Abstract
Objectives
Guidelines recommend ACE inhibitors (ACEi), angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs) and diuretics in all patients with diabetes mellitus. However, the effectiveness of these agents in South Asian and Chinese populations is unknown. We sought to determine whether ACEi, ARB, CCB and diuretics are associated with reduced mortality in South Asian, Chinese and other patients with diabetes.
Design
Population-based cohort study using administrative health databases.
Setting
Province of British Columbia, Canada (2006–2013).
Participants
Patients aged ≥35 years with incident diabetes.
Primary and secondary outcome measures
Primary outcome was all-cause mortality for each medication class compared with untreated patients within each ethnicity. Treatment effect was assessed using inverse probability of treatment weighted Cox proportional hazards models. Medication adherence effect on mortality was also evaluated.
Results
208 870 patients (13 755 South Asian, 22 871 Chinese, 172 244 other Canadian) were included. ACEi reduced mortality in other patients (HR=0.88, 0.84–0.91), but power was insufficient to evaluate for benefit in Chinese and South Asian patients. ARB and diuretics reduced mortality in Chinese (ARB HR=0.64, 0.50–0.82; diuretics HR=0.77, 0.62–0.96) and other patients (ARB HR=0.69, 0.64–0.74; diuretics HR=0.66, 0.63–0.69) compared with untreated patients. No mortality benefit was observed among South Asians for any drug class or for CCB among all ethnicities. Higher medication adherence was associated with lower mortality for other patients only (HR=0.79, 0.72–0.86).
Conclusions
Effectiveness of cardiovascular risk reduction therapy on mortality varies considerably by ethnicity. Further study is needed to evaluate the mortality benefit of antihypertensive agents in South Asians. Inclusion of these ethnic groups in future clinical trials is essential to examine for differential responses.
Keywords: epidemiology, hypertension
Strengths and limitations of this study.
This study addresses a substantial gap in the literature regarding long-term effectiveness of commonly used antihypertensive drug classes among patients with diabetes of South Asian and Chinese descent.
The analysis is conducted on a large, population-based data set including significant numbers of people of different ethnicities in Canada, allowing for measurement of real-world effects on mortality.
Limitations include possible residual confounding due to unmeasured variables.
Introduction
Pharmacological treatment of hypertension in patients with type 2 diabetes mellitus (diabetes) is associated with significantly reduced mortality.1 International guidelines recommend routinely using antihypertensive medications to reduce cardiovascular risk in all patients with diabetes, including those of Asian ethnicity.2–5 However, most trials of cardiovascular risk reduction therapy in patients with diabetes occurred in western populations.
Response to these therapies can be affected by ethnicity. ACE inhibitors (ACEi) were found to be less effective in reducing mortality and cardiovascular events among black patients with hypertension and diabetes compared with other antihypertensive agents.6–8 Several studies also reported higher risk of ACEi-induced cough in Chinese patients suggesting that there may be some underlying differences in response to these medications.9 Others reported that South Asians may have increased sympathetic activity, possibly causing differing responses to antihypertensive classes.10 An analysis in South Asian and Chinese patients with newly diagnosed diabetes found significant mortality reductions associated with statin use.10 However, similar analyses are currently lacking for antihypertensive agents.
The benefit of ACEi in reducing cardiovascular risk in diabetes was established in multiple large randomised control trials (RCT) of western patients, with 24% reduction in the secondary outcome of total mortality seen in the HOPE study.11–13 These benefits were similar to angiotensin receptor blockers (ARBs) based on the ONTARGET study subset of patients with diabetes.14 However, the PRoFESS trial included 18% of patients of Chinese ethnicity and 8.4% of South Asian ethnicity, and found no benefit of telmisartan in reducing major cardiovascular events.15 Additionally, major randomised trials examining thiazide and thiazide-like diuretics (SHEP,16 ALLHAT7), calcium channel blockers (CCB) (ALLHAT7) and CCB-based combinations (ACCOMPLISH17) were conducted in predominantly western populations.
The burden of diabetes in South Asian and Chinese populations is tremendous, with these ethnic groups representing 62% of all adults with diabetes globally.18 In this context, the paucity of large studies specifically comparing long-term effectiveness of major antihypertensive drug classes in these ethnicities is concerning.19 With the existing, widespread use of these medications, such studies are unlikely to be conducted in the near future. In an effort to fill the information gap, we conducted a population-based cohort study to determine whether ACEi, ARB, dihydropyridine CCB and diuretics are effective in reducing all-cause mortality in a population cohort of South Asian (originating from Pakistan, India or Bangladesh), Chinese (originating from China, Taiwan or Hong Kong) and other patients with newly diagnosed diabetes.
Research design and methods
Study overview
We conducted an analysis using population-based administrative data of adults aged ≥35 years living in British Columbia, Canada, with newly diagnosed diabetes between 1 April 2006 and 31 March 2013.
Data sources
We used administrative data from British Columbia, Canada. We obtained deidentified linked health datasets through Population Data BC with approval of relevant data stewards and the University of British Columbia’s Behavioural Research Ethics Board.20 All inferences, opinions and conclusions drawn in this report are those of the authors and do not reflect the opinions or policies of Population Data BC.
