Abstract
Aims
The aims were to (1) estimate the prevalence of alcohol and drug use disorders in prisoners on reception to prison and (2) estimate and test sources of between study heterogeneity.
Methods
Studies reporting the 12‐month prevalence of alcohol and drug use disorders in prisoners on reception to prison from 1 January 1966 to 11 August 2015 were identified from seven bibliographic indexes. Primary studies involving clinical interviews or validated instruments leading to DSM or ICD diagnoses were included; self‐report surveys and investigations that assessed individuals more than 3 months after arrival to prison were not. Random‐effects meta‐analysis and subgroup and meta‐regression analyses were conducted. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines were followed.
Results
In total, 24 studies with a total of 18 388 prisoners across 10 countries were identified. The random‐effects pooled prevalence estimate of alcohol use disorder was 24% [95% confidence interval (CI) = 21–27], with very high heterogeneity (I 2 = 94%). These ranged from 16 to 51% in male and 10–30% in female prisoners. For drug use disorders, there was evidence of heterogeneity by sex, and the pooled prevalence estimate in male prisoners was 30% (95% CI = 22–38; I 2 = 98%; 13 studies; range 10–61%) and, in female prisoners, was 51% (95% CI = 43–58; I 2 = 95%; 10 studies; range 30–69%). On meta‐regression, sources of heterogeneity included higher prevalence of drug use disorders in women, increasing rates of drug use disorders in recent decades, and participation rate.
Conclusions
Substance use disorders are highly prevalent in prisoners. Approximately a quarter of newly incarcerated prisoners of both sexes had an alcohol use disorder, and the prevalence of a drug use disorder was at least as high in men, and higher in women.
Introduction
Prisons around the world detain large numbers of individuals with substance use problems, which increase the risk of mortality after prison release 1, 2, 3 and repeat offending 4, 5. In addition, alcohol use disorders (AUD) are associated with suicide inside prison 6 and of perpetrating violence and being victimized inside custody 7, 8.
The treatment gap for substance use disorders (SUD) inside prison has been reported in many studies 9, 10. Estimates of the prevalence of these disorders in prisoners can assist in planning service provision effectively, targeting scarce resources and developing and evaluating initiatives to reduce the gap between health needs and interventions. A previous systematic review reported ranges for drug abuse and dependence of 10–48% in men and 30–60% in women on reception or arrival to prison. For alcohol abuse and dependence, ranges of 18–30% for men and 10–24% for women were reported 11. There were very high rates of heterogeneity between these included studies (with I 2 values of more than 80%), which were investigated in subgroup analyses. Lower prevalences were associated with studies where psychiatrists acted as interviewers and higher prevalences for drug use disorders in remand prisoners. However, this review is now dated, with its search for primary studies ending in 2004, and a number of relevant investigations have been published subsequently. In addition, subgroup analyses were the limited number of primary studies by sex, and an updated review will allow for further investigation of sources of between‐study variation.
The aim of the current paper is to provide an update of prevalence estimates of alcohol and drug use disorders in prisoners and estimate sources of between‐study heterogeneity. As part of this, we have used the term ‘substance use disorder’, which does not distinguish between ‘abuse’ and ‘dependence’. In this update, we have also conducted meta‐analyses to report pooled prevalence estimates and meta‐regression to examine sources of variation between included studies.
Methods
Search strategy
We identified surveys of alcohol and drug use disorder in general prison populations (defined as remand/detainee and/or sentenced prisoners who are sampled from the whole population of a correctional institution) published between January 1966 and August 2015. For the period January 1966 and January 2004, methods have been described in a previous systematic review conducted by one of the authors (S.F.) 11. For this update, we searched the following databases from 1 January 2004 to 11 August 2015: PsycINFO, MEDLINE, Global Health, PubMed, CINAHL, National Criminal Justice Reference Service and EMBASE. We used a combination of search terms relating to substance use disorder (i.e. substance*, alcohol, drug*, misuse, dependen*, abuse) and prisoners (i.e. inmate*, sentenced, remand, detainee*, felon*, prison*, incarcerat*), which are same search terms used in the previous review except for the addition of ‘incarcerat*’. Additional targeted searches covered relevant reference lists, and non‐English papers were translated. We corresponded with authors to clarify data when necessary. We followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines 12 (Supporting information, Appendix S1) and registered the protocol for this review with PROSPERO (registration code CRD42016036416) 13.
Study eligibility
Inclusion criteria were studies: (a) reporting diagnoses of substance use disorder (i.e. substance abuse and/or dependence) based on clinical examination or by interviews using validated diagnostic instruments [based on DSM (versions III to IV‐R; codes 303.90, 304.00–90, 305.00–90, excluding nicotine‐related disorders) and ICD versions 9 and 10 (ICD‐9: 303–305; ICD‐10 codes: F10–19.1‐2 except F17)]; (b) with diagnoses based on the previous 12 months from the time when participants were interviewed/examined; and (c) that sampled the general prison population within 3 months of arrival to prison. We excluded studies that selected subgroups for interview (e.g. prisoners referred for treatment, specific categories of offenders), as the aim was to provide a prevalence estimate for the whole prison population 14, 15, 16. After correspondence with authors, if studies reported combined prevalence for alcohol and drug 17, 18 or combined male and female prevalence, these were excluded 19, as we aimed to report estimates separately by sex and by drug and alcohol use disorder. Studies that reported specific drugs 20, 21, self‐screening measures 22, 23 or solely life‐time prevalence were also excluded 24.
Publications in any language were included in the search: studies from low‐ and middle‐income (LMI) countries were reported separately, given high heterogeneity 25, 26. Similarly, studies with juvenile/youth prisoners were analysed separately 27, 28, 29, 30, 31.
Data extraction and analysis
Two researchers (I.Y. and A.H.) extracted independently information on year of publication, geographical location, total sample, sex, prisoner status (remand/sentenced), average age, method of sampling, sample size, participation rate, type of interviewer, diagnostic instrument, diagnostic criteria (ICD versus DSM) and number diagnosed with substance use disorders. If older studies reported dependence prevalence, this was prioritized over abuse, as we considered that these had higher diagnostic validity 32, 33 (except when only combined prevalence for abuse and dependence was available). Eligible studies were assessed for quality using the JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data, which uses nine criteria including sample size, sampling, sample description, appropriate statistical analysis and response rates (Supporting information, Appendix S2) 34.
We conducted a random‐effects analysis, which assigns similar weights to all studies included in the meta‐analysis regardless of sample size 35. If there were high levels of overall heterogeneity (I 2 > 75%), we also reported estimate ranges as an alternative. Meta‐regression analysis was performed to examine sources of between‐study heterogeneity on a range of study pre‐specified characteristics [i.e. sex, age, publication year, country (United States versus other countries), prisoner status (sentenced versus remand/detainee/unsentenced), participation rate, sample size, diagnostic criteria (ICD versus DSM) and psychiatric interviewer]. Univariable analysis was conducted for both dichotomous and continuous definitions of a variable (e.g. publication year: continuous versus before or after 2000). Multivariable analyses were not conducted due to the limited number of primary studies. If there were fewer than 10 studies that reported an explanatory variable, it was excluded from the meta‐regression 36. Selected continuous variables (study year and proportion sentenced) were converted to dichotomous variables for reporting of pooled prevalence estimates of subgroups. Accordingly, in the meta‐regression, studies that combined both remand and sentenced prisoners were excluded if: (1) prisoner type comprised more than 10% of the total study participants or was unspecified and (2) separate prevalence data were not provided for each type 37, 38, 39, 40, 41, 42.
