Abstract
Background and Aims:
Increasing and indiscriminate use of antibiotics has led the bacteria to develop resistance to most of the antibiotics. Beta-lactamase production is the mechanism of resistance to beta-lactams. Extended-spectrum beta-lactamases (ESBLs) have been found in the members of Enterobacteriaceae such as Escherichia coli and Klebsiella spp. which are the common health-care-associated pathogens. The aim was to study the rate of fecal carriage of ESBL-producing Enterobacteriaceae in patients admitted to the Intensive Care Unit (ICU) of tertiary care hospital and follow them subsequently for the development of infections.
Materials and Methods:
A hospital-based descriptive study was conducted in the department of microbiology of a tertiary care hospital for a period of 2 months from June 2016 to August 2016. Rectal swabs were collected from the patients admitted to the ICU after a period of 48 h. The swab was inoculated onto a special selective media (ChromID ESBL media). The results were noted according to the color of the colony produced. These patients are followed for the development of infection and the ESBL-producing organisms.
Results:
A total of 60 rectal swabs were cultured, 39 (65%) showed a positive result. Out of which, 22 (56%) were ESBL-producing E. coli and 17 (43%) Klebsiella spp. Twenty-three (38%) of the total patients screened were infected with ESBL-producing organisms.
Conclusion:
The study revealed high rates of carriage of ESBL producers in patients admitted to the ICU.
Keywords: Escherichia coli, extended-spectrum beta-lactamase, fecal carriage, Intensive Care Unit
INTRODUCTION
The widespread use of antibiotics during the past few decades has led the bacteria to acquire resistance enzymes. The extended-spectrum beta-lactamases (ESBLs) hydrolyze extended-spectrum cephalosporins but are usually susceptible to inhibition by clavulanic acid and tazobactam. The genes for ESBL production are carried on plasmids, and this contributes to spread of these resistant genes in the bacterial population. The first reports of ESBLs were first in the mid-1980s and were mostly in Klebsiella pneumoniae and Escherichia coli.[1]
Carriage of ESBL-producing commensal strains of Enterobacteriaceae is a threat as it can get transferred to the pathogenic strains. The first reports on fecal carriage of ESBL-producing Enterobacteriaceae were from Spain and Poland in 2001 and 2002, respectively.[2]
Knowledge of the fecal carriage of ESBL strains is essential for formulation of antibiotic policy. ESBL strains render the antibiotic therapy ineffective and contribute to the seriousness of hospital-acquired and community infections.[3]
Infections with ESBL-producing organisms are associated with higher morbidity, longer hospitalization. Infections due to these organisms are hospital acquired with stay in the Intensive Care Units (ICUs), exposure to antibiotics, and in dwelling devices being the associated risk factors.[4] The infections caused by ESBL producers are urinary tract infection, intra-abdominal infections such as peritonitis, cholangitis, and intra-abdominal abscess.[5]
This study focuses on screening for fecal carriage of ESBL-producing Enterobacteriaceae members using rectal swab cultures in patients admitted to ICU of a tertiary care hospital and follows the patients for the subsequent development of infections with ESBL-producing organisms in the gut flora.
MATERIALS AND METHODS
A hospital-based descriptive study was conducted in the diagnostic microbiology laboratory of a tertiary care hospital for a period of 2 months from June 2016 to August 2016. Rectal swabs were collected from all the patients admitted to the ICU after a period of 48 h. The swab was inoculated onto a special selective media (ChromID ESBL media, BioMerieux, France) and incubated at 37°C for 18–24 h. The color of the colonies grown on the media was matched with the color chart that is provided in the kit literature for the detection of ESBL producers.[5]
The ESBL producers were confirmed by simultaneously performing the Clinical and Laboratory Standards Institute confirmatory test for the detection of ESBL using cefotaxime, ceftazidime, cefotaxime/clavulanate (30/10 μg), and ceftazidime/clavulanate (30/10 μg).
Descriptive statistics were used to evaluate the rate of infection in ESBL-colonized and noncolonized patients.
RESULTS
Sixty patients were included in the study. The rectal swabs were cultured, of which 39 (65%) showed a positive result. Out of which, 22 (56%) were ESBL-producing E. coli and 17 (43%) Klebsiella spp.
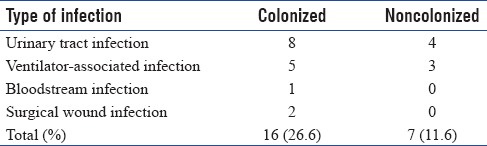
All the sixty patients screened were followed for the development of infection and 23 (38%) developed infection with ESBL-producing organisms. Infections were seen both in colonized and noncolonized patients. The average time for the development of infection in colonized patients was 48–72 h. The common infection diagnosed was urinary tract infection 12 (20%) followed by ventilator-associated infection 8 (13.3%) [Table 1]. The rate of infection was higher in colonized patients (26.6%) compared to noncolonized patients (11.6%) [Table 1].
Table 1.
Infections seen in colonized and noncolonized patients
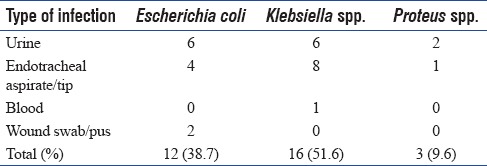
Thirty-one organisms were isolated from the clinical specimen obtained from both colonized and noncolonized patients. Among the 31 bacteria, ESBL-producing Klebsiella spp. were 16 (51.6%), E. coli 12 (38.7%), and Proteus spp. 3 (9.6%) Table 2.