The databases covered all British Columbians except those whose prescription drug coverage fell under federal jurisdiction (ie, military, veterans, inmates of federal penitentiaries and status Indians living on reserves, approximately 4.0% of the total population). All residents included in our dataset are covered under British Columbia’s universal, public health insurance programme for medical and hospital care; and all are eligible for coverage under British Columbia’s universal, public drug benefit plan, under which deductibles are set in relation to household income.
British Columbia has a total population of 4.6 million people, including approximately 210 400 South Asian and 373 800 Chinese people.21 22 Because the public health insurance programme covers virtually all health encounters, data from physician billing claims can be used to identify diagnoses. We extracted International Classification of Diseases (ICD-9 and ICD-10) codes from physician claims including both inpatient and outpatient encounters. Outpatient billing data include a single diagnosis for each encounter. Inpatient data include both primary (most responsible diagnosis) and secondary (comorbid conditions) diagnosis codes from hospital discharge abstracts (up to 25 codes for each encounter). Data on medication use were extracted from PharmaNet, a provincial electronic database that contains a record of all dispensed prescriptions from community pharmacies. The accuracy of this database against prescriptions is estimated to be greater than 99%.23 Data on time of death were obtained from the vital statistics database and reporting of all deaths in the province is mandatory.
Study population
The study population was restricted to people with a new diagnosis of diabetes during the study period. A new diagnosis of diabetes was defined as an ICD-9 or ICD-10 code for diabetes for at least one hospital discharge abstract or two physician claims within 2 years (ICD-9-CM: 250.x; ICD-10: E109, E119, E139, E149, E101, E111, E131, E141, E105, E115, E135 and E145). To ensure that these cases were truly new diagnoses, we set a washout period of 3 years (ie, no physician claims for diabetes in the preceding 3 years). This algorithm is entirely based on administrative billing data, and was previously validated against physician diagnosis of diabetes in adults aged ≥35 years with sensitivity 92% and specificity 97% in identifying diagnoses of diabetes in British Columbia.24–26 Index date was defined as the earliest contact with the healthcare system with the diabetes diagnosis. Patients who died within 1 month of diabetes diagnosis were excluded from the analysis.
Categorising ethnic group
Because ethnicity is not routinely recorded in Canadian administrative health data, we used an algorithm developed to identify surnames of South Asian and Chinese origin that has been validated for use in administrative data research by Shah et al. 27 Canadian census data show that 93% of South Asians and 90% of Chinese marry people of the same ethnic background, minimising the chance of misidentification due to mixed marriages.28 We labelled the remaining population as ‘other.’ In the province of British Columbia, the vast majority of this group consists of individuals of European ancestry (>90%), with very few people of African ancestry (<1%).29
Sociodemographics and comorbid conditions
We estimated socioeconomic status (SES) using income quintile. We estimated household income based on a combination of household-specific and area-based income data.30 We also included comorbidities from the Charlson comorbid conditions list.31 These conditions were extracted from all inpatient and outpatient claims dating from up to 1 year prior to the index date.
Cardiovascular risk reduction medications
Within each ethnicity, we classified study patients as either treated or untreated with each antihypertensive medication class: ARB, ACEi, dihydropyridine CCB and thiazide or thiazide-type diuretics. We considered patients as treated with a medication if they received at least one prescription within 1 year after index diagnosis, a time period used in other similar studies.32
Outcome measures
Patients were followed for up to 4 years for the primary outcome measure, time to death from any cause. Risk was determined for South Asian, Chinese and other patients treated on each medication as compared with untreated patients (regardless of other antihypertensive use) within each ethnicity as a baseline.
