Abstract
Objectives
To evaluate the role of pentraxin-3 (PTX-3) in determining the presence and severity of coronary atherosclerosis in patients with coronary artery disease (CAD).
Subjects and Methods
Ninety-five patients (77 males and 18 females) who underwent elective coronary angiography were enrolled in this study. Patients with heart failure, renal failure, diabetes and thyroid disease were excluded. The study population was divided into 3 groups: individuals with normal coronary arteries, patients with critical CAD (n = 35) and patients with noncritical CAD (n = 36). The association of PTX-3 levels with the presence and severity of CAD and the number of involved vessels were analyzed.
Results
The mean age was 53.40 ± 10.25 years. The PTX-3 levels were significantly higher in patients with CAD than without CAD (146.48 ± 48.52 vs. 109.83 ± 49.06 pg/ml, p < 0.001). A statistically significant difference was found among the 3 groups regarding the severity of CAD (165.66 ± 49.10, 127.83 ± 40.51 and 109.83 ± 49.06 pg/ml, p < 0.001, respectively). The serum PTX-3 levels in normal arteries were 110.4 ± 48.11 pg/ml, in single-vessel disease 132.35 ± 32.96 pg/ml, in 2-vessel disease 142.57 ± 55.88 pg/ml, in 3-vessel disease 156.07 ± 50.53 pg/ml, and in 3-vessel disease 160.50 ± 30.41 pg/ml. After adjusting for baseline confounders, older age (OR = 1.107, 95% CI = 1.027-1.193, p = 0.008) and higher PTX-3 levels (OR = 1.017, 95% CI = 1.003-1.032, p = 0.021) were detected as significant predictors for the presence of CAD.
Conclusions
Higher PTX-3 levels were associated with the presence of CAD and its increased severity in clinically stable patients. Higher PTX-3 levels may be regarded as a novel diagnostic predictor and may offer therapeutic options in the clinic.
Key Words: Coronary angiography, Coronary artery disease, Pentraxin-3
Introduction
Coronary artery disease (CAD) is the leading cause of death for adults in industrialized countries [1]. It has also been reported that this entity will rank first among the causes of death in developing countries in the immediate future [1]. Based on the data from the Turkish Adult Risk Factor Study (TEKHARF), which is the most comprehensive study conducted in Turkey on this subject, CAD ranks first among the causes of death for adults [2].
Inflammation plays an important role at each stage of the development of coronary atherosclerosis [3]. Therefore, many studies have been carried out on the relationship between inflammatory markers and the development of cardiovascular disease (CVD) [3,4]. The acute phase reactant C-reactive protein (CRP) is the most recognized marker for this purpose. CRP accumulations have been detected in atherosclerotic lesions, and serum CRP levels have been positively correlated with the risk of CVD in both healthy individuals and individuals at high risk [5]. CRP is a member of the pentraxin (PTX) family that shares a characteristic pentameric structure, and it is synthesized by the liver in response to inflammatory processes and is a nonspecific indicator of inflammation [5,6,7,8,9].
Recent studies have commonly focused on pentraxin-3 (PTX-3) which is the first member of the long PTX group. PTX-3 is synthesized by monocytes and macrophages, vascular endothelial cells, fibroblasts and smooth muscle cells in response to inflammatory stimulants such as tumor necrosis factor-α, interleukin-1 and lipopolysaccharides. The cells PTX-3 originates from are directly involved in atherosclerosis. Therefore, PTX-3 can be considered to be more specific for the development of atherosclerosis [10,11]. It is also determined as a novel inflammatory marker to be associated with the metabolic syndrome [12].
Hence, in the present study, we aimed to investigate whether or not there is any association of the serum levels of PTX-3 with the presence and severity of CAD, the number of diseased vessels based on angiographic findings in patients without any glucose metabolism disorder [diabetes mellitus (DM), impaired fasting glucose (IFG) and impaired glucose tolerance (IGT)] and chronic renal failure.
