Abstract
Background and Objectives
The authors sought to study patient-reported outcomes following nipple-sparing mastectomy (NSM).
Methods
From 2008 to 2011, the BREAST-Q was administered to women undergoing NSM surgery for cancer treatment or risk-reduction prior to surgery and at two years after completion of reconstruction. The change in score over time and the impact of surgical indication, complication occurrence and laterality on scores were analyzed.
Results
The BREAST-Q was prospectively administered to 39 women undergoing NSM for cancer treatment (n=17) or risk-reduction (RR) (n =22). At two years after operation, median overall satisfaction with breasts was 75 (IQR=67,100). There were significant postoperative increases in scores for overall satisfaction with breasts (+8, p=0.021) and psychosocial well-being (+14, p=0.003). Postoperatively, RR patients had significantly higher scores for psychosocial wellness, physical impact (chest), and overall satisfaction with outcome compared to cancer treatment patients (p<0.05). Also, increase from preoperative to postoperative psychosocial wellness was higher in the RR compared to cancer treatment patients (+17 vs. +1, p=.043). Complication occurrence did not significantly impact postoperative scores.
Conclusions
Following NSM for cancer treatment or RR, patients demonstrated high levels of satisfaction and quality of life as measured by BREAST-Q. Satisfaction level increased two years following operation.
Keywords: Nipple-Sparing Mastectomy, Mastectomy, BREAST-Q, outcomes, satisfaction
Introduction
The surgical treatment of breast cancer has evolved over the past century in an attempt to improve cosmetic outcomes and reduce surgical morbidity while still providing an oncologically sound surgical procedure. From the original Halsted radical mastectomy came the modified radical mastectomy (MRM), total mastectomy (TM), skin-sparing mastectomy (SSM) and now nipple-sparing (NSM) or total skin-sparing mastectomy (TSSM). The current surgical technique of NSM evolved from the well-described technique of skin-sparing mastectomy, creating thinner skin flaps and a 2-3 mm nipple-areolar flap.[1,2] Multiple previous studies with long-term outcomes have shown similar recurrence and survival outcomes for NSM patients compared to SSM patients in the cancer setting.[3] Likewise, NSM for risk reduction (RR) has also shown favorable outcomes; indeed, a previous study from our group of NSM in BRCA carriers with cancer showed no nipple recurrences.[4]
However, literature on the psychosocial benefits of nipple sparing mastectomy is varied. Although most studies have shown that preservation of the nipple improves physical and mental quality of life,[5-10] few studies have preoperative data on psychosocial aspects of body image, sexuality, and quality of life for those undergoing NSM. Therefore, it is difficult to know to what degree nipple sparing mastectomy has improved psychosocial aspects from baseline.
There has been an increased emphasis on patient reported outcomes (PRO) particularly with respect to breast surgery.[7] The BREAST-Q is a validated PRO measure used to study patient satisfaction as well as various aspects of health-related quality of life (QOL) for patients undergoing breast reconstruction. The BREAST-Q was initially developed and validated in 2009. [11-15] This PRO measure provides a scientifically rigorous and clinically valid tool, providing independent scoring and discrimination in both short and long-term outcomes.
In this study we utilized the BREAST-Q to measure QOL and satisfaction with NSM in both the cancer and RR setting. We obtained BREAST-Q data prior to and after surgery to directly measure the impact of NSM on surgical outcomes. We hypothesized that NSM would result in changes in QOL and high levels of patient satisfaction that would persist over time.
Materials and Methods
Study Design
Patient Selection
This study was approved by our institutional review board. Between 2008 and 2010, sixty-five (65) women undergoing NSM were enrolled in a prospective study and were given the BREAST-Q survey prior to surgery and at one and two years following completion of reconstruction. Despite multiple contacts, thirteen (13) patients were lost to follow-up, and thirteen (13) did not complete the final study survey and were excluded. The remaining thirty-nine (39) participants completed the two-year follow-up survey.
Inclusion criteria (Table 1) for the study included NSM for both cancer (n=17) and risk reduction (n=22). All patients underwent reconstruction. We collected data on patient demographics, medical history, family history, tumor characteristics, surgical complications, reconstruction technique, oncologic and aesthetic outcome, and ultimate nipple outcome. Breast measurements, including cup size, nipple diameter and photographic documentation of outcome were collected.