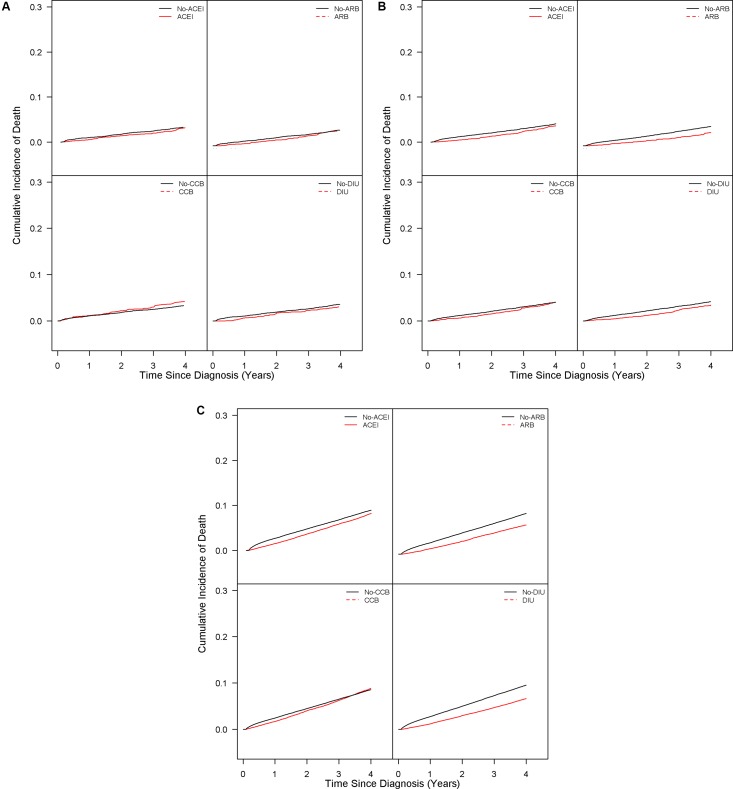
Statistical analysis
Baseline characteristics for each ethnic group were summarised and compared among the groups using the χ2 test for categorical variables and analysis of variance for continuous variables. We constructed inverse probability of treatment weighted (IPTW) Cox proportional hazards models for the treatment effect on mortality.33 34 This method is aimed at minimising effects of confounding by indication.35 The weight was based on a propensity score of having treatment, estimated from a multivariable logistic regression model with receiving treatment as a binary outcome variable and age, gender, SES, Charlson comorbidities and baseline use of other medications as independent variables. In particular, the weight for each subject was computed by taking the inverse probability of receiving treatment that the subject received and stabilised by multiplying marginal probability of the actual treatment received.36 Means and SD of the weights were assessed to verify the positivity assumption. Schoenfeld residuals were explored to examine the proportional hazards assumption. Cumulative incidence of death was also visualised for the weighted sample. Use of other medications (insulin, use of other antihypertensive agents and statins) at baseline was defined as a prescription recorded within 1 month before or after diagnosis. The data were censored at the end of the 4-year observation period or at death, whichever came first.
Statistical power for each drug by ethnicity was calculated using the log-rank test, specifying actual sample sizes, allocation ratio, treatment and event rates observed and HR as derived from the risk reduction observed in major clinical trials (online supplementary table S1). Estimated power was >99.9% for the other group (all classes) and for ARB in Chinese, >80% for ARB in South Asians and ACEi in Chinese patients, and <80% for the remaining categories.
bmjopen-2016-013808supp001.pdf (83.6KB, pdf)
In a sensitivity analysis to account for effects of differential drug exposure (including treatment cessation or switching between classes), we evaluated the association of level of medication adherence with mortality among patients who were treated with at least one of the four study medication classes. We constructed the IPTW Cox proportional hazards models to compare among the medication adherence levels. In particular, the adherence of each medication was measured over 1 year since the first prescription using proportion of days covered (PDC), which has a high predictive validity for hospitalisation episodes.37 The PDC is defined as [(number of days supply of medication in the index period)/(number of days in the study period)]×100. The mean PDC across the four classes was calculated and classified into three levels with PDC ≥0.80 classified as high adherence, 0.50≤PDC<0.80 as moderate adherence and PDC <0.50 as low adherence.
All p values presented are two tailed, and a value of less than 0.05 was considered significant for all computations. Analyses were performed with SAS V.9.4.
Results
Baseline characteristics and prescribing
There were 208 870 patients (13 755 South Asian, 22 871 Chinese, 172 244 other) included in the analysis (table 1). Most patients were elderly with South Asian patients being younger than the other groups at time of diagnosis. South Asian and Chinese patients were more likely than other patients to be in the two lowest socioeconomic quintiles. Hypertension was present in almost half of patients across all ethnicities (42% South Asian, 44% Chinese, 48% other). The prevalence of comorbid conditions was low in this cohort with South Asian and Chinese patients having generally a lower prevalence of conditions compared with others, including myocardial infarction, congestive heart failure, peripheral vascular disease and cerebrovascular disease.
Table 1.