In addition, pooled prevalence estimates of the subgroups that did not have more than one study in each relevant category were not reported, even if they had significant results on meta‐regression. Further, we conducted subgroup analyses stratified on pre‐specified variables based on our previous review—sex, whether or not the country of origin was United States, remand/detainee versus sentenced prisoner status and whether or not the assessment was conducted by a psychiatrist. We added a new subgroup analysis based on the date of publication (2000, which was approximately the median date). To test for publication bias, funnel plot analysis and Egger's test were conducted on all studies stratified by disorder (i.e. AUD and SUD) and also by sex and disorder 43. Thus, six separate Egger's tests were performed. Studies with juvenile prisoners or LMI countries were not included, as they were clinically heterogeneous and limited in number. The Egger test quantifies bias captured in the funnel plot analysis with linear regression using the value of effect sizes and their precision [standard error (SE)] and assumes that the quality of study conduct is independent of study size 35 All analyses were conducted in Stata (STATA‐IC) version 14 using the following commands: metan (for random‐effects meta‐analysis), metareg (for meta‐regression), metabias (for publication bias analysis) and heterogi (for calculation of confidence intervals for heterogeneity level).
Results
Study characteristics
We identified 24 publications for the main analysis (Fig. 1), 13 of which were from the previous review 37, 38, 39, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, and 11 new studies from 2004 40, 41, 42, 54, 55, 56, 57, 58, 59, 60, 61. Two additional studies in LMI countries (Chile 26 and Brazil 25) and five studies on juvenile prisoners (mean age = 16.7 years) were examined separately (Supporting information, Appendix S3) 27, 28, 29, 30, 31.
Figure 1.
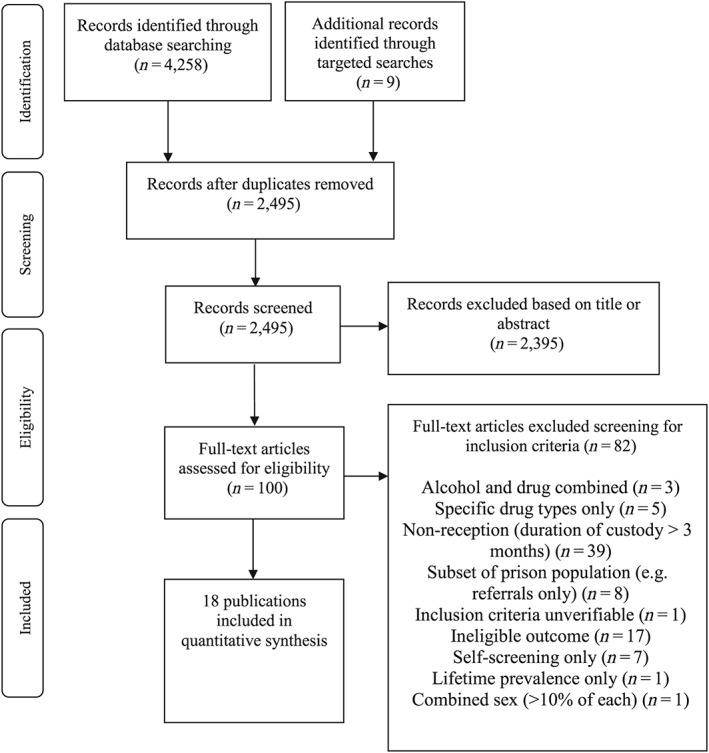
Flow diagram of search strategy for update (2004–15)
Studies in the main analysis were from 10 different countries (Australia 40, Austria 61, England 48, France 42, Germany 56, Iceland 60, Ireland 39, 41, 51, 55, the Netherlands 57, New Zealand 37 and United States 38, 44, 45, 46, 47, 49, 50, 52, 54, 59), with 40.5% (7456 prisoners) of the adult combined sample from the United States. Participants were 18 388 prisoners, both sentenced and remand/detainee, 64% of whom were male. The mean age was 30.2 years (range = 17–67 years). Of the 5835 prisoners with criminal history information reported, 924 prisoners (15.8%) were charged or convicted with a violent offence. There were more sentenced (11 065; 60.2%) than remand/detainee/unsentenced prisoners (2975; 16.2%), and 11 investigations included both sentenced and remand prisoners (4348; 23.6%) (‘mixed’ studies) 38, 39, 40, 42, 51, 55, 56, 57. Apart from two studies based on clinical interviews 48, 51, the others involved trained interviewers using validated, structured diagnostic instruments (Table 1 for details). Prevalence of drug use disorder were based on all drugs excluding alcohol and tobacco (i.e. cannabis, opioids, cocaine, amphetamine, hallucinogens, inhalants, other stimulants and tranquillizers). The individual prevalence estimates of substance use disorders are summarized in Table 2. In terms of quality of the included studies, we determined that nine of 24 studies were of high quality, as they met all nine criteria in the quality checklist, including a sufficient sample size (> 250), low refusal rate (< 20%) and detailed description of study subjects and setting 38, 41, 42, 44, 46, 49, 53, 54, 59 (see Supporting information, Appendix S2 for full criteria).
Table 1.
Study characteristics of newly included studies of substance use disorder in prisoners on arrival into custody (by study year).