Subjects and Methods
Study Group
The present study was conducted in 95 patients who underwent an elective coronary angiographic procedure due to the suspicion of CAD in the Department of Cardiology, Gulhane Military Medical Academy, Ankara, Turkey, between July 2011 and June 2012. Then, all the patients were referred to the Outpatient Clinic's Department of Cardiology. The patients were interviewed face to face by researchers (Y.C.D., P.N., H.A.) in an observation room soon after the angiographic procedure. All patients were informed of the study protocol before the face-to-face interview, and they signed the informed consent form. The institutional ethics committee approved this study.
Laboratory Tests
Before the angiographic procedure, the following routine test results were recorded: fasting blood glucose, urea, creatinine, sodium, potassium, aspartate aminotransferase, alanine aminotransferase, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, very low-density lipoprotein cholesterol, triglyceride and sedimentation as well as the results of uric acid tests and the complete blood count parameters. In order to exclude the presence of a prediabetic state and DM, a fasting oral glucose tolerance test was done at the Outpatient Clinic of Diabetes.
An exercise stress test was implemented on 65 participants. Coronary angiography was performed in those patients with a variety of complaints (chest pain, palpitation, shortness of breath and reduction in effort capacity), with ECG findings or who had been referred for stent control. All participants were clinically stable. The procedure was performed by a specialist cardiologist (C.B.) through the right femoral artery using standard methods. In cases of the presence of a peripheral artery disease in the lower extremities or when a guidewire failed to move forward, the left femoral artery or radial artery was used. The procedures were done using a Philips Integris 3000 angiography device (Philips Medical Systems, Best, The Netherlands).
The patients were assessed both in terms of the presence and the intensity of their CAD based on the findings of the coronary angiography. The number of coronary arteries was classified anatomically regarding the involvement of stenotic lesions [13]. Coronary artery stenoses of 50% (at least 1 of 4 coronary arteries: left coronary artery, left anterior descending artery, circumflex artery and right coronary artery) were classified as critical CAD, and stenoses of <50 % were classified as noncritical CAD. According to this classification, 35 patients with ≥50% stenosis in coronary arteries (at least 1 artery), 36 patients with >50% stenosis and 24 CAD-free subjects (with no stenosis) were included.
The exclusion criteria were: patients with a known disorder of the glucose metabolism (DM, IGT, IFG) or any disorder of the glucose metabolism (DM, IGT, IFG) detected according to the results of the fasting oral glucose tolerance test, patients with manifest renal insufficiency (glomerular filtration rate ≤60 ml/min/1.73 m2), patients who had had an acute coronary event [myocardial infarction (MI), stroke etc.] before the coronary angiography (within the last 3 months), patients with a thyroid function disorder, patients with an erythrocyte sedimentation rate of >20 mm/h, which is measured routinely before the angiographic procedure, and patients younger than 20 years old and older than 70 years old. The glomerular filtration rate was calculated by using the Cockcroft-Gault and MDRD (Modification of Diet in Renal Disease) formulae.
PTX-3 Measurement Method
The ELISA method was used to measure the serum PTX-3. The measurements were carried out by using human PTX-3 ELISA kits (Quantakine DPTX 30) in the Bio-Tek reader of the Department of Biochemistry of the Gulhane Military Medical Academy. The human PTX-3 ELISA kit measures the PTX-3 values in serum and plasma (EDTA, citrate, heparin) in line with the sandwich enzyme immunoassay principle. The references, quality control and study samples were incubated in antihuman PTX-3 antibody-coated wells. Following the process of incubation, washing and conjugation, an absorbance-related standard curve was plotted depending on the PTX-3 concentration. The unknown PTX-3 values of the samples were calculated using this curve. Using the human PTX-3 ELISA kit, the reference range for PTX-3 is 7-116 pg/ml.
Statistical Analysis
The data obtained were analyzed using the statistical package program SSPS15.0 for Windows (Chicago, Ill., USA). In the statistical analyses, the descriptive analyses were given as numbers and percentages for categorical variables and as means ± standard deviation or medians with ranges for continuous variables. The coherence of the normally distributed data was evaluated using the Kolmogorov-Smirnov test. An ANOVA test and a Bonferroni test as a post hoc test were performed for the multiple group comparisons of the parameters which were normally distributed. The Student t test was used for the comparison of the 2 CAD risk groups. For the parameters which were not consistent with normal distribution, the Kruskal-Wallis test was used for multiple group comparisons and the Bonferroni-adjusted Mann-Whitney U test was used for further comparisons between the 2 groups. Interdata relationships were assessed using the Pearson or Spearman correlation tests. A p value of <0.05 was considered statistically significant. A receiver operating characteristic curve was plotted to estimate the effects of the variables on the CAD state. The factors which are considered to affect CAD were assessed by using the backward logistic regression model.
