Abstract
Objective
The purpose of this study was to determine the efficacy of the Lidopat® 5% skin patch in relieving rib fracture pain.
Subjects and Methods
From June 2009 to May 2011, 44 trauma patients with isolated rib fractures were enrolled in this study and randomized in a double-blind method into 2 groups. The experimental group (group E: 27 patients) used a Lidopat® 5% skin patch at the trauma site and took an oral analgesic drug for pain relief. The placebo group (group P: 17 patients) used a placebo vehicle patch and an oral analgesic drug.
Results
The mean age, weight and hospital stay of patients were 56.8 ± 13.8 years, 67.4 ± 12.6 kg and 6.34 ± 1.3 days, respectively. In the first 4 days, there were no significant differences in pain scores between the groups (p > 0.05). After the 5th day, the average pain score was significantly less in group E (mean 1.5) than in group P (mean 3.10; p < 0.05). There was no significant difference in the number of fractured ribs between groups (p = 0.904). The use of meperidine and the length of hospital stay (6.0 vs. 6.9 days) were both significantly less in group E (p = 0.043 and 0.009, respectively).
Conclusion
In this study, the use of the Lidopat® 5% skin patch in patients with isolated rib fractures alleviated pain and shortened the hospital stay, and a lower dose of pain-relieving medication was used.
Key Words: Rib fracture, Analgesia, Nerve block
Introduction
Thoracic traumas comprise 10-15% of all trauma cases, and the incidence of rib fractures ranges from 7 to 38.7% [1,2,3]. The treatment of isolated rib fractures consists primarily of the control of pain, the prevention of translocation of the broken ribs, the physical rehabilitation of the chest and encouragement of physical activity as soon as possible [4]. Effective pain relief has a considerable impact on the prognosis of patients with rib fractures, especially those with multiple fractures. Traditionally, treatment of rib fractures includes painkillers (nonsteroidal anti-inflammatory drugs or opioids), transcutaneous electrical nerve stimulation and regional analgesics [5]. Of these, intercostal nerve block by the injection of lidocaine is an effective method of regional anesthesia and is associated with minimal systemic side effects (that could cause unforeseen risks such as pneumothorax and systemic anesthetic toxicity) [6].
Lidopat® 5% (Dersan Company, Chiayi, Taiwan) is an approved, local, pain control skin patch for postherpetic neuralgia [7], reported to be useful in the treatment of lower back pain [8], bony arthritis [9], carpal tunnel syndrome [10] and the pain related to diabetes polyneuropathies [7]. Empirically, it is also for patients with traumatic rib fractures for relieving pain; however, there has been no prospective randomized study with respect to its analgesic effect in these patients. Thus, the purpose of our study was to determine the effects of Lidopat® in the treatment of intercostal neuralgia due to rib fractures (intercostal neuropathic pain).
Subjects and Methods
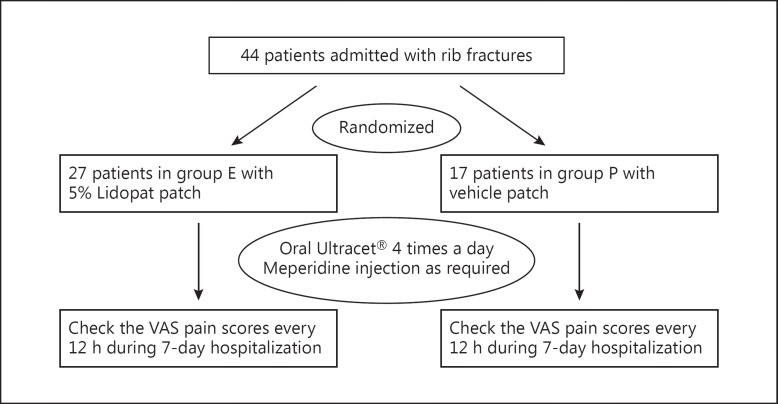
For this study, conducted from June 2009 to May 2011, 44 trauma patients (23 men and 21 women) with isolated rib fractures treated at the E-Da Hospital, a university-affiliated hospital in Kaohsiung, Southern Taiwan, were prospectively enrolled. Exclusion criteria were: bilateral or occult rib fractures or other associated injuries, and if the patient was admitted to the intensive care unit. All the patients were followed up till the last one in July 2013. Definitive diagnoses were established by chest X-ray or thoracic computed tomography. The patients were randomized into 2 groups: an experimental group (group E) treated with a Lidopat® 5% skin patch and a placebo group (group P) treated with a vehicle patch. All physicians and patients were blinded as to which skin patch was used. This study was approved by the Institutional Review Board of our hospital, and all patients provided written informed consent. The study design is shown in figure 1.
Fig. 1.
Study design.
