Abstract
Background and Aims:
The use of weaning predictive indicators can avoid early extubation and wrongful prolonged mechanical ventilation. This study aimed to determine the power of the integrative weaning index (IWI) in predicting the success rate of the spontaneous breathing trial (SBT) in patients under mechanical ventilation.
Materials and Methods:
In this prospective study, 105 patients undergoing mechanical ventilation for over 48 h were enrolled. Before weaning initiation, the IWI was calculated and based on the defined cutoff point (≥25), the success rate of the SBT was predicted. In case of weaning from the device, 2-h SBT was performed and the physiologic and respiratory indices were continuously studied while being intubated. If they were in the normal range besides the patient's tolerance, the test was considered as a success. The result was then compared with the IWI and further analyzed.
Results:
The SBT was successful in 90 (85.7%) and unsuccessful in 15 (14.3%) cases. The difference between the true patient outcome after SBT, and the IWI prediction was 0.143 according to the Kappa agreement coefficient (P < 0.001). Moreover, regarding the predictive power, IWI had high sensitivity (95.6%), specificity (40%), positive and negative predictive values (90.5% and 60), positive and negative likelihood ratios (1.59 and 0.11), and accuracy (86.7%).
Conclusion:
The IWI as a more objective indicator has acceptable accuracy and power for predicting the 2-h SBT result. Therefore, in addition to the reliable prediction of the final weaning outcome, it has favorable power to predict if the patient is ready to breathe spontaneously as the first step to weaning.
Keywords: Integrative weaning index, mechanical ventilation, predictive power, spontaneous breathing trial
INTRODUCTION
Delayed and early weaning from the mechanical ventilation device both impose serious consequences to the patient and the health system. Therefore, it is recommended that weaning is done after accurate and objective assessment and when the patient is truly ready for separation from the ventilator.[1]
As a routine approach, the patient is assessed both objectively and subjectively for weaning readiness. Subjective assessment is done based on the physician's judgment and after evaluating the level of consciousness, awareness of time and place, the level of sedatives used, presence or absence of restlessness, effectiveness of cough, perspiration, and no paradoxical respiration. Objective evaluation is done based on the gas exchange status (arterial blood oxygen saturation) and hemodynamic status stability (heart rate [HR] and respiratory rate RR] per minute and blood pressure [BP]).[2,3] What is certain is that the expert's clinical judgment alone cannot be an accurate basis for making decisions about weaning from the ventilator; as wrongful decision-making and early weaning from mechanical ventilation can cause major stress to the patient.[4] However, based on the available evidence, none of the common criteria used have an accuracy above the median in predicting the weaning outcome.[5]
The spontaneous breathing trial (SBT) is a method suggested for use immediately after weaning from the ventilator to assess the patient's ability to tolerate independent ventilation. The result of this test can be considered as the basis for weaning from the mechanical ventilator and as a standard reference for further evaluation.[6,7]
This means that if the patient tolerated spontaneous ventilation, the physician can go forward with the next step, extubation of the tracheal tube. This decision is of significant clinical value, as a failure in extubation which may occur in 10%–20% of cases, is associated with serious consequences for the patient.[8,9] Therefore, the outcome of this test could be predicted with accurate and objective assessment minimizing the probability of failure and serious complications of reintubation while delayed weaning can be avoided.
One the most novel introduced indices for predicting the patients' outcome following weaning is the integrative weaning index (IWI). Based on the conducted studies so far, it has a sensitivity of 99% and specificity of 86% in predicting the outcome of weaning from the mechanical ventilation device.[10]
This index is a function of three basic parameters, the lungs capacity, arterial oxygen saturation (PaO2), respiratory rate, and tidal volume which can be calculated easily and with no need for patient's cooperation based on the following equation: (Cst, rs (Static compliance of the respiratory system) × SaO2 (Arterial oxygen saturation)/F(Respiratory rate)/VT(Tidal volume) ratio). For many reasons, this indicator can be a more objective index compared to the conventional methods, as it considers the function of the cardiovascular system, respiratory system, and the respiratory static compliance simultaneously. Therefore, this study was designed to investigate the IWI power in predicting a successful and an unsuccessful weaning outcome for SBT in mechanically ventilated patients.