Results
The mean age was 53.40 ± 10.25 years, and 77 of the patients were male. While overall, the mean age of the group with critical CAD was 57.2 ± 9.95, in the group with noncritical CAD it was 54.19 ± 9.44 and in the healthy controls 46.67 ± 8.81, and the difference in the mean age between the groups was statistically significant (p < 0.001). The causes of admission for coronary angiography were chest pain and dyspnea, stent control, follow-up visit of a previous acute coronary syndrome (at least 3 months earlier), primary percutaneous transluminal coronary angioplasty, palpitation, suspicious exercise ECG results and a strong family history as shown in table 1.
Table 1.
Descriptive statistics for all patients (n = 95)
| Frequency | % | |
|---|---|---|
| Gender, male | 77 | 81.1 |
| Family history of CAD | 59 | 62.1 |
| HT | 33 | 34.7 |
| Dyslipidemia | 83 | 87.4 |
| Smoking status | ||
| No smoking | 27 | 28.4 |
| Exsmoker | 45 | 47.4 |
| Current smoker | 23 | 24.2 |
| Reason for coronary angiography | ||
| Chest pain and dyspnea | 67 | 70.5 |
| Follow-up after ACS | 4 | 4.2 |
| Stent control | 7 | 7.4 |
| Otders | 17 | 17.9 |
| Age, years | 53.40 ± 10.25 | |
| BMI | 27.54 ± 5.08 | |
| GFR, ml/min/1.73 m2 | 74.37 ± 10.66 | |
| OGTT0, mg/dl | 94.79 ± 12.24 | |
| OGTT120, mg/dl | 111.97 ± 23.20 |
Values represent n and % or mean ± SD. ACS = Acute coronary syndrome; GFR = glomerular filtration rate; HT = hypertension; OGTT0 and OGTT120 = 0- and 2-hour values of an oral glucose tolerance test, respectively.
The assessment of the presence of CAD alone revealed that while 24 (25.3%) of the patients were healthy, 71 (74.7%) of the patients were diagnosed with CAD. Of the 71 patients with CAD, stenosis of ≥50% was detected in 35 (49.3%) patients and stenosis of <50% in 36 (50.7%) patients. Of the 71 patients with CAD, 59 (83.1%) were males and 12 (16.9%) females. Of the 24 CAD-free patients, 18 (75%) were males and 6 (25%) were females. In the cases of severe stenosis of ≥50% based on coronary angiography, 19 (20%) patients had single-vessel disease, 12 (16.7%) had 2-vessel disease, 3 (3.2%) had 3-vessel disease, and 1 (1.1%) patient had 4-vessel disease.
Of the 48 patients with a positive exercise test performed before the angiographic procedure, an artery involvement of ≥50% was detected in 19 (39.6%) of the patients, a <50% involvement in 17 (35.4%) of the patients and a normal coronary artery in 12 (25%) of the patients. In the 17 patients with a negative exercise test, a coronary artery involvement of ≥50% was detected in 29.4% of the patients (n = 5), a <50% involvement was detected in 47.1% (n = 8) of the patients, and a normal coronary artery anatomy was detected in 23.5% (n = 4) of the patients.