| Study | Country | Population | Sampling strategy | Sampling method | Instrument criteria | Diagnostic criteria | Mean age (years) | Age range | Psychiatric interviewera | Mean duration in prison | Type of prisoner | % male | No. committed violent offences | No. not consenting |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Collins 1988 | USA | North Carolina prisons | All males admitted March–June 1983 | Consecutive new arrivals at reception | DISb | DSM‐IIIc | 27.6 | Not reported | N | Not reported | Sentenced | 100% | 157 | 117 |
| Daniel 1988 | USA | Missouri Correctional Classification Center | Consecutive arrivals over 7 months | Consecutive sampling at reception | DIS | DSM‐III | 29 | SD 8.2 | N | Not reported | Sentenced | 0% | 21 | 0 |
| Teplin 1994 | USA | Cook County Departmentof Corrections, Chicago | All remands 1983–84 | Stratified randomsampling | DIS | DSM‐III‐R | Not reported | Not reported | Not reported | Not reported | Remand | 100% | Not reported | 35 |
| Jordan 1996 | USA | Correctional Institution for Women, Raleigh, NC | All sentenced incoming prisoners in 1991–92 | Combined consecutive and random sampling | CIDId | DSM‐III‐R | 31.5 | 18–65 | Y | 5–10 days | Sentenced | 0% | 98 | 42 |
| Smith 1996 | Ireland | Mountjoy Prison, Dublin | All new arrivals in 1992–93 | Simple random sampling | Clinical interview | DSM‐III‐R | Not reported | Not reported | Y | 1 day | Mixed | 100% | Not reported | 2 |
| Teplin 1996 | USA | Cook County Departmentof Corrections, Chicago | All remands 1991–93 | Stratified randomsampling | DIS | DSM‐III‐R | 28 | 17–67 | N | Not reported | Remand | 0% | 201 | 59 |
| Mason 1997 | England | Durham Remand prison for men | All remands over 7 months | Consecutive sampling at reception | Clinical interview | DSM‐IV | Not reported | Not reported | Y | Not reported | Remand | 100% | Not reported | 0 |
| McClellan 1997 | USA | Prison unit for men and reception centre for women, Texas | All newly admitted inmates | Simple random sampling | DIS | DSM‐III | 32.8 male 32.3 female | Not reported | N | Not reported | Mixed | 67% | Not reported | 202 |
| Mohan 1997 | Ireland | Mountjoy Prison, Dublin | Consecutive new arrivals over 3 months | Simple random sampling | SCANe | DSM‐IV | 25.8 | 17–48 | Y | Not reported | Mixed | 0% | 0 | 0 |
| Peters 1998 | USA | Holliday Transfer Facility, Texas | Consecutive new arrivals in 1996 | Consecutive sampling at reception | SCID IVf | DSM‐IV | 32.6 | SD 10.2 | Y | 14–60 days | Sentenced | 100% | 61 | 100 |
| Lo 2000 | USA | Cuyahoga County Jail, Cleveland, USA | All sentenced incoming prisoners in 1997–98 | Consecutive sampling | DIS | DSM‐IV | 30 | 18–58 | N | Not reported | Sentenced | 76% | Not reported | 29 |
| Marquart 2001 | USA | Texas Deptartment of Criminal Justice, institutional division | All female prisonersadmitted in 1994 | Simple random sampling | DIS | DSM‐IV | 32.3 | 17–63 | Y | Not reported | Remand | 0% | Not reported | 0 |
| Butler 2003 | Australia | Metropolitan Remand and Reception Centre, female Correctional Centre and remote reception sites | Consecutive convenience sample of admissions over 3 months | Convenience sample among those admitted over 3 months | CIDI | DSM‐IV and ICD‐10g | Men 29.61, women 29.10 | Not reported | Mental health nurses | Not reported | Mixed | 100% | Not reported | Non‐screened: 67.4% |
| Wright 2006 | Ireland | The Dochas Centre, female wing of Limerick Prison near Dublin | Consecutive admissions in August 2003 and between April 2004 and May 2004 | All consenting prisoners interviewed at reception (10.7% of all committals) | SADS‐L,h SODQi | ICD‐10 | 27.4 | Not reported | Post‐membership psychiatrists | Aimed to interview within 72 hours of reception | Mixed | 0% | 14/60 = 23.3% | 30 |
| Jones 2006 | England | HMP Grendon (therapeutic community prison) | Consecutive admissions in 2003 | All consenting prisoners interviewed at reception | CAAPEj | DSM‐IV | 30.7 | 18–66 | Psychological counsellor | Shortly after admission | Sentenced | 100% | Not reported | 0 |
| Bulten 2009 | Netherlands | Vught prison | Random sample of admissions to ‘general wards’ of prison | Random sample among new admissions | MINIk | DSM‐III‐R | 30.4 | 18–59 | Trained psychologist | First weeks of incarceration | Mixed | 100% | 73 | 50 |
| Curtin 2009 | Ireland | Cloverhill, Limerick and Cork Prisons (remand), Mountjoy and Cork Prisons (sentenced) | Consecutive admissions, up to 10 per day | All consenting prisoners interviewed at reception | SADS‐L | ICD‐10 | 29.8 | 18+ | Post‐membership psychiatrists | Within 72 hours | Mixed | 100% | 79 | 54 |
| Einarsson 2009 | Iceland | Icelandic prison for sentenced inmates | All new admissions in study period (females excluded) | All consenting prisoners interviewed at reception | MINI 5 | DSM‐IV | 31 | 19–56 | Psychologist | Within 10 days | Sentenced | 100% | 15 | 16 |
| Stompe 2010 | Austria | Prison Vienna‐Josefstadt | Consecutive recruitment of admissions | All eligible new admits. | SCAN | ICD‐10 | Not reported | 18+ | Doctor (psychiatry trainee) | Not reported | Mixed | 100% | Not reported | 0 |
| Proctor 2012 | USA | Minnesota state prisons | All reception 2000–03 | All consenting prisoners interviewed at reception | SUDDS‐IVl | DSM‐IV | 32.8 | 18–58 | Addictions counsellors (computer recorded interview) | Not reported | Sentenced | 0% | Not reported | 0 |
| Sarlon 2012 | France | Local prisons of Fleury‐Merogis, Loos, Lyon, Marseille | Reception: new receptions to local prisons in four areas | All consenting prisoners interviewed at reception | MINI plus 5.0 | DSM‐IV | 29.9 | 18–64 | Clinicians (psychiatrist and psychologist) | within 14 days | Mixed | 100% | Not reported | 30 |
| Tavares 2012 | Brazil | Porto Alegre prison | Consecutive admissions | Random sample among new admits (calculation of 30 a base‐point for recruitment) | MINI‐plus (Brazilian version) | DSM‐IV | 27.88 | Not reported | Not reported | Within 3 months | Sentenced | 100% | 10 | 0 |
| Mir 2015 | Germany | Penal justice system in Berlin | Consecutive admissions screened for eligibility | All eligible new admits. Aimed for sample of 150. | MINI 6.0 (German version) | DSM‐IV | 34.3 | Not reported | Clinical psychologist | Within 1 month (usually <1 week) | Mixed | 0% | 0 | 48 |
| Mundt 2015 | Chile | Santiago Uno central facility, Centro Penitenciario Feminino, San Joaquín, CPF San Miguel central admission facilities | Consecutive admissions | All consenting prisoners interviewed at reception | MINI Spanish version | DSM‐IV | 31.6 | Not reported | Clinical psychologist/nurse (trained by senior consultant psychiatrist) | 7.7 days | Remand | 54% | 127 | 30 |
| Hoffmann 2015 | USA | 8 adult state prison facilities of Minnesota | Uses routine data collected on admissions, all admissions during 2002–03 | All consenting prisoners interviewed at reception | SUDDS‐IV | ICD‐10 | 31 | 18–65 | Addiction counsellors | On admission | Sentenced | 90% | Not reported | 0 |
Y = Yes; psychiatrist, N = no; non‐psychiatrist (trained interviewer);
DIS = Diagnostic Interview Schedule;
DSM = Diagnostic and Statistical Manual of Mental Disorders; DSM‐IIIR = DSM‐III revised;
CIDI = Composite International Diagnostic Interview;
SCAN = Schedules for Clinical Assessment in Neuropsychiatry;
SCID = Structured Clinical Interview for DSM Disorders;
ICD = International Classification of Diseases;
SADS‐L = Schedule for Affective Disorders and Schizophrenia – life‐time version;
SODQ = Severity of Opiate Dependence Questionnaire;
CAAPE = Comprehensive Addictions and Psychological Evaluation;
MINI = Mini International Neuropsychiatric Interview;
SUDDS = Substance Use Disorders Diagnostic Schedule.
Table 2.
