Abstract
To account for tobacco users' excess health care costs and encourage cessation, the Affordable Care Act (ACA) allowed marketplace plans to impose a surcharge on tobacco users' premiums. Because tax credits were calculated from premiums for non-tobacco-users, this policy greatly increased many smokers' out-of-pocket costs. Using data from the 2011-2014 Behavioral Risk Factor Surveillance System, we examined the effect of tobacco surcharges on insurance coverage and smoking cessation in the first year of marketplace implementation, among adults most likely to purchase insurance from state marketplaces. Relative to those facing no surcharges, smokers facing medium or high surcharges had significantly reduced insurance coverage (-4.3 to -11.6 percentage points), but no significant differences in smoking cessation. In contrast, those facing low surcharges showed significantly reduced smoking cessation. Taken together, these findings suggest that tobacco surcharges conflicted with a major goal of the ACA – increased financial protection – without increasing smoking cessation. States should consider these potential effects when deciding whether to constrain the surcharge below the federal limit in the future.
The Affordable Care Act (ACA) introduced several policies aimed at increasing tobacco cessation as well as individual responsibility for the consequences of ongoing tobacco use. In particular, the law required exchange plans to cover screening for tobacco use and cessation treatment at no cost sharing, while also allowing tobacco premium rating: the imposition of an up to 50 percent increase in premiums for tobacco users compared with non-users.1 Other than age and geography, the only factor allowed to affect premiums in the exchanges is tobacco use. For the purposes of the tobacco surcharge, the definition of tobacco use is, “use of a tobacco product or products four or more times per week within no longer than the past 6 months.”1 Several states rejected this outright, requiring equal premiums for users and non-users, while others capped the maximum penalty at a lower level (i.e., 10-40 percent of the premium).1 This policy increased the out-of-pocket cost of coverage substantially for many because ACA tax credits for marketplace insurance plans are calculated based on premiums for non-tobacco-users. Thus, although the goal of tax credits was to reduce premiums to an affordable level, even individuals with very low incomes were charged the full cost of the tobacco use surcharge.
The net effect of these policies is unclear. Some tobacco users may have responded by foregoing insurance. Prior research on the population expected to purchase insurance through the exchanges indicated that higher premiums would significantly reduce insurance take-up.2 While the insurance penalty associated with the ACA's individual mandate—a fee required of many who remain uninsured—is designed to encourage insurance take-up, individuals are exempt from this penalty if premiums are deemed “unaffordable” for them; that is, if the least expensive bronze plan's annual premium, including any tobacco surcharges, exceeds eight percent of their household income. Applying this definition, Kaplan et al. found that plan options in more than 30 percent of states were unaffordable for a 45 year old tobacco user with low to middle income.3 Thus, alongside surcharges, this exemption from the individual mandate could further dampen tobacco users' enrollment rates, even as the penalty rises to its full level in 2016.
However, introducing coverage of tobacco cessation treatment has been found to significantly increase smoking cessation.4 This suggests that quit rates could rise among smokers who do take up insurance. In some cases, financial incentives for quitting have also been found to increase cessation; yet, even then, studies tend to focus on rewards for quitting, not penalties for continuing to smoke.5–7 Still, evidence from one recent study suggests that penalties may be more effective than straightforward rewards.8
Given this evidence, we hypothesized that tobacco surcharges would affect both health insurance coverage and tobacco cessation, with larger surcharges reducing tobacco users' insurance enrollment but increasing their cessation rates. As the available data provided a detailed history of smoking cessation but not cessation from other tobacco products, we were able to consider the impact of tobacco surcharges on cigarette smokers but not all tobacco users. Reassuringly, in our sample, 90.4 percent of tobacco users smoked cigarettes, and 94.2 percent of these used no other tobacco products. Thus, the surcharges' effects on cigarette smokers reflect the impact on the vast majority of tobacco users in these data.
While some states capped their surcharge levels, insurers were empowered to set their specific plans' tobacco surcharges (within the bounds of a given state's maximum). Thus, plan surcharges varied both between and within states, with enrollees often able to choose among plans with different surcharge levels. We used this variation to test the effect of surcharge size on both outcomes. To estimate the association between surcharge level and health insurance enrollment, a triple-difference analysis compared coverage status before and after the surcharges went into effect, across states with different levels of tobacco surcharges, for current smokers versus non-smokers. For smoking cessation, an analogous difference-in-differences design compared cessation before and after the marketplace plans went into effect across states with different levels of tobacco surcharges.
