Abstract
Mobile technology use is nearly ubiquitous which affords the opportunity for using these technologies for modifying health related behaviors. At the same time, use of mobile health (mHealth) technology raises privacy and security concerns of consumers. The goal of this analysis was to understand the perceived ease of use, usefulness, risk and trust that contribute to behavioral intention to use a mobile application for meeting the healthcare needs of persons living with HIV (PLWH). To understand these issues, we conducted focus group sessions with 50 persons living with HIV and 30 HIV healthcare providers. We used the e-commerce acceptance model to analyze our focus group data. Findings from the study demonstrated the need for mHealth to be perceived as useful, easy to use, with little perceived risk accompanied by a measure of trust in the creators of the technology. Findings from this work can inform future work on patients and providers’ perceptions of risk, trust, ease of use and usefulness of mHealth technology.
Keywords: mobile health, HIV, privacy, trust, security
Introduction
Mobile technology is nearly ubiquitous as increasing numbers of people carry a mobile device [1]. As such, mobile technology offers a unique opportunity for the diffusion of behavioral health interventions. Mobile health (mHealth) technology can guide decisions about health by providing round-the-clock real-time feedback [2] and opportunities for consumers to learn about and manage their disease.
These characteristics of timeliness and accessibility are particularly relevant to care for HIV which has shifted from a disease with a high mortality rate to one requiring lifetime chronic care and health monitoring. mHealth tools can help address many of the healthcare needs of persons living with HIV (PLWH) to promote retention in HIV care and adherence to medication regimens[3]. In the US, 1.2 million people are currently living with HIV [4], with worldwide estimates at 35 million [5]. A number of studies have shown promise for the use of mHealth for supporting HIV care [6–9].
Our study population included PLWH who were the targeted end users of a smartphone application (app) designed for monitoring and managing their health and for communicating with their care providers. PLWH is a relevant study population due to both their need for self-management support in chronic care as well as the persistent cultural stigma associated with HIV/AIDS [10].
Despite the promise of mHealth in monitoring health behaviors and improving the delivery of health care, little is known about users’ concerns over privacy and information sharing using mHealth technology. Privacy has been a topic of interest to researchers in psychology, sociology and more recently information technology (IT) [11–13]. Existing research on privacy emphasizes data security and confidentiality, largely focusing on electronic medical records. Yet consumers concerns around privacy related to mHealth technology use remain poorly understood. There are a number of issues related to privacy and information security in HIT that need to be carefully monitored and addressed in order to offer a technology most likely to engage consumers. The purpose of this study was to understand the perceived ease of use, usefulness, risk and trust that contribute to behavioral intention to use a mobile app for meeting the healthcare needs of PLWH.
Theoretical Framework
We used the e-commerce acceptance model (EAM) to understand technology acceptance of mHealth for PLWH [14]. The EAM has not been previously studied in the context of health or mobile technologies. It builds on the most widely employed model of IT adoption, the technology acceptance model (TAM) which we have previously studied in the context of the delivery of HIV care through an electronic record [15].
The dependent variable in this model is the same as in the TAM: behavioral intention to use the technology. The key constructs in the TAM are perceived usefulness and perceived ease of use [16]. In the case of health information technology (HIT), perceived usefulness is defined as the extent to which a person believes that using the HIT system will enhance his/her outcomes. Perceived ease of use is defined as the degree to which system use will be free from additional effort [17].
In the EAM, trust and perceived risk are two key drivers added to the TAM variables using the overall structure of the Theory of Reasoned Action (TRA) [18]. Integration of the four independent variables were tested and their relationships were validated. The model proposes that these four drivers lead to the primary constructs of “intention to transact” and “on-line transaction behavior” in the e-commerce sector, which in many ways may mimic consumer behavior in eHealth.
Trust is a behavioral belief that has been studied in e-commerce and has been shown to have a favorable effect on consumers’ intent to use a technology. Trust may be defined as the belief that the other party will behave responsibly and will not attempt to exploit the vulnerabilities of the user [14]. There are two kinds of trust: 1) party trust - trust in the benevolence and credibility of a particular party; and 2) control trust - trust in the integrity of the transaction medium. The importance of trust is heightened when there is a high degree of uncertainty which can happen in the case of HIT when users don’t understand where their information is being stored or how it is being transmitted.
For mHealth use, we would expect that consumer trust in the mHealth app is likely to influence behavioral intention to use the technology [19]. Trust is also related to perceived usefulness because users may not be certain that outcomes may be achieved unless there is confidence in the entities behind the HIT system. Trust is related to perceived ease of use because it reduces the efforts that would otherwise be necessary to monitor the proper functioning of the system. Trust is also related to perceived risk as a higher level of trust in an on-line entity reduces the perception of risk during the interaction.
