Summary
Background
Unprecedented levels of habitat transformation and rapid urbanisation are changing the way individuals interrelate with the natural environment in developing countries with high economic disparities. Although the potential benefit of green environments for mental health has been recognised, population-level evidence to this effect is scarce. We investigated the effect of green living environment in potentially countering incident depression in a nationally representative survey in South Africa.
Methods
We used panel data from the South African National Income Dynamics Study (SA-NIDS). Our study used SA-NIDS data from three waves: wave 1 (2008), wave 2 (2010), and wave 3 (2012). Households were sampled on the basis of a stratified two-stage cluster design. In the first stage, 400 primary sampling units were selected for inclusion. In the second stage, two clusters of 12 dwelling units each were drawn from within each primary sampling unit (or 24 dwelling units per unit). Household and individual adult questionnaires were administered to participants. The main outcome, incident depression (ie, incident cohort of 11 156 study participants without significant depression symptoms at their first entry into SA-NIDS), was assessed in the adult survey via a ten item version of the Center for Epidemiologic Studies Depression Scale; a total score of ten or higher was used as a cutoff to indicate significant depressive symptoms. Each participant was assigned a value for green living space via a satellite-derived normalised difference vegetation index (NDVI) based on the GPS coordinates of their household location.
Findings
Overall, we found uneven benefit of NDVI on incident depression among our study participants. Although the green living environment showed limited benefit across the study population as a whole, our final analysis based on logistic regression models showed that higher NDVI was a predictor of lower incident depression among middle-income compared with low-income participants (adjusted odds ratio [aOR] 0·98, 0·97–0·99, p<0·0001), although when this analysis was broken down by race, its positive effect was particularly evident amongst African individuals. Living in rural areas was linked to lower odds of incident depression (aOR 0·71, 0·55–0·92, p=0·011) compared with study participants residing in urban informal areas that often lack formal planning.
Interpretation
Our results imply the importance of green environments for mental wellbeing in sub-Saharan African settings experiencing rapid urbanisation, economic and epidemiological transition, reaffirming the need to incorporate environmental services and benefits for sustainable socioeconomic development.
Funding
South African Medical Research Council, National Institutes of Health, and Academy of Finland.
Introduction
Over the past four decades biodiversity has continued to decline around the world.1 In sub-Saharan Africa, the decline is mainly fuelled by rapid urban growth.2 Despite the adoption of the UN Sustainable Development Goals for equitable development in low-income and middle-income countries (LMICs), there is an inevitable and unavoidable conflict between biodiversity conservation and natural resource-based economic growth strategies.3,4 Urbanisation, fuelled by economic development, is perceived as a major potential force for large-scale poverty reduction, but urban growth can also be a key driver of biodiversity loss.5
The growing urbanisation and declining biodiversity characteristic of sub-Saharan Africa means that more people are at risk of living in environments with fewer green spaces, which is of concern because substantial evidence shows that exposure to green space is associated with reduced mortality6 and multiple positive health outcomes,7–10 in some cases in a dose-response fashion.11 The evidence for access to and interaction with green space and mental health largely supports an association11–14 that is independent of physical activity,15,16 and might be related to the buffering effects of greenness against stress.17,18 Evidence supporting a causal relationship is constrained by the cross-sectional design of most studies, with the three longitudinal studies done on the topic to date showing mixed results.19–21 Clarifying the implications of a green environment for population mental health is important because this can contribute key evidence to the ongoing sustainable development debate around how to balance biodiversity conservation and economic growth for sustainable development within a resilient environment.22
Mental illness is widely recognised as a development challenge; so much so that its promotion and the prevention and treatment of mental illness are included within the Sustainable Development Goals for 2030.23 Among mental health disorders, depression is increasingly identified as a growing and costly public health burden across the world and is the second leading cause of years lived with disability both globally and in sub-Saharan Africa.24,25 The economic burden of depression is substantial, estimated at roughly US$210 billion for the USA in 201026 and €118 billion for Europe in 2004.27
With its legacy of a discriminatory apartheid regime that promoted racial, economic, and land inequality,28,29 South Africa is a sub-Saharan African nation in economic and epidemiological transition, and has the one of the highest levels of population development inequity, as measured by Gini coefficient, globally.30 Although poverty, income inequality, and unemployment are persistent development challenges,31 industrial expansion is occurring rapidly in South Africa,32 and the middle class is growing.33 The HIV infection rate is stabilising and life expectancy is increasing because of life-saving antiretroviral therapy.34 Consequently, focus is shifting from communicable to non-communicable chronic health conditions (ie, the epidemiological transition) as growing and leading causes of morbidity and burden in the country.35 Depression is one of the most common mental disorders in South Africa, with an estimated 9·8% lifetime prevalence for major depressive disorder in adults.36 The workplace-related economic loss due to major depression in South Africa is estimated at $17 billion per year—equivalent to 4·9% of the country’s gross domestic product.37