Prevalence estimates of substance use disorder in reception studies of prisoners.
| Study | Total no. | Males (%) | No. with alcohol use disorder | No. with drug use disorder | Prevalence of alcohol use disorder (%) | Prevalence of drug use disorder (%) |
|---|---|---|---|---|---|---|
| Daniel 1988 | 100 | 0 | 10a | – | 10.0 | – |
| Collins 1988 | 1120 | 100 | 302a | 112a | 27.0 | 10.0 |
| Teplin 1994 | 728 | 100 | 116a | 129a | 15.9 | 17.7 |
| Jordan 1996 | 805 | 0 | 244a | 138a | 30.3 | 17.1 |
| Smith 1996 | 235 | 100 | 63 | 46 | 26.8 | 19.6 |
| Teplin 1996 | 1272 | 0 | 667a | 304a | 52.4 | 23.9 |
| Bushnell 1997 | 100 | 100 | 19a | 14a | 19.0 | 14.0 |
| Mason 1997 | 548 | 100 | 116a | 214a | 21.2 | 39.1 |
| McClellan 1997 |
1030 male 500 female |
67 |
309 male 93 female |
331 male 227 female |
30.0 male 18.6 female |
32.1 male 45.4 female |
| Mohan 1997 | 45 | 0 | 0 | 26 | 0.0 | 57.8 |
| Peters 1998 | 400 | 100 | 86a | 100a | 21.5 | 25.0 |
| Lo 2000 |
152 male 48 female |
76 | – |
73 male 29 female |
– |
48.0 male 60.4 female |
| Marquart 2001 | 500 | 0 | 88a | 224a | 17.6 | 44.8 |
| Butler 2003 |
756 male 165 female |
82 |
142 male 27 female |
378 male 111 female |
19.2 male 16.5 female |
52.0 male 68.9 female |
| Wright 2006 | 94 | 0 | 23 | 45 | 24.7 | 48.4 |
| Jones 2006 | 118 | 100 | 53 | – | 44.9 | – |
| Bulten 2009 | 191 | 100 | 53 | 57 | 27.7 | 29.8 |
| Curtin 2009 | 615 | 100 | 148 | 206 | 24.1 | 33.5 |
| Einarsson 2009 | 90 | 100 | 46 | 55 | 51.1 | 61.1 |
| Stompe 2010 | 200 | 100 | 59a | – | 29.5 | – |
| Proctor 2012 | 801 | 0 | 242 | 456 | 30.2 | 56.9 |
| Sarlon 2012 | 267 | 100 | 43 | 47 | 16.1 | 17.6 |
| Mir 2015 | 150 | 0 | 31 | 71 | 20.7 | 47.3 |
| Hoffmann 2015 | 6871 | 90 | 2177 | – | 31.7 | – |
| LMI countries | ||||||
| Tavares 2012 | 60 | 100 | 26 | 18 | 43.3 | 30.0 |
| Mundt 2015 |
229 male 198 female |
54 |
68 male 23 female |
128 male 47 female |
29.7 male 11.6 female |
55.9 male 23.7 female |
| Juvenile prisoners | ||||||
| Köhler 2009 | 149 | 100 | 31 | – | 20.8 | – |
| Vreugdenhil 2003 | 204 | 100 | 45 | – | 22.1 | – |
| McClelland 2004 |
1143 male 631 female |
64 |
289 malea
156 femalea |
276 malea
260 femalea |
25.3 male 24.7 female |
24.1 male 41.2 female |
| Plattner 2012 | 275 | 100 | 45 | 135 | 16.4 | 49.1 |
| Dixon 2005 | 100 | 0 | 55a | 85a | 55.0 | 85.0 |
Figures for combined abuse and dependence; the rest are dependence only.
Alcohol use disorder
The overall pooled prevalence estimate of alcohol use disorder was 24% [95% confidence interval (CI) = 21–27], with very high levels of between‐study heterogeneity (I 2 = 94%; 95% CI = 92–95). Fifteen studies of alcohol use disorder in men were identified in 12 739 prisoners 37, 38, 40, 41, 42, 44, 48, 50, 51, 52, 57, 58, 60, 61. Pooled prevalence estimate for males was 26% (95% CI = 23–30), with substantial heterogeneity between studies (I 2 = 94%; 95% CI = 92–96) and a range of 16–51% in individual studies. We identified 10 investigations that measured alcohol use disorder in female prisoners 38, 39, 40, 45, 46, 49, 53, 54, 55, 56, and pooled prevalence estimate was 20% (95% CI = 16–24) with high heterogeneity (I 2 = 88%; 95% CI = 80–93). Primary studies provided estimates that varied from 10 to 30% (Figure 2).
Figure 2.
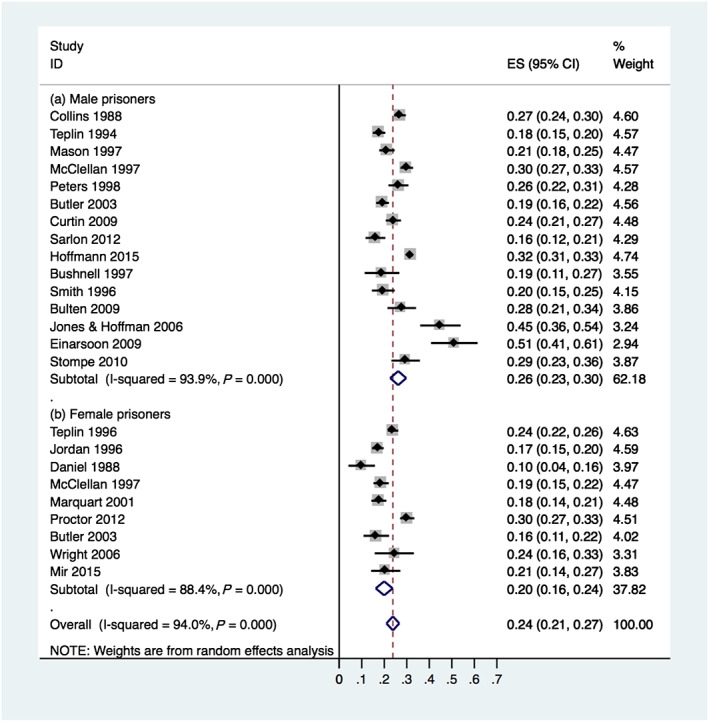
Prevalence of alcohol use disorder in male and female prisoners on reception to prison (ES = prevalence estimates). [Colour figure can be viewed at wileyonlinelibrary.com]
Two investigations in LMI countries reported prevalences of 43% 25 and 30% 26. There were four investigations of alcohol use disorder in juvenile men, and prevalences ranged from 16 to 25% 27, 28, 29, 31).
Drug use disorder
There was evidence of heterogeneity by sex in univariable meta‐regression, and prevalence estimates for drug use disorder are stratified accordingly.
Men
Thirteen studies reported drug use disorder in male prisoners 37, 38, 40, 41, 42, 44, 47, 48, 50, 51, 52, 57, 60. The pooled prevalence estimate was 30% (95% CI = 22–38), with very high heterogeneity (I 2 = 98%; 95% CI = 98–99). These varied from 10 to 61%. In LMI countries, reported prevalences were 30% 25 and 56% 26.
Women
Ten relevant studies on drug use disorder in female prisoners were identified 38, 39, 40, 46, 47, 49, 53, 54, 55, 56. The pooled prevalence estimate was 51% (95% CI = 43–58) with substantial heterogeneity (I 2 = 95%; 95% CI = 93–97). Prevalences ranged from 30 to 69%.