Perceived risk is an important factor for eHealth use in light of the distance, in both time and space, between the consumer and the healthcare entity, as with most on-line transactions. It may be described as a degree of uncertainty related to use of the medium that is beyond the control of the information manager associated with the eHealth service. The consumer risks the possibility of suffering a loss while using the technology [20]. mHealth users perceive risk when the security of the infrastructure for securing their personal health information is not verified. Consumer perception of risk is negatively associated with intention to transact. Similarly, if an end-user perceives the risk of disclosure of their personal health information to be low then they are more likely to use a mHealth app.
To better understand the applicability of this model for mHealth technnology, we used focus group data which was collected as part of a larger study to to inform the development of a mobile app for HIV treatment and care for PLWH. The purpose of the larger study was to elicit from potential app users and their care providers the desired content and features of a mobile app for meeting and improving the health care needs of PLWH. The goal of this analysis was to understand the EAM constructs that contribute to behavioral intention to use a mobile app for PLWH.
Methods
Design
This study applied user-centered participatory design methods to inform the content of a mobile app for HIV treatment and care. The qualitative study was implemented using focus group methodology.
Sample
The sample comprised PLWH and clinicians and case managers who provide care to PLWH.
Procedures
The Columbia University Medical Center Institutional Review Board reviewed and approved this study protocol. Focus group sessions were moderated by a trained facilitator using a focus group guide. Each focus group session was also attended by at least one additional study team member who recorded notes and tended to logistics such as consent forms, food, and compensation to ensure that the groups ran smoothly. Following completion of the individual informed consent process and prior to the start of each focus group session, participants completed a demographic survey.
Each PLWH focus group session took place in a conference room at the Columbia University School of Nursing campus, lasted between 48–72 minutes and was conducted in English or Spanish. The HIV clinicians and case managers’ focus groups took place at a conference room at their workplace in the following locations: New York Presbyterian Hospital, the Brooklyn Hospital Path Center, and AIDS Service Center, a community-based organization. We gave $25 to our PLWH participants and $50 to the clinicians and case managers as a token of appreciation for their time. Food appropriate for the time of day was served during each focus group session. All focus group sessions were audio-recorded and transcribed for analysis.
We asked a series of questions during our focus groups sessions to identify the functional specifications of a mobile app for PLWH. At the end of our focus group sessions, we specifically asked focus group participants: “What are some of the privacy and confidentiality concerns that you anticipate encountering when using a mobile health app on your phone?”
Data collection continued until saturation was reached, which occurred when we heard similar patterns and themes across groups and no new information was being shared [21].
Data Analysis
Descriptive statistics of the demographic information were calculated using SPSS version 21. To support the credibility of the data, we used “member checks,” i.e., sharing of initial data interpretations with participants to ensure accurate interpretations. In addition, after each focus group, we conducted peer debriefing and triangulated findings across participants and facilitators. Research team members subsequently coded the transcripts using NVivo™ (QSR International, Victoria, Australia) software. We coded the data using the four constructs of the E-commerce acceptance model to deductively code focus groups to understand factors related to mHealth technology use. Coding of transcripts continued until consensus was reached.
Results
Sample
We conducted six focus group sessions with PLWH (n=50). Two of the focus groups were conducted in Spanish and one of the groups was comprised of only female participants. There were 37 male participants and 13 female. Participants’ ages ranged from 18–59. Participants self – identified as Black (N =26), White (N =7), Pacific Islander (N = 1), and American Indian (N =1) and the remainder of the participants did not report their race. Half of our participants (N =25) self-identified as being of Hispanic/Latino ethnicity.
In addition, we conducted three focus group sessions with HIV care providers which included clinicians and case managers. All focus groups were conducted in English. Participants’ ages ranged from 23–62 years and included 5 males, 24 females and 1 transgender female. Participants identified as Black (N =9), White (N =17), Pacific Islander (N = 1), and Asian (N =3). Six participants self-identified as being of Hispanic/Latino ethnicity.
Findings
We used the four constructs of the EAM to understand factors related to mHealth use in PLWH. Our focus group findings were organized according to the four broad constructs: trust, perceived risk, perceived usefulness, and perceived ease of use (Table 1).
Table 1.