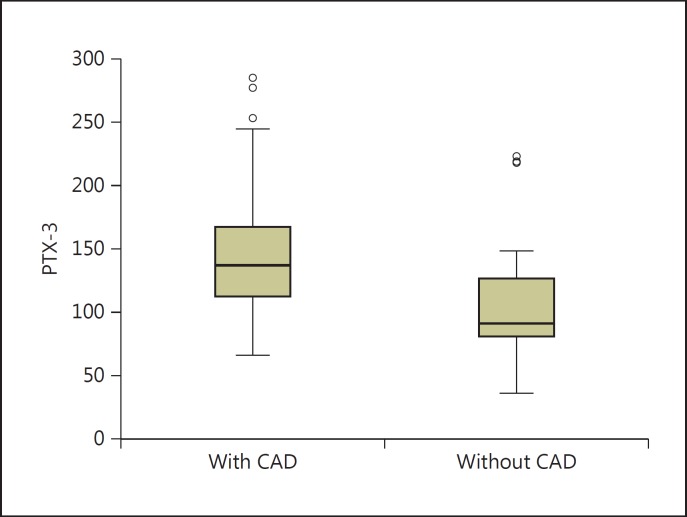
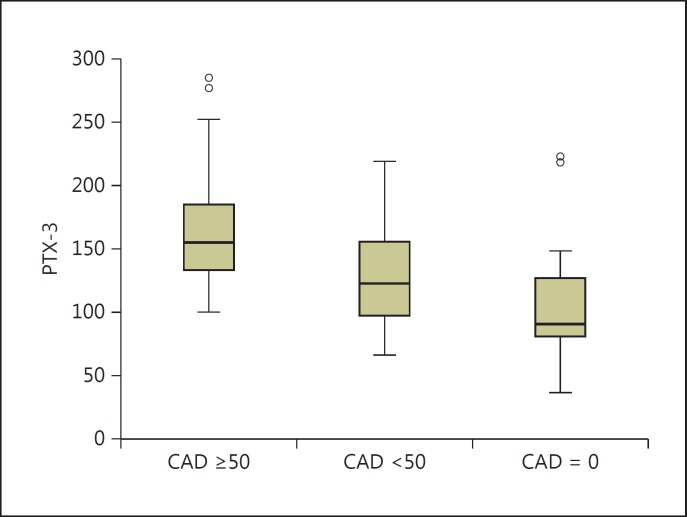
Regarding the presence of CAD, the mean PTX-3 level was 109.83 ± 49.06 in the CAD-free group, and 146.48 ± 48.52 in the group with CAD. The difference was statistically significant (p = 0.002) (fig. 1). The mean PTX-3 level was found to be 165.66 ± 49.10 pg/ml in the critical CAD group, 127.83 ± 40.51 pg/ml in the noncritical CAD group and 109.83 ± 49.06 pg/ml in the CAD-free group. The difference was also statistically significant (p < 0.001) (fig. 2) based on the comparison between the CAD-free group and the critical group.
Fig. 1.
Comparison of the mean PTX-3 levels according to the presence of CAD.
Fig. 2.
Comparison of the mean PTX-3 levels according to the severity of CAD.
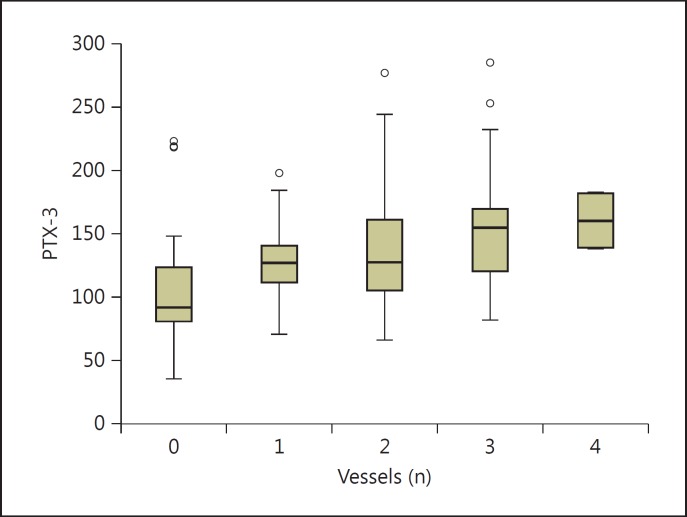
The mean PTX-3 values by the number of the diseased vessels were as follows: CAD-free group, 110.40 ± 48.11 pg/ml; single-vessel involvement group, 132.35 ± 32.96 pg/ml; 2-vessel involvement group, 142.57 ± 55.88 pg/ml; 3-vessel involvement group, 156.07 ± 50.53 pg/ml, and 4-vessel involvement group 160.50 ± 30.41 pg/ml. The difference in PTX-3 levels among the groups by the number of the diseased vessels was found to be statistically significant (p = 0.018) (fig. 3).
Fig. 3.
