Abstract
Pulmonary tumour thrombotic microangiopathy (PTTM) is a rare complication of cancer, which can be lethal due to progressive pulmonary hypertension (PH). Several case reports have demonstrated that imatinib, a platelet-derived growth factor receptor–tyrosine kinase inhibitor, can improve severe PH in patients with PTTM.
We describe the case of a 56-year-old woman. Her mean pulmonary arterial pressure (mPAP) was 47 mm Hg, and her dyspnoea worsened rapidly over several days. Although pulmonary embolism was not observed on CT, enlargement of the para-aortic lymph nodes was detected. Gastro-oesophageal endoscopy revealed signet-ring cell carcinoma. We diagnosed her as having PTTM based on her clinical course, and started treatment with imatinib. Five days after its administration, her mPAP decreased dramatically. She was discharged and lived without symptoms of PH until her death due to systemic metastasis of carcinoma. In some cases of PTTM, imatinib may be an effective therapeutic option for PH.
Keywords: Gastric Cancer, Pulmonary Hypertension
Background
Pulmonary tumour thrombotic microangiopathy (PTTM) is a rare but fatal pulmonary complication of cancer, which was first described by von Herbay et al. The clinical presentation typically is acute dyspnoea, followed by a very rapid clinical course, progressing to death in a matter of hours to days.1 In fact, it has been reported that only 7 of 103 patients were pathologically diagnosed with PTTM while still alive.2
Platelet-derived growth factor (PDGF) stimulation has been reported to be involved in the proliferation and anti-apoptosis of pulmonary artery endothelial cells and smooth muscle cells in patients with pulmonary hypertension (PH).3–5 PDGF is also involved in the progression of PTTM.6 Several case reports from Japan have demonstrated that imatinib, a PDGF receptor–tyrosine kinase inhibitor, can improve severe PH in patients with PTTM. Here, we report a case of PTTM that was alleviated dramatically with imatinib therapy.
Case presentation
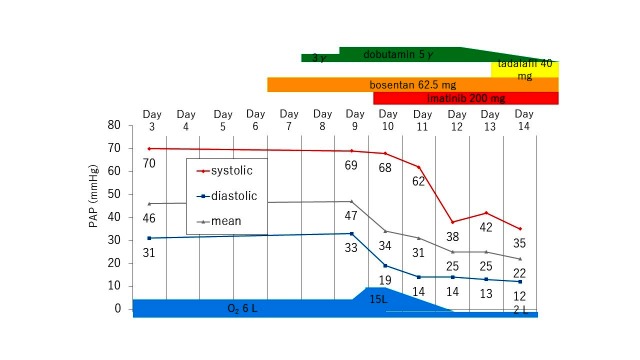
A 56-year-old woman had a 2-month history of oedema and exertional dyspnoea (WHO functional class II). She had no prior diseases or relevant family history. She was admitted to a nearby hospital where she was found to have severe PH. Figure 1 shows CT; it showed no thrombus in the pulmonary artery as well as no parenchymal lesion such as malignant tumour, lymphangitis carcinomatosa or interstitial pneumonia. However, enlargement of the para-aortic lymph nodes was found.
Figure 1.
CT on admission. (A) Mediastinal window image of lung field shows no thrombus in the pulmonary artery. (B) Lung window image shows no abnormality in the parenchymal parenchyma. (C,D) Mediastinal window image of abdomen shows enlargements of the para-aortic lymph nodes (yellow arrow).
Investigations
Right heart catheterisation showed significant PH (mean pulmonary arterial pressure (mPAP), 47 mm Hg). In Japan, the probability of Helicobacter pylori infection is high; it is known that gastric cancer is much more frequent than in Western countries. In this case, enlargement of the para-aortic lymph nodes was recognised, so we performed gastro-oesophageal endoscopy at an early stage. Gastric cancer was detected, pathologically diagnosed as poorly differentiated adenocarcinoma involving the signet-ring cells.