EAM Constructs and Sample Quotes
| Construct | Sample Quotes |
|---|---|
| Trust |
|
| Perceived Risk |
|
| Perceived Usefulness |
|
| Perceived Ease of Use |
|
Trust
PLWH recognized the need for security safeguards and controls so that they could trust using an mHealth app. For example, one participant said, “provided the company that furnishes the app, has the right security so the information does not leak. Having that security, then there is no problem.” Another participant cited an example of a security system tied to the device which would make him feel comfortable using a mHealth app for PLWH. “The warranty from the company that makes it…the security the company has of itself, which in this case, well, benefits us, so that information does not leak.” Participants had concerns over who would have access to their information and didn’t trust certain entities to access their personal health information.
Perceived Risk
A number of participants expressed concerns over the risk of who would have access to their information, where it would be stored and if their HIV status had the potential to be disclosed. One participants said, “It’s like she said about technology, you don’t know where this information is going.” Another participant had the perception that anyone can access any information that is on the Internet. She said “Because right now anybody could get into the Internet and go into your information.”A younger participant in another focus group which was comprised of 21–24 year olds said, “As far as using an app I would probably never put information in, I wouldn’t personally because technology is out of order now. People can find out anything. You can do the fingerprint thing. Where is this information going to, who is seeing it, because it’s being documented? Where is it going?” Since smartphones have the functionality to detect your location, participants percievd a great risk to being tracked. For example one participant said “It’s like I don’t know…with the location settings with the iPhone and all that stuff.” Participants did acknowledge that a certain amount of risk may be acceptable or unavoidable. One focus group participant said, “We just have to get, how can I say it, a litttle secure about it. Because I didn’t like, where I worked at, I didn’t like them scanning all my information and putting it on the computer. Because the computer can be hacked in, in any given time, you understand? But I got comfortable with it. So, it’s a period you got to go through. You’ve got to adjust to certain things in life.”
Perceived Usefulness
PLWH thought that mHealth had the potential to be very useful for their care. For example one patient thought that it would provide updates on medications. “Like new medications. Every couple of months they come out with new HIV medication.” Another PLWH thought the mHealth would be a useful tool for creating reminders “I think some phones have a memo device where you could actually talk into it and say…” Participants also thought it would be useful for learning more about their disease or sharing information with others. For example, one PLWH said, “Since we already have our immune system compromised, we should know for example if we have something, know what it is, and the faster the better so we take care of our health.”
Providers, like patients, thought that mHealth can be very useful in the delivery of care to PLWH in a private manner. For example, one provider said, “Think about it, when they’re on the phone somebody else can hear their end of the conversation. If they’re texting, no one knows what’s going on.” Providers also thought that mobile technology was important for their patients to be able to self-manage their care. “Some of them use their phones for alarms. They have alarms set on their phones and they have calendar applications where they can write appointments.”
Perceived Ease of Use
Both PLWH and providers described a number or factors related to ease of use that would facilitate use if present and otherwise would present a barrier, such as reliable phones, simplicity, and operation autonomous from an internet connection. One PLWH said that “I would be willing to use the app if I have the phone with no problems.” Another participant echoed a similar sentiment and said that “because sometimes there are some apps that are a bit complicated and well people get frustrated immediately, and later they don’t use them. It has to be something simple.” Both PLWH and providers thought that an app should not rely on Internet connectivity. In specific one provider said “An app would be helpful if certain parts of the app didn’t need internet.”
There were also a number of patients and providers who described the need for a simple, easy to understand app. A provider commented on the need for information presentation to be understandable even to patients with “cognitive disability.” In specific, she said, “So even a graph that can be simple to us maybe not be something they’re easily able to read.” Another healthcare provider, in a different group echoed a similar idea and said, “It has to be simple enough that the person can really get hooked to it.”
Discussion
The increase in the use of mobile technology has the potential to improve the delivery of healthcare, but it has also raised new concerns over privacy and security of personal health information [22]. At the same time little attention has been paid to understanding technology acceptance in mHealth with a particular focus on privacy and security. Mobile devices and apps have created a new set of privacy concerns since protected health information can be stored on mobile devices, processed within these apps or shared via networks that are not secure [23]. While mHealth holds great promise, if patients are not willing to use the technology because it is not perceived as useful, easy to use or they have concerns over data security then it will not be able to improve health outcomes.
Concerns over mHealth acceptance and use becomes particularly relevant as patients and consumers begin to transfer their personal health information from their mobile devices to a central electronic health record. For example, Apple has started a partnership with Epic [24]. In addition, open platforms such as Apple’s Healthkit [25] and Google Fit allow patients to transfer their personal health information to a central electronic health record, yet these systems are still quite limited and are focused on fitness.
In this study, we sought to examine PLWH and their healthcare providers’ perceptions of the technology acceptance factors necessary for PLWH to use an HIV app to manage their health. Many study participants thought that a mobile app for PLWH would be extremely useful.
