Abstract
Objective
The aim of this work was to verify the usefulness and efficacy of treating superficial vascular lesions of the face using rhodamine intense pulsed light (r-IPL).
Subjects and Methods
Fifty patients suffering from telangiectasias of the face were enrolled and subsequently treated 4 times (every 20 days) with a new intensified r-IPL system optimized at the same wavelength as the dye laser (595 nm). The outcome was assessed using photographs, and clinical evaluations were made based on the percentage of fading of the erythema and telangiectasias in the lesions after treatment.
Results
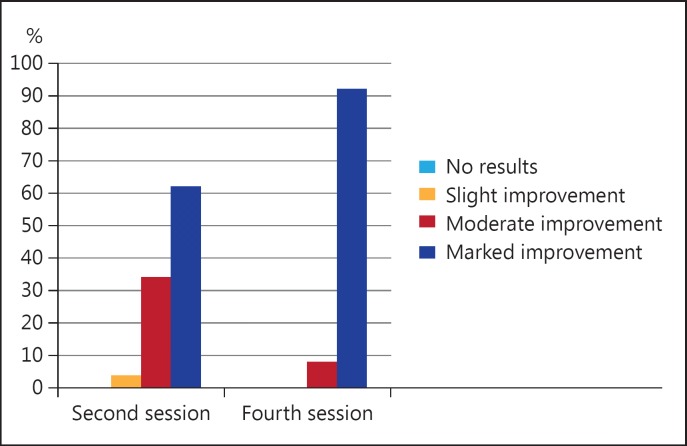
Marked clinical improvements (70-100s%) were observed in 31 (62s%) patients after the second session of r-IPL, while 46 (92s%) showed a marked improvement after the fourth session. No patients had to resort to topical or systemic drugs.
Conclusion
r-IPL was effective in treating superficial vascular lesions, no side effects were observed and the patients readily accepted the treatment. Hence, r-IPL could be promising for the treatment of superficial vascular lesions of the face. Future study would be necessary to confirm the long-term efficacy of this technique.
Key Words: Telangiectasias, Laser, Pulsed light
Introduction
Vascular lesions of the face represent an aesthetic problem and are a symptom of different skin diseases [1]. Currently, laser technology can be considered an effective treatment modality for superficial vascular lesions of the face using light sources with visible (500-800 nm) and near-infrared (800-1,300 nm) wavelengths [2]. Initially, the most widely used systems to treat these lesions were potassium titanyl phosphate (KTP, 532 nm), the copper vapor laser (511/578 nm), the alexandrite laser (755 nm) and the diode laser (800/810/930 nm). The current systems such as the dye laser (595 nm), Nd:Yag laser (1,064 nm) and pulsed-light system (500-1,200 nm) were then introduced [3].
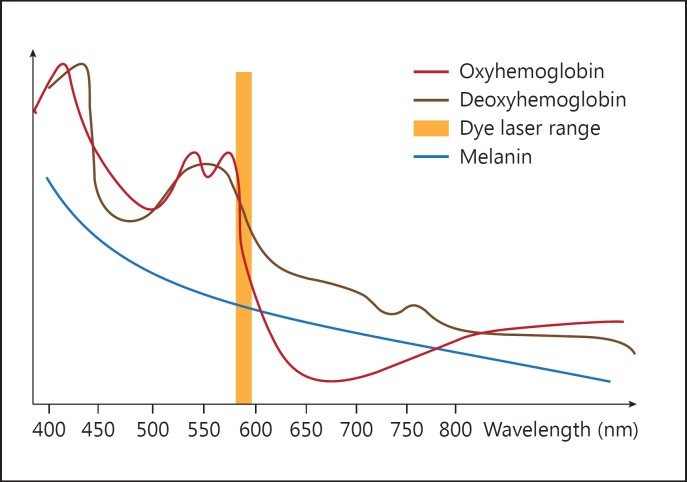
The choice of an effective laser for treating vascular lesions should take into account the wavelength at which the vascular chromophore has the greatest absorption; these devices focus on oxyhemoglobin which has 3 wavelength absorption peaks, i.e. at 418, 542 and 577 nm (fig. 1) [4].
