Abstract
Objective
The purpose of this study was to evaluate the frequency and attitude of medical students towards cleaning their stethoscopes.
Subjects and Methods
A cross-sectional study was carried out in the first week of December 2013. The study included 771 students (397 in their fourth and 374 in their sixth year) from the Faculty of Medicine, University of Belgrade, Serbia. An anonymous questionnaire was distributed to students before the start of compulsory lessons in classrooms.
Results
317 of the 397 fourth-year students (79.8%) and 306 of the 374 sixth-year students (81.9%) cleaned their stethoscope. The stethoscope diaphragm was most commonly cleaned, while the flexible tubing was the least commonly cleaned area, mainly using ethyl alcohol-based agents. The strongest positive attitude was observed for the statement ‘It is important that my stethoscope is clean’ (4.3 out of 5.0). A positive correlation (Spearman's ρ = 0.105) was observed between a higher frequency of cleaning and the stronger positive notion that a stethoscope should be cleaned.
Conclusion
A considerably high proportion of the students studied had ever cleaned their stethoscopes. Based on the students' responses, it would be useful to implement instructions on stethoscope hygiene in the regular practical curriculum with the aim of applying stethoscope disinfection in daily work.
Key Words: Stethoscope, Hygiene, Cleaning, Medical students
Introduction
The stethoscope is one of the most commonly used instruments in daily medical practice. Because of contact with remarkably large numbers of patients, contaminations with pathogenic microorganisms are frequent, both in industrialized and nonindustrialized countries [1,2,3]. Subsequently, bacterial contamination of stethoscopes may be associated with occurrence of health care-associated infections [2]. Worldwide, health care-associated infections represent a considerable health burden and are associated with increased costs of health care [4,5].
A study had shown that up to 100% of stethoscope diaphragms may be contaminated [5]. Even though stethoscopes may harbor regular skin flora (such as coagulase-negative staphylococci), they may also harbor pathogens [6]. Pathogenic bacteria most commonly found in stethoscope swabs include methicillin-resistant Staphylococcus aureus and also Pseudomonas spp., Clostridium difficile, Acinetobacter, Escherichia coli and vancomycin-resistant enterococci [2,3,7,8,9,10]. Besides the diaphragm, other parts of the stethoscope could be contaminated, such as plastic ear pieces, which may remain colonized in spite of cleansing [11]. Because of the risk of contamination and the subsequent spread of pathogenic agents, stethoscope disinfection and hygiene maintenance constitute an essential preventive strategy in hospital wards.
Hence, stethoscopes are usually cleaned using ethanol solutions. A randomized double-blind trial, with the aim to assess short- and long-term effects of 66% ethyl alcohol as a cleaning agent, had shown a high level of effectiveness and also underscored that outcomes of immediate versus daily cleaning were similar [12]. Although it has been suggested that routine cleaning with alcohol may dry out rubber seals and damage stethoscope tubing [13], there is no evidence-based reference in the current literature to support this notion. Nevertheless, most stethoscope manufacturers recommend that stethoscopes are not submerged in liquids or exposed to steam sterilization, as these could cause esthetic or functional damage and reduce acoustic quality. Despite a plethora of studies evaluating stethoscope contaminations in a variety of hospital wards, only a small number has documented the level of stethoscope cleanliness in the medical school setting [14,15]. It has been reported that medical students have a poor level of knowledge and practice of universal precaution measures [16]. However, there is a lack of information regarding current practice and teaching of stethoscope disinfection. Bearing in mind that proper education in terms of hygiene could potentially influence work-related behavior, maintaining stethoscope cleanliness should be initiated during undergraduate medical training. To the best of our knowledge, previous surveys among medical students did not report the frequency of cleaning according to specific stethoscope parts. Hence, the purpose of this study was to evaluate the frequency of stethoscope cleaning among medical students and to assess the attitude of medical students towards cleaning stethoscopes.