Participants also stressed the need for the app to be easy to use, consistent with past research in HIV care. In particular, participants suggested the app not rely on Internet connectivity. Both PLWH and providers described the cognitive deficits that are often experienced by PLWH and therefore the need for the app to be very simple and straightforward.
At the same time, there was an underlying concern over security of their information. Participants throughout our sessions wanted to understand who would have access to their personal health information. They emphasized the need to trust the “owner” of the app and if a particular company or institution was associated with the app then they would not be willing to use the app for accessing, entering or sharing their personal health information.
Perceived risk was an underlying theme throughout our nine focus group sessions. Participants were concerned over where their data was being stored and who would have access to their data. Their concerns included trust in the institutions that collect, store, or transmit their data as well as general apprehension about data transfer using the internet network and technological devices which are continually under development. In the US, there have been a number of policy initiatives at the federal level to protect patient health data being transferred electronically. Of note, the Markle Common Framework has a set of published principles that provide the foundation for managing personal health information within consumer accessible data streams[26]. The Markle Connecting for Health Framework has guided the US government implementation of IT including the Health Information Technology for Economic and Clinical Health (HITECH) Act [27].
Even with this guiding set of principles that is quite extensive and comprehensive, consumers remain concerned that their personal health information is not secure and they have particular concerns regarding the risks associated with mobile technology in sharing and accessing their personal health information.
We did not specifically ask study participants about their intention to use this technology. Instead, we examined study participants’ perceived ease of use, usefulness, trust and privacy. The lessons learned from our examination of each of these constructs are important for the development of this technology especially in a highly stigmatized population [28]. As a result, the intersection between the findings from each of our study constructs is likely to predict a PLWH’s behavioral intention to use a mobile app for managing his/ her health.
Limitations
We conducted this study in New York City, which limits the generalizability of the findings to one geographic area. Even so, New York City has the greatest number of PLWH in the Unites States making this an appropriate setting for conducting this work [29]. In addition there may have been a response bias from our study participants since our methods relied on self-report.
Conclusion
Findings from this work can inform future work on patients and providers’ perceptions of risk, trust, ease of use and usefulness of mHealth technology. Findings from this work have broader applicability to others living with chronic diseases as well as any individuals who seek to use mobile technologies for accessing, storing and sharing their personal health information. Future development of mHealth technology needs to integrate ease of use, usefulness, trust and perceived risk to facilitate the use of mHealth technology for consumers.
Figure 1.
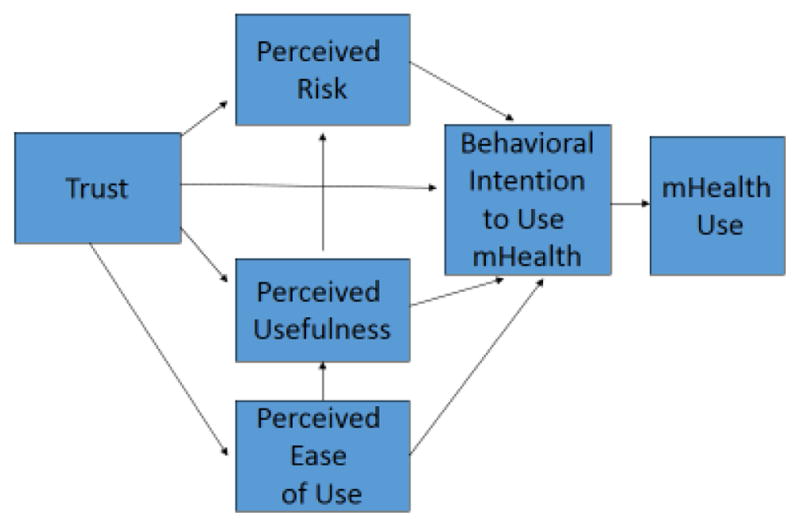
E-Commerce Acceptance Model applied to mHealth Technology Use
Acknowledgments
This publication was supported by a cooperative agreement between Columbia University School of Nursing and the Centers for Disease Control and Prevention (CDC; 1U01PS00371501; PI: R Schnall). The findings and conclusions in this report do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Estrin D, Sim I. Health care delivery. Open mHealth architecture: an engine for health care innovation. Science. 2010;330(6005):759–60. doi: 10.1126/science.1196187. [DOI] [PubMed] [Google Scholar]
- 2.Kumar S, Nilsen W, Pavel M, Srivastava M. Mobile Health: Revolutionizing Healthcare Through Transdisciplinary Research. Computer. 2013;46(1):28–35. [Google Scholar]
- 3.Schnall R, Bakken S, Rojas M, Travers J, Carballo-Dieguez A. mHealth Technology as a Persuasive Tool for Treatment, Care and Management of Persons Living with HIV. AIDS Behav. 2015:1–9. doi: 10.1007/s10461-014-0984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV in the United States: At a Glance. 2014 [cited 2014 November 30]. Available from: http://www.cdc.gov/hiv/statistics/basics/ataglance.html.
