Abstract
Objective:
This study examined the impact of shoe closure on plantar thermal stress response (TSR), which is known to be a surrogate of shear stress and skin perfusion. It is aimed to explore potential impact of shoe closure on increasing risk factors associated with plantar ulcers in people with diabetic peripheral neuropathy (DPN).
Methods:
Fifteen eligible subjects were enrolled. The left foot was used as a reference and fitted to a self-adjusted and habitual lace-tightening method by each subject. The right foot was used as a test closure and fitted into three lace closure conditions: loose, tight, and preset optimal closure (reel clutch, BOA technology). Thermal images were taken after 5 minutes of acclimatization (pre-trial) and immediately after 200 walking steps in each shoe closure condition (post-trial). TSR was calculated from the thermal images.
Results:
TSR was significantly higher in the test closure with loose (70.24%, P = .000) and tight (66.85%, P = .007) and lower (−206.53%, P = .000) in the preset optimal closure when compared to the reference closure. Only lace closure conditions affected TSR with no significant impact from age, BMI, and gender in our sample in a multivariable regression model.
Conclusion:
The results from this study suggest that shoelace closure technique can have a profound effect on TSR. It therefore stands to reason that optimal lace closure may have an impact in reducing risk of plantar ulcers in people with DPN. Interestingly, results revealed that even a self-adjusted lace closure may not be necessarily optimal and a preset closure setting like reel clutch might ultimately be recommended to minimize risk. Further study is warranted to confirm or refute these interesting results.
Keywords: diabetic foot ulcer, shear stress, shoelace, shoe closure, thermal response to stress
Novel footwear technologies attempt to improve human foot protection. Shoelace tightening systems are an example of such efforts to maximize the fitting and comfort of shoes. Optimizing the closure of footwear is particularly important among those who are vulnerable to foot injuries such as people with diabetic peripheral neuropathy (DPN) which impacts about 50% of people with diabetes.1 People with DPN and loss of protective sensation have reduced peripheral nerve functioning, which means the nerves do not carry pain sensation to the brain from the feet. Thus treading on something, wearing tight shoes, cuts, blisters, and bruises can all develop into diabetic foot ulcers (DFUs) due to lack of plantar sensation. The cumulative risk for a patient with diabetes to develop this condition is estimated to be 25%1-3 and costs Americans about $23 billion in direct medical expenses each year.4
While many studies have demonstrated the importance of effective offloading to reduce risk of DFU, appropriate shoe closure to reduce DFU has received little attention. Tight shoes disrupt the blood flow, slow tissue regeneration, and reduce heat transfer.5 High tissue temperature and dally recovery from impacts are major factors in DFU.6-8 On the other hand, lacing the knots loosely allows for foot soles to slide inside the shoe and endure higher shear stresses that will also increase the temperature on the soles. An increased level of sole shear stresses has also been associated with foot ulcer formations.9,10
In-shoe shear stress measurements remain a challenge for researchers and industries. The difficulties in measuring shear stress come from the sensitivity of the sensors to the environmental factors of higher temperature and moisture in the footwear.11 Element cross-talk, calibration difficulties, and handling of the attached wires also add to the problems.12 Even with the best measurement method, the data on shear stress are mostly localized to the areas of sensor placement under the foot. To overcome these challenges an alternative method was implemented by Wrobel et al in 2014.13 They argued that shear stress on the sole will result in a hike in plantar temperature. They showed that the use of a shear reduction insole significantly slows the increase in temperature compared to standard control insoles. In addition, the continuous map of temperature from an infrared camera allowed them to identify the distribution of shear stress throughout the sole.13
The purpose of this study is to assess the effect of optimal shoelace tightening on temperature rise (thermal stress response) on the sole during walking. This will allow us to discuss the consequence of nonoptimized shoe fitting on the confounding factors of shear stress and lack of blood flow in DFU. In particular, we will compare a recently developed optimal lace tightening technology (reel clutch) to normal, tight and loose fitting shoes with traditional laces.
Methods
Participants
This study required a significant amount of walking with different shoe closures; thus to minimize risk of foot injury, only healthy and young subjects (age < 30) were recruited. The subjects were excluded if they had any foot pain, major foot deformity, or any condition that may impact their gait and balance. The study was approved by the University of Arizona Institutional Review Board. Written informed consent, according to the principles expressed in the Declaration of Helsinki,14 were obtained from all subjects before participation.