Table I. Nipple-Sparing Mastectomy Inclusion/Exclusion Criteria.
| Inclusion criteria for nipple-sparing mastectomy study: |
| 1. Unilateral or bilateral prophylactic mastectomy |
| 2. Ipsilateral breast cancer patients not meeting exclusion criteria detailed below |
| 3. Appropriate reconstructive surgery candidate |
| 4. Patient undergoing immediate breast reconstruction |
| Absolute exclusion criteria for nipple sparing mastectomy study: |
| 1. Direct nipple involvement with tumor on permanent pathologic exam of a biopsy taken from the remaining major duct on retroareolar complex |
| 2. Large tumor size (T3 or greater) |
| 3. Patient not undergoing immediate reconstruction |
| Relative exclusion criteria for study participation: |
| 1. Extensive DCIS or microcalcifications (as determined by mammogram, US or MRI) |
| 2. Poor reconstructive candidate (as determined by plastic surgeon) |
| 3. Tumors with characteristics not meeting the above inclusion criteria |
BREAST-Q Survey
The BREAST-Q is a validated PRO measure developed at Memorial Sloan Kettering Cancer Center and University of British Columbia.[13,15] The BREAST-Q consists of independent scales measuring various aspect of outcome for the patient perspective. The scales were developed using Rasch psychometric methods and are scored using Q-score software. Results may range from 0-100 with higher scores reflecting high satisfaction or better QOL. The BREAST-Q survey was administered prior to mastectomy after consultation with both the surgical oncologist and the plastic surgeon, and at 12 and 24 months following final completion of the reconstruction. At these time points, surveys were given directly to patients during an office visit or mailed to the patient's home. The investigators contacted non-responders through written and telephone communication. All aspects of the BREAST-Q reconstructive module were administered with exception of questions regarding abdominal donor site.
Surgical Technique: Nipple Sparing Mastectomy
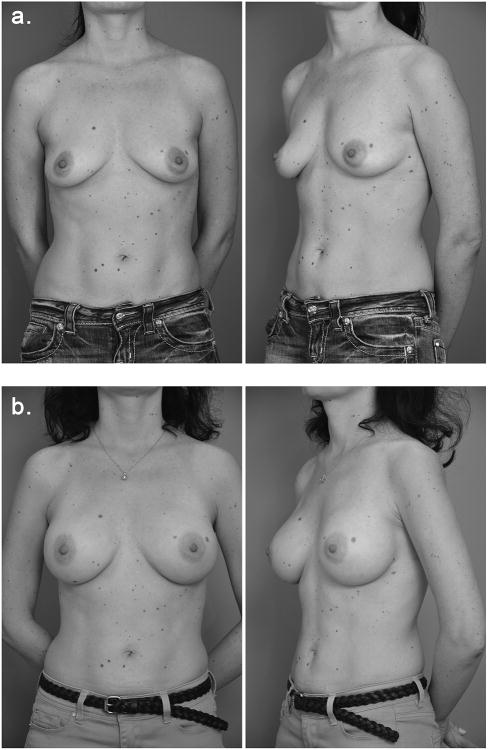
Our surgical technique for NSM (Figure 1 –patient photo) and immediate 1- and 2-stage implant or autologous reconstruction has been described previously.[4,16] A radial or inferior-lateral mammary crease incision was most commonly used following consideration of breast size and surgeon/patient preferences. To maximize the vascularity of the mastectomy flap and nipple, care was taken to preserve the NAC subdermal plexus by sharp dissection and to preserve the internal mammary artery perforators at the medial aspect of the breast.
Figure 1.
a. Pre-op and b. 4-month postoperative images of patient undergoing bilateral NSM for BRCA2+ risk reduction.
During the mastectomy, the nipple was everted; the core of sub-areolar tissue was removed and submitted for frozen section. The sub-areolar margin on the breast specimen was marked for permanent pathologic evaluation. If there was atypia or cancer in the subareolar breast or the underside of the nipple on either frozen or permanent analysis, the nipple was removed. Sentinel node biopsy and/or axillary dissection were performed as indicated or determined by surgical oncologist.
At the conclusion of the procedure, care was taken to ensure nipple viability by visual inspection, and flurocyntigraphy (SPY™, NOVADAQ Technologies, Inc., Bonita Springs, FL) was available if there was any concern on exam.
