Abstract
Nonsteroidal anti-inflammatory drugs work through inhibition of cyclooxygenase (COX) and are highly effective for the treatment of pain and inflammation in horses. There are two clinically relevant isoforms of COX. Cyclooxygenase-1 is constitutively expressed and is considered important for a variety of physiologic functions, including gastrointestinal homeostasis. Thus, NSAIDs that selectively inhibit COX-2 while sparing COX-1 may be associated with a lower incidence of adverse gastrointestinal effects. Various formulations of firocoxib, a COX-2–selective NSAID, labeled for use in horses are available in the United States. Equine practitioners should know that the FDA limits the use of firocoxib to formulations labeled for horses, regardless of price concerns. In addition, practitioners will benefit from understanding the nuances of firocoxib administration, including the importance of correct dosing and the contraindications of combining NSAIDs. Together with knowledge of the potential advantages of COX-2 selectivity, these considerations will help veterinarians select and treat patients that could benefit from this new class of NSAID.
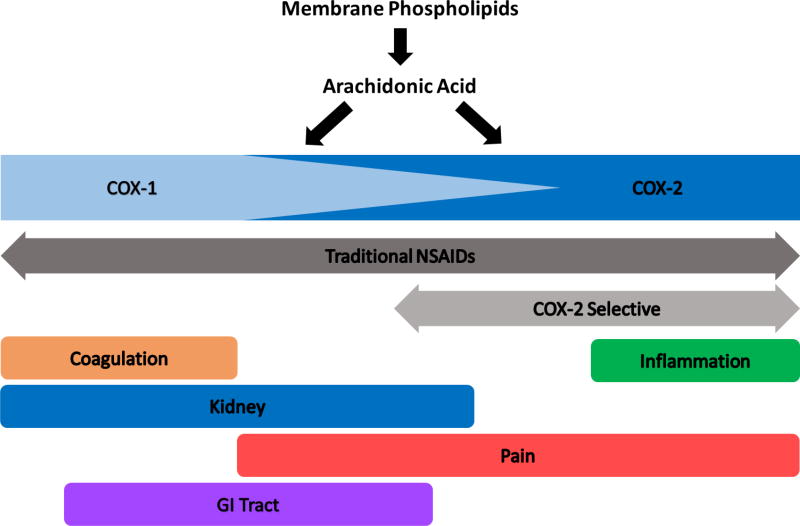
Nonsteroidal anti-inflammatory drugs are highly effective for the treatment of a variety of common diseases in horses, including degenerative joint disease and colic.1,2 The anti-inflammatory properties of NSAIDs are a result of COX inhibition.3 However, studies4 have demonstrated that there are multiple COX isoforms, each with its own physiological expression and function (Figure 1). As a result, COX-2–selective drugs have been developed that allow more targeted inhibition of COX-2, the inducible COX isoform associated with inflammation.
Figure 1.
Diagrammatic representation of the overlapping functions of prostanoids elaborated by COX-1 and COX-2.
Cyclooxygenase-2–selective NSAIDs entered the marketplace as human drugs intended for treatment of pain and inflammation associated with osteoarthritis. The principal advantage of COX-2–selective NSAIDs was a reduction in adverse gastrointestinal effects, compared with effects of nonselective NSAIDs, presumably because of enhanced sparing of COX-1 activity.5,6 Although these drugs showed promise for improved treatment of degenerative joint disease in people, 2 COX-2–selective NSAIDs were found to have unexpected adverse cardiovascular and thromboembolic effects that theoretically arose from inhibition of COX-2 (reducing the concentration of vasodilatory prostaglandin E2) and a lack of inhibition of COX-1 (permitting continued production of thrombogenic thromboxane A2).7,8 Eventually, these drugs were voluntarily withdrawn from the market.
