were related to the LOH. The information about potential AOMI determinants was collected in four domains: (1) the Outpatient Primary Urgent Care (OPUC) related to different aspects of care provided to patients with AOMIs prior to their hospitalization. The OPUC domain included the following determinants: accessing or not accessing OPUC prior to hospitalization, waiting time prior to accessing OPUC, time when OPUC was received, costs of OPUC, seeking hospitalization after referral from OPUC and admission to a hospital. (2) The AOMI severity domain included the following determinants: anatomical spaces involved in AOMIs, extension of AOMIs (unilateral or bilateral), type of anesthesia (local or general), type of incision to drain AOMIs (intraoral or extraoral) and occurrence of complications due to AOMIs. (3) The lifestyle domain (table 1) included information about smoking, oral self-care, self-treatment when having oral pain and if dental care was sought only in the case of an emergency. (4) The disease domain (table 1) comprised information about the presence of systemic diseases, experience of dental diseases and periodontal health status.
Table 1.
LOH (in days) for patients with AOMIs
| Domain | Outpatient care prior to hospitalization |
p value | ||
|---|---|---|---|---|
| yes | no | |||
| Domain of lifestyle determinants | ||||
| Smoking | ||||
| Yes | 8.6 ± 4.4 | 7.9 ± 4.8 | 0.393 | |
| No | 8.8 ± 4.7 | 7.9 ± 5.7 | 0.307 | |
| p value* | 0.808 | 0.969 | ||
| Oral self-care | ||||
| Less than weekly | 9.0 ± 3.9 | 8.2 ± 5.2 | 0.444 | |
| Weekly | 8.9 ± 5.2 | 6.9 ± 5.0 | 0.069 | |
| Daily | 8.0 ± 4.0 | 8.4 ± 5.3 | 0.670 | |
| p value | 0.463 | 0.337 | ||
| Self-treatment | ||||
| None | 9.6 ± 4.6 | 6.9 ± 4.1 | 0.022 | |
| Analgesics | 9.5 ± 4.5 | 8.1 ± 4.6 | 0.132 | |
| Antibiotics and analgesics | 8.0 ± 4.5 | 8.4 ± 6.4 | 0.712 | |
| p value | 0.138 | 0.401 | ||
| Visits only for emergencies | ||||
| Yes | 7.9 ± 3.4 | 7.9 ± 5.1 | 0.997 | |
| No | 8.6 ± 4.5 | 7.9 ± 5.8 | 0.319 | |
| p value | 0.435 | 0.966 | ||
| Domain of disease determinants | ||||
| Systemic diseases | ||||
| Yes | 9.4 ± 5.2 | 11.8 ± 9.6 | 0.263 | |
| No | 8.4 ± 4.3 | 7.5 ± 4.5 | 0.103 | |
| p value | 0.244 | 0.006 | ||
| Dental diseases – total numbers of DMFT | ||||
| Lowest 1/3 of DMFT scores | 8.3 ± 3.6 | 7.4 ± 4.3 | 0.609 | |
| Middle 1/3 of DMFT scores | 9.4 ± 5.0 | 7.2 ± 5.4 | 0.057 | |
| Highest 1/3 of DMFT scores | 8.6 ± 4.8 | 9.4 ± 6.5 | 0.057 | |
| p value | 0.505 | 0.189 | ||
| Periodontal diseases | ||||
| No | 7.4 ± 3.6 | 6.0 ± 1.2 | 0.193 | |
| Yes | 8.9 ± 4.2 | 6.9 ± 5.2 | 0.069 | |
| p value | 0.168 | 0.444 | ||
Values are expressed as mean ± SD. DMFT = Decayed, missing and filled teeth.
ANOVA with post hoc Bonferroni adjustment/independent samples t test was used.
Statistical Analysis
Statistical analysis was performed using SPSS version 21.0 software, and the threshold for statistical significance was set at p < 0.05. Univariate statistics was used to test the data for normality in preparation for the inferential statistics. Given that data were normally distributed, the parametric tests were used for subsequent analysis. The bivariate analysis included the independent samples t test for the comparison of two groups and ANOVA with post hoc Bonferroni adjustment for the comparison of three or more groups. Linear multiple regression (LMR) models were used for the multivariate analysis.