Experimental Trials
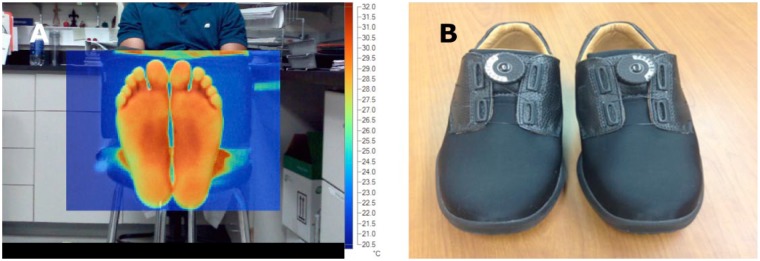
Each subject was asked to walk in three foot closure conditions. To explore whether shoe closure would impact thermal stress response, a thermal image was taken before and immediately after each walking test. Thermal imaging was conducted with a Fluke® Ti25 thermal imager (Fluke Corporation, Everett, WA, USA). There was a 5-minute acclimatization period without weight-bearing, shoes, or socks prior to baseline thermal imaging for each trial and standardized walking stress test.15 In random sequence, each shoe closure condition was tested for gait during habitual speed.16 Baseline thermal imaging was done right after acclimatization and before the start of each trial. Thermal images of the barefoot soles were also taken immediately after 200 steps of walking in each trial (Figure 1A).
Figure 1.
(A) Experimental setup for thermal imaging of the foot sole. Each subject was asked to take off shoes and socks before capturing the image. The images were taken after 5 minutes acclimatization (pre-trial) and immediately after 200 steps of walking in each trial (post-trial). (B) The BOA reel clutch technology shoes.
Shoe Closure Conditions
To have a fair comparison between different shoe closure conditions, one side was considered as a reference and the contralateral side was used as a tested shoe closure condition. In all of the walking trials the left foot (the reference shoe closure) had a well-fitting regular lace shoe (henceforth referred to as the reference shoe closure). The lace tightening was self-adjusted by subjects and claimed to be their habitual closuring tightening method. The right foot had either loose lace, tight lace or preset optimal closure using reel clutch technology (BOA Technology Inc, Denver, CO, USA; Figure 1B) fittings in the trials that henceforth will be referred to as loose, tight and optimal closures respectively. The closure conditions were evaluated using the method of heel fit.17 The loose, reference and tight conditions corresponded to very loose, loose, and fit conditions respectively as was described by Tanigawa et al.17
Data Analysis
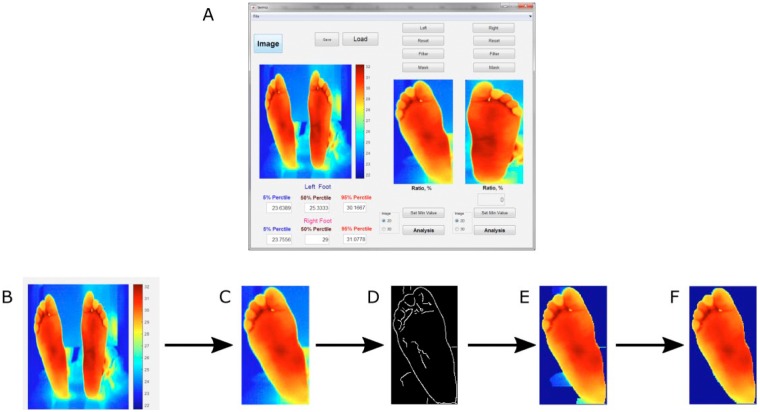
A custom image processing toolbox (Figure 2) designed and validated in our previous study15 was used to automatically isolate each foot from the thermal image using an edge detection algorithm. The toolbox also afforded manual enhancement and noise removal prior to the analysis and allows separation between right and left foot thermal images. Each processed thermal image was manually inspected and if needed further image enhancement was applied. We estimated the 5th, 50th, and 95th temperature percentiles from the extracted thermal images of the right and left foot as recommended by Najafi et al study.15 For the purpose of this study, only the 95th percentile value representing a hot spot was reported. Thermal stress response was defined as changes in 95th percentile value post walking trial compared to baseline. The thermal stress response was calculated for each side and each shoe closure condition.
Figure 2.
Overview of image processing toolbox and steps for acquiring thermal stress response. (A) Toolbox graphical user interface. (B) Raw thermal image. (C) Isolation of one foot (eg, left). (D) Filtering the image by making a complete boundary of the sole. (E) Masking of the filtered image. (F) Isolated image of the sole that will be used to estimate 5th, 50th, and 95th percentiles of temperature distribution.