Statistical Analysis
Charts for participants who completed both the preoperative and 2-year post-operative BREAST-Q were examined for complications during the two-year study follow-up window. Using Q-Score program, BREAST-Q scores were converted from survey raw scores (1 through 4 or 5) to a continuous range from 0 (worst outcome) to 100 (best outcome). Median scores for each BREAST-Q matrix indexes were determined at each time point and were compared using the Wilcoxon Signed-Rank test (SAS 9.3). Data were segregated based upon surgical indication (cancer v. risk reduction). Comparisons between groups were made using the Wilcoxon Rank-Sum test for preoperative and postoperative scores. A similar analysis was done to compare postoperative scores of patients without surgical complications to patients who experienced a major or minor complication. P values of <0.05 were considered statistically significant.
Results
Between 2008 and 2011, 39 patients underwent nipple-sparing mastectomy, of which 17 were for cancer treatment and 22 were for risk reduction. The vast majority of patients (Table 2) were Caucasian (n=38, (97.4%) and underwent bilateral mastectomy (n=35, 89.7%). Demographic characteristics were similar between those undergoing NSM for cancer versus risk reduction with the exception that women undergoing NSM for RR were significantly younger (median 38.7 vs. 48.4 years, p=0.015) than those who underwent NSM for current cancer treatment. Also, cancer treatment patients were more likely to have a unilateral mastectomy (n=4, 23.5% vs. n=0, 0%, p=0.029) than RR patients. Incidental stage 0 cancer was found in 1 patient (4.5%) in the RR group. Twenty-eight patients underwent one-step immediate reconstruction and 11 underwent two-stage tissue expander/implant reconstruction, but there was no statistical difference between reconstruction type between cancer treatment and risks reduction patients (p=0.48). Race and median BMI between the two groups were not statistically different (p=0.44 and 0.66, respectively).
Table II. Demographic characteristics.
| All Patients (N=39) | Risk Reduction (N=22) | Current Cancer Treatment (N=17) | ||
|---|---|---|---|---|
| N (%) | N (%) | N (%) | p-value | |
| Median Age (Q1, Q3) | 43.7 (35.2, 49.7) | 38.7 (34.6, 46.3) | 48.4 (43.7, 53.0) | 0.0145* |
| Race | 0.4359 | |||
| White | 38 (97.4) | 22 (100) | 16 (94.1) | |
| African American/Black | 1 (2.6) | 0 (0) | 1 (5.9) | |
| Median BMI (Q1, Q3) | 21.7 (20.3, 25.2) | 22.1 (20.3, 25.4) | 21.7 (20.4, 23.6) | 0.6632 |
| Surgery | .0289* | |||
| Unilateral Mastectomy | 4 (10.3) | 0 (0) | 4 (23.5) | |
| Bilateral Mastectomy | 35 (89.7) | 22 (100) | 13 (76.5) | |
| Cancer Stage | <.0001* | |||
| N/A | 21 (53.8) | 21 (95.5) | 0 (0) | |
| 0 | 11 (28.2) | 1 (4.5) | 10 (58.8) | |
| I | 2 (5.1) | 0 (0) | 2 (11.8) | |
| II | 4 (10.3) | 0 (0) | 4 (23.5) | |
| Other (phyllodes) | 1 (2.6) | 0 (0) | 1 (5.9) | |
| Reconstruction | 0.4824 | |||
| 1-step | 28 (71.8) | 17 (77.3) | 11 (64.7) | |
| 2-stage | 11 (28.2) | 5 (22.7) | 6 (35.3) | |
| Reconstruction Type | 0.2080 | |||
| Autologous | 2 (5.1) | 1 (4.6) | 1 (5.9) | |
| Autologous and Othera | 2 (5.1) | 0 (0.0) | 2 (11.8) | |
| Tissue Expander | 10 (25.6) | 5 (22.7) | 5 (29.4) | |
| One Stage Implant | 21 (53.9) | 12 (54.5) | 9 (52.9) | |
| Reverse – One Stage | 4 (10.3) | 4 (18.2) | 0 (0.0) | |
| Adjuvant Treatments | 0.1678 | |||
| None | 31 (79.5) | 20 (90.9) | 11 (64.7) | |
| Chemotherapy | 4 (10.3) | 1 (4.6) | 3 (17.6) | |
| Endocrine Therapy | 2 (5.1) | 1 (4.6) | 1 (5.9) | |
| Chemotherapy and Endocrine Therapyb | 2 (5.1) | 0 (0.0) | 2 (11.8) | |
| Complications | 0.2429 | |||
| None | 30 (76.9) | 19 (86.4) | 11 (64.7) | |
| Minor | 2 (5.1) | 1 (4.5) | 1 (5.9) | |
| Major | 7 (18.0) | 2 (9.1) | 5 (29.4) |
N=1 patient had an Autologous and One Stage Implant, and N=1 patient had an Autologous and Tissue Expander procedure
N=1 patient had Chemotherapy, Endocrine Therapy, and Radiation Therapy
p <.05 by Wilcoxon Rank-Sum Test or Fisher's Exact Test
There were 9 patients (23.1%) who experienced complications. Two had minor complications, including cellulitis treated with oral antibiotics (n=1) and delayed wound healing exceeding 3 weeks after operation (n=1)). Seven patients had major complications, including three with capsular contracture and four with partial mastectomy flap loss treated by surgical revision (n=1), hyperbaric oxygen and local wound care (n=1), and local care only (n=2)). No nipples were removed due to necrosis of the NAC, but three patients had nipples removed due to positive margins on pathological analysis.