The sustainable development challenges facing South Africa are as complex as anywhere else in sub-Saharan Africa—namely, how to preserve rich biological diversity and slow the inevitable loss of natural habitat, while prioritising poverty alleviation through economic development.38 This challenge has led some to question whether the green living environment is even relevant within developing countries where poverty is widespread—a position seemingly supported by evidence for “the apparent incompatibility between biodiversity and development”.39 For example there is evidence that “states with high material wealth have low biodiversity wealth and vice versa”,40 while the Millennium Ecosystem Assessment41 concluded that “the degradation of biodiversity over the last decades had led to significant improvements in human wellbeing and a decrease in poverty”.39 The Netherlands Environmental Assessment Agency42 suggested that “a country’s biodiversity is inversely related to its human development index (HDI)”.43 Importantly, among the hypotheses proposed by Raudsepp-Hearne and colleagues44 to explain this “environmentalist paradox”39—ie, the apparent improvement in human wellbeing globally despite ecosystem services decline—is the argument that within the sustainable development debate, researchers have failed to adequately capture human welfare with existing indicators.
Aiming to contribute useful evidence to this debate, we planned to investigate the relationship between exposure to green space and onset of depression in South Africa. To our knowledge, no previous study has explored this relationship in any setting. In this study, we used nationally representative panel data from South Africa to investigate the effect of the green living environment on risk for incident depression.
Methods
Study design and sample
Data were obtained from the South African National Income Dynamics Study (SA-NIDS), a longitudinal panel survey of a nationally representative sample of households.45 Our study used SA-NIDS data from three waves: wave 1 (2008), wave 2 (2010), and wave 3 (2012). The sampling methods are detailed in the SA-NIDS technical report.46 Sampling of households was based on a stratified two-stage cluster design. In the first stage, 400 of 3000 primary sampling units defined by Statistics South Africa were selected for inclusion. In the second stage, two clusters of 12 dwelling units each were drawn from within each primary sampling units for a total of 24 dwelling units per primary sampling unit. All resident household members at the selected dwelling units were included in the panel (ie, multiple households can be nested within a single dwelling). SA-NIDS is dynamic in the sense that it accounts for changes in the wellbeing and living conditions of household members (including movement) across three waves. Data from household and individual adult questionnaires were used in this study. After consent was obtained from the person filling in the questionnaire, the household questionnaire was administered by trained fieldworkers to the oldest woman in each household, or to another household member knowledgeable about living arrangements. Every consenting household member aged 15 years or older in all the sampling units participated in the adult questionnaire. A sample adult questionnaire (2008) is available online. The adult questionnaire included the ten item abridged version of the Center for Epidemiologic Studies Depression Scale (CES-D), which was used to assess depression symptoms, with a score of ten or more considered to represent major depressive symptoms. The global positioning system (GPS) was used to establish and record the geographical coordinates of each household included in the study. The questionnaires were available and administered in South Africa’s 11 official languages.
Our study is based on an incident depression cohort. To be included, study participants had to have been assessed for depression risk at least twice within waves 1–3. We excluded all participants positive for significant depressive symptoms at their first entry into SA-NIDS. The remaining participants with at least one other depression symptomatology rating between waves 2 and 3 made up our incident cohort. For this incident cohort, we right censored the data at the earliest observation at which a participant screened positive for depression risk or at the last observation if the participant did not screen for depression. We constructed the incident cohort to lessen the possibility of reverse causation. The use of the SA-NIDS data was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE 111/14).
Outcomes
The main outcome of the study was incident depression, as obtained from the CES-D component of the adult questionnaires. The original 20 item CES-D is a psychometrically tested instrument to screen for depression risk,47 and has been used in other studies in South Africa.48,49 The abridged version of CES-D50 has been shown to retain psychometric validity.51,52 CES-D is self-reported and captures depression-associated symptoms during the past week with four possible responses: scores of 0 denote rarely or none of the time (less than 1 day); scores of 1 denote some or little of the time (1–2 days); scores of 2 denote occasionally or a moderate amount of time (3–4 days); and scores of 3 denote almost or all of the time (5–7 days). Depression symptomatology is based on a composite score of ten items from the CES-D ranging from 0 to 30 (Cronbach’s α was 0·73 for our study), with a higher score indicating higher risk for the disorder. Consistent with previous studies,50 we dichotomised the composite CES-D measure using a total score of 10 or greater as a cutoff to represent significant depressive symptoms.