Study Data and Methods
Respondent-Level Data
Data on individuals came from the U.S. Centers for Disease Control and Prevention's Behavioral Risk Factor Surveillance System (BRFSS), an annual survey of non-institutionalized adults that provides a representative sample for each state and the District of Columbia (DC).9 Analyses examined 2011 through 2014: three years prior to the marketplaces' implementation (2011-2013) and one year post-implementation (2014).
We determined individual insurance status based on responses to the question, “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?”10 “Current smokers” were defined as respondents who indicated they either currently smoked every day or some days, or that they had last smoked a cigarette within the past month. We included this latter group due to evidence that relapse rates are high in the first month after “quitting.”11 When estimating the effects on smoking cessation, the sample was restricted to “recent smokers,” defined as those who smoked within the past six months. As above, a respondent was considered to have quit if they both identified as a former smoker and had stopped smoking more than a month before being surveyed. Each respondent's federal poverty level (FPL) was imputed using reported income and marital status (as a proxy for household size among childless adults), based on the 2013 state-specific standards.
Sample Restrictions
Analyses considered adults who were eligible for premium tax credits on the health insurance marketplaces. This focus limited our sample to respondents with incomes between 100 and 400 percent of FPL, who were ineligible for both Medicare (i.e., under age 65) and Medicaid based on their state's 2014 Medicaid eligibility standards.12,13 To ensure reasonable comparison groups across states, individuals under 138 percent of FPL were omitted, as this income range was Medicaid eligible in every state that expanded Medicaid. Additionally, respondents under age 26 had access to dependent coverage beginning in late 2010, such that they were less likely to make independent insurance decisions.14 The BRFSS data codes age groups but not exact age, so we dropped those under age 25 but retained 25 year olds (who could not be omitted without dropping 26 through 29 year olds as well).
Several additional exclusions were made to prevent bias in our estimates. Specifically, we excluded Massachusetts residents because their marketplace preceded the ACA, as well as BRFSS respondents who completed the survey during open enrollment (the last quarter of 2013 or first quarter of 2014). Including respondents from the last quarter of 2013 could have biased results towards the null if some incorrectly reported insurance coverage at the point of enrollment, when their insurance had not yet gone into effect. The first quarter of 2014 was omitted as this was not a treatment period in the same sense as the remainder of that year: marketplace open enrollment continued throughout this quarter; and, many did not enroll for 2014 coverage until March.15
Finally, due to our inability to identify the insurance relationship between respondents and other household members (and thus to calculate family premiums), analyses considered only individuals in households without children. This restriction has a notable benefit: it may have yielded effect sizes that better pinpoint the impact of the surcharge's financial incentive on the individual who faced that incentive, since surcharge levels were based on the individual's premium.
Exhibit 1 describes the final sample (N=206,952). Eighty percent had health insurance coverage, and 25 percent were current smokers. Among respondents who had smoked in the prior six months (N=48,942), 72 percent had coverage and 7 percent reported having quit—that is, identified as former smokers and had not smoked for more than 30 days.
Exhibit 1. Characteristics of the Study Population, 2011-2014.
| Health Insurance Coverage Analysis | Smoking Cessation Analysis | |
|---|---|---|
| Health and health care (%) | ||
| Health care coverage | 80.4 | 72.4 |
| Current smoker | 24.7 | 93.3 |
| Male sex (%) | 52.5 | 59.2 |
| Age (%) | ||
| Age bin: 25-29 | 12.8 | 14.1 |
| Age bin: 30-34 | 7.8 | 9.5 |
| Age bin: 35-39 | 5.2 | 6.6 |
| Age bin: 40-44 | 7.1 | 8.1 |
| Age bin: 45-49 | 10.1 | 11.7 |
| Age bin: 50-54 | 17.8 | 18.9 |
| Age bin: 55-59 | 18.1 | 16.3 |
| Age bin: 60-64 | 21.2 | 14.9 |
| Race and ethnicity (%) | ||
| White | 69.8 | 73.5 |
| Black | 12.3 | 11.4 |
| Hispanic | 11.2 | 9.1 |
| Other race or ethnicity | 6.7 | 5.9 |
| Education (%) | ||
| Less than high school graduate | 9.8 | 14.7 |
| High school graduate | 33.3 | 38.5 |
| Some college | 35.3 | 34.6 |
| College graduate | 21.7 | 12.3 |
| Income (%) | ||
| 138-200% of FPL | 24.6 | 29.9 |
| 200-300% of FPL | 34.5 | 34.9 |
| 300-400% of FPL | 40.9 | 35.3 |
| Cellular phone respondent (%) | 37.4 | 43.9 |
| Economic Indicators | ||
| Cigarette tax (mean $) | 1.5 | 1.4 |
| Unemployment rate (mean %) | 7.8 | 7.8 |
| Respondents (N) | 206,952 | 48.942 |
SOURCE Authors' analysis of respondent-level data from the 2011-2014 BRFSS surveys, cigarette tax rates from the Federation of Tax Administrators (2014), and state unemployment rates from the Bureau of Labor Statistics (2014). NOTES All statistics are weighted means. Both samples are restricted to Medicaid ineligible 25 to 64 year olds with incomes between 138 and 400 percent of the federal poverty level (FPL) and no children in the household. Respondents from Massachusetts are excluded, as are those surveyed in the last quarter of 2013 or the first quarter of 2014. The smoking cessation analysis sample is further restricted to those respondents who reported smoking within the 6 months prior to interview.