Table 3 lists self-reported median measures of wellness at the preoperative setting compared to two years after reconstruction. There were significant increases in the matrix indexes for overall satisfaction with breasts (+8, IQR= (-7, +22), p=0.021) and psychosocial well-being (+14, IQR= (0, +30), p=0.003) amongst all patients. The index for physical impact of the surgery declined from pre- versus post-op but this was not significant (-2, IQR= (-14, +6), p=0.055). The measure of overall satisfaction with outcome, which can only be measured post-operatively, was 75 (IQR=67,100).
Table III. Self-reported measures of wellness improved amongst all patients undergoing nipple sparing mastectomy up to two years postoperatively.
| Preoperative | Postoperative | Delta | ||
|---|---|---|---|---|
| Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | p-value | |
| Satisfaction- Breasts | 63 (53, 79) | 73 (64, 81) | 8 (-7, 22) | 0.0213* |
| Psychosocial Wellness | 70 (58, 86) | 86 (70, 100) | 14 (0, 30) | 0.0032* |
| Sexual Well-Beinga | 57 (47, 63) | 57 (49, 72) | 3 (-7.5, 21.5) | 0.1527 |
| Physical impact (chest)b | 85 (68, 100) | 77 (74, 85) | -2 (-14, 6) | 0.0547 |
| Overall Satisfaction with Outcome | 75 (67, 100) |
N=36 patients with pre and postoperative scores
N=38 patients with pre and postoperative scores
p <.05 by Wilcoxon Signed-Rank Test
The impact of the indication for surgery (cancer treatment vs. RR) on median BREAST-Q scores was determined (Table 4). There was no significant difference in pre-operative BREAST-Q scores between the cancer and RR groups. However, two years after surgery, risk reduction patients had significantly higher scores for the psychosocial well-being (92 vs. 73, p=0.019) and physical well-being of the chest region (79 vs. 72.5, p=0.010) compared to the cancer treatment NSM group. When analyzing the degree of change from pre-op to post-op measures based on the surgical indication, RR patients had a significantly greater psychosocial function (+17 vs. +1, p=0.043) two years following reconstruction compared to those undergoing NSM for cancer treatment. Patients undergoing NSM for RR demonstrated a significantly greater satisfaction with outcome than current cancer treatment patients (75, IQR= (75,100) vs. 75, IQR= (67, 75), p=0.033).
Table IV. Impact of active cancer on patient reported measures.