MATERIALS AND METHODS
This diagnostic validation study was designed as a prospective study in 2015 in which 105 mechanically ventilated patients hospitalized in the Intensive Care Units (ICUs) of Imam Reza Hospital, Mashhad, Iran were enrolled.
The sample size was calculated based on the mentioned equation according to Nemer et al. study.[10]
Patients over 18 years of age receiving mechanical ventilation for at least 48 h to 3 weeks and with no neuromuscular disease were selected target-based. Patients with a tracheostomy tube and those whom were intubated more than once due to weaning failure were excluded from the study. The study protocol was approved by the Ethics Committee of Golestan University of Medical Sciences.
In the studied wards, the decision for weaning readiness and discontinuation of mechanical ventilation was made by the anesthesiologists in charge and based on the following criteria:
Improvement of the underlying disease, no fever, PaO2 >90% with an inspired O2 concentration of <0.4 and a positive end-expiratory pressure (PEEP) <8, hemodynamic stability (no use of high-dose vasopressive drugs), readiness for return to spontaneous ventilation, favorable level of consciousness (awake or easily awakeable), and pH >7.2.
Given that the specialists were blind to the study goal, they followed the recommended protocol designed by the 6th Conference of the Intensive Care International Association for weaning initiation and all decisions regarding weaning or return to mechanical ventilation were made by the same physician to avoid any bias related to difference in the weaning approach.
The required data were gathered by a checklist which included the following data: demographic data (age, sex, hospitalization history, disease diagnosis, other underlying diseases, level of consciousness, length of intubation, and length of ICU stay) and the physiologic status of the patient (HR/min, RR/min, BP, PaO2, PaCO2, fraction of inspired oxygen (FiO2), PEEP, tidal volume, static compliance, temperature, level of consciousness, and pH).
Based on the physician in charge's protocol, before weaning from mechanical ventilation, all patients were placed on the spontaneous mode with a pressure support (PS) of 8–10 cmH2O, a PEEP of 5 cmH2O and FiO2 <40%. Afterward, the device's PS was changed to 0, and the RR/tidal volume, PaO2, Cst, rs, and the patient's hemodynamic status were recorded. The static compliance was measured and recorded from the ventilation device by placing the patient in the volume mode and a 30 s pause at the end of inspiration.
The patient was then weaned from the mechanical ventilation device and underwent SBT by the T-Tube. In case of tolerance by the patient, the SBT result was considered as successful, and in case of any of the following results, an unsuccessful test result was recorded:
Reduced SaO2 <95%, PaO2 <60 mmHg, PaCO2 >50 mmHg, pH <7.33 or >0.07 reduction in pH, RR >38/min or an increase >50% during 5 min, HR >140/min, systolic BP >180 and <90 mmHg, agitation, perspiration, and reduced level of consciousness.
Along with the doctor's call for starting the weaning process, the researcher recorded the required parameters for calculating the IWI including SaO2, Cst, F/VT, and according to the related formula, this index was measured. The basis for predicting success was an index level ≥25 whereas the basis for failure was an index level <25.
The collected data were analyzed by the SPSS version 16 SPSS16 software (SPSS, Inc., Chicago, IL, USA) and MedCalc version 13 (Medcalc, Mariakerke, Belgium). To determine the predictive power of this tool, diagnostic value indices such as sensitivity, specificity, predictive value, and likelihood ratio were used. To determine the agreement of the IWI predictive power and SBT outcome, the Kappa coefficient was used. Moreover, to investigate the relationship between the test result and the patients' demographic and clinical characteristics with a quantitative entity such as age, hospitalization period the normal distribution of variables in the two groups was initially studied by the Shapiro–Wilk test. Independent t-test was used for normally distributed data while Mann–Whitney nonparametric test was used for variables with an abnormal distribution with the weaning outcome.