Comparison of the PTX-3 levels by the number of the vessels revealing coronary involvement.
The mean PTX-3 values were assessed according to the total number of severely atherosclerotic vessels (≥50%). The mean PTX-3 values were found to be 120.63 ± 44.62, 166.42 ± 47.96, 165.42 ± 55.63 and 170.67 ± 53.58 pg/ml in the <50% stenosis, single-vessel, 2-vessel and 3- vessel CAD groups, respectively. The standard deviation could not be calculated, since the 4-vessel CAD group included only 1 patient. Intergroup comparisons based on the number of severely atherosclerotic vessels (≥50%) revealed statistically significant differences in the PTX levels (p = 0.001).
The patients were divided into 2 CAD risk groups, above and below 50 years of age. While the patients younger than 50 years of age accounted for 41.1% of the patients (n = 39), 58.9% (n = 56) of the patients were older than 50 years of age. The mean PTX-3 level was found to be 125.85 ± 47.91 pg/ml in the group of patients younger than 50 years of age and 145.15 ± 51.95 pg/ml in the group of patients older than 50 years of age. No statistically significant difference in the PTX-3 levels was found between these groups (p = 0.069).
The mean PTX-3 level was found to be 143.90 ± 53.05 pg/ml in the group of male patients and 108.67 ± 26.92 pg/ml in the group of female patients. A statistically significant difference in the PTX-3 levels was found between these 2 groups (p = 0.008).
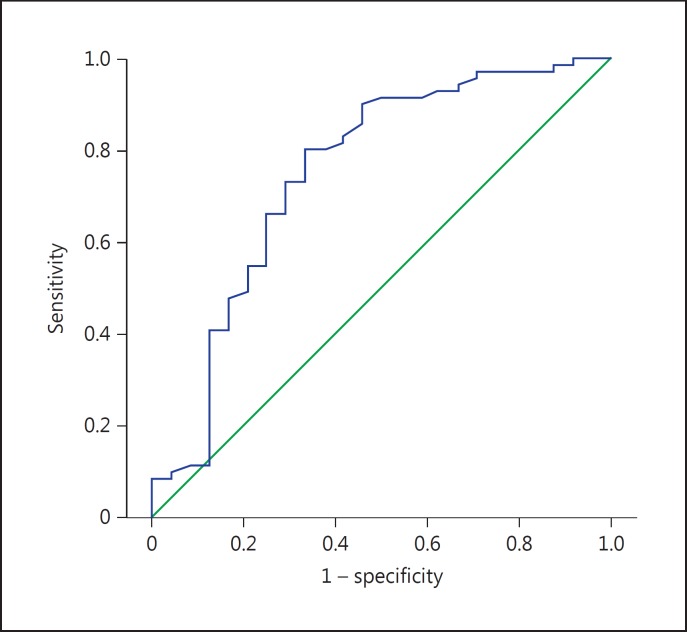
The highest sum of sensitivity and specificity was identified as the cutoff point in determining the presence or absence of CAD, and the sensitivity and specificity of a PTX-3 value of 117 pg/ml were found as 73.2 and 70.8%, respectively. The area under the receiver operating characteristic curve was calculated to be 0.751 (fig. 4).
Fig. 4.
Sensitivity and specificity graph for PTX-3 and the receiver operating characteristic curve.
A multivariate logistic regression analysis revealed that after adjusting for baseline confounders (gender, smoking status, BMI, glomerular filtration rate, 0- and 2-hour values of the fasting oral glucose tolerance test, hypertension, dyslipidemia, family history of CAD), older patients (OR = 1.107, 95% CI = 1.027-1.193, p = 0.008) and patients with higher PTX-3 levels (OR = 1.017, 95% CI = 1.003-1.032, p = 0.021) were more likely to be affected by CAD (table 2).
Table 2.