Treatment
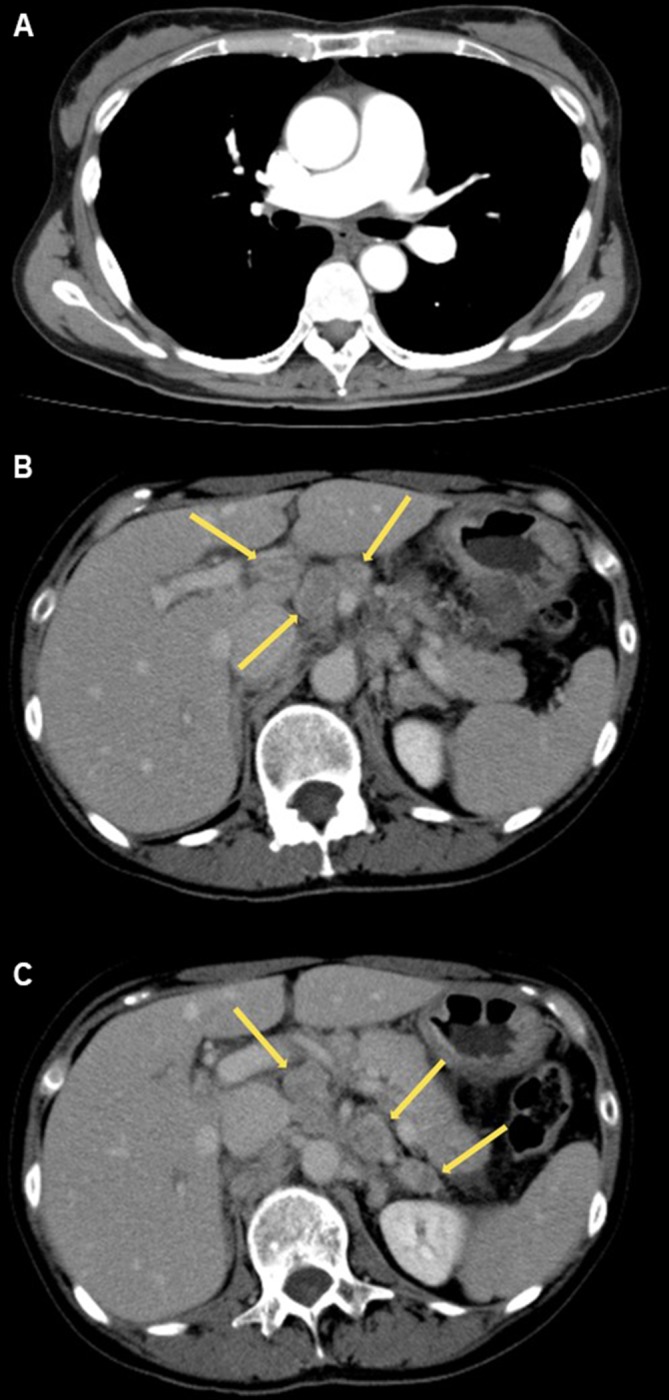
Figure 2 shows the clinical course, with PAP measured directly with a Swan-Ganz catheter indwelling from the right internal jugular vein. We started sequential oxygen, dobutamine and bosentan, but there was no improvement in her haemodynamics. Her respiratory condition deteriorated rapidly, and we diagnosed her as having PTTM based on her clinical course. After consulting Dr Hatano from The University of Tokyo, who reported a similar case of PTTM, we started treatment with imatinib (200 mg once daily) on day 10. Because imatinib therapy was off-label, we obtained urgent approval from the institutional ethics committee and received written informed consent from the patient.
Figure 2.
Clinical course. PAP, pulmonary arterial pressure; γ, μg/kg/min.
Outcome and follow-up
After administration of 200 mg imatinib, her PAP decreased dramatically. Five days later, her haemodynamics normalised (mPAP, 12 mm Hg) and her dyspnoea disappeared. Figure 3 shows her echocardiograms before and after imatinib administration. Although mild pericardial effusion remained, the prominent right heart dilatation showed obvious improvement.
Figure 3.
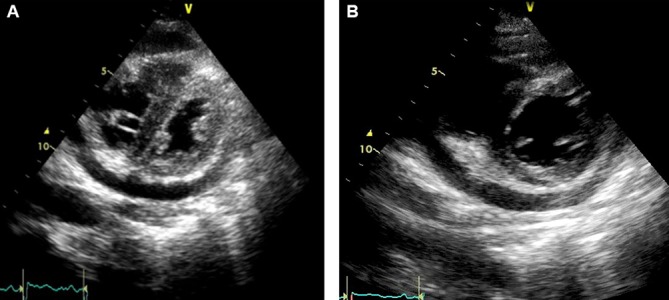
Short axis view echocardiograms. (A) On admission, the right ventricle was remarkably dilated, suggesting severe pulmonary hypertension (PH). (B) Three days after imatinib administration, there was obvious improvement of severe PH.
She was discharged and periodically visited our hospital for chemotherapy including titanium silicate-1 and oxaliplatin. She did not experience recurrence of PH, and died from systemic metastasis of carcinoma 7 months later.
Discussion
In our case, imatinib remarkably improved acute right heart failure due to PTTM associated with signet-ring cell carcinoma.