Results are expressed as mean ± standard deviation (SD). Mann-Whitney U test was used to compare between feet (ie, right and left) plantar thermal values as baseline. If no significant difference between two sides at baseline was observed (indicating sufficient acclimatization), between-foot thermal stress response difference was assessed using analysis of variance (ANOVA) after adjustment for age, body mass index (BMI), and gender.
The ANOVA was performed to study the effect of age, trial group, BMI, and gender on the temperature change between the soles after 200 steps. Post hoc Tukey’s test was performed for the factors that show a significant effect on the response variable.
All analyses were performed using JMP (version 11; SAS Institute Inc), with a significance level of P < .05. In case of difference in baseline temperatures, the difference in temperature change from the baseline on each foot was calculated as the study response.
Results
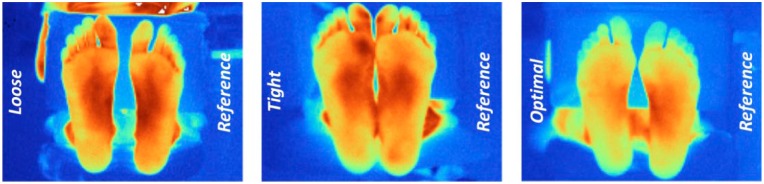
Fifteen subjects (age: 21.2 ± 1.1 years, BMI: 24.4 ± 4.5 kg/m^2, 60% male) participated in the study. No between feet temperature differences were observed after each acclimatization phase and prior each walking test condition (P > .050), indicating sufficient acclimatization duration prior initiating the next trial. Figure 3 shows a sample of thermal images of the plantar regions of both feet (right: closure condition; left: reference) for each closure condition after respective 200 steps trial . On average, TSR was significantly higher for the loose closure (70.24%, P = .000) and tight closure (66.85%, P = .007) conditions and lower (−206.53%, P = .000) in the optimal closure condition (Figure 4) when compared to the reference side (left foot with self-adjusted shoe closure). No statistically significant difference in TSR was observed between the loose closure and the tight closure conditions (P = .971). Table 1 summarizes the results of multivariate regression model including TSR as dependent variable and the closure condition, age, BMI, and gender as independent variables. The effects results show that TSR depends only on the closure condition and how the shoelaces are tightened (P = .000). The post hoc Tukey’s test on the closure conditions (Table 2) shows that there is no difference between the mean intersole changes in TSR for the loose closure and the tight closure conditions (P = .981); however mean intersole changes in TSR for the optimal closure were different from both of the loose and the tight conditions (P = .000).
Figure 3.
A sample of thermal images of the plantar regions of both feet (right: closure condition; left: reference) for each closure condition after respective 200 steps trial. Notice the difference in two sole temperatures. Here red represents highest temperature and blue is the minimum temperature. Each foot is labeled with their respective shoelace closure condition.
Figure 4.
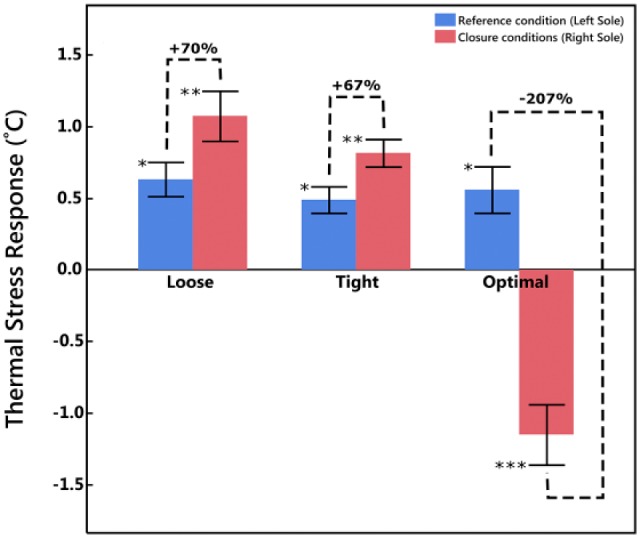
The increase in thermal stress response (TSR) for the reference closure (blue) and the testing closure conditions (red). The result show an increase in TSR for loose and tight closure conditions and a decrease in TSR for self-adjusted closure (denoted as optimize from the subject’s perception). Bars with the same number of asterisks are statistically similar.
Table 1.