Multivariate logistic regression analysis of the predictors related to the presence of CAD
| p | OR | 95% CI | |
|---|---|---|---|
| PTX-3 | 0.021 | 1.017 | 1.003 − 1.032 |
| GFR | 0.810 | 1.007 | 0.953 − 1.064 |
| Age | 0.008 | 1.107 | 1.027 − 1.193 |
| BMI | 0.543 | 1.048 | 0.901 − 1.220 |
| Family history of CAD | 0.323 | 1.966 | 0.515 − 7.506 |
| Gender | 0.756 | 1.331 | 0.219 − 8.074 |
| HT | 0.246 | 2.743 | 0.500 − 15.066 |
| Dyslipidemia | 0.130 | 0.212 | 0.028 − 1.578 |
| OGTT0 | 0.604 | 1.012 | 0.966 − 1.061 |
| OGTT120 | 0.661 | 0.993 | 0.965 − 1.023 |
| Smoking status | |||
| Nonsmoker | Ref. | Ref. | Ref. |
| Exsmoker | 0.339 | 2.050 | 0.470 − 8.941 |
| Current smoker | 0.103 | 5.741 | 0.701 − 47.044 |
GFR = Glomerular filtration rate; HT = hypertension; OGTT0 and OGTT120 = 0- and 2-hour values of an oral glucose tolerance test, respectively.
Discussion
In this study, we hypothesized that the serum PTX-3 level might be useful for the early diagnosis of atherosclerosis and might be an easy way to diagnose the disease and determine its intensity, and we investigated whether or not there are any associations of the PTX levels with the presence and intensity of CAD in a group of stable patients who were suspected of having CAD. The analysis of the data obtained from this study revealed that the serum PTX-3 levels were higher in the patients with CAD in comparison to the patients with a normal coronary vessel anatomy. In the patients with CAD, the PTX-3 values were found to be higher in the group of patients with ≥50% stenosis compared to the group of patients with <50% stenosis. Furthermore, in the assessment based on the number of the severely diseased (≥50% stenosis) vessels, the serum PTX-3 levels were higher in patients with CAD compared to the patient group with a normal coronary anatomy. After adjusting for the baseline confounders, old age and higher PTX-3 levels were determined as significant predictors of CAD.
The researches on the association of clinical atherosclerotic events with serum PTX-3 levels have become more significant following immunohistochemical studies which revealed that the plasma PTX-3 levels were increased in atherosclerotic lesions, but not in nonatherosclerotic lesions, and that PTX-3 was an indicator of localized vessel inflammation and damage. In addition, the higher levels of PTX-3 of the patients with ST-elevation MI or subclinical CAD compared to the CAD-free individuals led researchers to focus on the PTX-3 levels in these groups of patients.
In the light of these basic studies, new researches have been conducted on the use of PTX-3 in clinical practice. In a study with a similar design to our study, Inoue et al. [14] collected blood samples of 162 patients with diabetes mellitus, hyperlipidemia, hypertension or CVD who were on a follow-up visit at a doctor's office. Later on, the blood samples of 252 patients who underwent angiographic examination for the assessment of CAD in a university hospital were also collected, and a comparison between the mean PTX-3 levels of these 2 groups was done. The mean PTX-3 values were found to be significantly higher in patients who underwent coronary angiography with a preliminary diagnosis of ischemic heart disease as in our study. A further analysis was carried out in patients who underwent an angiographic procedure for being suspected of having CAD. The serum PTX-3 levels of 16 patients with unstable angina pectoris (UAP) were higher than those of the control group. In the same study, although the serum PTX-3 levels of 52 patients with exercise-induced angina were higher than those of the control group, the difference was not statistically significant [14]. Since patients with diseases that might increase the PTX-3 levels, such as DM and chronic renal insufficiency, are not included in this study, the PTX-3 levels might be more specific to CAD.