The skin patch was applied within 12 h of admission, and was changed every 12 h. It was affixed to the rib fracture on the side near the spine. An oral analgesic (Ultracet®) was administered at a dosage of 1 pill 4× daily for every patient, and patients were allowed to request an increase of dosage up to a maximum of 2 pills 4× daily. Intramuscular injection of meperidine 50 mg was administered as required. Visual analog scale (VAS) pain scores using a 10-point scale were recorded by a study nurse every 12 h (before oral analgesic administration) until discharge. After discharge, the pain score was annotated as 0. Forced expiratory volume in the first second (FEV1) was checked on the day of discharge and 3 months after entering the study.
Comparisons were made using Student's t test and data were presented as means ± standard deviation. A probability of ≤0.05 was considered statistically significant.
Results
The mean age of the patients was 56.8 ± 13.8 years. The mean weight of the patients was 67.4 ± 12.6 kg. The mean hospital stay was 6.34 ± 1.3 days. Of the 44 patients, 31 (70.5%) had left-sided rib fractures and 13 (29.5%) had right-sided fractures. The number of rib fractures ranged from 1 to 5; the average number in group E (3.04) was no different from that in group P (3.00; p = 0.904). No patients had chronic lung disease or underwent anticoagulant therapy preinjury. There were no significant differences between the groups with respect to gender (p = 0.593), age (p = 0.539), smoking status (p = 0.945) and average weight (p = 0.809; table 1). A total of 14 sets of pain scores were recorded in each group and there were no significant differences in the first 9 pain scores between the groups (p > 0.05; table 2). From the 10th pain score, the average score (group E: 2.52 reduced to 1.37 vs. group P: 3.29 reduced to 2.47) was significantly lower in group E (p < 0.05; table 2). The average hospital stay was significantly shorter in group E than in group P (6.0 vs. 6.9 days; p = 0.009). There was no significant difference in the use of oral analgesics between the groups (p = 0.173), but the use of meperidine was significantly less in group E than in group P (p = 0.043). The improvement change in FEV1 at 3 months after discharge was not different between the groups (p = 0.201). The mean follow-up period was 2.5 ± 0.1 years.
Table 1.
The demography of the patients in each group
| Character | Group E | Group P | p value |
|---|---|---|---|
| Gender, n | 0.593 | ||
| Female | 12 | 9 | |
| Male | 15 | 8 | |
| Age, years | 55.7 ± 13.7 | 58.4 ± 14.7 | 0.539 |
| Smoking status, n | 0.945 | ||
| Smoker | 14 | 9 | |
| Nonsmoker | 13 | 8 | |
| Body weight, kg | 67.0 ± 12.7 | 68.0 ± 13.0 | 0.809 |
| Fractures, n | 3.04 ± 1.2 | 3.0 ± 0.8 | 0.904 |
Table 2.
The table shows the average VAS pain scores between group E (Lidopat®) and group P (placebo)
| Record | Lidopat® | Placebo | Difference | p value |
|---|---|---|---|---|
| 1st | 5.63 | 5.94 | –0.31 | 0.659 |
| 2nd | 4.67 | 3.88 | 0.79 | 0.094 |
| 3rd | 4.11 | 4.82 | –0.71 | 0.142 |
| 4th | 3.85 | 3.88 | –0.03 | 0.937 |
| 5th | 3.63 | 4.00 | –0.37 | 0.414 |
| 6th | 3.59 | 3.65 | –0.06 | 0.910 |
| 7th | 3.37 | 4.00 | –0.63 | 0.225 |
| 8th | 3.37 | 3.59 | –0.22 | 0.595 |
| 9th | 2.81 | 3.41 | –0.60 | 0.103 |
| 10th | 2.52 | 3.29 | –0.77 | 0.021 |
| 11th | 2.26 | 3.41 | –1.15 | 0.003 |
| 12th | 1.78 | 3.47 | –1.69 | 0.000 |
| 13th | 1.52 | 2.53 | –1.01 | 0.041 |
| 14th | 1.37 | 2.47 | –1.10 | 0.049 |
Scores were recorded at 12-hour intervals over 7 days. After the 10th recording, group E had VAS scores that were significantly lower statistically.
Discussion
The results of this study showed that, when using the Lidopat® skin patch, meperidine was required less and the hospital stay was shorter. We used the patch to replace intercostal injections for relieving neuropathic pain in patients with traumatic rib fractures, and our results indicate that it may have some effects in the treatment of this pain.
Effective pain relief for rib fractures, especially multiple fractures, has a considerable impact on recovery, and is essential when these patients need thoracic rehabilitation. Intercostal nerve block anesthesia by injecting a small amount of an anesthetic drug, usually 2% lidocaine, can achieve the sensory block of the affected intercostal nerves [5]. Lidocaine blocks the transmission of the voltage-gated sodium channels to achieve pain relief because the overconduction of this in the injured nerve is the cause of the pain (neuropathic pain). However, intercostal nerve block carries some unforeseen risks which deter its widespread use in clinical situations.
