Abstract
Intracranial infections may result from contiguity, such as mastoiditis or acute otitis media, or from haematogenous dissemination from an infectious source. Streptococcus constellatus, a coccus from the normal genital, oral and gastrointestinal flora, has a tendency to form abscesses, but not to cause infective endocarditis (IE). Also, S. constellatus is an extremely rare causative agent of brain abscess. We report the case of a woman with a colorectal tumour who presented with IE and cerebellar abscesses due to a S. constellatus bacteraemia.
Keywords: General Practice / Family Medicine, Infectious Diseases
Background
A brain abscess may result from other infections, such as acute otitis media, periodontitis and upper respiratory tract infections. The clinical presentation is determined by the size, the location of the abscess and the acute or subacute onset.1 Although one of the features of the Streptococcus anginosus group is the tendency to develop abscesses,2 members of this group are rarely involved in the development of intracranial abscesses, and they are also unlikely pathogens of infective endocarditis (IE).3–5 However, Streptococcus constellatus may become an opportunistic cause of both IE and brain abscess in certain underlying conditions, such as diabetes, immunosuppression and malignancy.2 Regarding the presence of tumours, they may lead to the rupture of the mucosal barrier and allow the haematogenous spread of the aforementioned pathogens.
Case presentation
A 69-year-old woman was admitted to our hospital after an accidental fall. She reported lying on the floor for several hours until her sister found her and stated that she did not lose consciousness at any time. At the hospital, she told the clinicians she had lost weight unintentionally, about 10 kg over the last year. She had also lost her appetite and had constipation. The patient described a loss of sensitivity in the left side of her face. She was obese and had hypertension, and was on losartan 50 mg daily. She did not have any prior underlying heart disease.
On physical examination, her temperature was 36.4°C, heart rate was 74 bpm and blood pressure was 125/78 mm Hg. The patient had good oral hygiene. The clinicians found she had left-sided facial hypoesthesia. Mental status, cranial nerves, motor system and reflexes were normal. In terms of cerebellar testing, the patient showed a lack of balance and a wide-based gait, and the Romberg test was positive. The patient’s balance was impaired, as she veered to the left, and she even fell to the left with her eyes closed. Clinicians found an ataxic gait, as the patient showed an unbalanced, uncoordinated gait. She presented with staggering to keep her balance, truncal instability and impaired tandem walking. No dysarthria was found, and she had no problems with fine movements such as picking up small objects or buttoning clothes. No dysmetria, nystagmus or tremor of dysdiadochokinesis were found.
On auscultation, breath sounds were normal, but a systolic murmur was identified, which had not been previously described.
Blood tests revealed a white cell count of 18 x109/L, with 92% neutrophils, a haemoglobin level of 16.2 g/dL and a platelet count of 261 x109/L, and a C-reactive protein level of 161 mg/dL (normal range: <5 mg/dL). Liver and kidney functions were normal.
The patient was not stuporous, and no lumbar puncture was performed. However, she had a temperature of 38.4°C while in the emergency medicine department, and samples for blood cultures were therefore drawn.
Differential diagnosis
The patient showed a subacute neurological disorder, mainly abnormal gait, which was deemed to be the cause of the accidental fall. We then decided to perform neuroimaging techniques. A brain CT scan was suggestive of an acute ischaemic infarction in the left cerebellar hemisphere, but we decided to perform an MRI to confirm and better characterise the findings. It revealed two cerebellar lesions: one in the left middle cerebellar peduncle (1.8 cm in size) and one in the left lateral hemisphere (3.5 cm in size). Both lesions were hypointense in T1, hyperintense in T2 and were surrounded by vasogenic oedema (figure 1). These findings were consistent with cerebellar abscesses. The differential diagnosis of a brain or cerebellar abscess includes infarction, haemorrhage and brain injury, but primary and metastatic tumours should also be ruled out. Other infectious conditions include focal encephalitis, mycotic aneurysm, and opportunistic and parasitic infections, such as cryptococcosis, toxoplasmosis and cysticercosis. However, the sensitivity of the MRI allowed us to characterise the radiological features as typical of pyogenic abscesses.
Figure 1.
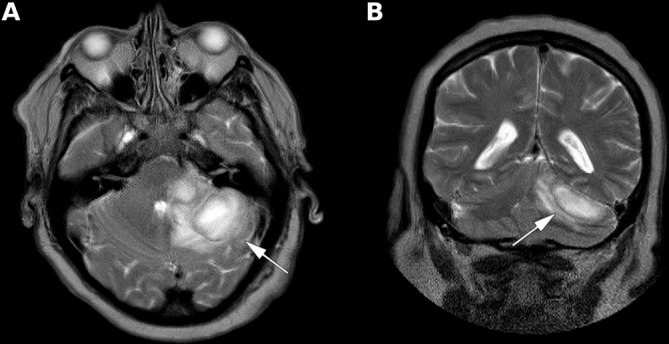
Slides of the brain MRI show two cerebellar lesions (arrows): one in the left middle cerebellar peduncle (1.8 cm in size) and one in the left lateral hemisphere (3.5 cm in size). Both lesions were hypointense in T1 (not shown), hyperintense in T2 and were surrounded by vasogenic oedema. (A) Transversal plane. (B) Coronal plane.