Results
Of 285 patients with AOMIs, 166 (58.2s%) were males and 119 (41.8s%) were females. The mean age was 41.5 ± 16.9 years (range 18–90). Of these 285 patients, 121 (42.4s%) causal teeth were lower third molars.
The mean LOH stay was 8.3 ± 4.9 days (range 2–29). The determinants for the provision of OPUC for patients with severe AOMIs who sought such care in different treatment facilities and locations throughout the country are shown in table 2. Of the 285 patients with severe AOMIs, 150 (52.6s%) sought professional dental care prior to hospitalization; 121 (81.1s%) of them arrived at the hospital the same day, while the remaining 29 (19.9s%) delayed their hospitalization for different reasons for up to almost 1 week. There was no statistically significant difference in the LOH between the patients who sought OPUC (8.8 ± 4.6 days) and the patients who did not seek OPUC (7.9 ± 5.2 days) for their urgent dental condition (p = 0.254). Of the 150 patients with AOMIs who sought professional dental care prior to hospitalization, 144 (96.0s%) were accessed at the OPUC the same day.
Table 2.
LOH in relation to OPUC for patients with AOMIs
| Determinant of OPUC | LOH, days |
|||
|---|---|---|---|---|
| n | mean ± SD | range | significance p value* |
|
| Receiving OPUC due to AOMIs | ||||
| No OPUC | 135 (47.4)a | 7.9 ± 5.2 | 2 – 29 | |
| OPUC in a public clinic | 134 (47.0)a | 8.8 ± 4.6 | 2 – 26 | 0.254 |
| OPUC in a private clinic | 16 (5.6)a | 7.8 ± 3.6 | 4 – 15 | |
| Time of accessing OPUC | ||||
| Same day | 144 (96.0)B | 8.7 ± 4.6 | 2 – 26 | |
| Next day | 4 (2.7)B | 7.5 ± 3.5 | 4 – 11 | 0.598 |
| After > 2 days | 2 (1.3)B | 9.0 ± 8.8 | 3 – 15 | |
| Time of receiving OPUC | ||||
| <0.5 h | 28 (18.9)B | 8.6 ± 4.2 | 3 – 17 | 0.580 |
| Within 1 h | 8 (5.4)B | 10.9 ± 4.5 | 5 – 17 | |
| Within 2 h | 75 (50.7)B | 8.5 ± 5.0 | 2 – 26 | |
| Within 3 h | 37 (25.0)B | 8.5 ± 3.8 | 4 – 23 | |
| Costs of OPUC | ||||
| Free | 89 (60.1)B | 8.8 ± 4.9 | 3 – 23 | |
| <10 EUR | 39 (26.4)B | 8.7 ± 4.3 | 2 – 26 | |
| 11 – 15 EUR | 5 (3.4)B | 8.2 ± 3.6 | 5 – 13 | 0.817 |
| 16 – 35 EUR | 4 (2.7)B | 9.8 ± 4.5 | 2 – 15 | |
| >36 EUR | 11 (7.4)B | 7.2 ± 3.3 | 4 – 15 | |
| Seeking hospitalization after referral from OPUC | ||||
| Same day | 120 (81.1)B | 8.7 ± 4.4 | 2 – 23 | |
| Next day | 11 (7.4)B | 8.6 ± 4.5 | 5 – 17 | |
| Within 2 days | 7 (4.7)B | 7.0 ± 2.1 | 4 – 9 | 0.761 |
| Within 3 days | 7 (4.7)B | 10.29 ± 7.7 | 4 – 26 | |
| Within 1 week | 3 (2.0)B | 9.3 ± 6.7 | 5 – 17 | |
| Time from the start of acute clinical symptoms due to AOMIs prior to hospitalization | ||||
| <3 days | 89 (31.2)B | 8.2 ± 4.6 | 2 – 26 | 0.864 |
| »4 days | 196 (68.8)B | 8.3 ± 5.0 | 2 – 29 | |
ANOVA with post hoc Bonferroni adjustment/independent samples t test was used.
Percentages of the total sample of hospitalized patients with AOMIs.
Percentages of the total sample of patients receiving primary care in outpatient facilities prior to hospitalization.