Imatinib is a tyrosine kinase inhibitor approved as an anticancer drug for chronic myelogenous leukaemia, Philadelphia chromosome-positive acute lymphoid leukaemia, KIT antibody-positive gastrointestinal stromal tumour and idiopathic hypereosinophilic syndrome. Imatinib inhibits phosphorylation of the BCR-ABL fusion protein, c-KIT protein and PDGF receptor, subsequently blocking many intracellular downstream signalling pathways. Dasatinib, another tyrosine kinase inhibitor, has recently been drawing attention as a cause of drug-induced pulmonary arterial hypertension (PAH), whereas imatinib has been reported to be effective in patients with PAH in a recent randomised study (IMPRES study). However, serious adverse events and study drug discontinuations were common.7 PTTM is thought to occur by obstruction of the pulmonary arterioles by microembolisms of tumour cells, thrombus formation induced by activation of thrombogenic cascades on the surface of tumour embolisms and abnormal proliferation of vascular cells caused by growth factors, such as PDGF and vascular endothelial growth factor, which are induced by tumours.6 8 9 In 2013, Ogawa et al reported the first case of PTTM with severe PH treated successfully with imatinib.6 However, few cases of PTTM treated with imatinib have been reported in Japan. We summarise the previous literature and our case in table 1.10–13 In this table, in patient 3, total gastrectomy was performed for mass reduction of the tumour, after which the patient’s mPAP decreased from 33 to 13 mm Hg. We also considered gastrectomy in our case, but the tumour mainly involved the para-aortic lymph nodes rather than the stomach itself. Therefore, we did not perform surgery, and it is noteworthy that her PAP improved promptly after administration of imatinib alone.
Table 1.
Summary of cases with PTTM treated with imatinib
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 (our case) |
|
| Age at onset, y | 47 | 61 | 64 | 61 | 45 | 56 |
| Sex | F | M | F | F | F | F |
| Author | Ogawa A | Higo K | Minatsuki S | Fukuda I | Fukuda I | Kubota K |
| Year of report | 2013 | 2014 | 2015 | 2015 | 2016 | 2017 |
| Primary disease | Gastric adenocarcinoma (signet-ring cells) | Colorectal cancer | Gastric adenocarcinoma (signet-ring cells) | Breast cancer | Breast cancer | Gastric adenocarcinoma (signet-ring cells) |
| Drugs administered | Imatinib 100 mg bosentan 93.75 mg epoprostenol 27 ng/kg/min | Imatinib 50→200 mg bosentan tadalafil | Imatinib 200 mg sildenafil 60 mg ambrisentan 10 mg | Imatinib 200→400 mg tadalafil 40 mg | Imatinib 200→400 mg | Imatinib 200 mg bosentan 62.5 mg tadalafil 40 mg |
| Mean PAP after administration of imatinib | 47→25 mm Hg | 48→35 mm Hg | 48→33 mm Hg | 60→56 mm Hg | 27→30 mm Hg | 47→22 mm Hg |
| Chemotherapy | TS-1 40 mg | Bevacizumab 5 mg/kg TS-1 100 mg |
TS-1 | Eribulin | Capecitabine | TS-1 oxaliplatin |
| Surgical therapy | (–) | (–) | Total gastrectomy | (–) | (–) | (–) |
| Survival time | 9 months | 12 months | 12 months | 54 days | 24 days | 7 months |
| Cause of death | Metastasis | Infection | Metastasis | Respiratory failure | Respiratory failure | Metastasis |
PAP, pulmonary arterial pressure; PTTM, pulmonary tumour thrombotic microangiopathy; TS, titanium silicate.
Imatinib can be particularly effective in patients with PTTM associated with signet-ring cell carcinoma. Fujishiro et al reported 103 patients with PTTM, among whom the most frequent primary cancer was gastric (58 cases), followed by lung (10 cases), breast (7 cases), cancer of unknown primary (f5 cases), ovarian (5 cases) and bladder (4 cases).2 As shown in table 1, imatinib was effective in three cases of signet-ring cell carcinoma, including our case, but was weaker in cases of colon (patient 2) and breast (patients 4 and 5) cancer. The mechanism is still unclear, but it has been suggested that production of growth factors, including PDGF, might be different depending on the tumour characteristics.
The limitation of this report is that there are few cases of PTTM treated with imatinib, which has not been adopted for PH. This is because PTTM progresses quickly and patients often die before drug administration. Therefore, further accumulation of cases is necessary.
In some cases, imatinib remarkably improves acute right heart failure caused by PTTM. Furthermore, imatinib can be highly effective in cases of PTTM caused by gastric adenocarcinoma, especially signet-ring cell carcinoma. Because patients with PTTM deteriorate rapidly, treatment with imatinib should be considered immediately.
Learning points.
Pulmonary tumour thrombotic microangiopathy (PTTM) is a rare haemodynamic complication of cancer, which can be lethal due to rapid progression of right heart failure caused by pulmonary hypertension.