Exposures
The primary study exposure was the satellite image-based normalised difference vegetation index (NDVI), a commonly used measure of vegetation greenness that is sensitive to the amount of actively photosynthesising biomass on the landscape.53 NDVI,54 introduced by Rouse and colleagues,55 has been used to generate vegetation productivity and distribution maps in different settings, including Africa.56,57 The index values range from −1·0 to +1·0, where +1·0 represents the highest possible density of green leaves58 and green environment per specified spatial unit.59 For this study, we used NDVI intervals of 0·1. Corresponding to the SA-NIDS waves 1–3, we accessed the annual mean NDVI indices of South Africa from 2008, 2010, and 2012 from National Aeronautics and Space Administration (NASA) MODIS satellite with the MODIS/Terra Vegetation Indices 16-Day L3 Global 1km SIN Grid V005 dataset (MOD13A3).60 The vegetation index product has obtained validation stage 3, as reported by the data producer, suggesting that uncertainties are well quantified from comparison with reference data.61 We chose to use mean NDVI at 1 km resolution to be consistent with other work in South Africa. Monthly mean NDVI was calculated as a weighted temporal average of all 16 day 1 km products for each month if data were cloud free. In case of clouds, the maximum value was used.62 Each household in SA-NIDS was assigned an NDVI value based on its corresponding GPS coordinate. To display and extract the NDVI values from each household in the study, we used ArcGIS version 10.3. From each georeferenced household, we obtained the corresponding NDVI value, which was then assigned to each individual belonging to that household. We accessed household GPS coordinates from the SA-NIDS from the DataFirst’s Secure Data Centre at University of Cape Town (Cape Town, South Africa).
Data on gender, marital status, education, age, race or ethnicity, and employment status were also obtained from the adult questionnaires, and household income data were obtained from the household questionnaires. The matter of what constitutes the middle-income class is one of considerable debate in South Africa. South Africa has one of the highest levels of income inequality in the world,63 and the income distribution is heavily skewed to the right, meaning that most households are clustered toward the bottom of the distribution. For this reason, households in our study with a minimum income of R13 565 (2017 US$1000) per month, which corresponded to the top quintile in the income distribution, were defined as middle class (ie, middle-income group). That figure is within the range of what is considered a middle income for a household of four individuals in South Africa.64 Participants with a household income below this threshold, which corresponded to the bottom 80% of the income distribution, were defined as the low-income group.
Statistical analysis
Following a descriptive analysis of the demographic and clinical details of the study participants, we assessed the association between NDVI and incident depression with three logistic regression models that account for the clustering of repeated observations within participants. Model 1 examined the role of NDVI and household income on the depression outcome without controlling for any covariate. For model 2, we added various covariates (gender, marital status, education, age, race or ethnicity, employment status, and land typology as a measure of development) to the first model. For model 3, we added an interaction term, NDVI by household income, to the second model. The aim of this analysis was to establish whether the effect of household income on depression was dependent on varying levels of NDVI. We also did a separate analysis to construct margin plots and calculate the predicted probability of depression risk by varying levels of NDVI and household income stratified by race or ethnicity (to avoid the complexity of three-way interactions). Because the study involved a complex survey, the analyses involving proportion and regression were adjusted by post-stratification weight. The post-stratification weight was adjusted to the age-sex-race distribution produced by Statistics South Africa for the mid-year population estimates for 2008 (wave 1), 2010 (wave 2), and 2012 (wave 3), respectively.65,66
Results
The baseline characteristics of our incident cohort of 11 156 participants (table 1) show that slightly more than half of study participants were female (6376 [53·3%] individuals) and were younger than 35 years (6414 [58·4%] individuals), and the largest racial group was African (8786 [78·6%] individuals). These results are consistent with general population demographics in South Africa. Roughly half of study participants had never been married (6499 [54·7%] individuals), and were not employed (7177 [59·2%] individuals). Most participants had completed at least a high-school equivalent level of education (10 045 [93·3%] individuals). Africans represented 48·4% (n=1073) and whites represented 30·9% (n=429) of the middle-income group in our study.
Table 1.