Baseline characteristics among patients with diabetes aged 35 years and older*
| Characteristics | South Asian (n=13 755) | Chinese (n=22 871) | Other (n=172 244) |
| Age, mean age (years)±SD or % | |||
| All patients | 56.4±12.6 | 59.2±12.7 | 61.5±12.8 |
| 35–49 | 33.2 | 24.7 | 18.8 |
| 50–64 | 39.8 | 43.1 | 42.0 |
| 65–79 | 23.2 | 25.3 | 29.5 |
| ≥80 | 3.87 | 6.8 | 9.7 |
| Women (%) | 45.0 | 48.4 | 45.1 |
| Income quintile (%) | |||
| First quintile (low) | 25.6 | 27.4 | 21.2 |
| Second quintile | 32.2 | 23.4 | 20.7 |
| Third quintile | 20.4 | 20.2 | 20.0 |
| Fourth quintile | 12.3 | 14.4 | 19.3 |
| Fifth quintile (high) | 8.8 | 13.4 | 17.5 |
| Unknown | 0.7 | 1.0 | 1.2 |
| Comorbidities (%) | |||
| Hypertension | 42.0 | 44.0 | 47.9 |
| Myocardial infarction | 2.2 | 1.0 | 2.6 |
| Congestive heart failure | 3.0 | 2.1 | 5.3 |
| Peripheral vascular disease | 0.6 | 1.3 | 2.0 |
| Cancer | 2.8 | 3.8 | 6.3 |
| Cerebrovascular disease | 1.8 | 2.0 | 3.2 |
| Chronic pulmonary disease | 11.2 | 6.4 | 11.4 |
| Renal disease | 2.2 | 2.3 | 3.1 |
| Medications prescribed at baseline, n (%) | |||
| ACEi | 15.7 | 11.0 | 22.8 |
| ARB | 7.2 | 10.0 | 8.7 |
| CCB | 8.1 | 9.1 | 8.5 |
| Diuretic | 11.3 | 12.4 | 18.3 |
| β-blocker | 9.5 | 8.4 | 13.3 |
| Metformin | 21.3 | 15.4 | 23.8 |
| Sulfonylurea | 3.8 | 2.6 | 3.5 |
| Insulin | 0.6 | 0.7 | 1.7 |
| Statin | 24.2 | 20.8 | 26.9 |
| Medications prescribed after 1 year of diabetes diagnosis, n (%) | |||
| ACEi | 26.1 | 17.8 | 33.5 |
| ARB | 12.6 | 16.3 | 13.7 |
| CCB | 12.6 | 13.9 | 12.8 |
| Diuretic | 18.7 | 18.6 | 27.0 |
| Any ACEi, ARB, CCB, diuretic | 55.2 | 47.7 | 64.9 |
*All p values comparing the three ethnic groups were less than 0.001.
ACEi, ACE inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
Other patients were the most likely to be prescribed antihypertensive agents at baseline, with the most frequently prescribed classes being ACEi (23%) and diuretics (18%). South Asians were also likely to be prescribed with ACEi (16%) and diuretics (11%). Chinese patients had a more equal distribution among ACEi, ARB, CCB and diuretic prescriptions (9.1%–12%). By the end of 1 year since initial diabetes diagnosis, almost two-thirds of other patients were prescribed at least one antihypertensive agent, with a lower proportion in South Asian and Chinese patients. The most frequently prescribed class of antihypertensive agent by this time was ACEi (26% South Asians, 18% Chinese, 34% other), followed by diuretics (19% South Asians, 19% Chinese, 27% other).
Mortality
Overall, 6.5% of patients (n=355 for South Asian, n=679 for Chinese, n=11 480 for other) died during the follow-up period (median 3 years; figure 1). Among other patients, ACEi (HR=0.88, 0.84–0.91; table 2), ARB (HR=0.69, 0.64–0.74) and diuretics (HR=0.66, 0.63–0.69) were associated with substantial reductions in all-cause mortality, with minimal association observed with CCB (HR=1.00, 0.94–1.05). Consistent with the positivity assumption, the means of the stabilised weights were close to one with low SD (online supplementary table S2).
Figure 1.
Cumulative incidence of death* for patients treated with ACEi, ARB, CCB and DIU according to ethnicity: (A) South Asian; (B) Chinese; (C) other. * Cox proportional hazards models were weighted using a propensity score model by the IPTW method adjusted for age, sex, SES, Charlson comorbidities and use of other medications (insulin, ACEi, ARB, beta-blockers, CCB, diuretics and statins) at baseline, defined as a prescription within 1 month before or after diagnosis. ACEi, ACE inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; DIU, diuretics; IPTW, inverse probability of treatment weighted; SES, socioeconomic status.
Table 2.
Association between antihypertensive medications and all-cause mortality according to ethnicity
| Drug | Adjusted HR* (95% CI) | |||||
| South Asian | Chinese | Other | ||||
| HR | p Value | HR | p Value | HR | p Value | |
| ACEi | 0.91 (0.71 to 1.17) | 0.47 | 0.84 (0.69 to 1.03) | 0.09 | 0.88 (0.84 to 0.91) | <0.0001 |
| ARB | 0.88 (0.63 to 1.25) | 0.48 | 0.64 (0.50 to 0.82) | 0.0004 | 0.69 (0.64 to 0.74) | <0.0001 |
| CCB | 1.25 (0.93 to 1.68) | 0.14 | 0.94 (0.77 to 1.15) | 0.56 | 1.00 (0.94 to 1.05) | 0.89 |
| Diuretic | 0.83 (0.61 to 1.12) | 0.22 | 0.77 (0.62 to 0.96) | 0.02 | 0.66 (0.63 to 0.69) | <0.0001 |
*Cox proportional hazards models were weighted using a propensity score model by the IPTW method adjusted for age, sex, SES, Charlson comorbidities and use of other medications (insulin, ACEi, ARB, beta-blockers, CCB, diuretics and statins) at baseline, defined as a prescription within 1 month before or after diagnosis.
ACEi, ACE inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; IPTW, inverse probability of treatment weighted; SES, socioeconomic status.
Similarly, among Chinese patients, ARB (HR=0.64, 0.50–0.82) and diuretics (HR=0.77, 0.62–0.96) were associated with significant mortality reduction. There was a non-significant trend towards benefit with ACEi (HR=0.84, 0.69–1.03), but there was no significant association observed with CCB.