| Preoperative survey measures | |||
|---|---|---|---|
| Active Cancer (N = 17) | Risk Reduction (N = 22) | p-value | |
| Breast Health | 58 (53, 79) | 70 (53, 70) | 0.8866 |
| Psychosocial Wellness | 79 (58, 86) | 68.5 (63, 82) | 0.6594 |
| Sexual Well-Beinga | 57 (54, 63) | 57 (45, 63) | 0.6505 |
| Physical impact (chest) | 74 (68, 85) | 91 (74, 100) | 0.0875 |
| Postoperative survey measures | |||
| Active Cancer (N = 17) | Risk Reduction (N = 22) | p-value | |
| Breast Health | 71 (61, 78) | 76.5 (69, 85) | 0.0990 |
| Psychosocial Wellness | 73 (65, 92) | 92 (82, 100) | 0.0194* |
| Sexual Well-Beingb | 57 (47, 67) | 60 (50.5, 80) | 0.2595 |
| Physical impact (chest)c | 72.5 (58.5, 79) | 79 (77, 100) | 0.0098* |
| Overall satisfaction with outcome | 75 (67, 75) | 75 (75, 100) | 0.0326* |
| Difference between preoperative and postoperative survey measures | |||
| Active Cancer (N = 17) | Risk Reduction (N = 22) | p-value | |
| Breast Health | 6 (-7, 15) | 8.5 (-4, 28) | 0.4744 |
| Psychosocial Wellness | 1 (-16, 24) | 17 (10, 33) | 0.0427* |
| Sexual Well-Beingd | 0 (-8, 15) | 20 (-5, 70) | 0.0767 |
| Physical impact (chest)c | -10.5 (-14, 6) | 0 (-14, 9) | 0.6171 |
N=21 patients in the Risk Reduction group
N=20 patients in the Risk Reduction group
N=16 patients in the Active Cancer group
N=19 patients in the Risk Reduction group
p <.05 by Wilcoxon Rank-Sum Test
There was no significant difference in postoperative BREAST-Q scores between those patients who experienced post-operative complications compared to those who did not (data not shown).
Discussion
The current study presents longitudinal, two-year BREAST-Q outcome data for a series of 39 patients who had NSM. This study further confirms high patient satisfaction following NSM surgery (overall median satisfaction with outcome= 75) and lends support to aesthetic consideration of NSM use. Further, this study demonstrates significant increase in the self-reported measures of wellness (overall satisfaction with breasts and psychosocial wellness as well as overall satisfaction with outcome) two years following NSM. Both cancer patients and RR groups demonstrated increase in satisfaction measures from pre-op to post-op. The RR patients had a significantly greater increase in psychosocial well-being than cancer patients, which may be explained by RR patients proactively choosing a procedure and cancer patients have less ‘choice’ and may have ongoing concerns about long-term prognosis of disease.
This study contains pre-surgical data in addition to data at two years after surgery. A similarly designed study by Peled, et al [17] was published in 2014, which reported 28 NSM patients evaluated with the BREAST-Q before operation and at one year following operation. Their prospective series demonstrated that the BREAST-Q domains of overall satisfaction with breasts, psychosocial and sexual well-being initially decreased but returned to baseline after 1 year. At one year, their satisfaction with breast score was 67.8 and satisfaction with outcome score was 68.1. Our findings show a higher satisfaction with outcome score of 75 at two-years, a difference may be attributed to the different patient populations. The relatively small numbers in these studies may not be an accurate estimate of a larger population view about NSM. Sugrue et al [18] also utilized preoperative BREAST-Q, but this was collected retrospectively.
There are additional studies that have utilized the BREAST-Q to survey NSM patients following surgery but do not have preoperative comparison data.[8,19-25] A study by Metcalfe et al [19] utilized the BREAST-Q on NSM and SSM patients four years after mastectomy (Table 5). NSM patients had a significantly higher “breast satisfaction” (71.7 vs. 61.2, p=.01), satisfaction with outcome (84.8 vs. 74.1, p = 0.02) and sexual well-being (68.5 vs. 52.1, p < 0.001) compared to SSM patients, but there was no preoperative measurement for comparison. Preoperative measurement of breast health, psychosocial well-being, and sexuality establish a baseline measurement with which to determine if NSM decreases or increases these quality of life outcomes. Without a baseline measurement it is impossible to know if a score at one, two or four years after surgery, even if high, is actually a change from the baseline score. At the same time, it is encouraging that our two-year scores correlate well with other published NSM studies that have utilized the BREAST-Q.[17,19,20]
Table V. Comparison of Breast Reconstruction Studies Utilizing the BREAST-Q.