Individual characteristics of respondents
| Study population (n=11 156) | |
|---|---|
| Gender | |
|
| |
| Male | 4780 (46·7%) |
| Female | 6376 (53·3%) |
|
| |
| Marital status | |
|
| |
| Married/living with partner | 3794 (38·1%) |
| Divorced/separated/widow | 863 (7·3%) |
| Never married | 6499 (54·7%) |
|
| |
| Race/ethnicity | |
|
| |
| African | 8786 (78·6%) |
| Coloured* | 1716 (9·3%) |
| Asian/Indian | 151 (2·6%) |
| White | 503 (9·5%) |
|
| |
| Age category | |
|
| |
| 15–19 | 2875 (22·8%) |
| 20–24 | 1480 (12·6%) |
| 25–29 | 1110 (11·8%) |
| 30–34 | 949 (11·2%) |
| ≥35 | 4742 (41·6%) |
|
| |
| Education | |
|
| |
| Less than high school | 1111 (6·7%) |
| Completed high school | 7458 (62·1%) |
| Beyond high school | 2587 (31·2%) |
|
| |
| Employment status | |
|
| |
| Not employed | 7177 (59·2%) |
| Employed | 3979 (40·8%) |
|
| |
| Household income | |
|
| |
| Lowest 20% | 2650 (21·7%) |
| Low/middle 20% | 2304 (16·9%) |
| Middle 20% | 2169 (17·3%) |
| Middle/high 20% | 2023 (17·6%) |
| Highest 20%† (middle income) | 2010 (26·4%) |
|
| |
| Land typology‡ | |
|
| |
| Rural | 1161 (7·4%) |
| Tribal authority | 4679 (31·8%) |
| Urban formal | 4613 (50·2%) |
| Urban informal | 703 (10·6%) |
SA-NIDS typology is derived from Statistics South Africa.67 Accordingly, distinction between urban and rural is often based on artificial and administrative political boundaries for government programming purposes. In this analysis, we consider urbanicity (a category of typology) to be a measure of development. Percentage results are weighted with post-stratification weights.
The term coloured is used by Statistics South Africa68 and includes children or descendants with black–white, black–Asian, white–Asian, and black–coloured mixed parentage.69
Middle-income group consists of individuals with a minimum household income of R13 565 (US$1000) per month.
Tribal authority area refers to rural areas with a mixture of traditional and civil authority; urban informal refers to areas with limited physical infrastructure or formal urban planning.70
At baseline (wave 1), our incident cohort was free of depressive symptoms. Prevalence of significant depressive symptoms increased to 15·9% (1656 individuals) in wave 2 and 20·8% (1896 individuals) in wave 3. The results of the adjusted logistic regression with model 1 showed that NDVI was not significantly associated with incident depressive symptomatology outcome (odds ratio [OR] 1·00, 95% CI 1·00–1·01, p=0·17; table 2) and that, compared with the low-income group, individuals in the middle-income group had reduced odds of significant depressive symptomats (OR 0·58, 0·50–0·67, p<0·0001). In model 2, a higher NDVI was significantly associated with a small increase in significant depressive symptoms (adjusted OR [aOR] 1·01, 1·01–1·02, p<0·0001), adjusting for well known predictors of depression. In model 3, the full model with interaction terms, higher NDVI in the middle-income group compared with low-income participants predicted lower odds of significant depressive symptoms (aOR 0·98, 95% CI 0·97–0·99, p=0·013). Residing in rural areas also predicted lower odds of significant depressive symptoms (aOR 0·71, 95% CI 0·55–0·92, p=0·011) compared with living in urban informal areas, which are often characterised by lack of physical infrastructure or formal urban planning. We also found that individuals who are younger, better educated, employed, and resided in a tribal authority had significantly decreased odds of incident depression, whereas Africans, and non-married study participants, had significantly increased odds of incident depression.
Table 2.