Both CT and MRI demonstrate similar radiological features, although MRI has a greater ability to distinguish a cerebral abscess from other ring-enhancing lesions. Apparent diffusion coefficient is typically low in abscesses but high in tumours. T2/FLAIR (T2-weighted-Fluid-Attenuated Inversion Recovery) shows central high intensity (hypointense to cerebrospinal fluid, and does not attenuate on FLAIR). Finally, the enhancing rims of pyogenic abscesses demonstrated cerebral blood volume is significantly lower than that of metastases.6
The ensuing differential diagnosis included some risk factors for haematogenous spread, such as septic cerebral emboli during IE, lung infections, systemic sepsis or right-to-left shunt. Infections that may also spread by contiguity include mastoiditis, acute otitis media, odontogenic abscess, periodontitis and sinusitis.
Outcome and follow-up
We decided to initiate ceftriaxone 2 g twice a day and metronidazole 500 mg every 8 hours. Given the suspicion of a possible haematogenous dissemination, an echocardiogram was performed, which was positive for native valve IE, with a vegetation on the mitral valve.
Blood cultures revealed S. constellatus, sensitive to clindamycin, levofloxacin, linezolid, vancomycin, ampicillin and ceftriaxone. The antibiotic therapy was changed to ceftriaxone 2 g every 12 hours and intravenous gentamicin 240 mg daily.
The subacute medical condition, that is, weight loss, fatigue, malaise, constipation and bacteraemia, raised the suspicion of a gastrointestinal origin. The abdominal CT revealed a pelvic mass measuring 8×6 cm (no images available). A colonoscopy was then performed, which revealed a rectal mass located 18 cm above the dental line (figure 2), which had an uneven, haemorrhagic surface, causing partial obstruction of the lumen. Biopsies revealed a poorly differentiated (high-grade) colorectal adenocarcinoma.
Figure 2.
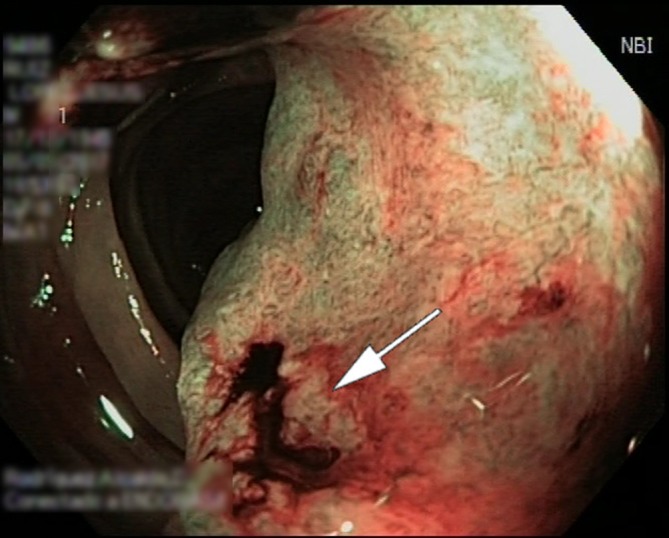
Lumen of the sigmoid colon was partially obstructed by a rectal mass located 18 cm above the dental line, and its surface was uneven and haemorrhagic (arrow).
While in the hospitalisation ward, 24 hours after this diagnosis, the patient’s condition became suddenly worse, with dyspnoea, chest pain, severe hypotension, tachycardia and oxygen saturation levels below 90%. A chest CT scan revealed a massive pulmonary embolism, and the patient passed away a few hours later while in the intensive care unit.
The risk of venous thromboembolism increases in patients with malignancy.7 Also, acute infections are associated with an increased risk of venous thromboembolic events.8 Autopsy was not performed, but our hypothesis was that both malignancy and acute infection were precipitants for venous thromboembolism and suggest a causal relation.
Discussion
The main educational message of the current manuscript is that S. anginosus group streptococci are the causative pathogens of several clinical syndromes, but due to their relationship with different underlying conditions such as immunosuppression or malignancy, the source of the infection should be identified. We would like to give special significance to the likelihood of forming abscesses, and thus we would like to emphasise the importance of an appropriate workup in the diagnosis of either occult abscesses or infection due to a bacteraemia caused by these pathogens.