In South Asian patients, no statistically significant mortality benefits were observed with ACEi (HR=0.91, 0.71–1.17), ARB (HR=0.88, 0.63–1.25), CCB (HR=1.25, 0.93–1.68) or diuretics (HR=0.83, 0.61–1.12).
In our sensitivity analysis that included level of drug exposure in all drug classes, a moderate to high adherence to the four antihypertensive classes was associated with lower mortality among other patients compared with low adherence (table 3). However, high or moderate adherence was not associated with reduced mortality compared with low adherence of antihypertensive medications among Chinese and South Asian patients. There was insufficient power to analyse the effects of high versus low adherence or adherence within single medication classes.
Table 3.
Association between medication adherence and all-cause mortality according to ethnicity
| Adjusted HR* (95% CI) | ||||||
| Drug | South Asian (n=9 404) |
p Value | Chinese (n=13 173) |
p Value | Other (n=124 594) |
p Value |
| Any ACEi, ARB, CCB, diuretic† | 1.11 (0.71 to 1.73) | 0.65 | 1.29 (0.83 to 2.01) | 0.25 | 0.79 (0.72 to 0.86) | <0.0001 |
*Cox proportional hazards models were weighted using a propensity score model by the IPTW method adjusted for age, sex, SES, Charlson comorbidities and use of other medications (insulin, ACEi, ARB, beta-blockers, CCB, diuretics and statins) at baseline, defined as a prescription within 1 month before or after diagnosis.
†HRs for patients prescribed any antihypertensive (ACEi, ARB, CCB, diuretic) with moderate or high adherence compared with low adherence.
ACEi, ACE inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
Discussion
Overall, we observed substantial ethnic differences in the association between of cardiovascular risk reduction therapies and mortality in patients with diabetes. Mortality reduction associated with treatment with ARB, diuretics and a trend towards mortality benefit with ACEi were observed Chinese patients. However, no significant associations with mortality and cardiovascular risk reduction therapy were seen in South Asians for any drug class.
It is difficult to directly compare our findings with those of previous major clinical trials due to differences in study methodology, inability to directly compare the magnitude of HRs and relative risks, and due to the specification of all-cause mortality as a non-primary outcome in most of these trials. Nevertheless, the associations we observed in the other population are generally consistent in direction with results from major clinical trials in patients with diabetes.13 14 33 For ACEi, the benefit we observed (HR=0.88, 0.84–0.91) is consistent with findings reported in the HOPE study (total mortality relative risk 0.76, 0.63–0.92) that compared ramipril to placebo in patients with diabetes and an additional cardiovascular risk factor.13 The mortality reduction for ARB (HR=0.69, 0.64–0.74) is similar to that seen in the LIFE study (relative risk 0.61, 0.45–0.84), comparing losartan to atenolol.38
Among Chinese patients, we observed generally similar mortality reductions associated with ACEi (HR=0.84, 0.69–1.03) and ARB (HR=0.64, 0.50–0.82) use, although the benefit of ACEi did not reach statistical significance. Notably, adherence to ACEi among Chinese patients (52%) compared with ARB (72%) is reported to be lower than other patients, and this difference may have attenuated the association with ACEi.23 Nevertheless, our results provide new evidence of these agents in a real world population extending the findings of the ONTARGET14 study, that included 14% of patients of Asian ethnicity. Given these findings, it is particularly important to emphasise the increased use of these medications, particularly given the gaps in prescription filling observed among Chinese and South Asian patients, who had lower than expected rates of renin–angiotensin system antagonist prescription.
Diuretics were associated with reduced mortality in Chinese. The effects observed (Chinese HR=0.77, 0.62–0.96) are largely consistent with those reported in the placebo-controlled SHEP trial16 diabetes subgroup (HR 0.80, 0.68–0.95). The present findings are the first to our knowledge to evaluate thiazide and thiazide-like diuretics to Chinese patients with diabetes.
We did not observe substantial benefits of CCB in any ethnic category. This result was unexpected given the findings of the ALLHAT study, that showed that CCB were equivalent to ACEi and diuretics as first-line antihypertensive agents in diabetes.7 These findings may reflect the trend that CCB are decreasingly likely to be used as initial antihypertensive therapy compared with ACEi and diuretics in Canada.39 This trend is in accordance with guidelines promoting CCB as an add-on agent given the ACCOMPLISH trial findings.17 Patients in the CCB group may have had more severe hypertension requiring more than one agent, thereby causing confounding by indication. Moreover, the comparison group in our study likely included patients treated with other agents such as ACEi, ARB and diuretics, leading to an attenuation of observed association. It is also possible that the real-world effect size varies from that observed in RCTs due to rigid selection criteria and selection bias. Further research is required to clarify the benefit of CCB, especially in South Asian and Chinese populations.