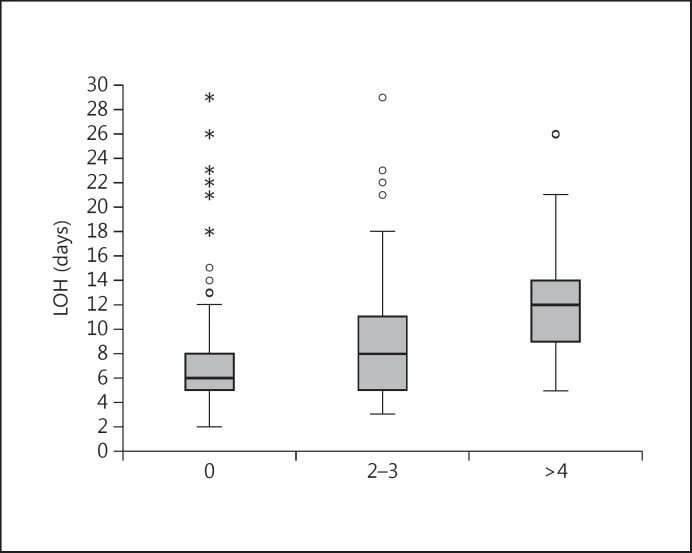
Overall, there were no statistically significant differences in the LOH among the patients who sought professional care immediately (8.7 ± 4.7 days) and those who delayed (9.0 ± 8.8 days) seeking care from professionals in outpatient treatment facilities. Of the 150 patients, 130 (86.5s%) did not have any or had little OPUC-related costs. For all patients with AOMIs who visited OPUC facilities, the LOH and the characteristics of infection severity are presented in table 3. The direct determinants for disease severity were the number of anatomical spaces involved in and the extension of AOMIs, while the indirect determinants were the type of anesthesia used or the type of incision required to drain AOMIs. These determinants were statistically significantly associated with a longer LOH (p < 0.001). The LOH among patient groups with a varying number of anatomical spaces involved in AOMIs is shown in figure 1. Patients with 1 anatomical space had an overall shorter (p < 0.001) hospital stay than those with ≥2 spaces.
Table 3.
Hospitalization of patients with AOMIs
| Domain of severity of AOMIs | LOH, days* | |||
|---|---|---|---|---|
| n | mean ± SD* | range | significance p value |
|
| Anatomical spaces involved in AOMIs | ||||
| 1 | 175 (61.4) | 7.0 ± 4.0 | 2–29 | |
| 2 – 3 | 63 (22.1) | 9.1 ± 5.5 | 2–29 | <0.001 |
| ≥4 | 47 (16.5) | 12.1 ± 4.8 | 4–26 | |
| Extension of AOMIs | ||||
| Unilateral | 267 (93.7) | 7.9 ± 4.5 | 2–29 | <0.001 |
| Bilateral | 18 (6.3) | 15.1 ± 5.6 | 8–29 | |
| Anesthesia for incisions of AOMIs | ||||
| Local | 209 (73.3) | 6.9 ± 3.8 | 2–29 | <0.001 |
| General | 76 (26.7) | 12.4 ± 5.2 | 4–29 | |
| Incision for draining AOMIs | ||||
| Intraorally | 94 (33.3) | 5.9 ± 2.2 | 2–15 | <0.001 |
| Extraorally | 191 (67.0) | 9.6 ± 5.3 | 2–29 | |
| Complications of AOMIsa | ||||
| No | 281 (98.6) | 8.38 ± 4.9 | 2–29 | 0.738 |
| Yes | 4 (1.4) | 7.5 ± 2.4 | 3–14 | |
Values in parentheses indicate percentages calculated from the total sample of hospitalized patients with AOMIs.
ANOVA with post hoc Bonferroni adjustment/independent samples test was used.
All patients who developed life-threatening complications were immediately transferred to central medical hospitals.
Fig. 1.
Anatomical spaces involved in AOMIs.
The 5-year cumulative incidence rate (1.4s%) of complications (mediastinitis and/or sepsis) due to AOMIs is presented in table 3. The LOH at the University Dental Hospital was nonsignificantly shorter for patients with complications than for those without.