| Reference | Patient Base | Number of patients | Breast-Q Done Preoperatively (y/n) | Breast-Q Postop Time point(s) | Scales | Preoperative Score | Postop Score | ||
|---|---|---|---|---|---|---|---|---|---|
| Howard 2016 | Nipple Sparing Mastectomy | 48 | y | 2 years | Satisfaction with breasts | 63 | 73 | ||
| Psychosocial well-being | 70 | 86 | |||||||
| Physical well-being | 85 | 77 | |||||||
| Sexual well-being | 57 | 57 | |||||||
| Satisfaction with outcome | n/a | 75 | |||||||
| Peled 2014 | Total Skin Sparing Mastectomy and Immediate Tissue Expander-Implant Reconstruction | 28 | y | 3, 6, 12 months | Satisfaction with breasts | 69.8 | 67.8 | ||
| Psychosocial well-being | 75.7 | 74.9 | |||||||
| Physical well-being | 84.3 | 72.5 | |||||||
| Sexual well-being | 58.3 | 57.7 | |||||||
| Satisfaction with outcome | n/a | 68.1 | |||||||
| Jeeven 2014 | Breast recon +/- immediate recon or delayed reconstruction | 7,110 | n | 3-mo, 18 mo | Satisfaction with breasts | 55 | |||
| Psychosocial well-being | 65 | ||||||||
| Physical well-being | 75 | ||||||||
| Sexual well-being | 46 | ||||||||
| McCarthy 2010 | Silicone implant subset | 176 gel patients | n | 2.4 years* | Satisfaction with breasts | 58.9 | |||
| Salgarello 2012 | Subset of immediate recon patients | 12 | n | “during reconstruction” | Satisfaction with breasts | 62.8 | |||
| Psychosocial well-being | 63.3 | ||||||||
| Physical well-being | 35.1 | ||||||||
| Sexual well-being | 64 | ||||||||
| Satisfaction with outcome | 65.8 | ||||||||
| No CPM | CPM | ||||||||
| Koslow 2013 | Subset of immediate implant-based recon in Contralateral Prophylactic Mastectomy (CPM)vs no CPM studyγ | 294 | n | 4.3 years post-mastectomy | Satisfaction with breasts | 54.9 | 64.4 | ||
| Psychosocial well-being | 72.3 | 75.4 | |||||||
| Physical well-being | 75 | 77.4 | |||||||
| Sexual well-being | 52.3 | 55.1 | |||||||
| Satisfaction with outcome | 67.7 | 74.8 | |||||||
| Sugrue 2013 | Immediate breast reconstruction following mastectomy | 33 | y, done retrospectively | Not defined | Satisfaction with breasts | 66 | 64 | ||
| Psychosocial well-being | 67 | 69 | |||||||
| Physical well-being | 81 | 81 | |||||||
| Sexual well-being | 52 | 54 | |||||||
| Satisfaction with outcome | n/a | Not reported | |||||||
| SSM | NSM | ||||||||
| Metcalfe 2015 | Bilateral Prophylactic Mastectomy (skin-sparing (SSM) versus nipple-sparing (NSM)) δ | 137 | n | 50 months* | Satisfaction with breasts | 62 | 71 | ||
| Psychosocial well-being | 76 | 82 | |||||||
| Sexual well-being | 49 | 72 | |||||||
| Satisfaction with outcome | 75 | 100 | |||||||
mean
Breast-Q reported as CPM versus No CPM
Breast-Q reported as SSM versus NPM
One may hypothesize that cancer patients would start at lower satisfaction levels, as a recent cancer diagnosis may negatively impact a patient's pre-operative BREAST-Q scores to a degree not seen in RR patients. However, our findings show that both RR and cancer patients started at relatively similar pre-testing values. It is possible that many RR patients are seen soon after a new diagnosis of BRCA1 or 2-mutation carrier status, which may have a similar negative psychological impact as a cancer diagnosis. As such, the finding of no significant pre-operative difference between the cancer and RR groups is not unexpected, particularly given the relatively smaller number of study patients. However, this study did find a difference in BREAST-Q scores between RR and cancer patients postoperatively at two-years. RR patients had higher scores for all measures although scores for psychosocial wellness were the only significant scores. Since bilateral mastectomy reduces the risk of cancer in RR patients by 90-95%, [26] it is interesting to see a higher psychosocial score for RR patients compared to cancer patients, warranting future investigation.
A comparison of the baseline numbers for BREAST-Q results in comparable studies are presented in Table 5. Overall, the numbers demonstrated similarities between the groups. In the current study, post-operative breast satisfaction was 73 (Peled= 67.8), psychosocial well-being was 86 (Peled=74.9), physical well-being was 77 (Peled=72.5), sexual well-being was 57(Peled = 57.7) and overall satisfaction was 75 (Peled = 68.1). These studies also provide new baseline scores for BREAST-Q results in NSM surgery for future comparison.