Tobacco Surcharge Data
For 35 states and DC, data on 2014 premiums and tobacco surcharges came from the Centers for Medicare and Medicaid Services' Health Insurance Marketplace Plan Attribute and Rate Public Use Files.16 We abstracted New York's data directly from the state's marketplace website, and obtained the remaining states' data via individual appeals, public records requests, and Freedom of Information Act filings to relevant state agencies.17 Only premiums and tobacco surcharges offered to individual beneficiaries were considered, as BRFSS data lack the information on legal relationships between household members and their insurance characteristics needed to define the true insurance unit.
On average, 49 year old smokers living in one of the 43 states that allowed surcharges in 2014 faced a median tobacco surcharge of $70 per month. We calculated the tobacco surcharge level as a percent increase over the unsubsidized premium, since federal limits on surcharge size were written in these terms (e.g., a plan's surcharge may not exceed 50 percent of its premium). Moreover, as premium size varied substantially across states, defining surcharges in dollar terms would confound responses to high surcharges with responses to higher premiums or costs of living.
We assigned BRFSS respondents the median tobacco surcharge for their age across all “on-exchange” bronze-level plans offered to adults in their state's largest-population rating area.18 Individuals were categorized as facing one of four median surcharge levels: zero (no surcharge), low (non-zero and <10%), medium (≥10% and <30%), and high (≥30%). See Appendix Exhibit A1 for a map illustrating state-level variation in tobacco surcharge categories for a 49-year-old.19
Data Analysis
We used a triple-difference approach to estimate the association between surcharge level and health insurance enrollment, comparing coverage status before and after the surcharges went into effect, across state-by-age groups with different levels of tobacco surcharges, for current smokers versus non-smokers. For the smoking cessation outcome, an analogous difference-in-differences design compared cessation before and after the marketplace plans went into effect across state-by-age groups with different levels of tobacco surcharges. Age-stratified analyses evaluated our models separately for individuals under age 40 and those aged 40 and older, while robustness checks re-estimated the main specifications via multiple imputation to verify that findings were unchanged by the inclusion of respondents with missing data.
To ease interpretation of regression results, we used the resulting coefficients to estimate the insurance- and cessation-responses to different surcharge levels in each year, for a “representative smoker” and a “representative non-smoker” (i.e., individuals with the characteristics of the average smoker and non-smoker in 2011 within our sample). By holding other characteristics constant, this “prediction” captures the changes in insurance coverage and smoking cessation that can be attributed specifically to the different surcharge levels. For brevity, only 2013 and 2014 predictions are presented.
All regressions were sample-weighted linear probability models with standard errors clustered at the state level. Controls included age in five-year bands, income (138-200, 200-300, and 300-400 percent of FPL), sex, education (less than high school graduate, high school graduate, some college, and college graduate), race (white, black, Hispanic, other), and whether the survey was conducted via cellular phone versus landline, as well as state cigarette taxes and unemployment rates, and state, year, and quarter fixed effects.20,21 Both the insurance and smoking cessation specifications passed the requisite common trends tests. See the Technical Appendix for further details on the methods.19
Limitations
This analysis had several important limitations. Due to a lack of data on respondents' plan preferences, exact geographic location, and key income and household information needed to calculate premium subsidies, the surcharge assignment mechanism was inexact. Given these limitations, respondents were matched to the median surcharge for bronze plans in their state's largest-population rating area, an approach similar to that of Kaplan et al.3 These median surcharges were highly correlated with the weighted average of median surcharges across all other rating areas within the same state (ρ = 0.95).