Material and Methods
Subjects
Fourth- and sixth-year students were recruited at the Faculty of Medicine, University of Belgrade, before the start of compulsory practical sessions in the classrooms in the period from December 2 to 9, 2013. Medical undergraduate training in the Republic of Serbia, restructured according to Bologna Process Principles [17,18], lasts for 6 years (3 years of preclinical and 3 years of clinical training). The students were introduced to patients during the first year, but their actual involvement in patient care begins in the fourth year. Therefore, we recruited students who actively used stethoscopes in hospital wards.
Four hundred and ninety-two students were enrolled in the fourth study year and 501 in the sixth study year of the Medical Faculty, making a total of 993 students. Three investigators (S.R., B.R., G.M.) introduced the study in detail to the students. Participation in the survey was anonymous. Ethics approval was obtained from the Institutional Review Board of the Faculty of Medicine, University of Belgrade. Signed informed consent was obtained from all students who agreed to participate.
Instrument
Data were collected by means of questionnaires. The questionnaire consisted of 20 items: demographic characteristics (age, gender, study year, grade point average) and stethoscope-specific questions modified from Saunders et al. [14]. Students were asked whether or not they owned a stethoscope, how frequently and what parts they kept clean as well as what type of cleaning agent they used. Answers related to attitudes towards stethoscope hygiene were graded using a Likert scale, where mark 1, denoting ‘I strongly disagree with this statement’, was the minimum and mark 5, denoting ‘I strongly agree with this statement’, was the maximum. These items examined the students' opinion as to whether they had enough time to clean their stethoscope and whether cleaning agents were readily available.
Also, students were asked whether they observed other persons cleaning their stethoscopes, and how important stethoscope hygiene was for them personally. Similarly, students were asked whether or not it was possible to transmit pathogens via stethoscopes and whether cleaning agents could damage the instrument. The final questions referred to cleaning procedures during practical classes in wards, whether they received instructions as to how to clean the stethoscope as well as whether they would want to improve their knowledge with regard to stethoscope hygiene.
Data Analysis
Attitude scores for each given statement in the questionnaire are presented as means with corresponding standard deviations, skewness and kurtosis. Skewness shows how much data weighs towards one extremity of the scale. Kurtosis refers to the convexity or flatness of data distribution. Differences in categorical variables were assessed by means of the χ2 test. Spearman's correlation test was used to investigate the association between selected variables. To assess the effect estimate for each attitude statement according to study year, univariate logistic regression was performed. In this analysis the dependent variable was study year (sixth vs. first year). The independent variable was ‘attitude score for each statement categorized as positive (marked 4 or 5 on the Likert scale)’ or ‘other’ (marked 1–3 on the Likert scale). A probability value of p < 0.05 was considered significant. The SPSS 17.0 statistical software package (SPSS Inc., Chicago, Ill., USA) was used in the statistical analysis.