While the number of the studies on PTX-3 increases, these studies also inspire the new ones. For example, Matsubara et al. [15] investigated the levels of a number of indicators, including PTX-3, in patients with heart failure, and eventually they demonstrated that only high levels PTX-3 might be accepted as an independent indicator in heart failure with a normal ejection fraction. In a large-scale study of 1,583 patients conducted by Jenny et al. [16], the association of PTX-3 with subclinic CVD and its consequences were analyzed. In that study, the PTX-3 levels were found to be higher in patients with subclinic CVD compared to CVD-free patients. Following the adjustments for the characteristics that might affect the development of CVD, such as age, sex and ethnic features, the PTX-3 levels were reassessed. While a positive correlation was found between the PTX-3 levels and CVD deaths, no significant relationship was found between the PTX-3 levels and angina, and finally these authors concluded that serum PTX levels correlated with both CVD deaths and all-cause mortality, independently from the risk factors for CRP and CVD. In a study conducted by Lee et al. [17], a group of patients with ST-elevation MI were compared to a group of patients diagnosed with UAP. An intergroup comparison revealed that in the ST-elevation MI group, the serum PTX-3 levels were statistically significantly higher than those of the UAP group. However, no significant difference in the PTX-3 levels was found between the non-ST-segment elevation MI and the UAP group. The serum PTX-3 concentration was closely associated with in-hospital death/MI as well as with death/MI within a period of 6 months. In a study conducted by Matsui et al. [18] in 2009, patients who were hospitalized due to unstable angina/non-ST-segment elevation MI, the levels of PTX-3 and N-terminal-pro-brain natriuretic peptide were independently correlated with the development of cardiac events in 26 patients within a period of observation of 6 months. The retrospective design of our study did not allow us to determine whether or not any cardiac event occurred and if so, whether or not there was any association of elevated PTX levels with the cardiac event.
The literature review of the epidemiological studies investigating the relationship between CAD and PTX-3 levels revealed that the PTX-3 levels were measured in the blood samples, mostly obtained during or immediately after an acute event, such as acute MI. In this study, serum PTX-3 was measured in the serum samples of patients who were suspected of having CAD, 5-10 days after an elective coronary angiography. Unlike the aforementioned studies, this study did not include a prospective follow-up of the patients, and subsequent cardiovascular events could not be assessed on the basis of the PTX-3 levels. However, the correlations between the PTX-3 values and the degree of coronary artery stenosis determined on the basis of coronary angiography as well as inflammatory indicators in CAD patients were in line with similar studies. Among the 3 groups of patients classified based on the degree of the stenosis in the coronary arteries (degree of stenosis in the coronary artery of ≥50%, with <50% in normal coronary arterial anatomy), the lowest mean PTX-3 level was in the group of patients with a normal coronary anatomy, and the highest mean PTX-3 level was in the group with CAD group with an atherosclerotic stenosis rate of ≥50%. This data was also consistent with the data previously reported in literature.
Limitations of the Study
In some of the aforementioned studies, the patients with CAD were prospectively followed up, and the risk for the development of secondary cardiovascular events (MI, death, stroke) was assessed with respect to the actual PTX-3 levels. Since our study was not a follow-up study, we could not carry out such an assessment. Furthermore, in the study sampling, factors that might affect CAD were reduced by excluding chronic renal insufficiency, thyroid dysfunction, earlier period of MI (<3 months) and glucose metabolism disorders (IGT, IFG, DM) in particular. Therefore, the size of the study sample is small. Future epidemiological studies with a larger study sample, excluding diseases and conditions accompanying CAD, will provide further evidence for PTX-3 to be an indicator for the presence and intensity of CAD.
Conclusion
Higher levels of PTX-3 were significantly associated with the presence of CAD and its increased severity in these clinically stable patients. The present study has shown that serum PTX-3 levels may be used as an early indicator to detect the presence and intensity of CAD in primary health care centers. Future epidemiological studies with larger populations, excluding diseases and conditions accompanying CAD, will provide evidence for the use of PTX-3 as a prognostic indicator for the presence and intensity of CAD.
Disclosure Statement
The authors have no conflicts of interest to reveal.