FPL assignment was also imperfect due to missing household size data and the BRFSS's use of grouped income levels. Consequently, some individuals' Medicaid eligibility may be misclassified. To be conservative, our FPL calculations used the lowest income in the reported income band and took marital status as a proxy for household size where the latter was unreported. Robustness checks reclassified individuals using the upper income band and used multiple imputation methods to address missing household sizes. Regressions found similar results in each case; see the Technical Appendix for further detail.19
Three additional limitations have to do with the surcharges' implementation. First, in the context of these surcharges, the ACA defined tobacco use as “use of a tobacco product or products four or more times per week within no longer than the past 6 months.”1 While states had discretion to further restrict this definition, none did so.22 Due to data limitations, our analysis only considers cigarette use and does not measure frequency. Next, if the surcharges were not salient (i.e., acutely evident to consumers), their effect on smoking cessation may have been muted. This seems plausible as, when asking potential enrollees about their smoking status, marketplace websites did not clearly note that smokers might be charged a higher premium, nor did they present tobacco user and non-user premiums side-by-side. Typically, the enrollee could only view their plan options after indicating their smoking status, with the listed premiums accounting for any tobacco surcharges. As the interfaces were consistent in this presentation across states, we could not empirically test for salience effects. A lack of salience, however, might attenuate the third limitation: potentially dishonest reporting of one's smoking status. Currently, tobacco use is self-reported and not verified in any way. The only allowed consequence for misrepresenting one's smoking status is retroactive payment of owed surcharges. Thus, the possibility of dishonest reporting presents a true concern for this policy's efficacy, assuming tobacco users are aware that honest reporting may increase their premiums.23 Critically, this would not bias the results presented here unless the policy led smokers to dishonestly report their smoking status in their BRFSS interview, a context unrelated to insurance enrollment.
Finally, this study identified relationships during the first year of marketplace implementation. Enrollment patterns may adjust as the penalty for remaining uninsured rises to its full level in 2016 and consumers become more familiar with the marketplaces, surcharges, and relatively low consequences of misreporting one's smoking status.
Study Results
The main specifications' results matched those of our robustness checks. Thus, for simplicity, only the former are discussed below. The full results for every analysis can be found in the Technical Appendix.19
Insurance Coverage
Exhibit 2 indicates predicted insurance coverage in 2013 and 2014 by surcharge size, for a representative smoker and non-smoker. While coverage rates in 2013 and those for non-smokers vary by surcharge level, this observation is neither surprising nor a threat to the analysis. Both insurance coverage and surcharge assignment differ by age within states, so a general association between these variables is expected. This relationship does not bias our estimates, as the results are based on how key outcomes changed over time, not the associations that were stable over time.
Exhibit 2. Predicted Health Insurance Effects by Tobacco Surcharge Level.
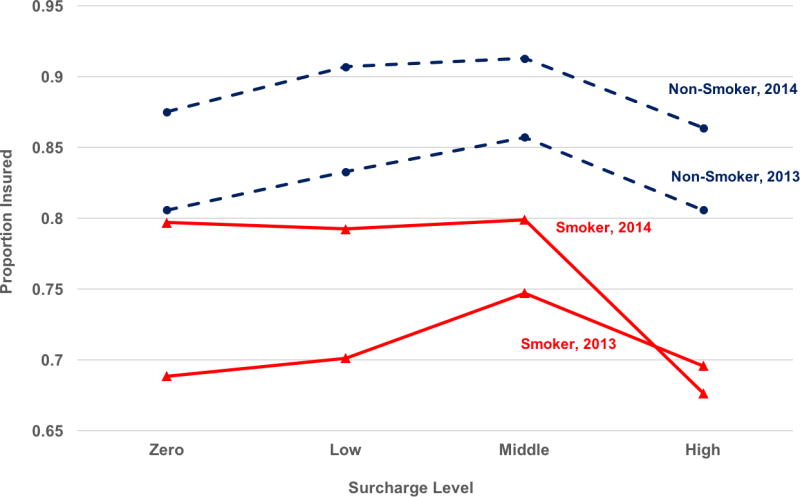
Source/Notes: SOURCE Authors' analysis of data from the 2011-2014 BRFSS surveys, with respondents matched to newly collected information on tobacco surcharges in the 2014 state health insurance marketplaces. NOTES The sample is restricted to Medicaid ineligible adults aged 25 to 64 with incomes between 138 and 400 percent of the federal poverty level and no children in their household. Those living in Massachusetts are also omitted. The figure plots predicted insurance coverage for a representative smoker and non-smoker (i.e., holding other characteristics constant), based on a triple difference analysis comparing insurance coverage among smokers versus non-smokers, before and after marketplace implementation, at different surcharge levels. The underlying regression controls for age, sex, race, education, income, and cell phone interviews, as well as state cigarette taxes and unemployment rates, and state, year, and quarter fixed effects. Surcharges are calculated as percent increases over the no-tobacco premium, with the levels above based on median surcharges in the highest population rating area within a respondent's state, for that respondent's age group. Surcharge levels are defined as follows: zero (no surcharge), low (non-zero and <10%), medium (>= 10% and <30%), and high (>=30%).