Results
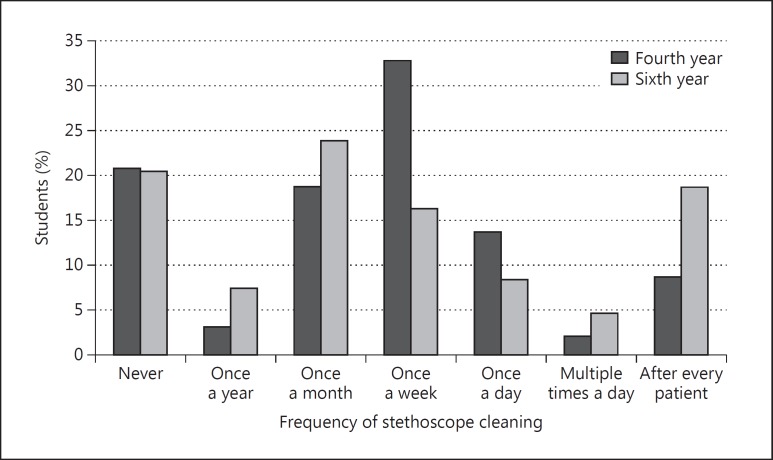
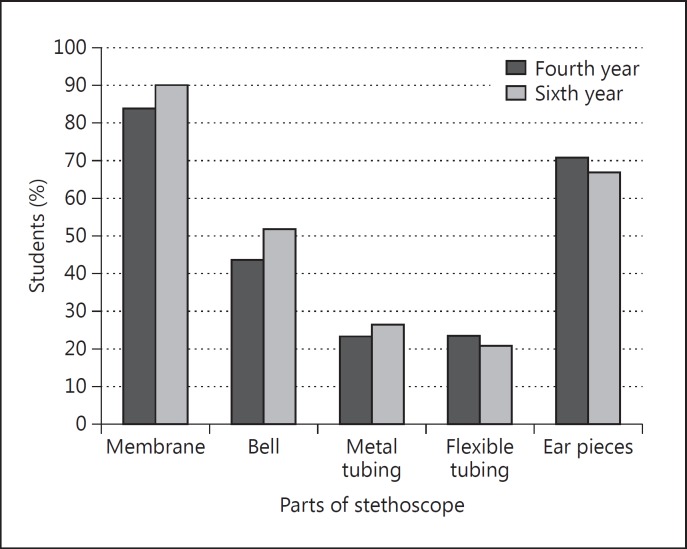
Of the 993 students who were enrolled in the study (492 in the fourth and 501 in the sixth year), 771 agreed to participate: 397 and 374 in the fourth and the sixth year, respectively. The overall response rate was 77.6% (80.7% for the fourth year and 74.6% for the sixth year). The mean age in the fourth year was 22.5 ± 1.2 years (range 21–33) and in the sixth 24.7 ± 1.7 years (range 23–37). Of the 771 students, 755 (98%) owned a stethoscope, 389 (98.0%) students in the fourth year and 370 (98.9%) in the sixth year. Three hundred and seventeen of the 397 students in the fourth year (79.8%) and 306 of the 374 in the sixth year (81.8%) had ever cleaned their stethoscopes. Frequencies of cleaning are shown in figure 1. Of those who reported stethoscope cleaning ever, over 40% (165/397) of students in the fourth year cleaned their stethoscopes at least once a day, compared with 30% (112/374) in the sixth year. Frequencies of cleaning stethoscope parts are presented in figure 2. Those who reported stethoscope cleaning most commonly cleaned the diaphragm, with 266/397 students in the fourth year (84%) and 275/397 students in the sixth year (89.9%), compared with the flexible tubing, where the numbers were 74/374 students in the fourth year (23.3%) versus 64/374 students in the sixth year (20.9%). Students usually used ethyl alcohol-based agents – 263/397 students in the fourth year (83.0%) and 270/374 students in the sixth year (88.2%) – but also a dry cloth (56/397, 9.0%), water (22/374, 3.5%) and other agents (47, 7.5%). The students' attitude towards stethoscope cleaning is given in table 1. The students expressed a strong positive attitude towards the notion to have a clean stethoscope (4.3 out of 5.0), while they expressed a negative attitude towards being shown how to properly clean their stethoscopes (1.5 out of 5.0).
Fig. 1.
Frequencies of stethoscope cleaning among medical students according to school year.
Fig. 2.
Frequency of cleaning according to specific parts of the stethoscope.
Table 1.