Fig. 1.
Absorption spectrum of the main skin chromophores and hemoglobin selectivity of the dye laser.
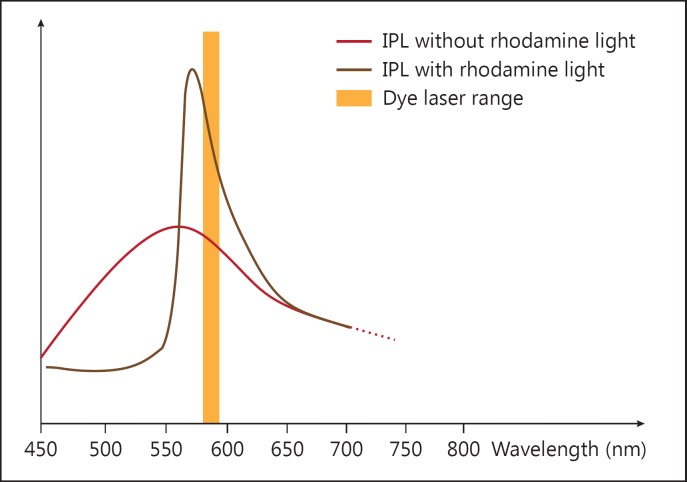
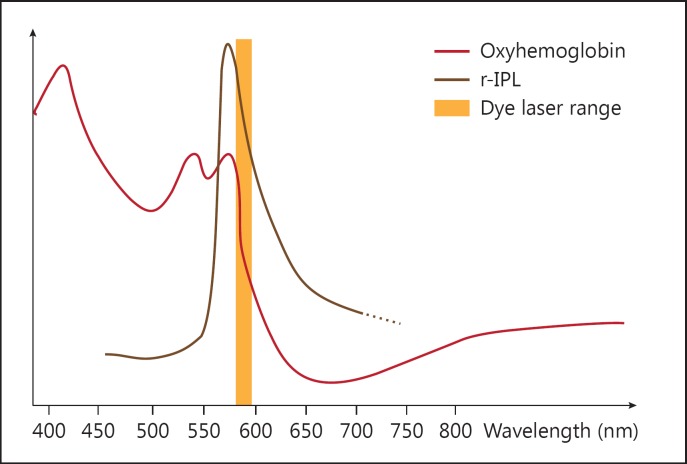
Rhodamine intense pulsed light (r-IPL) is a new pulsed-light system optimized for wavelengths ranging between 550 and 650 nm, which can achieve performances comparable to those of the dye laser (595 nm). The r-IPL handpiece uses rhodamine as a fluorescent substance that can absorb wavelengths in the UV spectrum up to 550 nm and re-emit these in fluorescence in a range of between 550 and 650 nm, with a rhodamine peak at approximately 570 nm, without losing energy during the transformation (fig. 2). This system of shifting the emission band via fluorescence can also exploit the component closest to the UV spectrum (between 450 and 500 nm) not selected for vascular lesions. This range of wavelengths would not produce therapeutic effects and cause interactions in the pigmentary component only, so it is usually eliminated in traditional pulsed-light systems through the use of filters. The r-IPL technology does not eliminate a significant amount of energy, but rather transfers it to a vascular frequency range, as for dye laser specifications, in order to increase both energy efficiency and performance on the hemoglobin chromophore (fig. 3).
Fig. 2.
Emission frequencies of IPL, rhodamine light and dye laser.
Fig. 3.
Increase in vascular performance of r-IPL on the hemoglobin cromophore.