Horses have similar susceptibility to the adverse gastrointestinal effects of nonselective NSAIDs but are not known to be predisposed to the types of adverse cardiovascular effects seen with the use of COX-2–selective NSAIDs in humans, suggesting that use of these drugs may be safe in this species. A COX-2–selective NSAID, firocoxib,a is now available and labeled for use in horses. However, the clinical benefits of firocoxib in horses remain incompletely understood, and recent legal concerns with extralabel use of a small animal formulation of firocoxibb in horses have come to light.9
Physiology of COX-1 and COX-2
When considering the use of COX-2–selective NSAIDs in treating pain and inflammation in horses, it is important to understand the differences in the physiology and pathophysiology of the various COX isoforms. Although there are at least three known isoforms of COX, COX-1 and COX-2, which have been shown to be present in equine tissues, are the most relevant in regard to clinical use of NSAIDs in horses.10–13 Cyclooxygenase-1 is constitutively expressed in virtually all tissues and is considered important for a variety of physiologic functions, including gastrointestinal homeostasis, coagulation, and renal homeostasis. In contrast, COX-2 is normally expressed at very low levels in most tissues under physiological conditions, but is upregulated during pro-inflammatory states.4 Accordingly, the principle that COX-1 is a beneficial isoform and COX-2 is associated with pain and inflammation has driven the development of COX-2–selective NSAIDS to reduce unwanted adverse effects.14 Both COX-1 and COX-2 produce prostaglandin H2, an intermediary that is locally metabolized to active prostanoids, such as thromboxanes and prostaglandins, by tissue synthases. Low-level continuous activity of COX-1 in organs such as the gastrointestinal tract and the kidneys produces sufficient prostaglandin H2 to support physiologic functions driven by prostaglandins. Upregulation of COX-2 in inflammatory states leads to increased production of prostaglandin H2 and pathophysiological amounts of prostaglandins, contributing to pain, inflammation, and clinical signs of endotoxemia.15,16 It is important, however, to understand that the specific function of the various COX isoforms is not necessarily the same in all tissues. For example, in the kidney, COX-2 is also constitutively expressed and serves important functions in renal homeostasis. Therefore, it is possible that a COX-2–selective NSAID can still have adverse renal effects.17 This highlights the need for careful patient selection when prescribing NSAIDs, including obtaining a full medical history and performing clinicopathologic testing in select patients.
NSAIDs and COX Selectivity
Cyclooxygenase-2–selective NSAIDs may be more suitably named COX-1–sparing. This is because although an NSAID may have high selectivity for COX-2, it will still inhibit COX-1 to some degree. The selectivity of an NSAID for COX-2 may be determined through assays of thromboxane A2 activity during whole blood clotting (as an indicator of COX-1 function) and of lipopolysaccharide-induced prostaglandin E2 activity in blood (as an indicator of COX-2 function).18 A ratio of the NSAID concentrations required to inhibit 50% of thromboxane A2 activity versus 50% of prostaglandin E2 activity is then used to calculate the COX-1:COX-2 selectivity ratio.19,20 Phenylbutazone and flunixin meglumine have ratios near 1, indicating that COX-1 and COX-2 are inhibited to similar degrees by these drugs, which are considered non-selective NSAIDs.20 In contrast, meloxicam and firocoxib have COX-2:COX-1 selectivity ratios of approximately 3 to 4 and approximately 200, respectively, in horses. This indicates that these NSAIDs predominantly inhibit COX-2, but will to some degree inhibit COX-1, particularly meloxicam with its lower selectivity. For this reason, terminology such as COX-2 preferential may be used to describe meloxicam rather than COX-2 selective. In recent years, many new COX-2–selective NSAIDs called coxibs with a high degree of COX-2 selectivity have entered the veterinary market, including deracoxib, mavacoxib, robenacoxib, and cimicoxib.21–25 However, only firocoxib is commercially available and labeled for use in horses in the United States. Meloxicam is of interest as a COX-2–preferential NSAID and is available in many countries outside the United States for use in horses.