The Effect of the Independent Variables on the Difference of Posttrial Left and Right Sole Temperature Change.
| Source | Sum of squares | Mean square | F ratio | Prob > F |
|---|---|---|---|---|
| Closure condition | 27.88 | 13.94 | 122.39 | <.0001* |
| Age | 0.01 | 0.01 | 0.06 | .8087 |
| BMI | 0.01 | 0.01 | 0.13 | .7250 |
| Gender | 0.06 | 0.06 | 0.56 | .4587 |
The closure condition is the only parameter that is affecting the response (P < .0001). * symbole indicates that statistical significant level has been reached.
Table 2.
Post Hoc Test on the Difference Between Tightness Levels.
| Level | Level | Difference | SE Diff | Lower CL | Upper CL | P value |
|---|---|---|---|---|---|---|
| Loose | Optimal | 1.68 | 0.12 | 1.38 | 1.98 | <.0001* |
| Tight | Optimal | 1.66 | 0.12 | 1.36 | 1.96 | <.0001* |
| Loose | Tight | 0.03 | 0.12 | −0.27 | 0.33 | .9712 |
The optimize BOA technology shoes demonstrate a different mean in intersole temperature change compared to the loose and tight trials (P < .0001). The tight and loose trials had no difference in mean intersole temperature change. * symbole indicates that statistical significant level has been reached.
Discussion
The effect of footwear closure condition on foot sole temperature changes in response to walking (thermal stress response) was studied. The change in magnitude of sole TSR was assumed to be in response to increased shear stress on the sole and/or a decrease of blood flow to cool the sole down.13 Results suggest that shoe closures could magnify TSR, thus they may increase risk of plantar ulcers in people at risk like those with DPN and loss of protective sensation. In this study, we examined TSR after 200 waking steps. However, given the fact that daily average of walking steps is estimated to be 7000-8000 steps for humans with unbroken walking bout also reaching up to 1000 steps in some individuals with DPN,18,19 the impact of shoe closure condition on TSR could be even more pronounced and potential harmful to lower extremity health. The negative impact of TSR increase could be dramatic in people with DPN and loss of protective sensation who are prone to development and redevelopment of DFUs.6-8,20,21
Considering that TSR was tested between right and left feet, which were exposed to identical walking condition and the same number of steps with no plantar TSR difference at baseline and after each acclimatization, it could be assumed that TSR difference observed between two feet is only in response to shoe closure condition. To ensure that foot health condition will not impact the results, in this proof of concept study, only healthy young subjects with no foot problem were recruited which confirms that observed difference in TSR between two feet is not affected by foot health condition. However, it may be possible that subjects walked slightly different in each of the shoe closure conditions, but this should not bias the results of this study, since TSR was compared between right (the test closure condition) and left (the reference closure condition), which were exposed to the same walking parameters. However, the comparison between loose closure and tight closure conditions could be biased by potential changes in spatiotemporal parameters of gait, but the bias is assumed to be negligible as demonstrated previously,13 where in-shoe changes in shear stress didn’t significantly impact spatiotemporal parameters of gait.
TSR values for the reference closure shoe (left side) were almost identically similar for all three walking trials, suggesting a high test-rest reliability for TSR measurements. The average increase in the reference closure sole temperatures (0.56 ± 0.40°C), in response to 200 walking steps, was also similar to the reported values in the previous study, in which people with DPN were studied13 (approximated 0.73 ± 0.27°C). Thus, we anticipate to observe similar TSR in people with DPN in response to shoe closure condition. However, this should be validated in the context of another study. In addition, future study is warrant to explore whether optimizing shoe closure, using a preset optimal shoe closure technology similar to reel clutch, could be effective in reducing the risk of plantar ulcers in people with DPN and loss of protective sensation.
An interesting observation in this study was revealing that self-adjusted lace tightness based on subject’s perception of optimal shoe closure may not necessary be optimal. In other words, when TSR was compared between a preset closure technology (BOA reel clutch) and a self-set closure, the TSR was significantly lower in the preset closure. Another study should be addressed to examine whether using a preset closure technology could be effective in reducing the risk of plantar ulcers in people with DPN.
Our study suggests that both loose closure and tight closure have similar effect on increasing TSR .This finding suggests that the thermal stress response, as measured by the post-trial temperature change of the sole in response to walking, is a quadratic space (Figure 5), where there is minima range in the thermal stress response, that allows for a heathy skin perfusion and preventing extensive sliding of the sole against the surface of the shoe. The extent of this optimal range (threshold for healthy/unhealthy thermal stress response; see Figure 5) can be measured in terms of cut-off torque of the reel clutch mechanism of the BOA closure technology. This goal requires future experimental studies.