The use of waveguides, which transfer the energy that is generated, and subsequently optimized, into the tissue, allows the handpiece to be moved away from the skin to increase treatment area visibility. The handpiece can be adapted to effectively reach every area of the face including those hardest to access, such as the base of the nose. As in other laser systems, optimized cooling of the waveguide protects the epidermis against pulsed-light radiation, thereby maintaining the integrity of the surrounding tissue. Cooling is also used to generate a local anesthetic effect over the radiated area, making the treatment more comfortable. The aim of this study was to verify the usefulness and effectiveness of r-IPL and to demonstrate if it can indeed merge the advantages of IPL and laser devices in treating superficial vascular lesions of the face.
Subjects and Methods
A total of 50 patients (29 females and 21 males, aged between 30 and 60 years), of skin phototypes I-IV and suffering from telangiectasias of the face, were examined and subsequently treated in our university-based Dermatology Outpatient Clinic from October 2013 to November 2014. Patients were suffering from common telangiectasias (n = 23), facial erythrosis (n = 11), acne rosacea (n = 7) or telangiectasias of the nose (n = 5) and chin (n = 4). The study was carried out according to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board. Written informed consent was obtained from each patient for the treatment and release of photographic images for scientific purposes.
The study treatment protocol involved the use of a new system, a rhodamine light handpiece (DEKA M.E.L.A srl, Florence, Italy), which exploits rhodamine as a selective fluorescent substance for the vascular target. Two handpieces were available with an emission area of 2 and 6.2 cm2, respectively, and supplied with an integrated cooling system. All the patients were subjected to an effectiveness check during the first visit (October 2013 to August 2014) and subsequently treated every 20 days for a total of 4 treatments. The protocol provided fluencies ranging between 18 and 23 J/cm2, with an emission area of 2 or 6.2 cm2, selected according to the severity and size of the lesions. We usually started with a low fluency of 18 J/cm2, which was gradually increased in subsequent sessions to up to 23 J/cm2. Two pulses of 6-8 ms each were performed with a delay of 10 ms between pulses. Conductive cold gel for pulsed light was placed between the crystal and the light to provide optimal contact and heat dispersion. Not much pressure was exerted during treatment so as to avoid causing any vessel ischemia. Patients were photographed before the first treatment and at the end of the therapy with a digital camera system, Anthology (DEKA M.E.L.A. srl), and with Antera 3D (Miravex Ltd., Dublin, Ireland), a noninvasive photographic device that uses a multisource spectrum and 3-dimensional mapping of the skin surface and is able to analyze both the hemoglobin and melanin skin components. It was thus possible to estimate the length and width of the capillaries, the area of the lesion and the concentration of hemoglobin with the Antera system. The most extensively vascularized areas showed in the pictures in colors ranging from red to purple. All images were evaluated on 2 databases (Anthology and Antera 3D) in order to verify the efficacy of r-IPL on the vascular pattern.
The outcomes were evaluated from photographs taken by independent clinical observers (G.C. and R.C.), i.e. not the operator dermatologist. Based on the percentage of fading of the erythema and telangiectasias in the lesions after treatment, they were divided into 4 categories: no outcomes (0s%), a slight improvement (1-40s%), a moderate improvement (40-70s%) and a marked improvement (70-100s%).
Both during and after therapy, the patients were asked to quantify the perceived pain as mild, moderate or severe. A clinical evaluation of transient erythema and posttreatment edema was carried out by a dermatologist (R.C.) and identified as absent, mild or intense.
Results
The mean age of the 50 patients was 44.6 s+ 15.3 years. A marked clinical improvement was observed in 31 (62s%) of the 50 lesions after the second session of r-IPL, and 46 (92s%) showed a marked improvement after the fourth session (fig. 4; table 1). The outcomes are highlighted in figures 5, 6, 7, 8, where clinical pictures taken before and after the treatment are compared with the images obtained with the Antera system.
Fig. 4.
Overall improvement assessment.
Table 1.