None of the drug classes were associated with any statistically significant mortality benefits among South Asians. A major reason for the lack of findings could have been a lack of power (online supplementary table S1) given low event rates (n=355 events, 2.6% event rate in South Asians; n=679 events, 3.0% in Chinese) and low prescription filling rates in this cohort. The lower rate of mortality events is consistent with evidence in our population demonstrating a lower rate of mortality following myocardial infarction, uniquely among South Asians.40 Moreover, the South Asian cohort had the youngest age distribution, and this could have led to relatively fewer mortality events and weaker associations particularly with diuretics, which may be more effective in older patients. It is conceivable that the association may also have been attenuated by additional factors such as cultural dietary practices (eg, salt intake41) and pharmacogenetical influences. For instance, ACE gene insertion/deletion polymorphisms affect serum levels of ACEi, although a long-term effect on cardiovascular outcomes has yet to be demonstrated.42 Pharmacogenetical differences may also lead to heterogeneous responses to antihypertensive agents within the same class.43 With these considerations in mind, further research is required to confirm the effectiveness and magnitude of mortality benefit of cardiovascular risk reduction therapy in South Asians.
The lack of significant associations among South Asians may also relate to poor medication adherence and reduced drug exposure. Although we performed a sensitivity analysis using drug adherence to evaluate whether drug discontinuation, switching between classes, or decreased adherence may have affected our results, only in other patients was a significant mortality reduction seen in those with moderate or high adherence. No significant associations were observed for South Asian and Chinese patients. The lack of adherence effects may be related to inadequate power to detect smaller treatment related effect size in these groups. Another possibility is that some of these patients could have switched from one medication class to another, thus, attenuating the negative effects of being unexposed to the initial medication (eg, switching from ACEi to ARB in Chinese patients due to cough). South Asian and Chinese patients may also import antihypertensive medications from out of country, limiting our ability to detect treatment differences.44 In the context of these limitations, more studies are required to evaluate the interaction between medication adherence and antihypertensive therapies in South Asian and Chinese patients.
Our large population-based observational study allowed for measurement of real-world mortality differences, minimising outcome misclassification and with virtually no loss to follow-up in the context of Canada’s universal healthcare system. Although observational studies of this nature have been shown to generally correlate with RCTs,45 we recognise that our cohort had lower prevalence of comorbid conditions compared with the more high-risk populations included in clinical trials. Thus, it is possible that a mortality benefit for ACEi and other cardiovascular risk reduction therapies may indeed exist among the subset of high-risk South Asian (and Chinese) patients that was not captured in this study. Additional studies with a larger sample size (given the relative lack of power in the South Asian cohort) or with a higher-risk cohort would be required to evaluate this possibility, especially considering the Canadian recommendation that ACEi or ARB be used for all patients with diabetes over age 55 years—even in the absence of end-organ damage or hypertension.4 To ensure that the results are generalisable to other real-world populations, more studies in other countries with different practice patterns and population compositions are required to improve external validity. We were also unable to assess for the additional benefits of combination therapies due to sample size considerations, although this likely would not have explained the lack of associations observed in the Asian cohorts. Further studies are required to assess these effects specifically in South Asian and Chinese populations with diabetes.46 Moreover, the IPTW can be used to estimate exposure effects adjusted for measured confounders only. However, there could have been residual confounding due to unmeasured variables including hypertension severity and duration, age of hypertension onset, treatment indication, treatment of previous cardiovascular comorbidities, blood pressure levels and haemoglobin A1C. Finally, there is a built-in selection bias that has been described with use of HRs.47 Given the limitations we have described, further investigations using different methodologies are required to confirm the present findings.
Given the tremendous and increasing burden of diabetes in South Asian and Chinese patients globally, there is an alarming paucity of large studies evaluating the effectiveness of routinely used cardiovascular risk reduction therapies in these groups. ACEi, ARB and diuretics are likely effective among Chinese and other patients. Although it is likely that these drugs are effective in high-risk patients with diabetes across all ethnicities including South Asians, we were unable to demonstrate this with our unselected, lower-risk population. Given that this study was not an RCT examining antihypertensive efficacy in these populations, these findings should be interpreted with caution. More research is required to evaluate the effectiveness of antihypertensive agents in South Asians and to confirm the benefit of ACEi in Chinese patients. Inclusion of these groups in future clinical trials is essential to examine for differential response by ethnicity.
Supplementary Material
Footnotes
Contributors: NAK and CHK take full responsibility for the work as a whole, including the study design, access to data and the decision to submit and publish the manuscript. NAK, CHK made substantial contributions to the conception and design, SM and KS made substantial contributions towards acquisition of data, all authors made substantial contribution to analysis of data, all authors made substantial contribution towards interpretation of data, CHK wrote the first draft and all authors participated in revising it critically for important intellectual content and all authors give final approval of the version submitted.
Funding: This study was funded by the Canadian Institutes of Health Research (CIHR). NAK is funded by a Michael Smith Foundation for Health Research Career Scientist award.
Disclaimer: The study sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Competing interests: None declared.
Ethics approval: University of British Columbia’s Behavioural Research Ethics Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All datasets are available through Population Data BC, subject to approval by relevant data stewards at the BC Ministry of Health.