- 5.World Health Organization (WHO) World AIDS Day 2014 - Closing the gap in HIV prevention and treatment services. 2014 [cited 2014 November 30]. Available from: http://www.who.int/hiv/en/
- 6.Catalani C, Philbrick W, Hamish F, Mechael P, Israelski D. mHealth for HIV Treatment & Prevention: A Systematic Review of the Literature. The Open AIDS Journal. 2013;7:17–41. doi: 10.2174/1874613620130812003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. The Cochrane database of systematic reviews. 2012;3:CD009756. doi: 10.1002/14651858.CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLoS Med. 2013;10(1):e1001362. doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pellowski J, Kalichman S. Recent Advances (2011–2012) in Technology-Delivered Interventions for People Living with HIV. Curr HIV/AIDS Rep. 2012;9(4):326–34. doi: 10.1007/s11904-012-0133-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. Aids. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Culnan MJ, Armstrong PK. Information Privacy Concerns, Procedural Fairness, and Impersonal Trust: An Empirical Investigation. Organization Science. 1999;10(1):104–15. [Google Scholar]
- 12.Stewart KA, Segars AH. An Empirical Examination of the Concern for Information Privacy Instrument. Info Sys Research. 2002;13(1):36–49. [Google Scholar]
- 13.Dinev T, Hart P. Internet privacy concerns and their antecedents - measurement validity and a regression model. Behaviour & Information Technology. 2004;23(6):413–22. [Google Scholar]
- 14.Pavlou PA. Consumer Acceptance of Electronic Commerce: Integrating Trust and Risk with the Technology Acceptance Model. International Journal of Electronic Commerce. 2003;7(3):101–34. [Google Scholar]
- 15.Schnall R, Bakken S. Testing the Technology Acceptance Model: HIV case managers’ intention to use a continuity of care record with context-specific links. Informatics for health & social care. 2011;36(3):161–72. doi: 10.3109/17538157.2011.584998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis FD. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quarterly. 1989;13(3):319–40. [Google Scholar]
- 17.Adams DA, Nelson RR, Todd PA. Perceived Usefulness, Ease of Use, and Usage of Information Technology: A Replication. MIS Quarterly. 1992;16(2):227–47. [Google Scholar]
- 18.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 19.Jarvenpaa SL, Tractinsky N, Saarinen L. Consumer Trust in an Internet Store: A Cross-Cultural Validation. Journal of Computer-Mediated Communication. 1999;5(2):0. [Google Scholar]
- 20.Bauer RA. In: Consumer behavior as risk taking. Cox DF, editor. Cambridge: Harvard University Press; 1960. [Google Scholar]
- 21.Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 22.Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, et al. Mobile Health Technology Evaluation: The mHealth Evidence Workshop. American Journal of Preventive Medicine. 2013;45(2):228–36. doi: 10.1016/j.amepre.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luxton DD, Kayl RA, Mishkind MC. mHealth data security: the need for HIPAA-compliant standardization. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2012;18(4):284–8. doi: 10.1089/tmj.2011.0180. [DOI] [PubMed] [Google Scholar]
- 24.Carr D. Apple Partners With Epic, Mayo Clinic For HealthKit. 2014 Available from: http://www.informationweek.com/healthcare/mobile-and-wireless/apple-partners-with-epic-mayo-clinic-for-healthkit/d/d-id/1269371.
- 25.Dolan B. Why Apple’s HealthKit launch is important for digital health. 2014 [cited 2014 September 6]. Available from: http://mobihealthnews.com/33765/why-apples-healthkit-launch-is-important-for-digital-health/
- 26.Connecting Consumers: Overview and Principles. New York: Markle Foundation; 2011. [cited 2014 December 6]. Available from: http://www.markle.org/health/markle-common-framework/connecting-consumers/overview. [Google Scholar]
- 27.Blumenthal D. Launching HITECH. New England Journal of Medicine. 2010;362(5):382–5. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- 28.Shacham E, Rosenburg N, Önen NF, Donovan MF, Turner Overton E. Persistent HIV-related stigma among an outpatient US clinic population. International Journal of STD & AIDS. 2015;26(4):243–50. doi: 10.1177/0956462414533318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.HIV Epidemiology and Field Services Program. HIV Surveillance Annual Report. New York, NY: 2013. [Google Scholar]