In some cases, imatinib remarkably improves acute right heart failure caused by PTTM.
Because patients with PTTM deteriorate rapidly, treatment with imatinib should be considered immediately.
Footnotes
Contributors: KK and TS were physicians in charge and wrote the manuscript. YI gave precise advice on medical treatment and refined the manuscript. KK supervised the aforementioned staffs and had responsibility for this case report.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: Because imatinib therapy was off-label, we obtained urgent approval from the institutional ethics committee and received written informed consent from the patient for therapy itself as well as publication. The consent form written in Japanese is attached as PDF files.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.von Herbay A, Illes A, Waldherr R, et al. . Pulmonary tumor thrombotic microangiopathy with pulmonary hypertension. Cancer 1990;66:587–92. [DOI] [PubMed] [Google Scholar]
- 2.Fujishiro T, Shuto K, Shiratori T, et al. . A case report of pulmonary tumor thrombotic microangiopathy (PTTM) caused by esophageal squamous cell carcinoma. Esophagus 2013;10:247–51. 10.1007/s10388-013-0382-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogawa A, Nakamura K, Matsubara H, et al. . Prednisolone inhibits proliferation of cultured pulmonary artery smooth muscle cells of patients with idiopathic pulmonary arterial hypertension. Circulation 2005;112:1806–12. 10.1161/CIRCULATIONAHA.105.536169 [DOI] [PubMed] [Google Scholar]
- 4.Fujio H, Nakamura K, Matsubara H, et al. . Carvedilol inhibits proliferation of cultured pulmonary artery smooth muscle cells of patients with idiopathic pulmonary arterial hypertension. J Cardiovasc Pharmacol 2006;47:250–5. 10.1097/01.fjc.0000201359.58174.c8 [DOI] [PubMed] [Google Scholar]
- 5.Ikeda T, Nakamura K, Akagi S, et al. . Inhibitory effects of simvastatin on platelet-derived growth factor signaling in pulmonary artery smooth muscle cells from patients with idiopathic pulmonary arterial hypertension. J Cardiovasc Pharmacol 2010;55:39–48. 10.1097/FJC.0b013e3181c0419c [DOI] [PubMed] [Google Scholar]
- 6.Ogawa A, Yamadori I, Matsubara O, et al. . Pulmonary tumor thrombotic microangiopathy with circulatory failure treated with imatinib. Intern Med 2013;52:1927–30. 10.2169/internalmedicine.52.0718 [DOI] [PubMed] [Google Scholar]
- 7.Hoeper MM, Barst RJ, Bourge RC, et al. . Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: results of the randomized IMPRES study. Circulation 2013;127:1128–38. 10.1161/CIRCULATIONAHA.112.000765 [DOI] [PubMed] [Google Scholar]
- 8.Kim R, Emi M, Arihiro K, et al. . Chemosensitization by STI571 targeting the platelet-derived growth factor/platelet-derived growth factor receptor-signaling pathway in the tumor progression and angiogenesis of gastric carcinoma. Cancer 2005;103:1800–9. 10.1002/cncr.20973 [DOI] [PubMed] [Google Scholar]
- 9.Yokomine T, Hirakawa H, Ozawa E, et al. . Pulmonary thrombotic microangiopathy caused by gastric carcinoma. J Clin Pathol 2010;63:367–9. 10.1136/jcp.2010.075739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minatsuki S, Miura I, Yao A, et al. . Platelet-derived growth factor receptor-tyrosine kinase inhibitor, imatinib, is effective for treating pulmonary hypertension induced by pulmonary tumor thrombotic microangiopathy. Int Heart J 2015;56:245–8. 10.1536/ihj.14-220 [DOI] [PubMed] [Google Scholar]
- 11.Higo K, Kubota K, Takeda A, et al. . Successful antemortem diagnosis and treatment of pulmonary tumor thrombotic microangiopathy. Intern Med 2014;53:2595–9. 10.2169/internalmedicine.53.2379 [DOI] [PubMed] [Google Scholar]
- 12.Fukada I, Araki K, Minatsuki S, et al. . Imatinib alleviated pulmonary hypertension caused by pulmonary tumor thrombotic microangiopathy in a patient with metastatic breast cancer. Clin Breast Cancer 2015;15:e167–e170. 10.1016/j.clbc.2014.10.008 [DOI] [PubMed] [Google Scholar]
- 13.Fukada I, Araki K, Kobayashi K, et al. . Imatinib could be a new strategy for pulmonary hypertension caused by pulmonary tumor thrombotic microangiopathy in metastatic breast cancer. Springerplus 2016;5:1582 10.1186/s40064-016-3280-4 [DOI] [PMC free article] [PubMed] [Google Scholar]