Students' responses to questions
| Item | Mean score ± SD | Skewness | Kurtosis |
|---|---|---|---|
| 1 I have enough time to clean my stethoscope in between examinations | 2.8 ± 1.4 | 0.113 | −1.343 |
| 2 Cleaning agents are always available | 2.5 ± 1.4 | 0.417 | −1.259 |
| 3 I regularly see others cleaning their stethoscopes | 1.8 ± 1.1 | 1.144 | 0.378 |
| 4 It is important that my stethoscope is clean | 4.3 ± 0.9 | −1.805 | 3.433 |
| 5 Various agents can be transmitted via the stethoscope | 3.8 ± 1.2 | −0.805 | −0.306 |
| 6 I heard in classes that a stethoscope should be cleaned | 2.3 ± 1.5 | 0.645 | −1.119 |
| 7 I was shown in classes how to properly clean a stethoscope | 1.5 ± 1.1 | 2.166 | 3.632 |
| 8 The stethoscope cannot be damaged after regular cleaning | 3.5 ± 1.1 | −0.260 | −0.515 |
| 9 I would like to know more about stethoscope hygiene | 3.8 ± 1.2 | −1.090 | 0.260 |
| 10 Visual reminders related to stethoscope hygiene would help me clean it regularly | 3.8 ± 1.3 | −0.888 | −0.226 |
| 11 After this survey I intend to clean my stethoscope more often | 3.7 ± 1.3 | −0.837 | −0.300 |
Strongly disagree: 1; disagree: 2; neither: 3; agree: 4; strongly agree: 5.
Students in the sixth year considered statistically significantly more often that they had enough time in between examinations to clean their stethoscope as well as that cleaning agents were readily available (table 2). Also, sixth-year students were more likely to hear in classes that stethoscopes should be cleaned (table 2). By contrast, significantly more students in the fourth year expressed willingness to clean their stethoscopes after having participated in the present survey (table 2).
Table 2.
Percentages of students who either agreed or strongly agreed with the given statements over the total number of respondents according to study year
| Item | Fourth year, Np/ Ntot | Sixth year, Np/ Ntot | OR | p |
|---|---|---|---|---|
| 1 I have enough time to clean my stethoscope in between examinations | 118/397 (29.7) | 176/372 (47.3) | 2.12 [1.58–2.85] | 0.001 |
| 2 Cleaning agents are always available | 94/396 (23.7) | 153/371 (41.2) | 2.25 [1.65–3.01] | 0.001 |
| 3 I regularly see others cleaning their stethoscopes | 28/394 (7.1) | 34/371 (9.2) | 1.32 [0.78–2.22] | 0.298 |
| 4 It is important that my stethoscope is clean | 340/396 (85.9) | 328/370 (88.6) | 1.29 [0.84–1.97] | 0.249 |
| 5 Various agents can be transmitted via the stethoscope | 263/394 (66.8) | 260/367 (70.8) | 1.21 [0.89–1.65] | 0.224 |
| 6 I heard in classes that a stethoscope should be cleaned | 96/397 (24.2) | 116/373 (31.1) | 1.41 [1.03–1.94] | 0.032 |
| 7 I was shown in classes how to properly clean a stethoscope | 32/396 (8.1) | 33/372 (8.9) | 1.11 [0.67–1.84] | 0.694 |
| 8 The stethoscope cannot be damaged after regular cleaning | 116/397 (41.8) | 168/373 (45.0) | 1.14 [0.86–1.52] | 0.367 |
| 9 I would like to know more about stethoscope hygiene | 300/396 (75.8) | 260/374 (69.5) | 0.73 [0.53–1.00] | 0.052 |
| 10 Visual reminders related to stethoscope hygiene would help me clean it regularly | 269/396 (67.9) | 247/374 (66.0) | 0.92 [0.68–1.24] | 0.578 |
| 11 After this survey I intend to clean my stethoscope more often | 264/397 (66.5) | 221/371 (59.6) | 0.74 [0.55–0.99] | 0.047 |
Figures in parentheses are percentages, those in square brackets are 95% confidence intervals. OR = Odds ratio; Np = number of students who expressed agreement or strong agreement with the given statement; Ntot = total number of respondents.