Lifestyle and disease domains are reported in table 1, showing two types of vertical comparisons for the patients: those who received prior outpatient urgent care (first column) and those who did not receive prior outpatient urgent care (second column). The horizontal comparisons report the LOH between similar patient subgroups, exemplified by smokers who used OPUC and those who did not use it (p = 0.393). There was only one statistically significant association: patients who sought outpatient urgent care prior to hospitalization and who did not treat themselves had a statistically significantly shorter (p = 0.022) LOH as compared to their counterparts who treated themselves.
Concerning disease domains, among the patients with AOMIs who were hospitalized without a prior OPUC, patients with coexisting systemic diseases had a statistically significantly longer LOH (p = 0.006) than those who did not have systemic diseases. Diabetic patients had a similar LOH (9.2 ± 6.8 days) as compared to patients with other systemic diseases but without diabetes (9.2 ± 5.6 days). Regarding the severity of either dental diseases or periodontal diseases, no statistically significant associations with LOH were found.
The joint effects of multiple determinants as measured by multivariate analysis are reported in table 4. The dependent outcome in multivariate analyses was the LOH. The multivariate testing was performed in two steps. Firstly, the risk determinants were tested employing four separate LMR analyses for each of the four domains: (1) OPUC, (2) the severity of AOMIs, (3) lifestyle, and (4) the disease domains. Then, the determinants from all four domains were tested in a joint LMR analysis.
Table 4.
Determinants of LOH due to AOMIs by LMR
| Outcomes of LOH | ß coefficient | p value | Tolerance |
|---|---|---|---|
| Predictors: domain of OPUC. Selection of predictors: enter. Model summary: p = 0.642, adjusted R2 = 0.030 | |||
| Receiving OPUC | 0.058 | 0.500 | 0.948 |
| Accessing OPUC | 0.091 | 0.292 | 0.933 |
| Costs of OPUC | 0.018 | 0.850 | 0.742 |
| Seeking hospitalization after referral from OPUC | 0.074 | 0.440 | 0.749 |
| Time from the start of symptoms to hospitalization | 0.101 | 0.263 | 0.853 |
| Predictors: domain of severity of AOMIs. Selection of predictors: enter. Model summary: p < 0.001, adjusted R2 = 0.253 | |||
| Anatomical spaces involved in AOMIs | 0.218 | <0.001 | 0.709 |
| Extension of AOMIs | 0.242 | <0.001 | 0.868 |
| Incisions for draining AOMIs | 0.215 | <0.001 | 0.789 |
| Predictors: domain of disease determinants. Selection of predictors: enter. Model summary: p = 0.241, adjusted R2 = 0.042 | |||
| Systemic diseases | 0.159 | 0.118 | 0.964 |
| Dental diseases | 0.074 | 0.476 | 0.926 |
| Periodontal diseases | 0.132 | 0.193 | 0.958 |
| Predictors: domain of lifestyle determinants. Selection of predictors: enter. Model summary: p = 0.546, adjusted R2 = 0.013 | |||
| Smoking | 0.042 | 0.537 | 0.906 |
| Oral self-care | 0.026 | 0.691 | 0.975 |
| Self-treatment when having oral pain | 0.095 | 0.147 | 0.967 |
| Dental visits only for urgency | 0.020 | 0.764 | 0.892 |
| Predictors: all domains. Selection of predictors: stepwise. Model summary: p < 0.001, adjusted R2 = 0.249 | |||
| Extension of AOMIs | 0.352 | <0.001 | 0.955 |
| Incision (extraoral vs. intraoral) | 0.298 | 0.002 | 0.955 |
Comparing the first four LMR models, one for each of the four domains, the only statistically significant LMR model was for the AOMI severity domain. The final joint LMR model simultaneously assessing all determinants found that extension of the acute odontogenic infection (direct indicator of severity) and use of an incision to drain the AOMIs (indirect indicator of infection severity) were the best statistically significant predictors for the longer LOH. These two predictors jointly explained 24.9s% (R2 = 0.249) of the variation in the LOH.