RESULTS
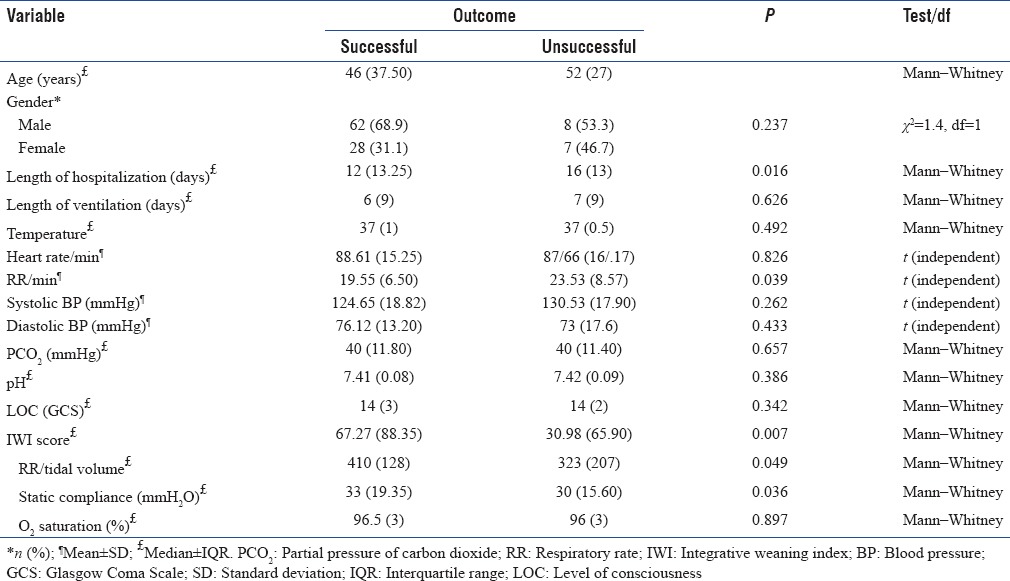
Given the SBT, among the 105 studied cases, 90 (85.7%) had a successful outcome whereas a failure was recorded in the other 15 (14.3%) patients. Among the successful cases, 62 (68.9%) were male and 28 (31.1%) female. The same figures were 8 (53.3%) and 7 (46.7%) in the failure group; indicating no meaningful difference between the two groups regarding sex (P = 0.186) Moreover, the findings showed a statistically meaningful difference between the two groups in terms of length of hospitalization, RR, static compliance, the RR-tidal volume ratio, and the IWI score [P < 0.05, Table 1]. The result of logistic regression model adjusted for the length of hospitalization was associated with a significantly decreased in the outcome of weaning (odds ratio = 0.9, confidence interval 95% = 0.848–0.978).
Table 1.
Distribution of spontaneous breathing trial result according to personal and clinical characteristics
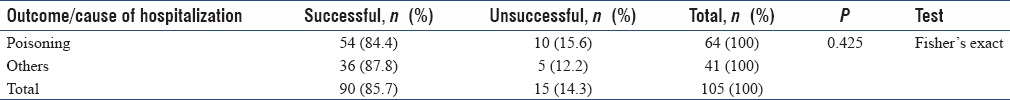
Based on the results, the most frequent cause of hospitalization was poisoning [Figure 1]. Hence, we categorized the causes into two main categories of poisoning and others. The finding shows no statistically meaningful association between the cause of hospitalization and the SBT result [Table 2].
Figure 1.
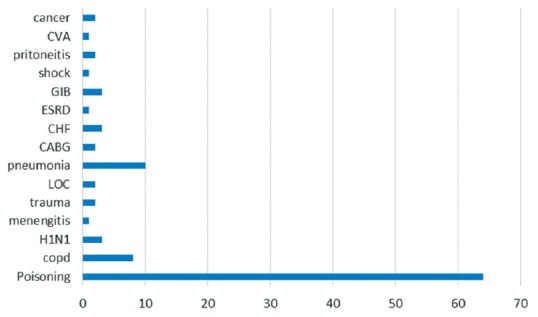
Frequency of the cause of hospitalization
Table 2.
Distribution frequency of spontaneous breathing trial according to the cause of hospitalization
Similarly, the IWI prediction regarding the success or failure of the SBT result showed success in 95 (90.5%) and failure in 10 (9.5%) cases. The agreement between the true patients' outcome after weaning and the IWI prediction revealed a Kappa coefficient of 0.413 (P < 0.001). This means that in only 41.3% of cases the IWI prediction regarding weaning was in agreement with the true SBT outcome [Table 3].