Students in the sixth year did not clean their stethoscopes more than students in the fourth year (χ2 = 0.416; p = 0.243). The level of grade point average was not correlated with ever cleaning (Spearman's ρ = −0.044, p = 0.087 for the fourth year; Spearman's ρ = 0.053, p = 0.123 for the sixth year). Being female was not associated with a higher frequency of stethoscope cleaning among students in the fourth year (Spearman's ρ = 0.102; p = 0.073), while in the sixth year we observed a positive correlation between these two variables (Spearman's ρ = 0.109; p = 0.049). In addition, students in the sixth year did not clean their stethoscopes more frequently than students in the fourth year (Spearman's ρ = 0.028; p = 0.433). A positive correlation was observed between a higher frequency of cleaning and a stronger positive notion that a stethoscope should be cleaned (Spearman's ρ = 0.105; p = 0.008). However, a higher frequency of cleaning did not correlate with a stronger positive attitude towards being shown how to clean your stethoscope (Spearman's ρ = 0.04; p = 0.915).
Discussion
The findings of this study showed that a vast majority of medical students (80.8%) had ever cleaned their stethoscopes in both fourth and sixth years. This finding suggests that students overall recognized that stethoscope cleaning should be practiced, despite having little or no formal teaching as to how to maintain a stethoscope in a hygienic condition. To date, only a few studies explored the prevalence of stethoscope cleaning in a medical student population [14,15,16]. For instance, 78.6% of medical students in Scotland reported cleaning their stethoscopes [14], which is in line with our findings. Also, a survey among 51 French students found a similar prevalence of 82% of students who clean their stethoscopes regularly or from time to time [15]. By contrast, in Pakistan, a considerably lower prevalence of stethoscope cleaning of 37.7% was observed [16]. These differences might be attributed to a distinctive cultural background and medical practice, but also to a choice of study population, as in the Pakistani survey responses of both medical students and physicians were analyzed together [16].
Although the students in our survey expressed the strongest positive attitude relative to the importance of their own stethoscope cleanliness, most students in the fourth year cleaned their stethoscopes once a week, while in the sixth year, it was done once a month. This finding is likely a result of the faculty curriculum, as the students follow a course in internal medicine in the fourth year, while in the sixth year the schedule is oriented towards other clinical courses (such as ophthalmology, otorhinolaryngology, forensic medicine, occupational medicine, clinical oncology and hygiene) that do not require regular use of a stethoscope. In our survey, approximately 11% of fourth- and 23% of sixth-year students confirmed that they cleaned their stethoscopes after examining each patient. Similarly, 13.7% of students in France performed stethoscope disinfection daily or after each patient [15]. However, Saunders et al. [14] in Scotland reported a low prevalence of 3.9% of students who apply a cleaner after each contact with a patient. These discrepancies could be a result of the ‘observer effect’ (also referred to as the Hawthorne effect) [19], defined as a circumstance in which persons improve their behavior or practice as a result of their awareness of being observed. Therefore, reporting a high prevalence of stethoscope cleaning after each patient among our students could reflect the modification and improvement of their objective cleaning practices when they found themselves in a situation to report it. Nevertheless, to provide opportunities for frequent stethoscope disinfection by use of alcohol-based foam or gels while cleaning the hands could be a cheap, fast and effective way to maintain hygiene of these instruments in hospital wards [3].
In our study, students in both years most commonly disinfected the stethoscope membrane, which indeed could harbor the highest number of pathogens [2,3], taking into account that the stethoscope membrane is a usual point of contact with patients. However, the stethoscope bell on the opposite side of the membrane may as well be used in auscultations of low-frequency sounds and murmurs and consequently get contaminated. The stethoscope bell is commonly cleaned among pediatricians, who disinfect the bell just as frequently as they clean the membrane [20]. We also observed that the flexible tubing was the least frequently cleaned. In order for a stethoscope to be functional, flexible tubing is required to have sufficient reach. Even though it does not have an apparent role in the auscultation process, it may also harbor microorganisms, given the variety of tubing lengths among different stethoscope manufacturers. However, it is unclear whether or not bacterial flora found on stethoscope tubing has a role in the spread of pathogens.