Adjusted logistic regression models on incident depression outcome
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| OR (95% CI) | SE | p value | aOR (95% CI) | SE | p value | aOR | SE | p value | |
| NDVI | 1·00 (1·00–1·01) | <0·01 | 0·17 | 1·01 (1·01–1·02) | <0·01 | <0·0001 | 1·01 (1·01–1·02) | <0·01 | <0·0001 |
|
| |||||||||
| Household Income | |||||||||
| Low income | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Middle income* | 0·58 (0·50–0·67) | 0·04 | <0·0001 | 0·92 (0·78–1·09) | 0·08 | 0·34 | 1·79 (1·03–3·11) | 0·50 | 0·038 |
|
| |||||||||
| Interaction terms | |||||||||
| ≥Middle income by NDVI | ·· | ·· | ·· | ·· | ·· | ·· | 0·98 (0·97–0·99) | 0·01 | <0·0001 |
|
| |||||||||
| Gender | |||||||||
| Male | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Female | ·· | ·· | ·· | 1·06 (0·94–1·20) | 0·06 | 0·31 | 1·06 (0·94–1·19) | 0·06 | 0·34 |
|
| |||||||||
| Marital status | |||||||||
| Married | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Divorced/widow/separated | ·· | ·· | ·· | 1·57 (1·27–1·94) | 0·17 | <0·0001 | 1·58 (1·29–1·95) | 0·17 | <0·0001 |
| Single | ·· | ·· | ·· | 1·42 (1·22–1·65) | 0·11 | <0·0001 | 1·43 (1·23–1·66) | 0·11 | <0·0001 |
|
| |||||||||
| Race | |||||||||
| White | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| African | ·· | ·· | ·· | 2·86 (1·74–4·73) | 0·73 | <0·0001 | 2·61 (1·56–4·37) | 0·69 | <0·0001 |
| Coloured† | ·· | ·· | ·· | 1·84 (1·08–3·13) | 0·50 | 0·025 | 1·67 (0·96–2·89) | 0·47 | 0·067 |
| Asian/Indian | ·· | ·· | ·· | 0·48 (0·19–1·23) | 0·23 | 0·13 | 0·50 (0·20–1·26) | 0·24 | 0·14 |
|
| |||||||||
| Age (years) | |||||||||
| 15–19 | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| 20–24 | ·· | ·· | ·· | 2·47 (2·00–3·05) | 0·27 | <0·0001 | 2·48 (2·01–3·06) | 0·27 | <0·0001 |
| 25–29 | ·· | ·· | ·· | 3·1 (2·46–3·89) | 0·36 | <0·0001 | 3·11 (2·47–3·91) | 0·36 | <0·0001 |
| 30–34 | ·· | ·· | ·· | 3·58 (2·77–4·64) | 0·47 | <0·0001 | 3·60 (2·78–4·66) | 0·47 | <0·0001 |
| ≥35 | 3·63 (2·93–4·49) | 0·40 | <0·0001 | 3·66 (2·95–4·53) | 0·40 | <0·0001 | |||
|
| |||||||||
| Educational attainment | |||||||||
| High school not completed | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Completed high school | ·· | ·· | ·· | 0·95 (0·80–1·13) | 0·08 | 0·55 | 0·95 (0·80–1·13) | 0·08 | 0·59 |
| Beyond high school | ·· | ·· | ·· | 0·67 (0·53–0·84) | 0·08 | 0·001 | 0·68 (0·54–0·85) | 0·08 | 0·001 |
|
| |||||||||
| Employment status | |||||||||
| Not employed | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Employed | ·· | ·· | ·· | 0·77 (0·67–0·88) | 0·05 | <0·0001 | 0·77 (0·67–0·88) | 0·05 | <0·0001 |
|
| |||||||||
| Land typology‡ | |||||||||
| Urban informal | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· | ·· |
| Rural | ·· | ·· | ·· | 0·72 (0·56–0·94) | 0·10 | 0·015 | 0·71 (0·55–0·92) | 0·09 | 0·011 |
| Tribal authority | ·· | ·· | ·· | 0·67 (0·56–0·81) | 0·07 | <0·0001 | 0·66 (0·55–0·80) | 0·06 | <0·0001 |
| Urban formal | ·· | ·· | ·· | 0·88 (0·73–1·07) | 0·09 | 0·21 | 0·88 (0·72–1·07) | 0·09 | 0·19 |
OR=odds ratio. aOR=adjusted odds ratio. SE=robust standard error.
Middle-income group consists of individuals with a minimum household income of R13 565 (US$1000) per month.