Marked improvement at the fourth session
| Disorder | Patients showing a marked improvement at the fourth session, n (s%) |
|---|---|
| Common telangiectasia | 23 (100) |
| Facial erythrosis | 10 (90.9) |
| Acne rosacea | 6 (85.7) |
| Telangiectasia of the nose | 4 (80) |
| Telangiectasia of the chin | 3 (75) |
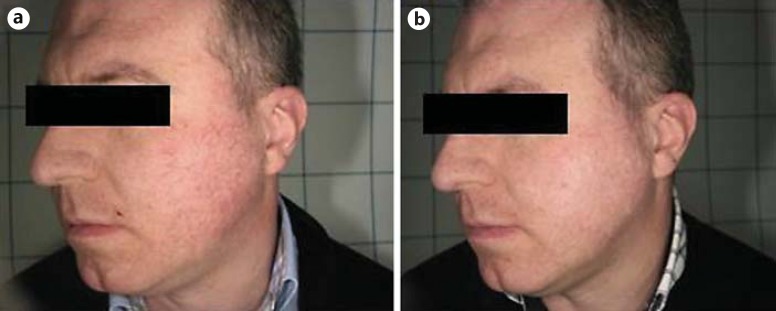
Fig. 5.
Clinical images of a patient with facial telangiectasia. a Before treatment. b After 4 treatments with r-IPL, there was a marked improvement.
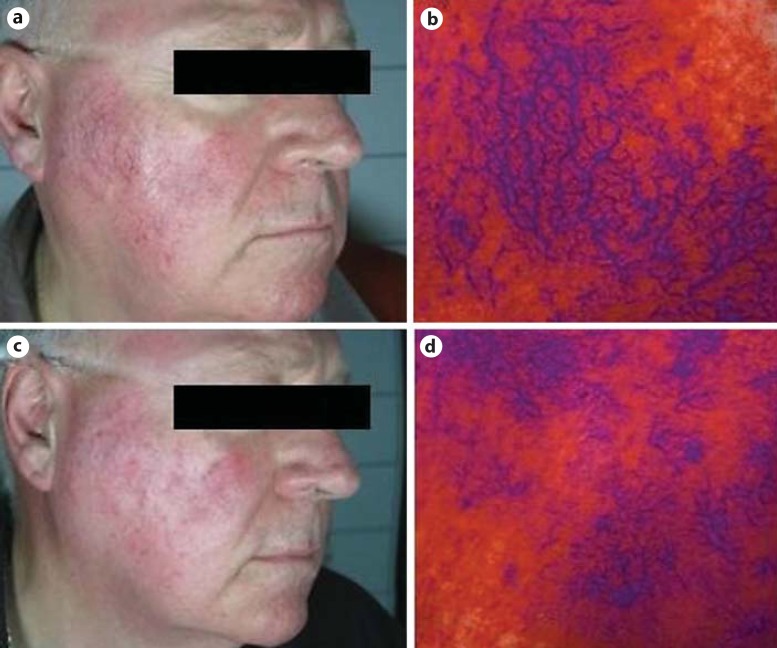
Fig. 6.
Marked improvement in a patient with severe telangiectasia and erythrosis of the face. Before treatment: clinical image (a) and image obtained with Antera (b). After 4 treatments with r-IPL, the clinical image (c) and images obtained with Antera (d) show a marked improvement.