When IE is diagnosed, the brain is the first organ involved due to septic emboli from an existing vegetation on a heart valve.9 Neurological symptoms are mild, and the clinical presentation is sometimes paucisymptomatic.10 A recent literature review9 showed that MRI is more sensitive than the CT scan in assessing brain involvement when an IE is diagnosed, as most lesions can go undetected in brain CT scans.
Intracranial bacterial infections are life-threatening conditions that usually require prompt management. Brain abscesses may result from the bacterial dissemination from a distant source, such as IE or bacteraemia. However, they can sometimes occur from adjacent foci, such as periodontitis or oral surgery, or due to acute otitis media or mastoiditis. Nevertheless, intracranial infections are dependent on underlying conditions, such as severe immunodeficiency.1
The haematogenous dissemination is usually associated with IE, lung diseases or other sources of infections. In our patient, the IE was deemed to be the source of the cerebellar abscesses.
Symptoms related to subacute intracranial infections may be difficult to identify since brain abscesses have a wide range of clinical manifestations, and symptoms may be subtle, as they depend on the site of the abscess and the time of development. Therefore, patients may present with symptoms related to the underlying infection. Seizures, behavioural changes and headache are frequent symptoms. However, when the cerebellum or brain stem are involved, cranial-nerve palsy and gait disorder are the most evident symptoms.1
Surgical approach on cerebellar abscesses, either for diagnostic or decompression purposes, depends on the patient’s clinical condition. In cases of small abscesses or deep brain locations, drainage is not recommended.1 In such situations, empirical antibiotic therapy and follow-up neuroimaging would be justified, and this was the management approach we took.
S. constellatus is a gram-positive round-shaped coccus that belongs to the Streptococcus anginosus group (formerly known as S. milleri group), along with S. anginosus and S. intermedius.11 It is part of the normal urogenital, oral and gastrointestinal flora, but in certain conditions, that is, malnourished, immunosuppressed patients, diabetes or malignancy, it may cause pyogenic infections as an opportunistic pathogen.2 Although the most striking feature of the Streptococcus anginosus group (SAG) is the abscess formation, not all the members (S. constellatus, S. intermedius and S. anginosus) have the same frequency in forming abscesses, and S. constellatus is the most likely pathogen to cause such infections.2
S. intermedius and S. constellatus are more associated with abscesses, but S. constellatus also causes a wider range of infections, including odontogenic disease, abdominal abscesses and respiratory tract infections.2 S. anginosus is the most frequent isolated species in bacteraemia (82%), while S. constellatus is detected infrequently in the blood (11%), and S. intermedius only 6%.11
However, IE caused by members of the SAG group is rare.3–5 Although S. intermedius and S. constellatus are more associated with abscesses, those caused by S. constellatus are more superficial.2 SAG streptococci are the most common pathogens associated with bacterial brain abscesses,12 but S. intermedius has been strongly associated with them.2 13
A high frequency of underlying conditions seems to characterise S. anginosus group infections. Between 56% and 77% of the patients in several studies had at least one comorbidity or a risk factor,11 14 15 and patients presenting with bacteraemia may have an underlying comorbidity, including hepatic and biliary disease, neoplasia and diabetes. It can also result from a disruption of the mucosal digestive barrier acting as a portal of entry.14 15
Our hypothesis was that the source of the infection was the underlying disease, that is, the colorectal tumour, as it ruptured the mucosal barrier. The haematogenous spread allowed the cocci to settle in the heart valve and develop a vegetation on it. Bacterial fragmentation of the vegetation was the most likely source of the cerebellar abscesses. The paucisymptomatic presentation might be justified by the subacute onset of the abscess. We considered such a scenario is theoretically plausible.
Nevertheless, a brain abscess caused by S. constellatus is very rare.16 17 Regarding the cerebral emboli, infective endocarditis was considered since this condition has been found to be associated with a significant proportion of patients with S. anginosus bacteraemia,15 although it is more common in viridans streptococci bacteraemia.18 A study of infective endocarditis caused by S. milleri group organisms found that 25% of the cases had extracardiac suppurative foci of infection.19
Learning points.
Cerebellar abscesses are much rarer than abscesses in other locations of the central nervous system.
S. constellatus and the other members of the Streptococcus anginosus group (SAG) are associated with different clinical syndromes, but the source of the infection must be identified.
Given the likelihood of forming abscesses, bacteraemia by these pathogens should lead the clinicians to identify an occult abscess.
Infective endocarditis by SAG cocci should lead the clinicians to an appropriate workup to identify any underlying conditions, such as immunosuppression or malignancy.
