Description
A previously healthy, 38-year-old man presented with non-pruritic rash over his legs and trunk noticed 2 hours back. Examination revealed non-palpable purpura over the limbs and trunk. There was multiple ‘wet purpura’ over the buccal mucosa, palate and tongue (figure 1A). He had mild pallor and direct ophthalmoscopy showed bilateral fundal haemorrhage with sparing of macula. There was no organomegaly or palpable lymphadenopathy. His investigation showed haemoglobin 125 g/L, white blood cell 8.7×109/L, platelet 7×109/L and normal peripheral smear. He was treated with intravenous methylprednisolone (1 g once a day x3 days) and received one single donor platelet (SDP) transfusion. His bone marrow aspirates showed increased megakaryocytes and no atypical cells or excess of blast; overall picture was consistent with immune thrombocytopenia (ITP). His platelet count on day +3 was 55×109/L. He was put on oral prednisolone (1 mg/kg/day). On day +7, he was asymptomatic with no evidence of any mucocutaneous bleed (figure 1B). He was off therapy from day +28 with platelet of 178×109/L.
Figure 1.
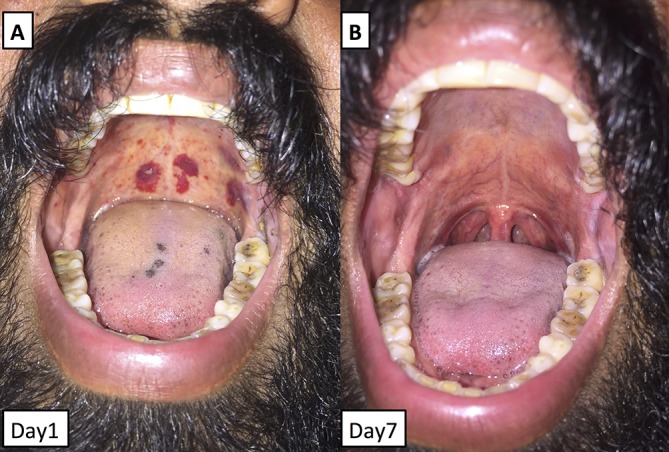
(A) Clinical photograph showing multiple blood-filled blisters (wet purpura) over the soft palate, tongue and buccal mucosa on day 1. (B) On day 7, complete resolution of wet purpura can be appreciated.
Thrombocytopenia (platelets <150×109/L) is usually caused by drug, infection, autoimmune diseases and malignancy involving bone marrow. ITP is diagnosed by excluding other causes of thrombocytopenia.1 Therapy is warranted if there is ongoing bleeding, eminent bleeding (wet purpura), severe thrombocytopenia (platelet <30×109/L) or a need for invasive or surgical procedure.2 First-line treatment is immunosuppression (steroid with or without immunoglobulins). Wet purpura is blood-filled vesicles seen over the buccal mucosa, palate, tonsillar fossa or lips.3 When clinically picked, it represents eminent bleeding and demands urgent therapeutic intervention giving a gratifying result. However, if missed or ignored, a catastrophe can strike at any point of time.
Learning points.
Wet purpura is blood-filled blisters over the mucosal surface representing eminent bleeding in patients with thrombocytopenia.
Presence of wet purpura in patients with thrombocytopenia demands aggressive therapeutic intervention.
Early and appropriate therapy gives a gratifying result.
Footnotes
Contributors: KM, AJ, PM and NV were involved in the management of the case. The manuscript was prepared by KM and AJ, which was vetted by all.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.George JN, Definition GJN. Definition, diagnosis and treatment of immune thrombocytopenic purpura. Haematologica 2009;94:759–62. 10.3324/haematol.2009.007674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood 2011;117:4190–207. 10.1182/blood-2010-08-302984 [DOI] [PubMed] [Google Scholar]
- 3.Crosby WH. Wet purpura, dry purpura. JAMA 1975;232:744–5. 10.1001/jama.1975.03250070040025 [DOI] [PubMed] [Google Scholar]