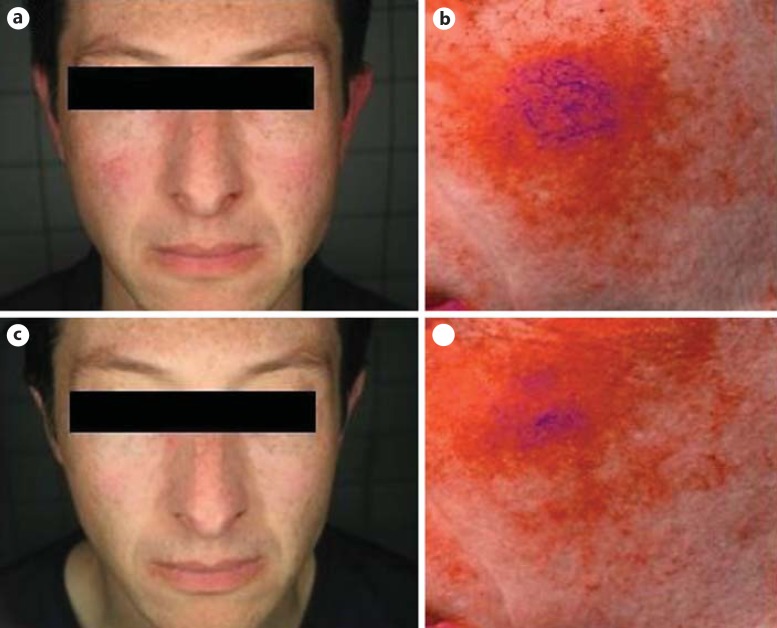
Fig. 7.
Patient with erythrosis and fine telangiectasia of the cheeks. Before treatment: clinical image (a) and image obtained with Antera (b). After 4 treatments with r-IPL, the clinical image (c) and images obtained with Antera (d) show a marked improvement.
Fig. 8.
Another patient with telangiectasia of the cheeks. Before treatment: clinical image (a) and image obtained with Antera (b). After 4 treatments with r-IPL, the clinical image (c) and image obtained with Antera (d) show a marked improvement.
All the patients tolerated the treatment well, 78s% reported mild pain and 22s% reported moderate pain that lasted a few minutes during and after the treatment. No patients underwent systemic antibiotic or corticosteroid therapy and there were no side effects.
In the immediate posttreatment period, slight transient erythema and edema were reported, which were treated with simple soothing creams.
Discussion
The treatment of facial telangiectasias is ever more frequently performed by laser or IPL devices. In this study, we demonstrate the efficacy and the safety of r-IPL for treating superficial vascular lesions of the face, combining the advantages of dye laser and IPL.
Dye laser is the mainstay of treatment of vascular lesions such as facial telangiectasias because of its high degree of safety and efficacy [5,6,7,8]. Despite its excellent results, the appearance of clear, purple bruises and subsequent scabbing in the posttreatment period that continue for several days could significantly limit its acceptance by patients who are treated for an aesthetic disease like telangiectatic rosacea. Conversely, according to our experience, treatment with r-IPL is not followed by the appearance of long-lasting purpura but only by transient erythema and edema which did not limit the patients' daily activities.
Several studies have demonstrated that IPL is another effective alternative or complementary therapeutic presidium to vascular laser [9,10,11,12]. IPL emits a polychromatic noncoherent broad-band light (500-1,200 nm). Its emission can, however, be made more selective by using proper filters and directing it towards specific chromophores such as melanin and hemoglobin [13]. The advantages of this technology are that it can hit the vascular target localized at different depths and with different wavelengths. Conversely, the most significant limitation of IPL is that more energy is released within the infrared spectrum, leaving little energy in the visible spectrum where the maximum peaks for hemoglobin absorptions are located, as is achieved with the dye laser [14]. According to our experience, r-IPL has proven to enhance performance in the working range of dye laser systems, thereby allowing greater outputs of energy at vascular wavelengths with no side effects.
In our study, marked improvements were observed in the majority of patients after the second session and in almost all of the patients after the fourth session. After the treatments, patients did not have to resort to topical or systemic drugs, so all of them showed excellent compliance during all 4 treatments established according to the protocol.
Thus, conversely to the other laser or light therapies, rhodamine light did not result in any side effects and patients readily accepted the treatment.
A limitation of this study was the absence of a long-term monitoring of the patients that would have demonstrated the efficacy of this technique over a long period.