Figure 5.
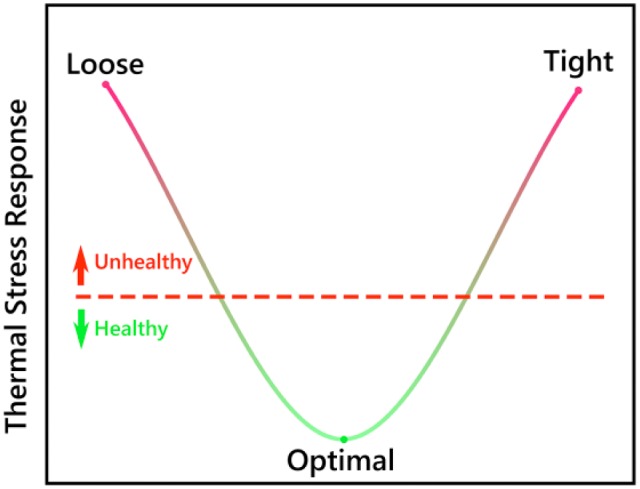
Quadratic space for distribution of thermal stress on the soles. The thermal stress response is high for the loose closure and the tight closure conditions. It was however low for the optimal closure. The red dashed line represents a conceptual threshold for the thermal stress response that should be determined to allow a guideline for production of new technologies addressing the optimal shoelace (preset closure) tightness.
We didn’t control the ambient temperature during trials. However, we believe this has minimal impact on our comparative results. All comparisons were pairwise and in comparison with the contralateral side (the reference foot). The test condition for both feet were identical except for the shoe lace tight condition, which were remained constant for the left foot (the reference foot) and changed for the right foot (the tested foot) condition. Since all tests were done in an air-conditioned facility and all tests were done in less than an hour duration, we believe the ambient temperature were not changed inter trials. Furthermore, since we estimated thermal stress response (change in plantar temperature post walking) after 5-minute acclimatization, we believe the ambient temperature will have minimum impact on our results.
On the same note, we didn’t measure core body temperature. However, baseline plantar temperature for each foot was measured using thermal camera, to ensure that plantar temperature before initiating walking trial is identical between two feet. Our results confirmed that before initiating each walking trail, there is no significant difference between feet plantar temperature. Thus we concluded that TSR difference observed between feet is due to shoelace tightening condition.
For testing loose and tight shoelace conditions, the footwear between the right and left foot were identical. Thus, the observed TSR difference between feet, is independent of shoe type. However, the type of footwear may amplify or reduce TSR difference between feet in response to shoelace tightening. This study is under power to examine the impact of footwear. Thus another study should be addressed to explore whether type of footwear is important on TSR irrespective of shoe lace tightening. In addition, when we compared a preset optimal shoelace closure (BOA technology), the footwear in the reference foot was not identical to the test foot. This may describe in part the difference observed in between feet TSR values. Another study with identical footwear condition should be addressed to confirm whether the magnitude of improvement observed in this study is uniquely due to optimization of shoelace closure or combination of shoelace and footwear design.
This study has few limitations. The sample size is convenient and the study should be considered as an exploratory proof of concept study. In addition, to minimize the risk and control the major confounders (eg, foot problems, poor skin perfusion, limb discrepancy, etc), only healthy and young subjects with no foot pathology were recruited. As discussed above, since the thermal stress response values in the reference foot were similar to the values observed in people with DPN, we may conclude that results would be generalizable to those, who are at risk of plantar ulcers as well. The fact that results were independent of age, BMI, and gender, may also conclude that similar interaction between TSR and shoe tightness may be observed in older adults irrespective of age, gender and BMI, but this needs to be confirmed in another study.
In conclusion, this pilot study reveals that shoelace tightening could play an important role in reducing or increasing risk factors associated with foot sole health. In addition, this study suggests that thermal stress response could be in further enhanced by using a preset closure technology compared to self-adjusted tightness, thus reducing the risk of plantar ulcers in those with DPN and loss of protective sensation.
Acknowledgments
None of the authors are employed or contracted by the funders. The sponsors did not contribute to subject recruitment, data analysis, or interpretation of the results. The authors would like to thank Ivan Marin who contributed in subject recruitment, study coordination, and data analysis.