The Use of COX-2–selective NSAIDs in Horses
Firocoxib is available in the United States in formulations labeled for use in horsesa and dogs.b The substantial difference in cost of the equine and canine formulations has led to frequent extralabel use of canine-labeled firocoxib tablets in horses to reduce treatment costs. However, according to the Animal Medicinal Drug Use Clarification Act of 1994,9 when various species-specific formulations of a drug are available, it is not permissible to use the formulation labeled for one species in a different species. In addition, the recent introduction of an FDA-approved 57-mg firocoxib tablet labeled for use in horses, which is the same formulation as the canine-labeled firocoxib tablet, has eliminated the need for use of canine-labeled firocoxib tablets in horses. A preliminary study has shown that the equine-labeled tablet and paste formulations have the same bioavailability in horses.26 A 57-mg tablet provides a dose of 0.114 mg/kg (0.052 mg/lb) in a 500-kg (1,100-lb) adult horse. Although it would be less expensive to administer a quarter of a 227-mg canine-labeled firocoxib tablet, this would be a violation of the Animal Medicinal Drug Use Clarification Act.9 Furthermore, it is difficult to accurately divide the 227-mg tablets in quarters, because these tablets are only scored in half. Thus, doing so may lead to inadvertent over- or underdosage.
Another important consideration when using firocoxib in horses is that COX selectivity is only achieved when the drug is administered at the correct dosage. If a COX-2–selective drug is overdosed, the selectivity diminishes and the same adverse effects seen with nonselective NSAIDs may occur. For instance, in dogs, administration of deracoxib, a COX-2–selective NSAID, at a higher than recommended dosage has, in some instances, been associated with gastric perforation.27
When firocoxib initially became available for use in horses in the United States, the United States Equestrian Federation permitted the administration of firocoxib in combination with other NSAIDs. However, this has since been changed, and firocoxib can no longer be given with any other NSAIDs.28 Given our current understanding of COX selectivity, it appears likely that co-administration of firocoxib with a nonselective NSAID would eliminate the intended benefits of COX-2–selective NSAIDs and, therefore, is not advisable. Additionally, administering combinations of NSAIDs increases the likelihood of complications. A prospective, non-blinded study17 involving co-administration of firocoxib (0.1 mg/kg [0.045 mg/lb], PO, q 24 h) and phenylbutazone (2.2 mg/kg [1 mg/lb], PO, q 24 h) to horses for 10 days showed significant increases in serum creatinine concentration, suggesting the possibility of adverse renal effects in these animals.
In the United States, firocoxib has been approved by the FDA for the treatment of degenerative joint disease in horses, and studies have proven its effectiveness in controlling pain and inflammation associated with osteoarthritis. For instance, a randomized, controlled, unblinded, multi-institutional clinical study29 funded by Merial found that 80% of horses with osteoarthritis treated with firocoxib at a dosage of 0.1 mg/kg, PO, every 24 hours had an improvement in lameness severity.
Some veterinarians have, on the basis of their clinical experience, expressed concerns that firocoxib may be inferior to phenylbutazone for controlling pain associated with degenerative joint disease. However, in a multicenter, unblinded, non-inferiority clinical trial30 funded by Merial that compared firocoxib (0.1 mg/kg, PO, q 24 h) and phenylbutazone (4.4 mg/kg [2 mg/lb], PO, q 24 h), there was no significant difference in the degree of lameness reduction after 7 or 14 days of treatment in horses with chronic (ie, > 4 weeks’ duration), moderate to severe (ie, a score ≥ 3 on a scale from 0 to 5 or ≥ 2 on a scale from 0 to 3) lameness.
The effectiveness of firocoxib for the treatment of gastrointestinal pain has also been investigated. In an experimental study12 involving horses recovering from surgically induced small intestinal strangulating obstruction, firocoxib (0.1 mg/kg, IV, q 24 h) was found to control pain as effectively as flunixin meglumine (1.1 mg/kg [0.5 mg/lb], IV, q 12 h).