Conclusion
Our study showed that r-IPL did not have any reported side effects and also had an excellent outcome in all patients. These benefits could make this form of IPL promising for the treatment of superficial vascular lesions of the face. The absence of intense erythema and scabs allows us to suggest that higher fluencies may be used in order to obtain the same results in a smaller number of treatments. This aspect will need to be verified in future studies.
Disclosure Statement
There were no conflicts of interest.
References
- 1.Doutre MS, Beylot-Barry M. About some red faces. Ann Dermatol Venereol. 2011;138:201–206. doi: 10.1016/S0151-9638(11)70090-4. [DOI] [PubMed] [Google Scholar]
- 2.Adamic M, Troilius A, Adatto M, et al. Vascular lasers and IPLS: guidelines for care from the European Society for Laser Dermatology (ESLD) J Cosmet Laser Ther. 2007;9:113–124. doi: 10.1080/14764170701280693. [DOI] [PubMed] [Google Scholar]
- 3.Benov L. Photodynamic therapy: current status and future directions. Med Princ Pract. 2015;24:14–28. doi: 10.1159/000362416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hare McCoppin HH, Goldberg DJ. Laser treatment of facial telangiectases: an update. Dermatol Surg. 2010;36:1221–1230. doi: 10.1111/j.1524-4725.2010.01613.x. [DOI] [PubMed] [Google Scholar]
- 5.Bencini PL, Tourlaki A, De Giorgi V, et al. Laser use for cutaneous vascular alterations of cosmetic interest. Dermatol Ther. 2012;25:340–351. doi: 10.1111/j.1529-8019.2012.01463.x. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein EF. The pulsed-dye laser for treatment of cutaneous conditions. G Ital Dermatol Venereol. 2009;144:557–572. [PubMed] [Google Scholar]
- 7.Conti R, Colucci R, Arunachalam M, et al. Hair and scalp disorders in a Tuscan pediatric dermatological outpatient clinic: a clinical and epidemiological evaluation. Med Princ Pract. 2016;25:67–71. doi: 10.1159/000439466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Zohairy SN, Oriowo MA, Ezeamuzie CI. Cyclic adenosine monophosphate-mediated enhancement of vascular endothelial growth factor released by differentiated human monocytic cells: the role of protein kinase A. Med Princ Pract. 2015;24:548–554. doi: 10.1159/000433540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campolmi P, Bonan P, Cannarozzo G, et al. Intense pulsed light in the treatment of non-aesthetic facial and neck vascular lesions: report of 85 cases. J Eur Acad Dermatol Venereol. 2011;25:68–73. doi: 10.1111/j.1468-3083.2010.03700.x. [DOI] [PubMed] [Google Scholar]
- 10.Myers P, Bowler P, Hills S. A retrospective study of the efficacy of intense pulsed light for the treatment of dermatologic disorders presenting to a cosmetic skin clinic. J Cosmet Dermatol. 2005;4:262–266. doi: 10.1111/j.1473-2165.2005.00202.x. [DOI] [PubMed] [Google Scholar]
- 11.Papageorgiou P, Clayton W, Norwood S, et al. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008;159:628–632. doi: 10.1111/j.1365-2133.2008.08702.x. [DOI] [PubMed] [Google Scholar]
- 12.Udo EE. Community-acquired methicillin-resistant Staphylococcus aureus: the new face of an old foe? Med Princ Pract. 2013;22:20–29. doi: 10.1159/000354201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ciocon DH, Boker A, Goldberg DJ. Intense pulsed light: what works, what's new, what's next. Facial Plast Surg. 2009;25:290–300. doi: 10.1055/s-0029-1243077. [DOI] [PubMed] [Google Scholar]
- 14.Neuhaus IM, Zane LT, Tope WD. Comparative efficacy of nonpurpuragenic pulsed dye laser and intense pulsed light for erythematotelangiectatic rosacea. Dermatol Surg. 2009;35:920–928. doi: 10.1111/j.1524-4725.2009.01156.x. [DOI] [PubMed] [Google Scholar]