References
- 1. Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–85. 10.1056/NEJMoa1001286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Diabetes Association. Standards of medical care in diabetes—2016. Diabetes Care 2016;39:S1–112.26696671 [Google Scholar]
- 3. Internal clinical guidelines Team. Type 2 diabetes in adults [Internet]. United Kingdom: National Institute for Health and Care Excellence; 2015 Dec, Report No: NG28 https://www.nice.org.uk/guidance/ng28/resources/type-2-diabetes-in-adults-management-pdf-1837338615493 (accessed 10 May 2017). [Google Scholar]
- 4. Cheng AY. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. introduction. Can J Diabetes 2013;37:S1–212. 10.1016/j.jcjd.2013.01.009 [DOI] [PubMed] [Google Scholar]
- 5. International Diabetes Federation Guideline Development Group. Global guideline for type 2 diabetes. Diabetes Res Clin Pract 2014;104:1–52. 10.1016/j.diabres.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 6. Wright JT, Dunn JK, Cutler JA, et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA 2005;293:1595–608. 10.1001/jama.293.13.1595 [DOI] [PubMed] [Google Scholar]
- 7. Whelton PK, Barzilay J, Cushman WC, et al. Clinical outcomes in antihypertensive treatment of type 2 diabetes, impaired fasting glucose concentration, and normoglycemia: antihypertensive and lipid-lowering treatment to prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005;165:1401–9. 10.1001/archinte.165.12.1401 [DOI] [PubMed] [Google Scholar]
- 8. Brewster LM, Seedat YK. Why do hypertensive patients of African ancestry respond better to calcium blockers and diuretics than to ACE inhibitors and β-adrenergic blockers? A systematic review. BMC Med 2013;11:141 10.1186/1741-7015-11-141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mahmoudpour SH, Leusink M, van der Putten L, et al. Pharmacogenetics of ACE inhibitor-induced angioedema and cough: a systematic review and meta-analysis. Pharmacogenomics 2013;14:249–60. 10.2217/pgs.12.206 [DOI] [PubMed] [Google Scholar]
- 10. Gupta AK. Racial differences in response to antihypertensive therapy: does one size fits all? Int J Prev Med 2010;1:217–9. [PMC free article] [PubMed] [Google Scholar]
- 11. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: ukpds 39. UK prospective Diabetes Study Group. BMJ 1998;317:713–20. [PMC free article] [PubMed] [Google Scholar]
- 12. Estacio RO, Jeffers BW, Hiatt WR, et al. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med 1998;338:645–52. 10.1056/NEJM199803053381003 [DOI] [PubMed] [Google Scholar]
- 13. Heart Outcomes Prevention Evaluation (HOPE) Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. The Lancet 2000;355:253–9. [PubMed] [Google Scholar]
- 14. Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008;358:1547–59. 10.1056/NEJMoa0801317 [DOI] [PubMed] [Google Scholar]
- 15. Yusuf S, Diener HC, Sacco RL, et al. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med 2008;359:1225–37. 10.1056/NEJMoa0804593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kostis JB, Wilson AC, Freudenberger RS, et al. Long-term effect of diuretic-based therapy on fatal outcomes in subjects with isolated systolic hypertension with and without diabetes. Am J Cardiol 2005;95:29–35. 10.1016/j.amjcard.2004.08.059 [DOI] [PubMed] [Google Scholar]
- 17. Weber MA, Bakris GL, Jamerson K, et al. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010;56:77–85. 10.1016/j.jacc.2010.02.046 [DOI] [PubMed] [Google Scholar]
- 18. International Diabetes Federation. IDF Diabetes Atlas [Internet]. 2015. http://www.diabetesatlas.org/component/attachments/?task=download&id=116 (accessed 6 May 2017).
- 19. Brewster LM, van Montfrans GA, Oehlers GP, et al. Systematic review: antihypertensive drug therapy in patients of African and South Asian ethnicity. Intern Emerg Med 2016;11:355–74. 10.1007/s11739-016-1422-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. BC Ministry of Health Data Stewardship Committee, BC Vital StatisticsAgency.. Consolidation File (MSP Registration & Premium Billing);Discharge Abstracts Database (Hospital Separations) and MedicalServices Plan (MSP) Payment Information File; PharmaNet; VitalStatistics Deaths [Internet]. 2012-2014. http://www.popdata.bc.ca/data
- 21. Lindsay C. The South Asian community in Canada [Internet]. Ottawa: Social and Aboriginal Statistics Division, Statistics Canada; 2001, Report No: 89–621–XIE http://www.statcan.gc.ca/pub/89-621-x/89-621-x2007006-eng.htm#4 (accessed 10 May 2017). [Google Scholar]
- 22. Lindsay C. The Chinese community in Canada [Internet]. Ottawa: Social and Aboriginal Statistics Division, Statistics Canada; 2001, Report No: 89–621–XIE http://www.statcan.gc.ca/pub/89-621-x/89-621-x2006001-eng.htm (accessed 10 May 2017). [Google Scholar]
- 23. Chong E, Wang H, King-Shier KM, et al. Prescribing patterns and adherence to medication among South-Asian, Chinese and white people with type 2 diabetes mellitus: a population-based cohort study. Diabet Med J Br Diabet Assoc 2014;31:1586–93. [DOI] [PubMed] [Google Scholar]
- 24. Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995–2005: a population-based study. The Lancet 2007;369:750–6. [DOI] [PubMed] [Google Scholar]
- 25. Chen G, Khan N, Walker R, et al. Validating ICD coding algorithms for diabetes mellitus from administrative data. Diabetes Res Clin Pract 2010;89:189–95. [DOI] [PubMed] [Google Scholar]
- 26. Khan NA, Wang H, Anand S, et al. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care 2011;34:96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shah BR, Chiu M, Amin S, et al. Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: a validation study. BMC Med Res Methodol 2010;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Milan A, Maheux H, Chui T. A portrait of couples in mixed unions. can Soc Trends [Internet]. 2010 Apr 20. 2010;89 http://www.statcan.gc.ca/pub/11-008-x/2010001/article/11143-eng.htm. [Google Scholar]
- 29. Government of Canada SC. Tables by subject: ethnic diversity and immigration [Internet]. 2013. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/ind01/l2_30000-eng.htm (accessed 6 May 2017).