As expected, non-smokers exhibited an increase in insurance coverage with the marketplaces' implementation that did not differ by the size of the tobacco surcharge (8.1 percentage points; p<.01; Technical Appendix Exhibit A2).19 For smokers, however, larger tobacco surcharges dampened the increase in insurance coverage associated with the ACA's implementation. Indeed, Exhibit 2 shows no increase in coverage for a representative smoker in the highest surcharge group.
The results in Exhibit 4 are from the regressions used to generate Exhibit 2. Those listed under Model I represent the differential impact of surcharge size on smokers' 2014 insurance coverage, relative to the effect on smokers in the no-surcharge group. Results for age-stratified analyses are also presented. Regardless of age group, low surcharges yielded a statistically insignificant drop in smokers' health insurance take-up in 2014, relative to the no-surcharge group. These effects grew and became statistically significant as surcharge levels rose, reaching -11.6 percentage points in the high group (p<.05). Effects were even larger in the under age-40 analysis, with statistical significance for both medium (-11.9 percentage points; p<.01) and high surcharges (-19.9 percentage points; p<.01).
Exhibit 4. Tobacco Surcharge Effects on Health Insurance Coverage and Smoking Cessation.
| Percentage Point Change Over the Zero-Surcharge Effect (CI) | |||
|---|---|---|---|
|
|
|
||
| Low Surcharge (0 < Surcharge <10%) |
Medium Surcharge (10% ≤ Surcharge <30%) |
High Surcharge (30% ≤ Surcharge) |
|
| Model I: Health Insurance | |||
| Full Sample (N=206,952) | -2.2 (-10.1, 5.7) | -4.3 (-9.4, 0.8)* | -11.6 (-21.0, -2.3)** |
| Age < 40 | -7.4 (-21.5, 6.7) | -11.9 (-19.3, -4.5)*** | -19.9 (-28.4, -11.3)*** |
| Age ≥ 40 | -0.1 (-6.8, 6.6) | -0.7 (-5.1, 3.6) | -8.2 (-18.4, 2.1) |
| Model I: Smoking Cessation | |||
| Full Sample (N=48.942) | -5.6 (-10.9, -0.3)** | -1.6 (-6.8, 3.7) | 0.0 (-6.8, 6.8) |
| Age < 40 | -5.4 (-16.7, 5.9) | 0.2 (-10.6, 11.0) | -1.2 (-12.2, 9.8) |
| Age ≥ 40 | -5.2 (-8.1, -2.4)*** | -2.6 (-5.5, 0.4)* | -0.2 (-6.5, 6.0) |
SOURCE Authors' analysis of data from the 2011-2014 BRFSS surveys, with respondents matched to newly collected information on tobacco surcharges in the 2014 state health insurance marketplaces. NOTES Analyses are sample-weighted linear probability models specified as triple-differences for health insurance and difference-in-differences for smoking cessation, with additional controls for age, sex, race, education, income, and cell phone interview indicators, as well as state cigarette taxes and unemployment rates, and state, quarter, and year fixed effects. Effects given above are the differential percentage point increases in health insurance coverage (Model I) and smoking cessation (Model II) exhibited by smokers facing each of the above surcharge levels, relative to the response of smokers in the zero surcharge group. Both samples are limited to Medicaid ineligible 25 to 64 year olds not living in Massachusetts, with incomes between 138 and 400 percent of the federal poverty level (FPL) and no children in the household. The smoking cessation sample is further restricted to those who smoked at least once in the 6 months prior to interview. Surcharge levels are based on median surcharges for a given respondent's age and state, calculated as a percent increases over the corresponding no-tobacco premium. 95 percent confidence intervals are in parentheses. Output from the full models is available in Exhibits A2 and A3 of the Technical Appendix.19 ***[**](*) denotes statistical significance at the 1% [5%] (10%) levels.
Thus, it appears that higher surcharges reduced smokers' gains in health insurance coverage during the first year of marketplace implementation.