Overall, the students in our survey reported use of ethanol-based products in stethoscope disinfection. This practice is likely a result of availability and reach of containers with ethanol-based hand sanitizers in domestic hospital wards. Previous surveys among medical students reported somewhat different patterns of stethoscope cleaning [15,16]. For example, in Pakistan, students and physicians altogether descibed different cleaning methods depending on the circumstances [16]. Specifically, if a patient's skin was dry and intact, a dry cloth was used (53.2%), while ethanol was applied when the stethoscope had been in contact with blood or other fluids (64.3%) [16]. Also, medical students in France preferred using antiseptic wipes (44.0%), while 70% ethanol solution was ranked second (36.0%) [15], which are likely readily available in wards. Ethanol-based disinfectants have been shown to effectively reduce stethoscope contamination [8]. Beside this, effects of isopropyl alcohol were also examined in stethoscope disinfection [21]. Although isopropyl alcohol reduced contamination, it was not more effective than an ethanol-based cleaner [21]. Furthermore, a recent study reported that isopropyl alcohol did not decrease methicillin-resistant S. aureus stethoscope counts [22]. Bearing in mind that a variety of antiseptic agents are available and are inexpensive, regular stethoscope disinfection should become habitual practice among health care workers.
The students expressed the strongest positive attitude towards the notion to have a clean stethoscope, highlighting that students endorse stethoscope cleaning practices in spite of the notion that they were not likely shown how to properly clean their stethoscopes in classes. Appropriate use of stethoscopes is an integral part of practical lessons in wards; however, it seems that their maintenance has not been properly addressed in classes. We observed a positive association between a higher frequency of cleaning and greater awareness that stethoscopes should be cleaned. This finding suggests that promotion of stethoscope cleaning may have a positive effect on cleaning compliance in hospital wards. Also, a history of receiving information on stethoscope cleaning has been one of the strongest predictors of stethoscope hygiene [16], as well as having role models [14]. Therefore, implementation of lessons on stethoscope hygiene should be the cornerstone of securing disinfection practices later in professional practice, as educational interventions that offer inexpensive but effective training in stethoscope cleaning have shown improved disinfection compliance among health care workers [9].
Some limitations of this study include information bias. It is possible that some students did not wish to acknowledge that they did not clean their stethoscope regularly or even at all. Noninclusion of other medical faculties within the country as well as health care workers in the assessment of potential differences relative to the student population may be another limitation.
Conclusion
The proportions of both four- and sixth-year medical students who clean their stethoscopes were high. Further, the students expressed interest in learning the proper maintenance of stethoscope hygiene. Hence, it would be useful to implement these lessons in the regular practical curriculum in earlier study years, with the aim of applying stethoscope disinfection in daily work.
Disclosure Statement
The authors have no conflict of interest.
Acknowledgment
This study was supported by the Ministry of Education and Science of the Republic of Serbia (grant No. 175087).
References
- 1.Shiferaw T, Beyene G, Kassa T, et al. Bacterial contamination, bacterial profile and antimicrobial susceptibility pattern of isolates from stethoscopes at Jimma University Specialized Hospital. Ann Clin Microbiol Antimicrob. 2013;12:39. doi: 10.1186/1476-0711-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campos-Murguía A, León-Lara X, Muñoz JM, et al. Stethoscopes as potential intrahospital carriers of pathogenic microorganisms. Am J Infect Control. 2014;42:82–83. doi: 10.1016/j.ajic.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 3.Schroeder A, Schroeder MA, D'Amico F. What's growing on your stethoscope? (And what you can do about it) J Fam Pract. 2009;58:404–409. [PubMed] [Google Scholar]