After chest trauma involving rib fractures, substantial recovery can be demonstrated by improved pulmonary function tests. These encourage maximal intensive care for these patients, especially pain relief. However, the method of pain relief has no impact on the long-term recovery of the lung function. As shown by our results, the improvement in FEV1 3 months after discharge was not different between the 2 groups. This is evidence that Lidopat® has no benefit in improving lung function, since what is recorded 3 months after the injury is regarded as the basic lung function for the patient.
Systemic injections of nonsteroidal anti-inflammatory drugs) or administration of opioids are simple and effective methods to lessen the pain. However, such medications can cause side effects. Oral analgesic drugs are used regularly, but for patients with rib fractures, particularly in the acute phase of injury, the relieving effects are often adjuvant. Regional analgesia for rib fractures is currently the most effective method of pain relief [11,12]. It can also decrease the impairment of the immune response that results from pain. However, this method needs administration by a specialist and carries a high risk. Using the Lidopat® 5% skin patch carries no risk, as shown in this study. The skin patch can be applied by a general physician or even by the patients themselves after discharge.
Isolated rib fractures with no associated injuries have a relatively low incidence, with only 13.1% diagnosed in 1 large series [2]. This is the reason why only 44 patients were enrolled in our study over a period of 2 years, and all were admitted via our emergency department.
The major limitation of this study was that patients with obvious rib fracture that demanded admission for pain relief were enrolled in the study while those with occult rib fractures were excluded. The other limitation was the small number of patients in each group.
Conclusion
In this study, the Lidopat® 5% skin patch reduced pain, the dose of analgesics required and the length of hospital stay in the patients with rib fractures.
Acknowledgement
I would like to thank Miss Shienpien Ku, a study nurse, for her assistance in recording the VAS pain scores.
References
- 1.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–979. doi: 10.1097/00005373-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Sirmali M, Türüt H, Topçu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24:133–138. doi: 10.1016/s1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 3.Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma. 2000;48:1040–1046. doi: 10.1097/00005373-200006000-00007. discussion 1046-1047. [DOI] [PubMed] [Google Scholar]
- 4.Easter A. Management of patients with multiple rib fractures. Am J Crit Care. 2001;10:320–327. quiz 328-329. [PubMed] [Google Scholar]
- 5.Karmakar MK, Ho AM. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–625. doi: 10.1097/01.TA.0000053197.40145.62. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JR, Maestrello CL, Campbell RL. Allergic response to metabisulfite in lidocaine anesthetic solution. Anesth Prog. 2001;48:21–26. [PMC free article] [PubMed] [Google Scholar]
- 7.Barbano RL, Herrmann DN, Hart-Gouleau S, et al. Effectiveness, tolerability, and impact on quality of life of the 5% lidocaine patch in diabetic polyneuropathy. Arch Neurol. 2004;61:914–918. doi: 10.1001/archneur.61.6.914. [DOI] [PubMed] [Google Scholar]
- 8.Galer BS, Gammaitoni AR, Oleka N, et al. Use of the lidocaine patch 5% in reducing intensity of various pain qualities reported by patients with low-back pain. Curr Med Res Opin. 2004;20((suppl 2)):S5–S12. doi: 10.1185/030079904X12933. [DOI] [PubMed] [Google Scholar]
- 9.Gammaitoni AR, Galer BS, Onawola R, et al. Lidocaine patch 5% and its positive impact on pain qualities in osteoarthritis: results of a pilot, 2-week, open-label study using the Neuropathic Pain Scale. Curr Med Res Opin. 2004;20((suppl 2)):S13–S19. doi: 10.1185/030079904X12951. [DOI] [PubMed] [Google Scholar]
- 10.Nalamachu S, Crockett RS, Mathur D. Lidocaine patch 5 for carpal tunnel syndrome: how it compares with injections: a pilot study. J Fam Pract. 2006;55:209–214. [PubMed] [Google Scholar]
- 11.Govindarajan R, Bakalova T, Michael R, et al. Epidural buprenorphine in management of pain in multiple rib fractures. Acta Anaesthesiol Scand. 2002;46:660–665. doi: 10.1034/j.1399-6576.2002.460605.x. [DOI] [PubMed] [Google Scholar]
- 12.AK K, Gursoy S, Duger C, et al. Thoracic paravertebral block for postoperative pain management in percutaneous nepholithotomy patients: a randomized controlled clinical trial. Med Princ Pract. 2013;22:229–233. doi: 10.1159/000345381. [DOI] [PMC free article] [PubMed] [Google Scholar]