Smoking Cessation
Exhibit 3 gives predicted smoking cessation by surcharge level for a representative smoker. The 2013 rates vary somewhat by surcharge level; but, this is not a threat to the analysis for the same reasons noted above. Respondents in no-surcharge states showed a statistically insignificant rise in smoking cessation from 2013 to 2014 (2.0 percentage points; [95%CI: -4.1, 8.0]; Technical Appendix Exhibit A3), potentially consistent with greater insurance coverage increasing quit rates.19 Concurrently, smoking cessation fell markedly in the low surcharge group, yielding a statistically significant 5.6 percentage point reduction (p<.05) in smoking cessation compared to the no surcharge group (Exhibit 4). Thus, low surcharges may have had the unintended consequence of reducing smoking cessation. The concurrent finding that medium and high surcharge responses were statistically insignificant and much closer to zero may be consistent with the hypothesis that sufficiently high surcharges do more to incentivize cessation than low surcharges.
Exhibit 3. Predicted Smoking Cessation Effects by Tobacco Surcharge Level.
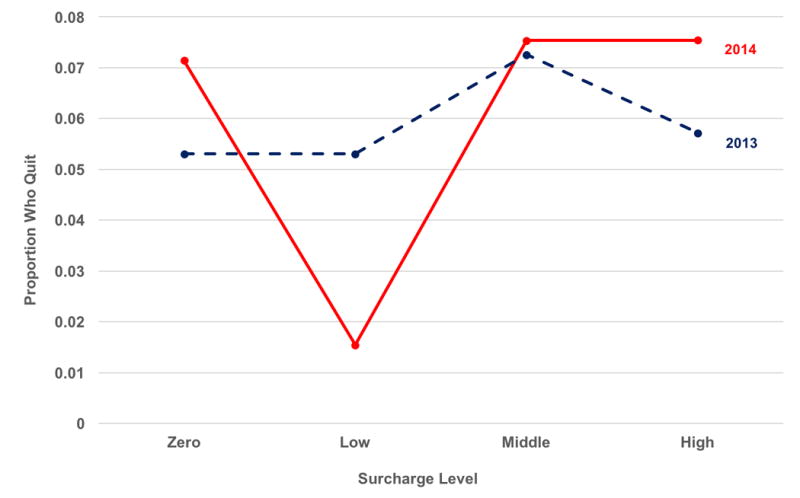
Source/Notes: SOURCE Authors' analysis of data from the 2011-2014 BRFSS surveys, with respondents matched to newly collected information on tobacco surcharges in the 2014 state health insurance marketplaces. NOTES The sample is restricted to Medicaid ineligible adults aged 25 to 64 who smoked in the 6 months before interview, with incomes between 138 and 400 percent of the federal poverty level and no children in their household. Respondents living in Massachusetts are also omitted. The figure plots predicted smoking cessation for a representative smoker (i.e., holding other characteristics constant), based on a difference-in-differences analysis comparing smoking cessation before and after marketplace implementation, at different surcharge levels. The underlying regression controls for age, sex, race, education, income, and cell phone interviews, as well as state cigarette taxes and unemployment rates, and state, year, and quarter fixed effects. Surcharges are calculated as percent increases over the no-tobacco premium, with the levels above based on median surcharges in the highest population rating area within a respondent's state, for that respondent's age group. Surcharge levels are defined as follows: zero (no surcharge), low (non-zero and <10%), medium (>= 10% and <30%), and high (>=30%).
Discussion
Insurance
We find that medium and high tobacco surcharges dampened the increases in insurance coverage for smokers in the first year of marketplace implementation. For the full sample analysis, smokers facing the highest surcharges exhibited a 12 percentage point reduction in coverage relative to the no surcharge group, while the under-40 sample showed a 20 percentage point difference. Comparing smokers' and non-smokers' responses to variation in tobacco surcharges as marketplace plans went into effect makes these results particularly compelling, as the effect among non-smokers controls for outside factors that may have influenced insurance enrollment in state-by-age groups with higher surcharges.
While reduced insurance take-up is not a surprising response to higher surcharges, it is concerning. Smokers were 7.3 percentage points less likely to have coverage than non-smokers (Appendix Exhibit A2), so their enrollment is critical to achieving universal coverage.19 Moreover, younger adults' enrollment in marketplace plans is important for risk pooling, suggesting that the large effects found among smokers under age 40 may have broader implications for the long-term stability of exchanges in states with high surcharge levels.
Smoking Cessation
Among the zero, medium, and high surcharge groups, the marketplace implementation's effects on smoking cessation were neither statistically significant nor statistically different from each other. However, relative to every other surcharge group, those facing low (non-zero) surcharges were significantly less likely to quit smoking. That high surcharge groups showed a greater cessation-response than those facing low surcharges, despite no gains in insurance coverage, suggests a direct response to surcharges (i.e., a tendency to respond to a high smoking penalty by quitting), rather than an insurance effect (i.e., individuals benefitting from enhanced access to providers and smoking cessation treatment through insurance). Indeed, some tobacco users may not have taken-up coverage in 2014, but still quit during that year in anticipation of wanting to purchase insurance for 2015 (to avoid the increasing individual penalty).