The term coloured is used by Statistics South Africa68 and includes children or descendants with black–white, black–Asian, white–Asian, and black–coloured mixed parentage.69
Tribal authority area refers to rural areas with a mixture of traditional and civil authority; urban informal refers to areas with limited physical infrastructure or formal urban planning.70
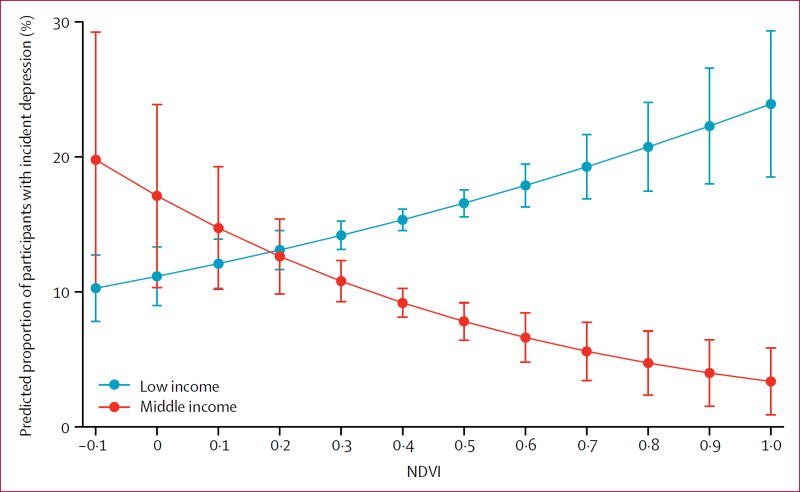
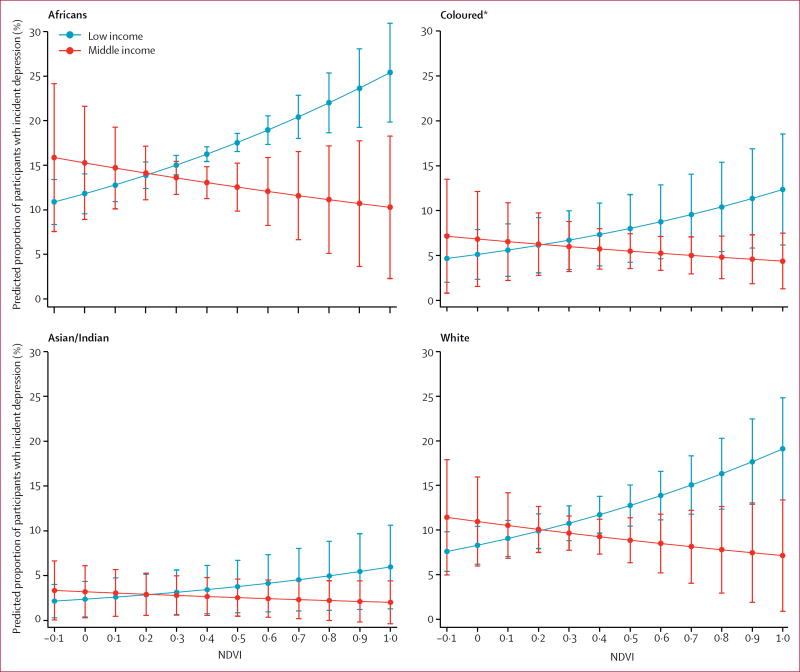
Our margin plot of probability of depression against NDVI (figure 1) showed a trend whereby, at higher NDVI indices, individuals in the middle-income group had lower odds of significant depressive symptoms compared with individuals in the low-income group. Predicted depression by NDVI and household income groups in South Africa by race or ethnicity is shown in figure 2. The trend looks similar in all groups. However, we found a significant difference in the predicted depression risk only among African participants whereby, as NDVI index increased, depression risk decreased significantly in the middle-income group compared with the low-income group, particularly when the NDVI index was 0·4 or higher, beyond which there were no overlaps in 95% CIs.
Figure 1. Predicted proportion of individuals with major depression by NDVI and household income group.
Middle-income group consists of individuals with a minimum household income of R13 565 (US$1000) per month. NDVI=normalised difference vegetation index.
Figure 2. Predicted depression by NDVI and household income group in South Africa by race or ethnicity.