Sources of heterogeneity
In univariable meta‐regression (n = 23 studies), factors associated with heterogeneity included: females reported higher drug use disorder than males (β = 0.21; 95% CI = 0.33–0.10; P = 0.001), more recent studies (published after 2000) reported higher rates of drug use disorder (β = 0.15; 95% CI = 0.12–0.28; P = 0.03), and participation rate was associated negatively with drug use disorder (β = −0.37; 95% CI = 0.73, −0.01; P = 0.045). No significant associations were reported with alcohol use disorder, although there was a non‐significant link with publication year as a continuous variable (β = 0.004; 95% CI = –0.00002, 0.008; P = 0.051).
Using subgroup analysis, we also investigated possible explanations for between‐study variation (Table 3). This found that there were higher estimates for drug use disorders in women, and for both drug and alcohol use disorders since 2000, which were consistent with findings on meta‐regression. In addition, in alcohol use disorders, there were higher prevalence estimates in sentenced (than remand) prisoners. However, these subgroup analyses had overlapping CIs, apart from a higher estimate for women with drug use disorder compared to men (Figure 3).
Table 3.
Pooled prevalence estimates for drug and alcohol use disorders in newly incarcerated men and women by pre‐specified subgroups.
|
Alcohol use disorder, % (95% CI) |
Drug use disorder, % (95% CI) |
|||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Country | ||||
| High income countries | – | – | 30 (22–38) (n = 5750; k = 13) | 51 (43–58) (n = 4379; k = 10) |
| USA | 23 (19–27) (n = 9619; k = 5) | 20 (15–25) (n = 3978; k = 6) | 37 (26–48)(n = 2948; k = 5) | 48 (39–57) (n = 3926; k = 6) |
| Non‐USA | 25 (21–28) (n = 3573; k = 14) | 20 (15–24) (n = 453; k = 4) | 40 (31–50) (n = 3255; k = 12) | 56 (44–68) (n = 453; k = 4) |
| Publication year | ||||
| Before 2000 | – | – | – | 46 (33–58) (n = 2622; k = 4) |
| 2000 and after | – | – | – | 54 (47–62) (n = 1757; k = 6) |
| Prisoner type | ||||
| Remand | 21 (18–25) (n = 1502; k = 4) | – | – | – |
| Sentenced | 33 (29–37) (n = 8808; k = 7) | – | – | – |
| Interviewer | ||||
| Psychiatrist | 23 (19–26) (n = 2265; k = 6) | – | – | – |
| Other | 30 (26–35) (n = 9746; k = 8) | – | – | – |
CI = confidence interval.
Figure 3.
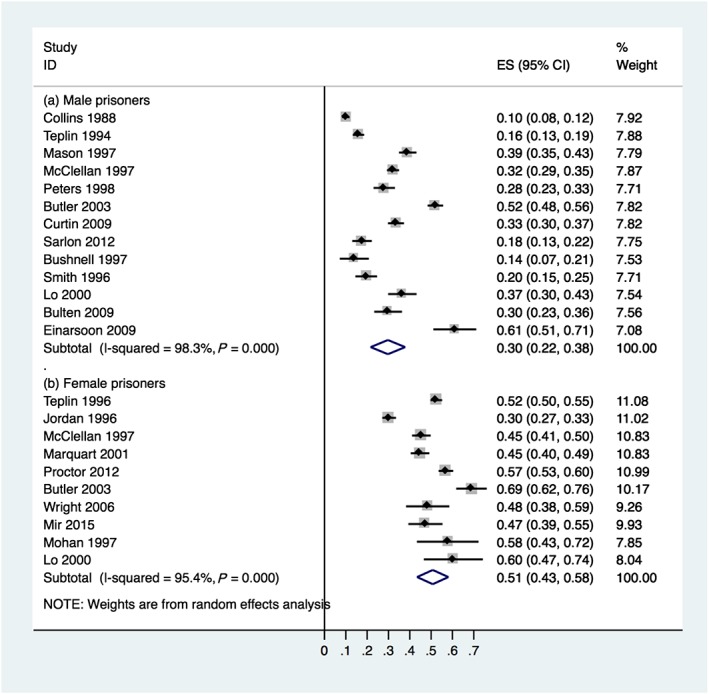
Prevalence of drug use disorder in male and female prisoners on reception to prison (ES = prevalence estimates). [Colour figure can be viewed at wileyonlinelibrary.com]
Publication bias
There was no evidence of publication bias overall and in subgroups stratified by sex apart from drug use disorder in male prisoners, where there was non‐significant evidence of publication bias in the funnel plot analysis (Egger's test, t = 2.19, SE(t) = 4.27, P = 0.051) 37, 38, 40, 41, 42, 44, 47, 48, 50, 51, 52, 57, 60. Visual analysis of the funnel plot suggested asymmetry, but appeared to be mainly attributable to one study 60 with a high prevalence and large standard error, which when removed did not suggest clear publication bias (Supporting information, Appendix S4).
Discussion
This updated systematic review of the prevalence of substance use disorder in prisoners is based on 24 studies and 18 388 individuals in 10 countries. In addition, we identified five studies in juvenile prisoners and two investigations in LMI countries. The sample size in this update is more than double of that a previous systematic review 11, which identified relevant prevalence studies until 2004, and this updated synthesis allowed for an investigation of sources of heterogeneity between included studies.
We report two main findings. The first is that alcohol use disorder was highly prevalent in prisoners, with a pooled estimate of 24% (95% CI = 21–27). In men, the lowest estimate suggests that one in six (16%) met the threshold for alcohol use disorder on arrival into prison, and in women it was one in 10. By way of comparison, in the United States in 2013 community rates of past year alcohol use disorder were estimated at 8.7% for men and 4.6% in women 62. According to the Global Burden of Disease 2015 Study, the global prevalence of alcohol use disorder was 1.5% for males and 0.3% for females (0.9% for both sexes) 63. The second major finding was that drug use disorder was as high as the alcohol estimates, and possibly higher in female prisoners, with a pooled estimate of 51% (95% CI = 43–58). Importantly, the lowest prevalence study in women found that 30% had a drug use disorder. This can be contrasted with US community samples, where 3.4% of men and 1.9% women had such a disorder 62, and 0.8% in men and 0.4% in women (0.6% for both sexes) worldwide 63.
We investigated sources of heterogeneity more carefully than previous work, which led to a number of potentially important findings. First, using meta‐regression, we found evidence of increasing drug use disorder in prison studies during the past three decades. This is in contrast with community trends in some high‐income countries such as the United States, where drug use disorder had not increased (and alcohol reduced slightly) between 2000 and 2013 64. Secondly, two other study characteristics were associated with significant variations in prevalence. Having a higher participation rate was associated with lower rates in drug use disorder, and there were higher rates of drug use disorders in women prisoners. Being assessed by a psychiatrist was also linked with lower alcohol use disorder prevalence in subgroup analyses, although the confidence intervals overlapped. This should inform the interpretation of single studies, particularly if used for service planning and development. One possible explanation for heterogeneity that we did not investigate are the community baseline rates of substance use disorders, and future work could examine this using comparable measures of drug and alcohol use, such as the ongoing Global Burden of Disease 63. In addition, the reported high prevalence range of 30–56% for substance use disorder in LMI countries needs further research, as it was based on only two investigations.