Table 2.
Extended-spectrum beta-lactamase producers isolated from clinical specimen
DISCUSSION
The widespread indiscriminate use of antimicrobials has led to the emergence and spread of antibiotic resistance. The prevalence of ESBL-producing isolates has increased in the past few decades. Outbreaks of infections in the health-care settings have been linked to higher rates of fecal carriage of ESBL-producing isolates. Our study showed a rate of 65% fecal carriage of ESBL producers. The prevalence of fecal carriage of ESBLs in our study was higher than similar studies conducted in South Africa[1] and Netherlands that reported rates of 32% and 25.9%, respectively.[6] In a study done by Paniagua et al., the rates of fecal carriage of ESBL producers had increased from 0.3% to 11.8% from 1991 to 2003.[7]
The higher rate of carriage in our study may be due to increased exposure of antibiotics over the years.
Our study showed a higher rate of subsequent development of infection as 26.6% with ESBL producers in ESBL colonizers compared to 11.6% infection rate in noncolonizers. The previous studies have reported 65% carriage rate in patients with urinary tract infection and 8.5% carriage rate in healthy individuals.[8] A study by Reddy et al. showed that 8.5% of the ESBL colonizers developed a subsequent ESBL bloodstream infections.[9] In our study, the rate of bloodstream invasion was 2.5% in colonized patients.
The rates of colonization with multiresistant isolates have shown an alarming rise over the past few decades. The matter of concern is the emergence and spread of ESBL-producing isolates. The rectal surveillance for ESBL-producing Enterobacteriaceae will play a pivotal role in infection control. The ESBL-colonized patients act as source of infection to the other hospitalized patients in high-risk areas.
Asymptomatic colonization of ESBLs can thus be a threat to the subsequent development of infection, especially in the ICU settings. The surveillance of rates of fecal carriage of ESBL-producing Enterobacteriaceae may be helpful to track and monitor the spread of these organisms in the hospital settings. The rates of infection can be controlled by following strict infection control measures.
CONCLUSION
The study revealed high rates of carriage of ESBL producers in patients admitted to the ICU. Screening of the ESBL producers in the ICU's and proper implementation of infection control measures can control the infections in ICU.
Financial support and sponsorship
The authors are grateful to Manipal University for the support.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are grateful to Manipal University for the support.
REFERENCES
- 1.Isendahl J, Turlej-Rogacka A, Manjuba C, Rodrigues A, Giske CG, Nauclér P, et al. Fecal carriage of ESBL-producing E. coli and K. pneumoniae in children in Guinea-Bissau: A hospital-based cross-sectional study. PLoS One. 2012;7:e51981. doi: 10.1371/journal.pone.0051981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woerther PL, Burdet C, Chachaty E, Andremont A. Trends in human fecal carriage of extended-spectrum β-lactamases in the community: Toward the globalization of CTX-M. Clin Microbiol Rev. 2013;26:744–58. doi: 10.1128/CMR.00023-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valverde A, Coque TM, Sánchez-Moreno MP, Rollán A, Baquero F, Cantón R, et al. Dramatic increase in prevalence of fecal carriage of extended-spectrum beta-lactamase-producing Enterobacteriaceae during nonoutbreak situations in Spain. J Clin Microbiol. 2004;42:4769–75. doi: 10.1128/JCM.42.10.4769-4775.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathai D, Kumar VA, Paul B, Sugumar M, John KR, Manoharan A, et al. Fecal carriage rates of extended-spectrum β-lactamase-producing Escherichia coli among antibiotic naive healthy human volunteers. Microb Drug Resist. 2015;21:59–64. doi: 10.1089/mdr.2014.0031. [DOI] [PubMed] [Google Scholar]
- 5.Réglier-Poupet H, Naas T, Carrer A, Cady A, Adam JM, Fortineau N, et al. Performance of chromID ESBL, a chromogenic medium for detection of Enterobacteriaceae producing extended-spectrum beta-lactamases. J Med Microbiol. 2008;57:310–5. doi: 10.1099/jmm.0.47625-0. [DOI] [PubMed] [Google Scholar]
- 6.Kluytmans-van den Bergh MF, Verhulst C, Willemsen LE, Verkade E, Bonten MJ, Kluytmans JA, et al. Rectal carriage of extended-spectrum-beta-lactamase-producing Enterobacteriaceae in hospitalized patients: Selective preenrichment increases yield of screening. J Clin Microbiol. 2015;53:2709–12. doi: 10.1128/JCM.01251-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paniagua R, Valverde A, Coque TM, Baquero F, Cantón R. Assessment of prevalence and changing epidemiology of extended-spectrum beta-lactamase-producing Enterobacteriaceae fecal carriers using a chromogenic medium. Diagn Microbiol Infect Dis. 2010;67:376–9. doi: 10.1016/j.diagmicrobio.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Rodríguez-Baño J, López-Cerero L, Navarro MD, Díaz de Alba P, Pascual A. Faecal carriage of extended-spectrum beta-lactamase-producing Escherichia coli: Prevalence, risk factors and molecular epidemiology. J Antimicrob Chemother. 2008;62:1142–9. doi: 10.1093/jac/dkn293. [DOI] [PubMed] [Google Scholar]
- 9.Reddy P, Malczynski M, Obias A, Reiner S, Jin N, Huang J, et al. Screening for extended-spectrum beta-lactamase-producing Enterobacteriaceae among high-risk patients and rates of subsequent bacteremia. Clin Infect Dis. 2007;45:846–52. doi: 10.1086/521260. [DOI] [PubMed] [Google Scholar]