Middle-income group consists of individuals with a minimum household income of R13 565 (US$1000) per month. NDVI=normalised difference vegetation index. *The term coloured is used by Statistics South Africa68 and includes children or descendants with black–white, black–Asian, white–Asian, and black–coloured mixed parentage.69
Discussion
Our study is the first to explore the relationship between exposure to green space and onset of depression. The findings suggest that, in South Africa, African individuals belonging to the middle-income group and residing in a green living environment had a reduced risk of incident depressive symptoms. Within the context of South Africa, with its long history of racially determined income disparity and land tenure inequality, which has persisted during the post-apartheid era, our findings highlight the importance of green space for its apparent protective effects against onset of depression. Our results contribute to a better understanding of how ecosystem services are related to a sense of place and human wellbeing.14
Results from several longitudinal studies outside sub-Saharan Africa (although not assessing incident depression) have suggested that green living environments and exposure to certain types of land cover have positive effect on mental health.71,72 It is well understood that multifactorial interactions (biological, psychological, social, and environmental) contribute to increased susceptibility to depression.73 However, our findings raise the important question as to why the protective benefit of a green living environment was only evident among African participants with higher household incomes, despite data from a past study suggesting that disadvantaged groups (ie, those of lower socioeconomic status) might benefit from exposure to greenness in reducing depressive symptoms.74 Serious engagement with the social, economic, racial, and developmental historical context of South Africa will be needed to answer this question. Results from past investigations,75,76 including a study originating from Africa (but outside sub-Saharan Africa),77 point to the complexity with which race and ethnicity, socioeconomic status, and context (ie, developing country) interact with the way a green environment can affect health in general. It is recognised that economic factors and a lingering sense of racism or unwelcomeness within what were once exclusively white South African recreational green spaces remain important challenges within the field of environmental development, well into the post-apartheid era.78 Land access and land reform are historically important psychological issues in South Africa.79 Under apartheid legislation (Natives [Urban Areas] Act of 192380 and Group Areas Act of 195081), Africans in South Africa were denied the right to reside in urban areas and were likewise forcibly removed from ancestral lands and barred from accessing national parks and other recreational green spaces. Instead, they were forced to live in Bantu homelands, where economic development and opportunities were restricted,82 and increased population density resulted in land degradation.
While poverty and racial income disparities persist in contemporary South Africa, the past 20 years have seen the gradual growth of an African middle class, as shown by the larger number of African individuals owning homes within the country’s affluent leafy suburbs.83 These post-apartheid shifts, which include economic and psychological freedoms and liberations for some previously disadvantaged people, could be associated with an enhanced sense of place or symbolic meanings, attachment, and fulfilment within a spatial setting for an individual or group.84 Feelings of reintegration with a cultural heritage related to land and restitution of justice for the historical forced removal from this land by whites, might underlie and help to explain why, in the our study, the benefit of a green living environment on mental health was evident among middle-income Africans who now have the economic means to access these spaces.
By contrast, we found no evidence that a green living environment had mental health benefits for the low-income group, which needs to be contextualised to the specific socioeconomic and political, historical, and contemporary experience of this majority group. Data from a previous national-level study showed that depression risk was highest among African individuals and those of the lowest socioeconomic status in South Africa.85 In the context of persistent poverty, which still affects about half of Africans in South Africa,86 the multiple social, economic, and health-related ills associated with poverty are likely to be the major drivers of depression, outweighing the effect of the surrounding physical environment as a potential risk factor. We speculate that maybe it is only when a person’s socioeconomic circumstances have improved, their basic needs been met, and they have moved out of poverty and into the middle class that other apparently non-essential factors such as the greenness of their living environment emerge as potential drivers of depression. We do not refute the buffering hypothesis87 (ie, that green space acts as a buffer between stressful life events and health) or suggest that people in poverty do not benefit from green space; rather we suggest that when someone is struggling for the basics of food and shelter and security, these essential needs might be the priority and the major determinants of wellbeing.
Our study has several limitations worth noting. First, the perceived quality of the green living environment in the SA-NIDS was not available, which might also affect the depressive symptom outcome. Access to or proximity to urban parks might also affect mental health, but such data were not available. Second, our study relied on NDVI as the measure of the green living environment. The NDVI measure does not capture the potentially important role of plant biodiversity, which might affect mental health. Additionally, residential history was captured once within each wave (ie, each year) in SA-NIDS. For each wave, we obtained a corresponding annual NDVI mean measure for that SA-NIDS household. We acknowledge that assigning only one NDVI mean value per household per wave is a limitation of our study. Although NDVI has been used extensively in environmental research,58 use of NDVI also suffers from, loss of sensitivity to changes in the amount of vegetation, soil effects, atmospheric effects, and cloud effects. Use of the MODIS NDVI partly overcame this issue (ie, clouds have been taken into consideration when compiling the MODIS data product), but in future studies, it might also be advisable to use another vegetation index, such as the enhanced vegetation index (EVI), the wide dynamic range vegetation index (WDRVI), or a combination of indices. Lastly, although the 1 km standard resolution used was consistent with that in a previous study in South Africa,88 future research might benefit from use of finer resolution (ie, <1 km) NDVI data that would help to better assess the impact of small patches of green areas in urban environments. Finer resolution (<1 km) NDVI data were not available at the time of our study. Although the SA-NIDS is a population-based dataset that is unique in sub-Saharan Africa, more datapoints would be warranted to investigate any long-term impact of a green living environment.