A number of implications arise from this updated meta‐analysis. First, it highlights the opportunity that jails and prisons present to treat substance use disorders 65. The high prevalences underscore the importance of evidence‐based interventions being available to all individuals entering custody. Four areas should be considered to improve management of substance use disorders in prisoners. First, prison arrival centres need to have systems in place to identify individuals with high treatment needs, and treatments should be matched to individual needs 65. Secondly, acute detoxification management should be available to all entrants to custody, which may include short‐term prescription of benzodiazepines for alcohol withdrawal 66 and symptomatic treatment of withdrawal from other substances that may include opioid agonists (such as methadone or buprenorphine). Detoxification programmes may benefit from the use of clinical tools to document withdrawal symptoms 67. Thirdly, combination pharmacological and psychosocial treatments should be available, considering the high prevalences and the subsequent effects on adverse outcomes, including mortality after release and violent re‐offending 68, 69. Finally, considering the high relapse rates, programmes need to link prisoners with community services. Structured, simple and scalable tools to identify those at highest risk 70 and case management 71 may assist in this process. A second implication from the review is that prevalence research needs to consider some areas of improvement. These include separating prevalences by drug and alcohol use disorder, and also providing information stratified by sex and prisoner status (i.e. sentenced or not). Baseline information on socio‐demographic and criminal history characteristics (such as those listed in Table 1, including the sample's age structure and index offence) should be provided in new studies, and supplemented with more clinically informative information, such as comorbidities with mental illness 72 and chronic pain, prevalence by individual drugs and most recent treatment. At the same time, as there are now at least 24 studies on prevalence on more than 18 000 prisoners, whether new research should prioritize how treatment can be delivered most effectively to prisoners and former prisoners needs to be considered by funding agencies, researchers and government agencies in criminal justice and public health.
Some limitations to this review need to be considered. First, there was variation in the diagnostic tools and interviewers used to assess substance use disorders, and we found that psychiatrist interviewers were associated with lower prevalences for alcohol use disorder. To reflect this clinical and statistical heterogeneity, we also reported prevalence ranges. Secondly, as we focused upon substance use disorders on prison entry, these estimates may not reflect treatment needs later in prison or on prison release, where novel psychoactive substances are increasingly problematic and may require different treatment approaches 73. In addition, the misuse of prescribed medication such as painkillers, anti‐epileptics and anxiolytics inside custody needs to be considered, and may further increase treatment needs. Finally, some of the subgroup analyses were based on fewer than 10 studies, and should be interpreted with caution.
In summary, the high prevalence of alcohol and drug use disorders in prisoners remains a key challenge for prison health. Tackling this will probably require interventions at all stages of the criminal justice process—from identifying and treating withdrawal in police custody 74 and on arrival to prison, to opiate maintenance and other treatments during any period in prison 68, to community links being made and integrated treatment provided on release 75. Comprehensive strategies to prevent relapse of substance dependence are likely to reduce premature mortality, recidivism and subsequent return to prison.
Declaration of interests
None.
Supporting information
Appendix S1 Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist.
Appendix S2 Quality checklist.
Appendix S3 Study characteristics of studies of substance use disorders in juvenile prisoners.
Appendix S4 Funnel plot of studies reporting drug use disorder prevalence in male prisoners.
Acknowledgements
We thank J. Borrill, B.K. Jordan, E.M. Kouri, C. Lo, J. Marquart, L. Teplin and T. Weaver for kindly providing additional data from their studies for the initial review. We are grateful to T. Butler, H. Kennedy, N. Hoffmann, A. Kopak, A. Dixon and B. Wright for providing further information about their studies for the update. In addition, D. Black, A.. Robertson, A Armiyau, R. Almeida, F. Sahajian, J. Baillargeon and J. Sigurðsson helpfully responded to queries. Professor Seena Fazel is funded by the Wellcome Trust (#202836/Z/16/Z). The Trust had no direct involvement in the conduct of this research.
Fazel, S. , Yoon, I. A. , and Hayes, A. J. (2017) Substance use disorders in prisoners: an updated systematic review and meta‐regression analysis in recently incarcerated men and women. Addiction, 112: 1725–1739. doi: 10.1111/add.13877.
[The copyright line for this article was changed on 11 October 2017 after original online publication.]
References
- 1. Pratt D., Appleby L., Piper N., Webb R., Shaw J. Suicide in recently released prisoners: a case–control study. Psychol Med 2010; 40: 827–835. [DOI] [PubMed] [Google Scholar]
- 2. Kinner S. A., Forsyth S., Williams G. Systematic review of record linkage studies of mortality in ex‐prisoners: why (good) methods matter. Addiction 2013; 108: 38–49. [DOI] [PubMed] [Google Scholar]
- 3. Chang Z., Lichtenstein P., Larsson H., Fazel S. Substance use disorders, psychiatric disorders, and mortality after release from prison: a nationwide longitudinal cohort study. Lancet Psychiatry 2015; 2: 422–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baillargeon J., Binswanger I. A., Penn J. V., Williams B. A., Murray O. J. Psychiatric disorders and repeat incarcerations: the revolving prison door. Am J Psychiatry 2009; 166: 103–109. [DOI] [PubMed] [Google Scholar]
- 5. Chang Z., Larsson H., Lichtenstein P., Fazel S. Psychiatric disorders and violent reoffending: a national cohort study of convicted prisoners in Sweden. Lancet Psychiatry 2015; 2: 891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rivlin A., Hawton K., Marzano L., Fazel S. Psychiatric disorders in male prisoners who made near‐lethal suicide attempts: Case‐control study. Br J Psychiatry 2010; 197: 313–319. [DOI] [PubMed] [Google Scholar]
- 7. Teasdale B., Daigle L. E., Hawk S. R., Daquin J. C. Violent victimization in the prison context: an examination of the gendered contexts of prison. Int J Offender Ther Comp Criminol 2016; 60: 995–1015. [DOI] [PubMed] [Google Scholar]
- 8. Steiner B., Wooldredge J. Inmate versus environmental effects on prison rule violations. Crim Justice Behav 2008; 35: 438–456. [Google Scholar]
- 9. Oser C. B., Knudsen H. K., Staton‐Tindall M., Taxman F., Leukefeld C. Organizational‐level correlates of the provision of detoxification services and medication‐based treatments for substance abuse in correctional institutions. Drug Alcohol Depend 2009; 103: S73–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Department of Health . The Patel Report: Reducing Drug‐Related Crime and Rehabilitating Offenders. London, UK: Department of Health; 2010. [Google Scholar]
- 11. Fazel S., Bains P., Doll H. Substance abuse and dependence in prisoners: a systematic review. Addiction 2006; 101: 181–191. [DOI] [PubMed] [Google Scholar]
- 12. Moher D., Liberati A., Tetzlaff J., Altman D. G. The PRISMA group: Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA statement. PLOS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fazel S., Yoon I., Hayes A. Substance abuse and dependence in prisoners: a systematic review‐ an update. PROSPERO. 2017-06-22. Available at: https://www.crd.york.ac.uk/prospero/display_record.asp?ID=CRD42016036416 (accessed 22 June 2017) (Archived at http://www.webcitation.org/6rPu54FrU).