Table 3.
2×2 contingency table, frequency distribution of the spontaneous breathing trial result, and integrative weaning index prediction
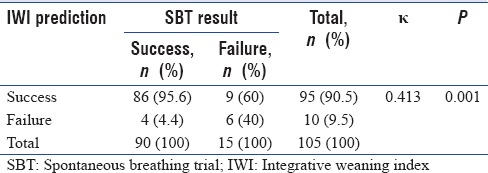
The study findings regarding the IWI predictive power showed a sensitivity of 95.6% for this index. It means that before weaning the IWI has correctly predicted the success of SBT in 95.6% of those with a true successful outcome.
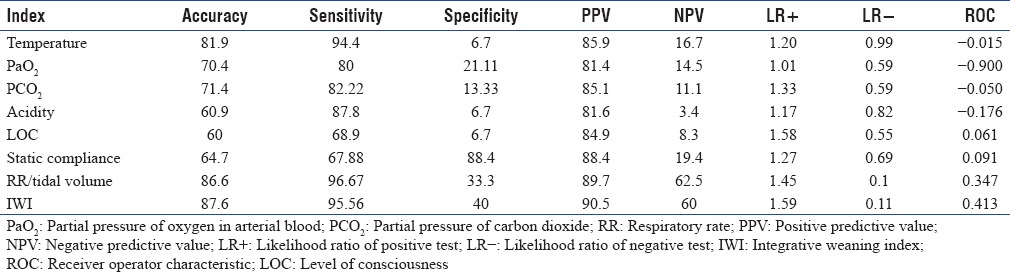
In addition, the study results declared 40% specificity for this index; this shows that this index was capable of predicting SBT failure in 40% of the patients. Based on the collected data, the positive and negative predictive values (NPVs) for IWI were 90.5% and 60%, respectively. This means that in 90.5% of the patients the true outcome after weaning (successful SBT) was in agreement with the IWI prediction whereas in 60% of the cases, the test had correctly predicted an unsuccessful outcome. The study results based on the sensitivity and specificity of the IWI showed a positive and negative likelihood ratio (NLR) of 1.59 and 0.11, respectively. Eventually, the accuracy of the IWI in the correct prediction of SBT, for either success or failure, was 87.6% [Table 4].
Table 4.
Comparing the predictive power of the parameters used by physicians and the integrative weaning index in determining the patient's readiness for weaning from mechanical ventilation
DISCUSSION
Among all patients whom were ready and were removed from the ventilation support according to the physician in charge's judgment, SBT was a success in 85.7% and a failure in 14.3%. This is consistent with the study by Eskandar et al. regarding the probable success rate following weaning. They claimed that despite all the medical treatments and care offered to patients receiving mechanical ventilation for over 24 h, the first attempt to wean is often a failure in almost 22% of the cases.[11]
The findings of the current study support a significant relationship between the length of hospitalization, the patients' respiratory parameters and the SBT outcome of the ventilation device; meaning that the prevalence of prolonged hospitalization, respiratory rate, RR-tidal volume ratio, and the inappropriate pulmonary compliance was higher among patients with an unsuccessful outcome. This result can not only be interpreted from the clinical and physiologic aspects, but similar studies also confirm these findings.[2,12] Especially when considering the RR-tidal volume ratio and the lungs static compliance, several studies have mentioned such indices as one of the main parameters associated with the weaning outcome.[10,13,14,15]
This study also revealed a fine agreement between the IWI and the parameters used by physicians in predicting the weaning outcome. As several studies have introduced IWI as an index with high sensitivity and specificity,[10,13,14] the small agreement between this index and other indices used by physicians can be attributed to the low sensitivity and specificity of the latter indices. Findings of the current study and Nemer et al. study both confirm that IWI parameters including the RR-tidal volume ratio and the lungs' static compliance are reliable parameters with high sensitivity and specificity in this respect.[10]
Given the diagnostic accuracy of this index, the results revealed 95.5% sensitivity, 40% specificity, 90.5% positive predictive value (PPV), 60% NPV, and 87.6% accuracy. However, several studies have introduced this index as a desirable tool for predicting the weaning outcome reporting 90%–97% sensitivity, 66.7%–94% specificity, a PPV of 90%–99%, NPV of 50%–93%, and an accuracy of 87%–92%.[3,10,14,16] As the comparison of these data shows, except for the specificity reported by the current study which is lower than the lowest level reported in the previous studies, other studied parameters are in the same range as previous reports.