Prior studies from our institution [4,16] and this current series, report a low complication rate for immediate implant-based breast reconstruction. In this study, occurrence of complications did not have a significant effect on the Breast Q scores two years following surgery. Most complications occur prior to two years, and thus their impact will be less at two years compared to a few months from the time of operation.
Our study has limitations. We did not utilize a comparison group of mastectomy patients not having a nipple-sparing operation. Further, our patient volume is low which, reflects the difficulty in obtaining baseline and two-year data on reconstructed patients. Although we have baseline and two-year data, our dataset at one year from surgery is deficient and therefore was not reported. However, we felt that measurements at two years would more accurately reflect patients' satisfaction with their outcome since many patients are still undergoing treatments for their cancer or still experiencing psychological stress from removal of the breasts. Our patient population is a highly selected population, most were white and of younger ages, although this does represent the demographic of patients that are undergoing NSM.
In conclusion, our study demonstrates that patient satisfaction with NSM is high at two years in both the cancer and RR setting despite operative complications. We are also encouraged by the fact that the BREAST-Q scores increased compared to baseline and did not decrease. The BREAST-Q has become the standard tool with which to measure patient reported outcomes after breast reconstruction. These findings demonstrate that NSM is associated with high patient satisfaction. And, with more studies demonstrating it is oncologically safe, we expect more surgeons will perform NSM with time for both cancer and RR patients.
Conclusions
The Breast Q is a well-accepted PRO measurement tool for breast surgery. Use of the BREAST-Q in patients undergoing NSM demonstrated high levels of satisfaction following surgery compared to baseline measurements prior to surgery. Patients undergoing NSM for RR demonstrated higher levels of satisfaction on the psychosocial and physical symptoms of the chest than cancer patients. These data add to the growing body of literature regarding PRO following NSM.
Synopsis.
Women undergoing nipple-sparing mastectomy (NSM) were given the BREAST-Q survey preoperatively and two years postoperatively as a measure of patient reported outcomes. Following NSM, patients demonstrated high levels of, and improved satisfaction on BREAST-Q measurement indices.
Acknowledgments
Financial Disclosures: Funding for this study was obtained from a research grant award from the NorthShore University HealthSystem Auxiliary Board.
Footnotes
Author disclosures: Dr. Pusic is a co-developer of the BREAST-Q and receives royalties when the questionnaire is used in for-profit industry-sponsored clinical trials.
Paper References
- 1.Sacchini V, Pinotti JA, Barros AC, et al. Nipple-sparing mastectomy for breast cancer and risk reduction: oncologic or technical problem? Journal of the American College of Surgeons. 2006;203:704–714. doi: 10.1016/j.jamcollsurg.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Etienne CA, Borgen PI. Update on the indications for nipple-sparing mastectomy. The journal of supportive oncology. 2006;4:225–230. [PubMed] [Google Scholar]
- 3.De La Cruz L, Moody AM, Tappy EE, et al. Overall Survival, Disease-Free Survival, Local Recurrence, and Nipple-Areolar Recurrence in the Setting of Nipple-Sparing Mastectomy: A Meta-Analysis and Systematic Review. Ann Surg Oncol. 2015;22:3241–3249. doi: 10.1245/s10434-015-4739-1. [DOI] [PubMed] [Google Scholar]
- 4.Yao K, Liederbach E, Tang R, et al. Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol. 2015;22:370–376. doi: 10.1245/s10434-014-3883-3. [DOI] [PubMed] [Google Scholar]
- 5.Djohan R, Gage E, Gatherwright J, et al. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plastic and reconstructive surgery. 2010;125:818–829. doi: 10.1097/PRS.0b013e3181ccdaa4. [DOI] [PubMed] [Google Scholar]
- 6.Kissin MW, Kark AE. Nipple preservation during mastectomy. The British journal of surgery. 1987;74:58–61. doi: 10.1002/bjs.1800740118. [DOI] [PubMed] [Google Scholar]