Footnotes
Abbreviations: ANOVA, analysis of variance; BMI, body mass index; DFU, diabetic foot ulcer; DPN, diabetic peripheral neuropathy; SD, standard deviation; TSR, thermal stress response.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The project described was supported in part by a grant from the Qatar National Research Foundation (Award NPRP 4-1026-3-277, http://www.qnrf.org/), Avex, LLC, and BOA Technology. The content is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
References
- 1. Lord SR, Sambrook PN, Gilbert C, et al. Postural stability, falls and fractures in the elderly: results from the Dubbo Osteoporosis Epidemiology Study. Med J Australia. 1994;160:684-685, 688-691. [PubMed] [Google Scholar]
- 2. Barshes NR, Sigireddi M, Wrobel JS, et al. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle. 2013;4:21847-P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Apelqvist J, Armstrong DG, Lavery LA, Boulton AJ. Resource utilization and economic costs of care based on a randomized trial of vacuum-assisted closure therapy in the treatment of diabetic foot wounds. Am J Surg. 2008;195:782-788. [DOI] [PubMed] [Google Scholar]
- 4. Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for Medicare and private insurers. Diabetes Care. 2014;37:651-658. [DOI] [PubMed] [Google Scholar]
- 5. Leonard DR, Farooqi MH, Myers S. Restoration of sensation, reduced pain, and improved balance in subjects with diabetic peripheral neuropathy. Diabetes Care. 2004;27:168-172. [DOI] [PubMed] [Google Scholar]
- 6. Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, Lavery LA. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Am J Med. 2007;120:1042-1046. [DOI] [PubMed] [Google Scholar]
- 7. Houghton VJ, Bower VM, Chant DC. Is an increase in skin temperature predictive of neuropathic foot ulceration in people with diabetes? A systematic review and meta-analysis. J Foot Ankle Res. 2013;6:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wrobel JS, Najafi B. Diabetic foot biomechanics and gait dysfunction. J Diabetes Sci Technol. 2010;4:833-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cavanagh PR, Hewitt F, Perry J. In-shoe plantar pressure measurement: a review. Foot. 1992;2:185-194. [Google Scholar]
- 10. Cavanagh PR, Ulbrecht JS, Caputo GM. New developments in the biomechanics of the diabetic foot. Diabetes Metab Res Rev. 2000;16(suppl 1):S6-S10. [DOI] [PubMed] [Google Scholar]
- 11. Rajala S, Lekkala J. Plantar shear stress measurements—a review. Clin Biomech (Bristol, Avon). 2014;29:475-483. [DOI] [PubMed] [Google Scholar]
- 12. Mohammad I, Huang H. “Pressure and shear sensing based on microstrip antennas.” SPIE Smart Structures and Materials+ Nondestructive Evaluation and Health Monitoring. International Society for Optics and Photonics; 2012: 83451. [Google Scholar]
- 13. Wrobel JS, Ammanath P, Le T, et al. A novel shear reduction insole effect on the thermal response to walking stress, balance, and gait. J Diabetes Sci Technol. 2014;8:1151-1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191. [DOI] [PubMed] [Google Scholar]
- 15. Najafi B, Wrobel JS, Grewal G, et al. Plantar temperature response to walking in diabetes with and without acute Charcot: the Charcot Activity Response Test. J Aging Res. 2012;2012:140968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Najafi B, Khan T, Fleischer A, Wrobel J. The impact of footwear and walking distance on gait stability in diabetic patients with peripheral neuropathy. J Am Podiatr Med Assoc. 2013;103:165-173. [DOI] [PubMed] [Google Scholar]
- 17. Tanigawa T, Masashi H, Naoto F, et al. Shoe-fit is correlated with exercise tolerance in community-dwelling elderly people. Footwear sci. 2015; 7: 37-42. [Google Scholar]
- 18. Najafi B, Crews RT, Wrobel JS. Importance of time spent standing for those at risk of diabetic foot ulceration. Diabetes Care. 2010;33:2448-2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Najafi B, Grewal GS, Bharara M, Menzies R, Talal TK, Armstrong DG. Can’t stand the pressure: the association between unprotected standing, walking, and wound healing in people with diabetes. J Diabetes Sci Technol. 2016; doi: 10.1177/1932296816662959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lavery LA, Higgins KR, Lanctot DR, et al. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care. 2004;27:2642-2647. [DOI] [PubMed] [Google Scholar]
- 21. Lavery LA, Higgins KR, Lanctot DR, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care. 2007;30:14-20. [DOI] [PubMed] [Google Scholar]