We would like to highlight the importance of an appropriate workup in the diagnosis of an uncommon intracranial infection due to a bacteraemia caused by an uncommon pathogen.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Brouwer MC, Tunkel AR, McKhann GM, et al. . Brain abscess. N Engl J Med 2014;371:447–56. 10.1056/NEJMra1301635 [DOI] [PubMed] [Google Scholar]
- 2.Claridge JE, Attorri S, Musher DM, et al. . Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Clin Infect Dis 2001;32:1511–5. 10.1086/320163 [DOI] [PubMed] [Google Scholar]
- 3.Concistre G, Chiaramonti F, Miceli A, et al. . Mitral and aortic valve endocarditis caused by a rare pathogen: Streptococcus constellatus. Interact Cardiovasc Thorac Surg 2012;14:889–90. 10.1093/icvts/ivs032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willcox MD. Potential pathogenic properties of members of the "Streptococcus milleri" group in relation to the production of endocarditis and abscesses. J Med Microbiol 1995;43:405–10. 10.1099/00222615-43-6-405 [DOI] [PubMed] [Google Scholar]
- 5.Yoshino Y, Kimura Y, Sakai T, et al. . Infective endocarditis due to a rare pathogen, Streptococcus constellatus, in a patient with gingivitis: a case report and review of the literature. Open Med 2013;8:489–92. 10.2478/s11536-013-0167-4 [DOI] [Google Scholar]
- 6.Toh CH, Wei K-C, Chang C-N, et al. . Differentiation of brain abscesses from glioblastomas and metastatic brain tumors: comparisons of diagnostic performance of dynamic susceptibility contrast-enhanced perfusion MR imaging before and after mathematic contrast leakage correction Sherman J, PLoS ONE. 9 San Francisco, USA: Public Library of Science, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JE, Kim HR, Lee SM, et al. . Clinical characteristics of pulmonary embolism with underlying malignancy. Korean J Intern Med 2010;25:66–70. 10.3904/kjim.2010.25.1.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smeeth L, Cook C, Thomas S, et al. . Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet 2006;367:1075–9. 10.1016/S0140-6736(06)68474-2 [DOI] [PubMed] [Google Scholar]
- 9.Champey J, Pavese P, Bouvaist H, et al. . Value of brain MRI in infective endocarditis: a narrative literature review. Eur J Clin Microbiol Infect Dis 2016;35:159–68. 10.1007/s10096-015-2523-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoen B, Duval X, Endocarditis I. New England Journal of Medicine. Massachusetts Medical Society 2013;368:1425–33. [DOI] [PubMed] [Google Scholar]
- 11.Siegman-Igra Y, Azmon Y, Schwartz D. Milleri group streptococcus—a stepchild in the viridans family. Eur J Clin Microbiol Infect Dis 2012;31:2453–9. 10.1007/s10096-012-1589-7 [DOI] [PubMed] [Google Scholar]
- 12.Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis 2007;26:1–11. 10.1007/s10096-006-0236-6 [DOI] [PubMed] [Google Scholar]
- 13.Whiley RA, Beighton D, Winstanley TG, et al. . Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol 1992;30:243–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bert F, Bariou-Lancelin M, Lambert-Zechovsky N. Clinical significance of bacteremia involving the "Streptococcus milleri" group: 51 cases and review. Clin Infect Dis 1998;27:385–7. 10.1086/514658 [DOI] [PubMed] [Google Scholar]
- 15.Casariego E, Rodriguez A, Corredoira JC, et al. . Prospective study of Streptococcus milleri bacteremia. Eur J Clin Microbiol Infect Dis 1996;15:194–200. 10.1007/BF01591353 [DOI] [PubMed] [Google Scholar]
- 16.Göbels K, Teichmann D, Grobusch MP, et al. . A case of multiple brain abscesses due to Streptococcus constellatus. Eur J Clin Microbiol Infect Dis 2002;21:156–7. 10.1007/s100960100625 [DOI] [PubMed] [Google Scholar]
- 17.Şenol Ö, Süslü HT, Tatarlı N, et al. . Thalamic abscess caused by a rare pathogen: Streptococcus constellatus. Pan Afr Med J 2016;24:256 10.11604/pamj.2016.24.256.9468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salavert M, Gómez L, Rodriguez-Carballeira M, et al. . Seven-year review of bacteremia caused by Streptococcus milleri and other viridans streptococci. Eur J Clin Microbiol Infect Dis 1996;15:365–71. 10.1007/BF01690091 [DOI] [PubMed] [Google Scholar]
- 19.Lefort A, Lortholary O, Casassus P, et al. . Beta-Hemolytic Streptococci Infective Endocarditis Study Group. Comparison between adult endocarditis due to beta-hemolytic streptococci (serogroups A, B, C, and G) and Streptococcus milleri: a multicenter study in France. Arch Intern Med 2002;162:2450–6. 10.1001/archinte.162.21.2450 [DOI] [PubMed] [Google Scholar]