Clinical Benefits of COX-2–selective NSAIDs
Although it is valuable to know that firocoxib is as effective as traditional nonselective NSAIDs at controlling lameness and postoperative gastrointestinal pain in horses, it is important to acknowledge that the primary advantage of treating patients with COX-2–selective NSAIDs is their COX-1–sparing activity, which should, in theory, reduce the likelihood of adverse effects, particularly adverse gastrointestinal effects. Further investigation is required to determine whether there is a decreased incidence of adverse gastrointestinal effects in horses treated with COX-2–selective NSAIDs. However, there have been informative studies11,12 assessing the efficacy of COX-2–selective NSAIDs in controlling visceral pain and endotoxemia as well as their effects on the intestinal barrier in horses with experimentally induced small intestinal strangulating obstruction. For example, a study13 of intestinal barrier recovery in horses with experimentally induced ischemic injury of the jejunum found that ex vivo application of flunixin meglumine inhibited intestinal barrier recovery, but that ex vivo application of etodolac, an NSAID shown to be COX-2 selective in horses,31 permitted recovery. In the previously referenced study12 comparing firocoxib and flunixin, healing jejunum from horses treated with flunixin had a significantly higher permeability to lipopolysaccharide, compared with healing jejunum from horses treated with firocoxib, supporting the assertion that sparing COX-1 may reduce the incidence of intestinal complications in horses with colic. A study11 examining the effects of meloxicam in horses with experimentally induced small intestinal strangulating obstruction had similar results. On the other hand, a non-blinded, randomized clinical trial32 of client-owned horses with small intestinal strangulating obstruction did not identify any significant differences between the effects of flunixin meglumine (1.1 mg/kg, IV, q 12 h) and meloxicam (0.6 mg/kg [0.27 mg/lb], IV, q 12 h) on intestinal permeability. However, it is important to consider the implications of the lack of blinding in this study as well as the fact that meloxicam was given at twice the usual dosage, which may have reduced its COX-2 selectivity.
Conclusions
The introduction of equine-labeled formulations of firocoxib to the US market provides an opportunity for equine veterinarians to use a COX-2–selective NSAID in the treatment of their patients. However, equine practitioners should know that the FDA limits the usage of firocoxib to formulations labeled for use in horses, regardless of price concerns. Practitioners will benefit from understanding the nuances of firocoxib administration, including the importance of correct dosing to achieve therapeutic concentrations while preserving COX selectivity and the contraindications of combining NSAIDs. Together with knowledge of the potential advantages of COX-2 selectivity, these considerations will help veterinarians select and treat patients that could benefit from this new class of NSAID.
Abbreviations
- COX
Cyclooxygenase
Footnotes
The authors disclose no conflicts of interest, financial or otherwise.
Equioxx, Merial Limited, Duluth, Ga.
Previcox , Merial Limited, Duluth, Ga.
References
- 1.Goodrich LR, Nixon AJ. Medical treatment of osteoarthritis in the horse—a review. Vet J. 2006;171:51–69. doi: 10.1016/j.tvjl.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Clark JO, Clark TP. Analgesia. Vet Clin North Am Equine Pract. 1999;15:705–723. doi: 10.1016/s0749-0739(17)30140-2. [DOI] [PubMed] [Google Scholar]
- 3.Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231:232–235. doi: 10.1038/newbio231232a0. [DOI] [PubMed] [Google Scholar]
- 4.Vane JR, Botting RM. A better understanding of anti-inflammatory drugs based on isoforms of cyclooxygenase (COX-1 and COX-2) Adv Prostaglandin Thromboxane Leukot Res. 1995;23:41–48. [PubMed] [Google Scholar]
- 5.Simon LS, Weaver AL, Graham DY, et al. Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA. 1999;282:1921–1928. doi: 10.1001/jama.282.20.1921. [DOI] [PubMed] [Google Scholar]
- 6.Bombardier C, Laine L, Reicin A, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343:1520–1528. doi: 10.1056/NEJM200011233432103. (Expression of concern. N Engl J Med 2005;353:2813–2814. Expression of concern reaffirmed. N Engl J Med 2006;354:1193.) [DOI] [PubMed] [Google Scholar]
- 7.Sibbald B. Rofecoxib (Vioxx) voluntarily withdrawn from market. CMAJ. 2004;171:1027–1028. doi: 10.1503/cmaj.1041606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atukorala I, Hunter DJ. Valdecoxib: the rise and fall of a COX-2 inhibitor. Expert Opin Pharmacother. 2013;14:1077–1086. doi: 10.1517/14656566.2013.783568. [DOI] [PubMed] [Google Scholar]
- 9.AVMA. [Accessed Jan 10, 2017];Clarification regarding substitution of Previcox for Equioxx. Available at: https://www.avma.org/KB/Resources/Reference/Pages/Previcox-for-Equioxx.aspx.