- 4.Allegranzi B, Bagheri Nejad S, Graafmans W, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 5.Wood MW, Lund RC, Stevenson KB. Bacterial contamination of stethoscopes with antimicrobial diaphragm covers. Am J Infect Control. 2007;35:263–266. doi: 10.1016/j.ajic.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell A, Dealwis N, Collins J, et al. Stethoscope or ‘staphoscope’? Infection by auscultation. J Hosp Infect. 2010;76:278–279. doi: 10.1016/j.jhin.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 7.Alleyne SA, Hussain AM, Clockie M, et al. Stethoscopes: potential vectors of Clostridium difficile. J Hosp Infect. 2009;73:187–189. doi: 10.1016/j.jhin.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Whittington AM, Whitlow G, Hewson D, et al. Bacterial contamination of stethoscopes on the intensive care unit. Anaesthesia. 2009;64:620–624. doi: 10.1111/j.1365-2044.2009.05892.x. [DOI] [PubMed] [Google Scholar]
- 9.Uneke CJ, Ndukwe CD, Nwakpu KO, et al. Stethoscope disinfection campaign in a Nigerian teaching hospital: results of a before-and-after study. J Infect Dev Ctries. 2014;8:86–93. doi: 10.3855/jidc.2696. [DOI] [PubMed] [Google Scholar]
- 10.Zachary KC, Bayne PS, Morrison VJ, et al. Contamination of gowns, gloves, and stethoscopes with vancomycin-resistant enterococci. Infect Control Hosp Epidemiol. 2001;22:560–564. doi: 10.1086/501952. [DOI] [PubMed] [Google Scholar]
- 11.Cohen SR, McCormack DJ, Youkhana A, et al. Bacterial colonization of stethoscopes: the effect of cleaning. J Hosp Infect. 2003;55:236–237. doi: 10.1016/s0195-6701(03)00297-4. [DOI] [PubMed] [Google Scholar]
- 12.Parmar RC, Valvi CC, Sira P, et al. A prospective, randomised, double-blind study of comparative efficacy of immediate versus daily cleaning of stethoscope using 66% ethyl alcohol. Indian J Med Sci. 2004;58:423–430. [PubMed] [Google Scholar]
- 13.Jones JS, Hoerle D, Riekse R. Stethoscopes: a potential vector of infection? Ann Emerg Med. 1995;26:296–299. doi: 10.1016/s0196-0644(95)70075-7. [DOI] [PubMed] [Google Scholar]
- 14.Saunders C, Hryhorskyj L, Skinner J. Factors influencing stethoscope cleanliness among clinical medical students. J Hosp Infect. 2013;84:242–244. doi: 10.1016/j.jhin.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Duroy E, Le Coutour X. Hospital hygiene and medical students. Med Mal Infect. 2010;40:530–536. doi: 10.1016/j.medmal.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Hyder O. Cross-sectional study of frequency and factors associated with stethoscope cleaning among medical practitioners in Pakistan. East Mediterr Health J. 2012;18:707–711. doi: 10.26719/2012.18.7.707. [DOI] [PubMed] [Google Scholar]
- 17.Karim J, Al-Saraji M, Al-Mousawi F, et al. Knowledge and self-reported practice of universal precautions among Kuwait University medical students in their clinical years. Med Princ Pract. 2012;21:328–333. doi: 10.1159/000335278. [DOI] [PubMed] [Google Scholar]
- 18.World Federation of Medical Education Statement on the Bologna Process and medical education. 2005. http://www.aic.lv/bolona/Bologna/contrib/Statem_oth/WFME-AMEE.pdf
- 19.Hagel S, Reischke J, Kesselmeier M, et al. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol. 2015 doi: 10.1017/ice.2015.93. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Muniz J, Sethi RK, Zaghi J, et al. Predictors of stethoscope disinfection among pediatric health care providers. Am J Infect Control. 2012;40:922–925. doi: 10.1016/j.ajic.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 21.Lecat P, Cropp E, McCord G, et al. Ethanol-based cleanser versus isopropyl alcohol to decontaminate stethoscopes. Am J Infect Control. 2009;37:241–243. doi: 10.1016/j.ajic.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Russell A, Secrest J, Schreeder C. Stethoscopes as a source of hospital-acquired methicillin-resistant Staphylococcus aureus. J Perianesth Nurs. 2012;27:82–87. doi: 10.1016/j.jopan.2012.01.004. [DOI] [PubMed] [Google Scholar]