Discussion
The present finding that acute odontogenic infections most frequently involved the third lower molars is consistent with findings from different countries [11,12,13,16,17]. Consequently, drainage of infections is easier and the healing period shorter for patients who have AOMIs involving teeth from the upper jaw, as compared to patients with AOMIs in the lower jaw. This may be explained by anatomical and bone-related differences between the two jaws. Possibly, gravitational forces lead to a better drainage of acute odontogenic infections in the upper jaw as compared to the lower jaw [14]. Other possible explanations are the higher bone density [18] in the lower jaw and a better blood supply in the maxilla [14]. The longer hospitalization time used to treat acute odontogenic infections in the lower jaw compared to the upper jaw was reported elsewhere [13,19].
The longer hospitalization time associated with coexisting systemic diseases confirmed those of previous studies regarding the involvement of, for example, diabetes [6], patients' older age [20], self-medication and delayed presentation at the hospital [1]. Therefore, timely management of acute odontogenic infections is necessary not only to avoid local complications but also to minimize systemic complications or death [21,22].
The mean LOH of 8.3 days for patients with AOMIs at the University Hospital was within the range of 3.9–9.2 days reported previously from different countries: Iran: 9.2 days [14]; Italy: 5.2 days [23], and USA: 3.9 [3] and 5.1 days [24]. Multicenter studies might be needed to understand why the LOH due to severe AOMIs varies among countries. The shorter hospitalization at the University Dental Hospital for the patients with complications is explained by the fact that, following the Lithuanian Medical System guideline, all patients who develop life-threatening complications are immediately transferred to specialized central medical hospitals.
In Lithuania, the averaged annual (2009–2013) incidence rate of <0.5s% for life-threatening complications due to AOMIs was relatively low. Possibly, this relatively low incidence rate could be attributed to the Lithuanian law that stipulated that primary urgent care should be provided within a relatively short time upon arrival to a treatment facility [25].
It is important to point out that there were no statistically significant differences in the LOH between the patients who sought OPUC treatment facilities prior to their hospitalization and those who were hospitalized without any prior outpatient primary care. These findings indicate that both groups of patients with AOMIs despite the type of urgent primary care they sought, either outpatient or hospital, received timely professional help.
Conclusions
The most important determinants of a hospitalization stay of >8.3 days were indicators of infection severity such as an extension of the odontogenic infection and the need for an extraoral incision to drain the infection.
References
- 1.Igoumenakis D, Gkinis G, Kostakis G, et al. Severe odontogenic infections: causes of spread and their management. Surg Infect. 2014;15:64–68. doi: 10.1089/sur.2012.178. [DOI] [PubMed] [Google Scholar]
- 2.Marioni G, Rinaldi R, Staffieri C, et al. Deep neck infection with dental origin: analysis of 85 consecutive cases (2000–2006) Acta Otolaryngol. 2008;128:201–206. doi: 10.1080/00016480701387157. [DOI] [PubMed] [Google Scholar]
- 3.Kim MK, Nalliah RP, Lee MK, et al. Factors associated with length of stay and hospital charges for patients hospitalized with mouth cellulitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:21–28. doi: 10.1016/j.tripleo.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Staffieri C, Fasanaro E, Favaretto N, et al. Multivariate approach to investigating prognostic factors in deep neck infections. Eur Arch Otorhinolaryngol. 2014;271:2061–2067. doi: 10.1007/s00405-014-2926-5. [DOI] [PubMed] [Google Scholar]
- 5.Flynn TR, Shanti RM, Hayes C. Severe odontogenic infections, part 2: prospective outcomes study. J Oral Maxillofac Surg. 2006;64:1104–1113. doi: 10.1016/j.joms.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 6.Rao DD, Desai A, Kulkarni RD, et al. Comparison of maxillofacial space infection in diabetic and nondiabetic patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e7–e12. doi: 10.1016/j.tripleo.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Kinzer S, Pfeiffer J, Becker S, et al. Severe deep neck space infections and mediastinitis of odontogenic origin: clinical relevance and implications for diagnosis and treatment. Acta Otolaryngol. 2009;129:62–70. doi: 10.1080/00016480802008181. [DOI] [PubMed] [Google Scholar]