- 10.Tomlinson JE, Wilder BO, Young KM, et al. Effects of flunixin meglumine or etodolac treatment on mucosal recovery of equine jejunum after ischemia. Am J Vet Res. 2004;65:761–769. doi: 10.2460/ajvr.2004.65.761. [DOI] [PubMed] [Google Scholar]
- 11.Little D, Brown SA, Campbell NB, et al. Effects of the cyclooxygenase inhibitor meloxicam on recovery of ischemia-injured equine jejunum. Am J Vet Res. 2007;68:614–624. doi: 10.2460/ajvr.68.6.614. [DOI] [PubMed] [Google Scholar]
- 12.Cook VL, Meyer CT, Campbell NB, et al. Effect of firocoxib or flunixin meglumine on recovery of ischemic-injured equine jejunum. Am J Vet Res. 2009;70:992–1000. doi: 10.2460/ajvr.70.8.992. [DOI] [PubMed] [Google Scholar]
- 13.Campbell NB, Blikslager AT. The role of cyclooxygenase inhibitors in repair of ischaemic-injured jejunal mucosa in the horse. Equine Vet J Suppl. 2000;32:59–64. doi: 10.1111/j.2042-3306.2000.tb05335.x. [DOI] [PubMed] [Google Scholar]
- 14.Blikslager AT. Do we need cyclooxygenase-2 inhibitors in equine practice? Compend Contin Educ Pract Vet. 1999;21:548–550. [Google Scholar]
- 15.Warner TD, Mitchell JA. Cyclooxygenase-3 (COX-3): filling in the gaps toward a COX continuum? Proc Natl Acad Sci U S A. 2002;99:13371–13373. doi: 10.1073/pnas.222543099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cook VL, Blikslager AT. The use of nonsteroidal anti-inflammatory drugs in critically ill horses. J Vet Emerg Crit Care (San Antonio) 2015;25:76–88. doi: 10.1111/vec.12271. [DOI] [PubMed] [Google Scholar]
- 17.Kivett L, Taintor J, Wright J. Evaluation of the safety of a combination of oral administration of phenylbutazone and firocoxib in horses. J Vet Pharmacol Ther. 2013;37:413–416. doi: 10.1111/jvp.12097. [DOI] [PubMed] [Google Scholar]
- 18.Duz M, Parkin TD, Cullander RM, et al. Effect of flunixin meglumine and firocoxib on ex vivo cyclooxygenase activity in horses undergoing elective surgery. Am J Vet Res. 2015;76:208–215. doi: 10.2460/ajvr.76.3.208. [DOI] [PubMed] [Google Scholar]
- 19.Brideau C, Van Staden C, Chan CC. In vitro effects of cyclooxygenase inhibitors in whole blood of horses, dogs, and cats. Am J Vet Res. 2001;62:1755–1760. doi: 10.2460/ajvr.2001.62.1755. [DOI] [PubMed] [Google Scholar]
- 20.Beretta C, Garavaglia G, Cavalli M. COX-1 and COX-2 inhibition in horse blood by phenylbutazone, flunixin, carprofen and meloxicam: an in vitro analysis. Pharmacol Res. 2005;52:302–306. doi: 10.1016/j.phrs.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Kim TW, Della Rocca G, Di Salvo A, et al. Evaluation of pharmacokinetic and pharmacodynamic properties of cimicoxib in fasted and fed horses. N Z Vet J. 2015;63:92–97. doi: 10.1080/00480169.2014.950355. [DOI] [PubMed] [Google Scholar]