However, these two competing mechanisms do not explain why those exposed to low surcharges exhibited a decline in smoking cessation relative to the zero surcharge group, when the two showed similar increases in insurance coverage. One possible explanation is that putting a ‘price’ on bad behaviors can alleviate the guilt of engaging in them, inducing an unexpected effect: the behavior increases. In one famous illustration, instituting a fee for late pick-up at an Israeli day care center resulted in more, not fewer, tardy caregivers.24 Similarly, low surcharges might dampen smoking cessation if some smokers feel that this payment compensates society for their behavior, and the fine is not high enough to incentivize quitting. Unfortunately, this hypothesis is not testable with the survey data used in this study.
One purpose of the tobacco surcharges is for tobacco users to pay the excess health care costs associated with their smoking. Yet, Kaplan et al. found that these surcharges were often significantly greater than smoking's added health care costs.3 As individuals with psychological distress or depression have much higher smoking rates than those without mental health conditions (34 versus 17 percent), some insurers could be using the tobacco surcharges to discourage enrollment by patients with these high-cost conditions.25 If the risk adjustment mechanism used in a state's marketplace does not adequately compensate plans for these disease states, insurers may profit by encouraging such adverse selection.26 Thus, an unintended consequence of tobacco surcharges may be reduced insurance coverage (or unfairly high premiums) for some individuals with persistently high health care costs unrelated to their tobacco use. Such individuals might have benefited greatly from gaining coverage. When considering the effects of tobacco surcharges, policymakers should account for such costs.
This study's findings may inform the evolution of state-level policy on tobacco premium ratings. Our results indicate that if coverage and cessation are the most important goals, having no surcharge is preferable to low, medium, and high surcharge levels, as it yields the highest or equivalent rates of both coverage and cessation. Low surcharges may actually work against cessation, while high surcharges appear to impede enrollment.
Conclusion
Compared to smokers facing low or zero tobacco surcharges, those faced with medium and high tobacco surcharges were less likely to gain insurance coverage after the marketplaces' implementation. Yet smokers facing non-zero surcharges were no more likely to quit than those who were not subject to a surcharge, and were less likely to quit when the surcharge was low. This suggests that tobacco surcharges increased neither smoking cessation nor financial protection from high health care costs – the primary goal of the ACA.
Supplementary Material
Notes
- 1.Overview: Final Rule for Health Insurance Market Reforms. Centers for Medicare and Medicaid Services; 2013. [Internet] [cited 2015 Aug 1]. Available from: https://www.cms.gov/CCIIO/Resources/Files/Downloads/market-rules-technical-summary-2-27-2013.pdf. [Google Scholar]
- 2.Krueger AB, Kuziemko I. Journal of Health Economics. 5. Vol. 32. Elsevier B.V.; 2013. The demand for health insurance among uninsured Americans: Results of a survey experiment and implications for policy; pp. 780–93. [Internet] Available from: http://dx.doi.org/10.1016/j.jhealeco.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan CM, Graetz I, Waters TM. Most Exchange Plans Charge Lower Tobacco Surcharges Than Allowed, But Many Tobacco Users Lack Affordable Coverage. Health Affairs. 2014;33(8):1466–73. doi: 10.1377/hlthaff.2013.1338. [Internet] Available from: http://content.healthaffairs.org/cgi/doi/10.1377/hlthaff.2013.1338. [DOI] [PubMed] [Google Scholar]
- 4.Land T, Warner D, Paskowsky M, Cammaerts A, Wetherell L, Kaufmann R, et al. Medicaid coverage for tobacco dependence treatments in Massachusetts and associated decreases in smoking prevalence. PloS one. 2010;5(3):e9770. doi: 10.1371/journal.pone.0009770. [Internet] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2841201&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cahill K, Hartmann-Boyce J, Perera R. Incentives for smoking cessation. In: Cahill K, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2015. May 18, [Internet] Available from: http://doi.wiley.com/10.1002/14651858.CD004307.pub5. [DOI] [PubMed] [Google Scholar]
- 6.Sigmon SC, Patrick ME. The use of financial incentives in promoting smoking cessation. Preventive Medicine. 2012;55(SUPPL):24–32. doi: 10.1016/j.ypmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Volpp KG, Galvin R. Reward-based incentives for smoking cessation: how a carrot became a stick. JAMA. 2014 Mar 5;311(9):909–10. doi: 10.1001/jama.2014.418. [Internet] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24493405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halpern SD, French B, Small DS, Saulsgiver K, Harhay MO, Audrain-McGovern J, et al. Randomized Trial of Four Financial-Incentive Programs for Smoking Cessation. New England Journal of Medicine. 2015 doi: 10.1056/NEJMoa1414293. [Internet] 150513140033002. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa1414293. [DOI] [PMC free article] [PubMed]
- 9.Annual Survey Data [Internet] Behavioral Risk Factor Surveillance System. 2015 [cited 2015 May 31]. Available from: http://www.cdc.gov/brfss/annual_data/annual_data.htm.