- 8.Petersen PE. Strengthening of oral health systems: oral health through primary health care. Med Princ Pract. 2014;23(suppl 1):3–9. doi: 10.1159/000356937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chrisopoulos S, Luzzi L, Brennan DS. Trends in dental visiting avoidance due to cost in Australia, 1994–2010: an age-period-cohort analysis. BMC Health Serv Res. 2013;13:381. doi: 10.1186/1472-6963-13-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slott SD. The role of free dental programs in care provision for the underserved. N C Med J. 2005;66:471–474. [PubMed] [Google Scholar]
- 11.Mathew GC, Ranganathan LK, Gandhi S, et al. Odontogenic maxillofacial space infections at a tertiary care center in North India: a five-year retrospective study. Int J Infect Dis. 2012;16:e296–e302. doi: 10.1016/j.ijid.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Moghimi M, Baart JA, Karagozoglu KH, et al. Spread of odontogenic infections: a retrospective analysis and review of the literature. Quintessence Int. 2013;44:351–361. doi: 10.3290/j.qi.a29150. [DOI] [PubMed] [Google Scholar]
- 13.Saito CT, Gulinelli JL, Marao HF, et al. Occurrence of odontogenic infections in patients treated in a postgraduation program on maxillofacial surgery and traumatology. J Craniofac Surg. 2011;22:1689–1694. doi: 10.1097/SCS.0b013e31822e5c8d. [DOI] [PubMed] [Google Scholar]
- 14.Pourdanesh F, Dehghani N, Azarsina M, et al. Pattern of odontogenic infections at a tertiary hospital in Tehran, Iran: a 10-year retrospective study of 310 patients. J Dent (Tehran) 2013;10:319–328. [PMC free article] [PubMed] [Google Scholar]
- 15.Sato FR, Hajala FA, Freire FW, et al. Eight-year retrospective study of odontogenic origin infections in a postgraduation program on oral and maxillofacial surgery. J Oral Maxillofac Surg. 2009;67:1092–1097. doi: 10.1016/j.joms.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Cachovan G, Phark JH, Schon G, et al. Odontogenic infections: an 8-year epidemiologic analysis in a dental emergency outpatient care unit. Acta Odontol Scand. 2013;71:518–524. doi: 10.3109/00016357.2012.696694. [DOI] [PubMed] [Google Scholar]
- 17.Sanchez R, Mirada E, Arias J, et al. Severe odontogenic infections: epidemiological, microbiological and therapeutic factors. Med Oral Patol Oral Cir Bucal. 2011;16:e670–e676. doi: 10.4317/medoral.16995. [DOI] [PubMed] [Google Scholar]
- 18.Hwang T, Antoun JS, Lee KH. Features of odontogenic infections in hospitalised and non-hospitalised settings. Emerg Med J. 2011;28:766–769. doi: 10.1136/emj.2010.095562. [DOI] [PubMed] [Google Scholar]
- 19.Ozsurekci Y, Tekcicek M, et al. Length of hospital stay and management of facial cellulitis of odontogenic origin in children. Pediatr Dent. 2014;36:18E–22E. [PubMed] [Google Scholar]
- 20.Chi TH, Tsao YH, Yuan CH. Influences of patient age on deep neck infection: clinical etiology and treatment outcome. Otolaryngol Head Neck Surg. 2014;151:586–590. doi: 10.1177/0194599814542589. [DOI] [PubMed] [Google Scholar]
- 21.Seppänen L, Lauhio A, Lindqvist C, et al. Analysis of systemic and local odontogenic infection complications requiring hospital care. J Infect. 2008;57:116–122. doi: 10.1016/j.jinf.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Antunes AA, Avelar RL, de Melo WM, et al. Extensive cervical necrotizing fasciitis of odontogenic origin. J Craniofac Surg. 2013;24:e594–e597. doi: 10.1097/SCS.0b013e31829ad57b. [DOI] [PubMed] [Google Scholar]
- 23.Boffano P, Roccia F, Pittoni D, et al. Management of 112 hospitalized patients with spreading odontogenic infections: correlation with DMFT and oral health impact profile 14 indexes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:207–213. doi: 10.1016/j.tripleo.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Jundt JS, Gutta R. Characteristics and cost impact of severe odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:558–566. doi: 10.1016/j.oooo.2011.10.044. [DOI] [PubMed] [Google Scholar]
- 25.Health Ministry of Lithuania Provision of Urgent Care in Lithuania. 4-4-2004. 12-4-2014. http://www.lrs.lt/pls/inter3/dokpaieska.showdoc_l?p_id=230805