References
- 1.World Health Report 1999 . Making a Difference. Geneva: World Health Organization; 1999. http://www.who.int/whr/1999/en/whr99_en (accessed June 25, 2014). [Google Scholar]
- 2.Onat A. Prevalence of heart disease in adults, frequency of new coronary events and death from heart disease. http://tekharf.org/images/2009/bolum2.pdf
- 3.Doganer YC, Aydogan U, Aydogdu A, et al. Relationship of cystatin C with coronary artery disease and severity. Coron Artery Dis. 2013;24:119–126. doi: 10.1097/MCA.0b013e32835b6761. [DOI] [PubMed] [Google Scholar]
- 4.George SJ, Lyon J. Pathogenesis of atherosclerosis. In: George SJ, Johnson J, editors. Atherosclerosis: Molecular and Cellular Mechanisms. Weinheim: Wiley-VCH; 2010. pp. 3–14. [Google Scholar]
- 5.Spagnoli LG, Bonanno E, Sangiorgi G, et al. Role of inflammation in atherosclerosis. J Nucl Med. 2007;48:1800–1815. doi: 10.2967/jnumed.107.038661. [DOI] [PubMed] [Google Scholar]
- 6.Norata GD, Garlanda C, Catapano AL. The long pentraxin PTX3: a modulator of the immunoinflammatory response in atherosclerosis and cardiovascular diseases. Trends Cardiovasc Med. 2010;20:35–40. doi: 10.1016/j.tcm.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Jenny NS, Tracy RP, Ogg MS, et al. In the elderly, interleukin-6 plasma levels and the −174G>C polymorphism are associated with the development of cardiovascular disease. Arterioscler Thromb Vasc Biol. 2002;22:2066–2071. doi: 10.1161/01.atv.0000040224.49362.60. [DOI] [PubMed] [Google Scholar]
- 8.Klouche M, Peri G, Knabbe C, et al. Modified atherogenic lipoproteins induce expression of pentraxin-3 by human vascular smooth muscle cells. Atherosclerosis. 2004;175:221–228. doi: 10.1016/j.atherosclerosis.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Rolph MS, Zimmer S, Bottazzi B, et al. Production of the long pentraxin PTX3 in advanced atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2002;22:10–14. doi: 10.1161/01.atv.0000015595.95497.2f. [DOI] [PubMed] [Google Scholar]
- 10.Parlak A, Aydoğan U, Iyisoy A, et al. Elevated pentraxin-3 levels are related to blood pressure levels in hypertensive patients: an observational study. Anadolu Kardiyol Derg. 2012;12:298–304. doi: 10.5152/akd.2012.092. [DOI] [PubMed] [Google Scholar]
- 11.Latini R, Maggioni AP, Peri G, et al. Prognostic significance of the long pentraxin PTX3 in acute myocardial infarction. Circulation. 2004;110:2349–2354. doi: 10.1161/01.CIR.0000145167.30987.2E. [DOI] [PubMed] [Google Scholar]
- 12.Karakas MF, Buyukkaya E, Kurt M, et al. Serum pentraxin-3 levels are associated with the severity of metabolic syndrome. Med Princ Pract. 2013;22:274–279. doi: 10.1159/000343904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sukhija R, Yalamanchili K, Aronow WS. Prevalence of left main coronary artery disease, of three- or four-vessel coronary artery disease, and of obstructive coronary artery disease in patients with and without peripheral arterial disease undergoing coronary angiography for suspected coronary artery disease. Am J Cardiol. 2003;92:304–305. doi: 10.1016/s0002-9149(03)00632-5. [DOI] [PubMed] [Google Scholar]
- 14.Inoue K, Sugiyama A, Reid PC, et al. Establishment of a high sensitivity plasma assay for human pentraxin3 as a marker for unstable angina pectoris. Arterioscler Thromb Vasc Biol. 2007;27:161–167. doi: 10.1161/01.ATV.0000252126.48375.d5. [DOI] [PubMed] [Google Scholar]
- 15.Matsubara J, Sugiyama S, Nozaki T, et al. Pentraxin 3 is a new inflammatory marker correlated with left ventricular diastolic dysfunction and heart failure with normal ejection fraction. J Am Coll Cardiol. 2011;57:861–869. doi: 10.1016/j.jacc.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Jenny NS, Arnold AM, Kuller LH, et al. Associations of pentraxin 3 with cardiovascular disease and all-cause death. The Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 2009;29:594–599. doi: 10.1161/ATVBAHA.108.178947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee DH, Jeon HK, You JH, et al. Pentraxin 3 as a novel marker predicting congestive heart failure in subjects with acute coronary syndrome. Korean Circ J. 2010;40:370–376. doi: 10.4070/kcj.2010.40.8.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsui S, İshii J, Kitagawa F, et al. Pentraxin 3 in unstable angina and non-ST-segment elevation myocardial infarction. Atherosclerosis. 2009;210:220–225. doi: 10.1016/j.atherosclerosis.2009.10.033. [DOI] [PubMed] [Google Scholar]