- 14. Carra G., Giacobone C., Pozzi F., Alecci P., Barale F. Prevalence of mental disorder and related treatments in a local jail: a 20‐month consecutive case study. Epidemiol Psichiatr Soc 2004; 13: 47–54. [DOI] [PubMed] [Google Scholar]
- 15. Brown K., Cullen A., Kooyman I., Forrester A. Mental health expertise at prison reception. J Forensic Psychiatry Psychol 2015; 26: 107–115. [Google Scholar]
- 16. Black D. W., Gunter T., Loveless P., Allen J., Sieleni B. Antisocial personality disorder in incarcerated offenders: psychiatric comorbidity and quality of life. Ann Clin Psychiatry 2010; 22: 113–120. [PubMed] [Google Scholar]
- 17. Horn M., Potvin S., Allaire J.‐F., Côté G., Gobbi G., Benkirane K. et al. Male inmate profiles and their biological correlates. Can J Psychiatry 2014; 59: 441–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhou J., Witt K., Zhang Y., Chen C., Qiu C., Cao L. et al. Anxiety, depression, impulsivity and substance misuse in violent and non‐violent adolescent boys in detention in China. Psychiatry Res 2014; 216: 379–384. [DOI] [PubMed] [Google Scholar]
- 19. Langeveld H., Melhus H. Are psychiatric disorders identified and treated by in‐prison health services? Tidsskr Nor Laegeforen 2004; 124: 2094–2097. [PubMed] [Google Scholar]
- 20. Stewart D. Drug use and perceived treatment need among newly sentenced prisoners in England and Wales. Addiction 2009; 104: 243–247. [DOI] [PubMed] [Google Scholar]
- 21. Proctor S. L., Kopak A. M., Hoffmann N. G. Compatibility of current DSM‐IV and proposed DSM‐5 diagnostic criteria for cocaine use disorders. Addict Behav 2012; 37: 722–728. [DOI] [PubMed] [Google Scholar]
- 22. MacAskill S., Parkes T., Brooks O., Graham L., McAuley A., Brown A. Assessment of alcohol problems using AUDIT in a prison setting: more than an ‘aye or no’ question. BMC Public Health 2011; 11: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kissell A., Taylor P. J., Walker J., Lewis E., Hammond A., Amos T. Disentangling alcohol‐related needs among pre‐trial prisoners: a longitudinal study. Alcohol Alcohol 2014; 49: 639–644. [DOI] [PubMed] [Google Scholar]
- 24. Lintonen T. P., Vartiainen H., Aarnio J., Hakamäki S., Viitanen P., Wuolijoki T. et al. Drug use among prisoners: by any definition, it's a big problem. Subst Use Misuse 2011; 46: 440–451. [DOI] [PubMed] [Google Scholar]
- 25. Tavares G. P., Scheffer M., de Almeida R. M. M. Drogas, violência e aspectos emocionais em apenados [Drugs, violence and emotional aspects in prisoners.]. Psicol Reflex Crit 2012; 25: 89–95. [Google Scholar]
- 26. Mundt A. P., Kastner S., Larraín S., Fritsch R., Priebe S. Prevalence of mental disorders at admission to the penal justice system in emerging countries: a study from Chile. Epidemiol Psychiatr Sci 2015; 1: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Köhler D., Heinzen H., Hinrichs G., Huchzermeier C. The prevalence of mental disorders in a German sample of male incarcerated juvenile offenders. Int J Offender Ther Comp Criminol 2009; 53: 211–227. [DOI] [PubMed] [Google Scholar]
- 28. Vreugdenhil C., Doreleijers T. A. H., Vermeiren R., Wouters L. F. J. M., Van Den Brink W. Psychiatric disorders in a representative sample of incarcerated boys in the Netherlands. J Am Acad Child Adolesc Psychiatry 2004; 43: 97–104. [DOI] [PubMed] [Google Scholar]
- 29. McClelland G. M., Elkington K. S., Teplin L. A., Abram K. M. Multiple substance use disorders in juvenile detainees. J Am Acad Child Adolesc Psychiatry; 43: 1215–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dixon A., Howie P., Starling J. Trauma exposure, posttraumatic stress, and psychiatric comorbidity in female juvenile offenders. J Am Acad Child Adolesc Psychiatry; 44: 798–806. [DOI] [PubMed] [Google Scholar]
- 31. Plattner B., Giger J., Bachmann F., Brühwiler K., Steiner H., Steinhausen H.‐C. et al. Psychopathology and offense types in detained male juveniles. Psychiatry Res 2012; 198: 285–290. [DOI] [PubMed] [Google Scholar]
- 32. Grant B. F., Harford T. C., Muthén B. O., Yi H. Y., Hasin D. S., Stinson F. S. DSM‐IV alcohol dependence and abuse: further evidence of validity in the general population. Drug Alcohol Depend 2007; 86: 154–166. [DOI] [PubMed] [Google Scholar]
- 33. Sheehan D. V., Lecrubier Y., Harnett S. K., Janavs J., Weiller E., Keskiner A. et al. The validity of the MINI international neuropsychiatric interview (MINI) according to the SCID‐P and its reliability. Eur Psychiatry 1997; 12: 232–241. [Google Scholar]
- 34. Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015; 13: 147–153. [DOI] [PubMed] [Google Scholar]
- 35. Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. Introduction to Meta‐Analysis. Somerset, NJ: Wiley; 2011. [Google Scholar]
- 36. Thompson S. G., Higgins J. P. How should meta‐regression analyses be undertaken and interpreted? Stat Med 2002; 21: 1559–1573. [DOI] [PubMed] [Google Scholar]
- 37. Bushnell J. A., Bakker L. W. Substance use disorders among men in prison: a New Zealand study. Aust NZ J Psychiatry 1997; 31: 577–581. [DOI] [PubMed] [Google Scholar]
- 38. McClellan D. S., Farabee D., Crouch B. M. Early victimization, drug use, and criminality: a comparison of male and female prisoners. Crim Justice Behav 1997; 24: 455–476. [Google Scholar]
- 39. Mohan D., Scully P., Collins C., Smith C. Psychiatric disorder in an Irish female prison. Crim Behav Ment Health 1997; 7: 229–235. [Google Scholar]
- 40. Butler T., Allnutt S. Mental illness among New South Wales prisoners. Sydney, NSW: Corrections Health Service; 2003. [Google Scholar]
- 41. Curtin K., Monks S., Wright B., Duffy D., Linehan S., Kennedy H. G. Psychiatric morbidity in male remanded and sentenced committals to Irish prisons. Ir J Psychol Med 2009; 26: 169–173. [DOI] [PubMed] [Google Scholar]
- 42. Sarlon E., Duburcq A., Neveu X., Morvan‐Duru E., Tremblay R., Rouillon F. et al. Imprisonment, alcohol dependence and risk of delusional disorder: a cross‐sectional study. Rev Epidemiol Sante Publique 2012; 60: 197–203. [DOI] [PubMed] [Google Scholar]
- 43. Sterne J. A. C., Egger M. Funnel plots for detecting bias in meta‐analysis: guidelines on choice of axis. J Clin Epidemiol 2001; 54: 1046–1055. [DOI] [PubMed] [Google Scholar]
- 44. Collins J. J., Bailey S. L., Phillips C. D., Craddock A. The Relationship of Mental Disorder to Violent Behavior. Research Triangle, NC: Research Triangle Institute, Center for Social Research and Policy Analysis; 1988. [Google Scholar]
- 45. Daniel A. E., Robins A. J., Reid J. C., Wilfley D. E. Lifetime and six‐month prevalence of psychiatric disorders among sentenced female offenders. Bull Am Acad Psychiatry Law 1988; 16: 333–342. [PubMed] [Google Scholar]