- 30. Hanley GE, Morgan S. On the validity of area-based income measures to proxy household income. BMC Health Serv Res 2008;8:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Monami M, Lambertucci L, Lamanna C, et al. Are comorbidity indices useful in predicting all-cause mortality in type 2 diabetic patients? comparison between Charlson index and disease count. Aging Clin Exp Res 2007;19:492–6. [DOI] [PubMed] [Google Scholar]
- 32. Brunner NW, Ramanathan K, Wang H, et al. Effectiveness of statin prescribing on reducing mortality in South Asian, Chinese, and white patients with diabetes. Can J Cardiol 2013;29:920–6. [DOI] [PubMed] [Google Scholar]
- 33. Mansournia MA, Altman DG. Inverse probability weighting. BMJ 2016;352:i189. [DOI] [PubMed] [Google Scholar]
- 34. Mansournia MA, Danaei G, Forouzanfar MH, et al. Effect of physical activity on functional Performance and knee pain in patients with osteoarthritis: analysis with marginal structural models. Epidemiology 2012;23:631–40. [DOI] [PubMed] [Google Scholar]
- 35. Gharibzadeh S, Mohammad K, Rahimiforoushani A, et al. Standardization as a tool for causal inference in medical research. Arch Iran Med 2016;19:666–70. [PubMed] [Google Scholar]
- 36. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 2014;33:1242–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Karve S, Cleves MA, Helm M, et al. An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med Care 2008;46:1125–33. [DOI] [PubMed] [Google Scholar]
- 38. Lindholm LH, Ibsen H, Dahlöf B, et al. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan intervention for endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. The Lancet 2002;359:1004–10. [DOI] [PubMed] [Google Scholar]
- 39. McAlister FA, Campbell NR, Duong-Hua M, et al. Antihypertensive medication prescribing in 27,822 elderly Canadians with diabetes over the past decade. Diabetes Care 2006;29:836–41. [DOI] [PubMed] [Google Scholar]
- 40. Khan NA, Grubisic M, Hemmelgarn B, et al. Outcomes after acute myocardial infarction in South Asian, Chinese, and white patients. Circulation 2010;122:1570–7. [DOI] [PubMed] [Google Scholar]
- 41. Brown IJ, Tzoulaki I, Candeias V, et al. Salt intakes around the world: implications for public health. Int J Epidemiol 2009;38:791–813. [DOI] [PubMed] [Google Scholar]
- 42. Vlm Y, Pirmohamed M. Expanding role of pharmacogenomics in the management of cardiovascular disorders. Am J Cardiovasc Drugs 2013;13:151–62. [DOI] [PubMed] [Google Scholar]
- 43. Tsoi KK, Wong MC, Tam WW, et al. Cardiovascular mortality in hypertensive patients newly prescribed perindopril vs. lisinopril: a 5-year cohort study of 15,622 Chinese subjects. Int J Cardiol 2014;176:703–9. 10.1016/j.ijcard.2014.07.114 [DOI] [PubMed] [Google Scholar]
- 44. Wang L, Immigration KM-J. Barriers to healthcare and transnational ties: a case study of South korean immigrants in Toronto, Canada. Soc Sci Med 1982 2015;133:340–8. [DOI] [PubMed] [Google Scholar]
- 45. Dahabreh IJ, Sheldrick RC, Paulus JK, et al. Do observational studies using propensity score methods agree with randomized trials? A systematic comparison of studies on acute coronary syndromes. Eur Heart J 2012;33:1893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yusuf S, Lonn E, Pais P, et al. Blood-pessure and cholesterol lowering in persons without cardiovascular disease. N Engl J Med 2016;374:2032–43. [DOI] [PubMed] [Google Scholar]
- 47. Hernán MA. The hazards of hazard ratios. Epidemiol Camb Mass 2010;21:13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013808supp001.pdf (83.6KB, pdf)