- 7.Lee C, Sunu C, Pignone M. Patient-reported outcomes of breast reconstruction after mastectomy: a systematic review. Journal of the American College of Surgeons. 2009;209:123–133. doi: 10.1016/j.jamcollsurg.2009.02.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salgarello M, Visconti G, Barone-Adesi L. Nipple-sparing mastectomy with immediate implant reconstruction: cosmetic outcomes and technical refinements. Plastic and reconstructive surgery. 2010;126:1460–1471. doi: 10.1097/PRS.0b013e3181ef8bce. [DOI] [PubMed] [Google Scholar]
- 9.Wellisch DK, Schain WS, Noone RB, Little JW., 3rd The psychological contribution of nipple addition in breast reconstruction. Plastic and reconstructive surgery. 1987;80:699–704. doi: 10.1097/00006534-198711000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Dossett LA, Lowe J, Sun W, et al. Prospective evaluation of skin and nipple-areola sensation and patient satisfaction after nipple-sparing mastectomy. J Surg Oncol. 2016 doi: 10.1002/jso.24264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cano SJ, Klassen AF, Scott AM, Pusic AL. A closer look at the BREAST-Q((c)) Clinics in plastic surgery. 2013;40:287–296. doi: 10.1016/j.cps.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Pusic AL, Klassen AF, Cano SJ. Use of the BREAST-Q in clinical outcomes research. Plastic and reconstructive surgery. 2012;129:166e–167e. doi: 10.1097/PRS.0b013e3182362e65. author reply 167e. [DOI] [PubMed] [Google Scholar]
- 13.Cano SJ, Klassen AF, Scott AM, et al. The BREAST-Q: further validation in independent clinical samples. Plastic and reconstructive surgery. 2012;129:293–302. doi: 10.1097/PRS.0b013e31823aec6b. [DOI] [PubMed] [Google Scholar]
- 14.Klassen AF, Pusic AL, Scott A, et al. Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC women's health. 2009;9:11. doi: 10.1186/1472-6874-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plastic and reconstructive surgery. 2009;124:345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 16.Rundell VL, Beck RT, Wang CE, et al. Complication prevalence following use of tutoplast-derived human acellular dermal matrix in prosthetic breast reconstruction: a retrospective review of 203 patients. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2014;67:1345–1351. doi: 10.1016/j.bjps.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Peled AW, Duralde E, Foster RD, et al. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg. 2014;72(1):S48–52. doi: 10.1097/SAP.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 18.Sugrue R, MacGregor G, Sugrue M, et al. An evaluation of patient reported outcomes following breast reconstruction utilizing Breast Q. Breast. 2013;22:158–161. doi: 10.1016/j.breast.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Metcalfe KA, Cil TD, Semple JL, et al. Long-Term Psychosocial Functioning in Women with Bilateral Prophylactic Mastectomy: Does Preservation of the Nipple-Areolar Complex Make a Difference? Ann Surg Oncol. 2015;22:3324–3330. doi: 10.1245/s10434-015-4761-3. [DOI] [PubMed] [Google Scholar]
- 20.van Verschuer VM, Mureau MA, Gopie JP, et al. Patient Satisfaction and Nipple-Areola Sensitivity After Bilateral Prophylactic Mastectomy and Immediate Implant Breast Reconstruction in a High Breast Cancer Risk Population: Nipple-Sparing Mastectomy Versus Skin-Sparing Mastectomy. Ann Plast Surg. 2014 doi: 10.1097/SAP.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 21.Jeevan R, Cromwell DA, Browne JP, et al. Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2014;67:1333–1344. doi: 10.1016/j.bjps.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 22.Davis GB, Lang JE, Peric M, et al. Breast reconstruction satisfaction rates at a large county hospital. Ann Plast Surg. 2014;72(1):S61–65. doi: 10.1097/SAP.0000000000000171. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010;116:5584–5591. doi: 10.1002/cncr.25552. [DOI] [PubMed] [Google Scholar]
- 24.Salgarello M, Rochira D, Barone-Adesi L, Farallo E. Immediate breast reconstruction after skin- or nipple-sparing mastectomy for previously augmented patients: a personal technique. Aesthetic Plast Surg. 2012;36:313–322. doi: 10.1007/s00266-011-9809-6. [DOI] [PubMed] [Google Scholar]
- 25.Koslow S, Pharmer LA, Scott AM, et al. Long-term patient-reported satisfaction after contralateral prophylactic mastectomy and implant reconstruction. Ann Surg Oncol. 2013;20:3422–3429. doi: 10.1245/s10434-013-3026-2. [DOI] [PubMed] [Google Scholar]
- 26.Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2004;22:1055–1062. doi: 10.1200/JCO.2004.04.188. [DOI] [PubMed] [Google Scholar]