The different reported values may be related to the different prevalence of successful and unsuccessful outcomes in different societies, various clinical characteristics of the patients, and a variety of underlying diseases in the studied populations.[17]
Another significant point is that all the aforementioned studies were performed as comparative interventional studies including a study and control group whereas the current study has a cross-sectional design due to the unfamiliarity of the authors with the mentioned index and not accepting it as an alternative to the conventional approach in predicting the patient's readiness for weaning. It is obvious that the findings of a comparative study will be different from those of a descriptive study. The positive likelihood ratio of the index was 1.59 in our study, meaning that the probability of the IWI to predict a positive outcome in those with a successful SBT is 1.59 times greater than those with a weaning failure. On the other hand, a NLR = 0.11 shows that the probability of a negative outcome prediction in those with SBT failure is 0.11 times higher than those with a successful outcome. The reported range for the IWI positive and NLR in different studies is 2.84, 16.5, 0.03–0.12, respectively.[3,10,14,16] The only point which can justify the inconsistency in these findings is the difference in study design and the association between the likelihood ratio and the specificity parameter which was less in the current study in comparison to other studies. And last but not least is the IWI accuracy which was similar to the values reported by other studies.
As mentioned in the “results” section, the accuracy of the IWI in the correct prediction of success and failure in the studied population was 88% in our study, the same value was reported from 87% to 97% in the previous studies.[10,14,16]
Moreover, the findings of the current study showed that IWI as an objective index has higher accuracy in comparison to the other parameters used by physicians in predicting the SBT outcome. This finding is in agreement with that of several other studies comparing objective protocols with the physician-oriented approach.[18,19,20,21]
This study was performed to investigate the IWI power in predicting the success and failure of the SBT outcome in patients under mechanical ventilation, hospitalized in Imam Reza Educational Hospital, in 1 year.
Given the findings of the current study and previous reports, it can be concluded that weaning indices which only evaluate one function usually have low accuracy. Therefore, the IWI which can evaluate main functions such as RR-tidal volume ratio, compliance, RR, oxygenation and the CROP index (Compliance, Resistance, Oxygenation, Pressure Index), has higher accuracy and can be considered as a more objective index compared to the indices used by physicians in predicting success or failure.
Therefore, it is recommended to use IWI as a valuable clinical parameter in determining the readiness of patients for weaning from ventilation support besides predicting the weaning outcome.
Eventually, conducting complementary studies with different methodologies in other clinical settings is highly recommended in the future studies. Moreover, the IWI power could also be studied in the pediatric ICUs.
CONCLUSION
The IWI as a more objective indicator has acceptable accuracy and power for predicting the 2-h SBT result. Therefore, in addition to the reliable prediction of the final weaning outcome, it has favorable power to predict if the patient is ready to breathe spontaneously as the first step to weaning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Soran A, Chelluri L, Lee KK, Tisherman SA. Outcome and quality of life of patients with acute pancreatitis requiring intensive care. J Surg Res. 2000;91:89–94. doi: 10.1006/jsre.2000.5925. [DOI] [PubMed] [Google Scholar]
- 2.Monaco F, Drummond GB, Ramsay P, Servillo G, Walsh TS. Do simple ventilation and gas exchange measurements predict early successful weaning from respiratory support in unselected general intensive care patients? Br J Anaesth. 2010;105:326–33. doi: 10.1093/bja/aeq184. [DOI] [PubMed] [Google Scholar]