- 22.Kim TW, Lebkowska-Wieruszewska B, Owen H, et al. Pharmacokinetic profiles of the novel COX-2 selective inhibitor cimicoxib in dogs. Vet J. 2014;200:77–81. doi: 10.1016/j.tvjl.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 23.Bienhoff SE, Smith ES, Roycroft LM, et al. Efficacy and safety of deracoxib for control of postoperative pain and inflammation associated with soft tissue surgery in dogs. Vet Surg. 2012;41:336–344. doi: 10.1111/j.1532-950X.2011.00942.x. [DOI] [PubMed] [Google Scholar]
- 24.Reymond N, Speranza C, Gruet P, et al. Robenacoxib vs carprofen for the treatment of canine osteoarthritis; a randomized, noninferiority clinical trial. J Vet Pharmacol Ther. 2012;35:175–183. doi: 10.1111/j.1365-2885.2011.01297.x. [DOI] [PubMed] [Google Scholar]
- 25.Payne-Johnson M, Becskei C, Chaudhry Y, et al. Comparative efficacy and safety of mavacoxib and carprofen in the treatment of canine osteoarthritis. Vet Rec. 2015;176:284. doi: 10.1136/vr.102397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freedom of information summary. [Accessed Jan 18, 2017];Original new animal drug application. NADA 141-458. Equioxx, firocoxib tablets, horses. Available at: http://www.fda.gov/downloads/AnimalVeterinary/Products/ApprovedAnimalDrugProducts/FOIADrugSummaries/UCM514663.pdf.
- 27.Lascelles BD, Blikslager AT, Fox SM, et al. Gastrointestinal tract perforation in dogs treated with a selective cyclooxygenase-2 inhibitor: 29 cases (2002–2003) J Am Vet Med Assoc. 2005;227:1112–1117. doi: 10.2460/javma.2005.227.1112. [DOI] [PubMed] [Google Scholar]
- 28.United States Equestrian Federation. 2016 guidelines for drugs and medications. Columbus, Ohio: United States Equestrian Federation; 2016. [Google Scholar]
- 29.Orsini JA, Ryan WG, Carithers DS, et al. Evaluation of oral administration of firocoxib for the management of musculoskeletal pain and lameness associated with osteoarthritis in horses. Am J Vet Res. 2012;73:664–671. doi: 10.2460/ajvr.73.5.664. [DOI] [PubMed] [Google Scholar]
- 30.Doucet MY, Bertone AL, Hendrickson D, et al. Comparison of efficacy and safety of paste formulations of firocoxib and phenylbutazone in horses with naturally occurring osteoarthritis. J Am Vet Med Assoc. 2008;232:91–97. doi: 10.2460/javma.232.1.91. [DOI] [PubMed] [Google Scholar]
- 31.Davis JL, Papich MG, Morton AJ, et al. Pharmacokinetics of etodolac in the horse following oral and intravenous administration. J Vet Pharmacol Ther. 2007;30:43–48. doi: 10.1111/j.1365-2885.2007.00811.x. [DOI] [PubMed] [Google Scholar]
- 32.Naylor RJ, Taylor AH, Knowles E, et al. Comparison of flunixin meglumine and meloxicam for postoperative management of horses with strangulating small intestinal lesions. Equine Vet J. 2013;46:427–434. doi: 10.1111/evj.12224. [DOI] [PubMed] [Google Scholar]