- 46. Jordan B., Schlenger W. E., Fairbank J. A., Caddell J. M. Prevalence of psychiatric disorders among incarcerated women: II. Convicted felons entering prison. Arch Gen Psychiatry 1996; 53: 513–519. [DOI] [PubMed] [Google Scholar]
- 47. Lo C. C., Stephens R. C. Drugs and prisoners: treatment needs on entering prison. Am J Drug Alcohol Abuse 2000; 26: 229–245. [DOI] [PubMed] [Google Scholar]
- 48. Mason D., Birmingham L., Grubin D. Substance use in remand prisoners: a consecutive case study. BMJ 1997; 315: 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Marquart J. W., Brewer V. E., Simon P., Morse E. V. Lifestyle factors among female prisoners with histories of psychiatric treatment. J Crim Justice 2001; 29: 319–328. [Google Scholar]
- 50. Peters R. H., Greenbaum P. E., Edens J. F., Carter C. R., Ortiz M. M. Prevalence of DSM‐IV substance abuse and dependence disorders among prison inmates. Am J Drug Alcohol Abuse 1998; 24: 573–587. [DOI] [PubMed] [Google Scholar]
- 51. Smith C., O'Neill H., Tobin J., Walshe D., Dooley E. Mental disorders detected in an Irish prison sample. Crim Behav Ment Health 1996; 6: 177–183. [Google Scholar]
- 52. Teplin L. A. Psychiatric and substance abuse disorders among male urban jail detainees. Am J Public Health 1994; 84: 290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Teplin L. A., Abram K. M., McClelland G. M. Prevalence of psychiatric disorders among incarcerated women: I. Pretrial jail detainees. Arch Gen Psychiatry 1996; 53: 505–512. [DOI] [PubMed] [Google Scholar]
- 54. Proctor S. L. Substance use disorder prevalence among female state prison inmates. Am J Drug Alcohol Abuse 2012; 38: 278–285. [DOI] [PubMed] [Google Scholar]
- 55. Wright B., Duffy D., Curtin K., Linehan S., Monks S., Kennedy H. G. Psychiatric morbidity among women prisoners newly committed and amongst remanded and sentenced women in the Irish prison system. Ir J Psychol Med 2006; 23: 47–53. [DOI] [PubMed] [Google Scholar]
- 56. Mir J., Kastner S., Priebe S., Konrad N., Ströhle A., Mundt A. P. Treating substance abuse is not enough: comorbidities in consecutively admitted female prisoners. Addict Behav 2015; 46: 25–30. [DOI] [PubMed] [Google Scholar]
- 57. Bulten E., Nijman H., van der Staak C. Psychiatric disorders and personality characteristics of prisoners at regular prison wards. Int J Law Psychiatry 2009; 32: 115–119. [DOI] [PubMed] [Google Scholar]
- 58. Jones G. Y., Hoffmann N. G. Alcohol dependence: international policy implications for prison populations. Subst Abuse Treat Prev Policy 2006; 1: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hoffmann N. G., Kopak A. M. How well do the DSM‐5 alcohol use disorder designations map to the ICD‐10 disorders? Alcohol Clin Exp Res 2015; 39: 697–701. [DOI] [PubMed] [Google Scholar]
- 60. Einarsson E., Sigurdsson J. F., Gudjonsson G. H., Newton A. K., Bragason O. O. Screening for attention‐deficit hyperactivity disorder and co‐morbid mental disorders among prison inmates. Nord J Psychiatry 2009; 63: 361–367. [DOI] [PubMed] [Google Scholar]
- 61. Stompe T., Brandstätter N., Ebner N., Fischer‐Danzinger D. Psychiatrische Störungen bei Haftinsassen [Psychiatric disorders in prison inmates]. J Neurol Neurochir Psychiatr 2010; 11: 20–23. [Google Scholar]
- 62. Substance Abuse and Mental Health Services Administration . Behavioral Health Barometer: United States, 2014. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- 63. Institute for Health Metrics and Evaluation (IHME) . Global Burden of Disease Study 2015 (GBD 2015) Results. Seattle, USA: Institute for Health Metrics and Evaluation (IHME); 2016. [Google Scholar]
- 64. Substance Abuse and Mental Health Services Administration . Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 65. Taxman F. S., Perdoni M. L., Harrison L. D. Drug treatment services for adult offenders: the state of the state. J Subst Abuse Treat 2007; 32: 239–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Amato L., Minozzi S., Vecchi S., Davoli M. Benzodiazepines for alcohol withdrawal. Cochrane Database Syst Rev 2010; Issue 3. Art. No.: CD005063. https://doi.org/10.1002/14651858.CD005063.pub3. [DOI] [PubMed] [Google Scholar]
- 67. Wakeman S. E., Rich J. D. Pharmacotherapy for substance use disorders within correctional facilities In: Trestman B., Appelbaum K., Metzner J., editors. Oxford Textbook of Correctional Psychiatry. New York: Oxford University Press; 2015, pp. 260–265. [Google Scholar]
- 68. Rich J. D., McKenzie M., Larney S., Wong J. B., Tran L., Clarke J. et al. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open‐label trial. Lancet 2015; 386: 350–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Mitchell O., Wilson D. B., MacKenzie D. L. Does incarceration‐based drug treatment reduce recidivism? A meta‐analytic synthesis of the research. J Exp Criminol 2007; 3: 353–375. [Google Scholar]
- 70. Fazel S., Chang Z., Fanshawe T., Långström N., Lichtenstein P., Larsson H. et al. Prediction of violent reoffending on release from prison: derivation and external validation of a scalable tool. Lancet Psychiatry 2016; 3: 535–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kinner S. A., Alati R., Longo M., Spittal M. J., Boyle F. M., Williams G. M. et al. Low‐intensity case management increases contact with primary care in recently released prisoners: a single‐blinded, multisite, randomised controlled trial. J Epidemiol Community Health 2016; 70: 683–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Fazel S., Seewald K. Severe mental illness in 33 588 prisoners worldwide: systematic review and meta‐regression analysis. Br J Psychiatry 2012; 200: 364–373. [DOI] [PubMed] [Google Scholar]
- 73. HM Inspectorate of Prisons . Changing Patterns of Substance Misuse in Adult Prisons and Service Responses. London, UK: Her Majesty's Inspectorate of Prisons; 2015. [Google Scholar]
- 74. Payne‐James J. J., Wall I. J., Bailey C. Patterns of illicit drug use of prisoners in police custody in London, UK. J Clin Forensic Med 2005; 12: 196–198. [DOI] [PubMed] [Google Scholar]
- 75. Thomas E. G., Spittal M. J., Heffernan E. B., Taxman F. S., Alati R., Kinner S. A. Trajectories of psychological distress after prison release: implications for mental health service need in ex‐prisoners. Psychol Med 2016; 46: 611–621. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist.
Appendix S2 Quality checklist.
Appendix S3 Study characteristics of studies of substance use disorders in juvenile prisoners.
Appendix S4 Funnel plot of studies reporting drug use disorder prevalence in male prisoners.