- 3.Madani SJ, Saghafinia M, Nezhad HS, Ebadi A, Ghochani A, Tavasoli AF, et al. Validity of integrative weaning index of discontinuation from mechanical ventilation in Iranian ICUs. Thrita. 2013;2:62–8. [Google Scholar]
- 4.Tobin MJ. Advances in mechanical ventilation. N Engl J Med. 2001;344:1986–96. doi: 10.1056/NEJM200106283442606. [DOI] [PubMed] [Google Scholar]
- 5.MacIntyre N. Ventilator discontinuation process: Evidence and guidelines. Crit Care Med. 2008;36:329–30. doi: 10.1097/01.CCM.0000297958.82589.E2. [DOI] [PubMed] [Google Scholar]
- 6.MacIntyre N. Discontinuing mechanical ventilatory support. Chest. 2007;132:1049–56. doi: 10.1378/chest.06-2862. [DOI] [PubMed] [Google Scholar]
- 7.Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Peñuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188:220–30. doi: 10.1164/rccm.201212-2169OC. [DOI] [PubMed] [Google Scholar]
- 8.Epstein SK. Decision to extubate. Intensive Care Med. 2002;28:535–46. doi: 10.1007/s00134-002-1268-8. [DOI] [PubMed] [Google Scholar]
- 9.Epstein SK. Extubation failure: An outcome to be avoided. Crit Care. 2004;8:310–2. doi: 10.1186/cc2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nemer SN, Barbas CS, Caldeira JB, Cárias TC, Santos RG, Almeida LC, et al. A new integrative weaning index of discontinuation from mechanical ventilation. Crit Care. 2009;13:R152. doi: 10.1186/cc8051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eskandar N, Apostolakos MJ. Weaning from mechanical ventilation. Crit Care Clin. 2007;23:263–74, x. doi: 10.1016/j.ccc.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Esteban A, Alía I, Tobin MJ, Gil A, Gordo F, Vallverdú I, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish lung failure collaborative group. Am J Respir Crit Care Med. 1999;159:512–8. doi: 10.1164/ajrccm.159.2.9803106. [DOI] [PubMed] [Google Scholar]
- 13.Nemer SN, Barbas CS. Predictive parameters for weaning from mechanical ventilation. J Bras Pneumol. 2011;37:669–79. doi: 10.1590/s1806-37132011000500016. [DOI] [PubMed] [Google Scholar]
- 14.El-Baradey GF, El-Shmaa NS, Ganna SA. Can integrative weaning index be a routine predictor for weaning success? Indian J Crit Care Med. 2015;19:703–7. doi: 10.4103/0972-5229.171352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boniatti VM, Boniatti MM, Andrade CF, Zigiotto CC, Kaminski P, Gomes SP, et al. The modified integrative weaning index as a predictor of extubation failure. Respir Care. 2014;59:1042–7. doi: 10.4187/respcare.02652. [DOI] [PubMed] [Google Scholar]
- 16.Nezhad HS, Davood S, Jalal S. Comparison of the outcomes of weaning with currrent and IWI-based methods in patients admitted to ICU of selected hospitals in Tehran. Iranian Journal of Anaesthesiology and Critical Care. 2013;3:17. [Google Scholar]
- 17.Zhou XH, McClish DK, Obuchowski NA. Statistical Methods in Diagnostic Medicine. Hoboken, New Jersey: John Wiley & Sons; 2009. [Google Scholar]
- 18.Chaiwat O, Sarima N, Niyompanitpattana K, Komoltri C, Udomphorn Y, Kongsayreepong S, et al. Protocol-directed vs. physician-directed weaning from ventilator in intra-abdominal surgical patients. J Med Assoc Thai. 2010;93:930–6. [PubMed] [Google Scholar]
- 19.Blackwood B, Wilson-Barnett J, Patterson CC, Trinder TJ, Lavery GG. An evaluation of protocolised weaning on the duration of mechanical ventilation. Anaesthesia. 2006;61:1079–86. doi: 10.1111/j.1365-2044.2006.04830.x. [DOI] [PubMed] [Google Scholar]
- 20.Girard TD, Ely EW. Protocol-driven ventilator weaning: Reviewing the evidence. Clin Chest Med. 2008;29:241–52, v. doi: 10.1016/j.ccm.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Kirakli C, Ediboglu O, Naz I, Cimen P, Tatar D. Effectiveness and safety of a protocolized mechanical ventilation and weaning strategy of COPD patients by respiratory therapists. J Thorac Dis. 2014;6:1180–6. doi: 10.3978/j.issn.2072-1439.2014.09.04. [DOI] [PMC free article] [PubMed] [Google Scholar]