- 10.2014 Questionnaire [Internet] Behavioral Risk Factor Surveillance System. 2014 [cited 2015 May 31]. Available from: http://www.cdc.gov/brfss/questionnaires/pdf-ques/2014_brfss.pdf.
- 11.Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 12.Medicaid Eligibility for Adults as of January 1, 2014. Kaiser Family Foundation; 2013. [Internet] [cited 2015 Jun 15]. Available from: http://kff.org/medicaid/fact-sheet/medicaid-eligibility-for-adults-as-of-january-1-2014/ [Google Scholar]
- 13.2013 Poverty Guidelines. Office of the Assistant Secretary for Planning and Evaluation. 2013 [Internet] [cited 2015 Jun 15]. Available from: http://aspe.hhs.gov/2013-poverty-guidelines.
- 14.Sommers BD, Kronick R. The Affordable Care Act and Insurance Coverage for Young Adults. JAMA. 2012 Mar 7;307(9) doi: 10.1001/jama.307.9.913. [Internet] Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.307.9.913. [DOI] [PubMed] [Google Scholar]
- 15.Office of the Assistant Secretary for Planning and Evaluation; 2014. Health Insurance Marketplace: Summary enrollment report for the initial annual open enrollment period. [Internet] [cited 2016 Feb 2]. Available from: https://aspe.hhs.gov/sites/default/files/pdf/76876/ib_2014Apr_enrollment.pdf. [Google Scholar]
- 16.Health Insurance Marketplace Public Use Files (Marketplace PUF) Center for Consumer Information & Insurance Oversight; 2015. [Internet] [cited 2015 Jun 25]. Available from: https://www.cms.gov/CCIIO/Resources/Data-Resources/marketplace-puf.html. [Google Scholar]
- 17.NY State of Health. 2014 [Internet] [cited 2015 Aug 25]. Available from: https://nystateofhealth.ny.gov/individual.
- 18.Annual Estimates of the Resident Population. U.S. Census American FactFinder; 2014. [Internet] [cited 2015 Jun 10]. Available from: https://www.census.gov/popest/data/counties/totals/2012/CO-EST2012-01.html. [Google Scholar]
- 19.To access the Appendix, click on the box to the right of the article online.
- 20.Local Area Unemployment Statistics. Bureau of Labor Statistics; 2014. [Internet] [cited 2015 Aug 19]. Available from: http://www.bls.gov/lau/ [Google Scholar]
- 21.The Tax Burden on Tobacco. Federation of Tax Administrators; 2014. [Internet] [cited 2015 Aug 19]. Available from: http://www.taxadmin.org/fta/tobacco/papers/tax_burden_2014.pdf. [Google Scholar]
- 22.Giovannelli BJ, Lucia K, Corlette S. Insurance Premium Surcharges for Smokers May Jeopardize Access to Coverage. The Commonwealth Fund Blog. 2015 [Internet] [cited 2015 May 6]. Available from: http://www.commonwealthfund.org/publications/blog/2015/jan/insurance-premium-surcharges-for-tobacco-use.
- 23.Liber AC, Hockenberry JM, Gaydos LM, Lipscomb J. The Potential and Peril of Health Insurance Tobacco Surcharge Programs: Evidence From Georgia's State Employees' Health Benefit Plan. Nicotine & Tobacco Research. 2014;16(6):689–96. doi: 10.1093/ntr/ntt216. [Internet] Available from: http://ntr.oxfordjournals.org/cgi/doi/10.1093/ntr/ntt216. [DOI] [PubMed] [Google Scholar]
- 24.Gneezy U, Rustichini A. A Fine Is a Price. Journal of Legal Studies. 2000;29(1) [Google Scholar]
- 25.Cook BL, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311(2):172–82. doi: 10.1001/jama.2013.284985. [Internet] Available from: http://www.ncbi.nlm.nih.gov/pubmed/24399556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Layton T, Ellis R, McGuire T. Assessing Incentives for Adverse Selection in Health Plan Payment Systems. Cambridge, MA: 2015. Sep, [Internet] Available from: http://www.nber.org/papers/w21531.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