Notwithstanding these limitations, the study is, to our knowledge, not just the first to investigate the relationship between exposure to green space and incident depression, but also the first investigation of the relationship between green space and mental health in general in southern Africa. Climate change and its effects on the environment and health are a major concern in South Africa.89 We suggest that our study has important environmental policy implications, particularly for developing countries undergoing rapid economic industrialisation and urbanisation, such as South Africa. Although the green living environment was not protective against depression across the whole study population, it appears to be an important factor for previously disadvantaged groups of individuals and households emerging into the middle class. This finding has important implications for post-apartheid South Africa because the growth of the middle class symbolises sociopolitical stability90 and social modernisation.91 Globally, in developing countries with high inequality where portions of the population are moving into the middle class, the importance of planned access to green space might mitigate many psychological challenges associated with such fundamental change in the context of a rapidly urbanising world.
Although we recognise the obvious benefits of economic development to mental health through the alleviation of poverty, it is important to recognise that poorly managed and uncontrolled economic development can be detrimental to environmental integrity in middle-income countries.92 As reported in a review of the ecosystem service of having a sense of place,14 the economic benefits derived from environmental protection and conservation are often neglected. The apparent trade-offs between economic development and environmental protection have long been debated, but they are not mutually exclusive goals. From the regulatory perspective of a developing country, spatial planning and land use management in South Africa is governed by the Spatial Planning and Land Use Management Act of 2013.93 Section 7(c)(ii) of the act requires that decision-making procedures minimise negative financial, social, economic, or environmental impacts. Furthermore, the national act requires provinces and municipalities to develop spatial development frameworks, and our findings emphasise the importance of planning for green space within spatial development frameworks. Progress is also being made in satellite development in South Africa to enhance vegetation monitoring, but access to relatively inexpensive satellite data with spectral band information that is reliable and accurate enough for national scale vegetation monitoring is needed.94 Environmental protection and biodiversity conservation that enhances a sense of place should be prioritised for long-term mental wellbeing as part of integrated sustainable development strategies. We argue that it is possible to incrementally work towards such ideals through sustainable development regulation that fosters economic, social, and environmental benefits and monitors progress even in resource-limited countries.
Research in context.
Evidence before this study
We searched PubMed/MEDLINE, EBSCO, Sabinet Online, and Google/Google Scholar databases for studies published before May, 2017, with combination of search terms including “green environment”, “green living environment”, “residential green”, “greenness”, “green space”, “NDVI”, “biodiversity”, “sense of place”, “health”, “mental health”, “depression”, “depressive”, and “depressive symptoms”, “Africa”, “sub-Saharan Africa”, and “South Africa”. We restricted the language of the publications to English. The growing urbanisation and declining biodiversity characteristic of sub-Saharan Africa means that more people are at risk of living in environments with fewer green spaces. Despite the potential benefits of exposure to green space for mental health, evidence supporting a causal relationship is constrained by the absence of longitudinal population-based evidence on the effects of green living environment on incident depression in the setting of sub-Saharan Africa. Such evidence would contribute meaningfully to the sustainable development debate focused on how to balance economic growth with biodiversity preservation in developing regions of the world.
Added value of the study
Our study was based on secure data from the South African National Income Dynamics Study, which contains household geographical data permitting novel spatial statistical methods in a way that no other study in sub-Saharan Africa has been able to do so far. We used data on depression and green living spaces assessed via the satellite-derived normalised difference vegetation index (NDVI), which was based on household GPS coordinates, during the first three study waves (2008, 2010, and 2012). To our knowledge, this study is not just the first to investigate the relationship between exposure to green space and incident depression, but also the first investigation of the relationship between green space and mental health in general in southern Africa. We found that higher NDVI (ie, a greener living environment) predicted significantly lower odds of incident depression among African individuals belonging to the middle-income group. Furthermore, living in rural areas was linked to lower odds of incident depression compared with living in urban informal areas that often lack formal planning.
Implications
Our results have major implications for the often neglected cross-cutting issues of biodiversity (Sustainable Development Goal [SDG] 15.4) and mental health (SDG 3.4) in countries in sub-Saharan Africa undergoing rapid economic development and urbanisation. Our results emphasise the importance of green environments for human wellbeing, reaffirming the need to incorporate environmental services and benefits for sustainable social and economic development.
Acknowledgments
AT, AMV, and FT were supported by South Africa Medical Research Council Flagship grant (MRC-RFAUFSP-01-2013/UKZN HIVEPI). AT was also supported by a National Institutes of Health Research Training Grant (R25TW009337), funded by the Fogarty International Center and the National Institute of Mental Health. EDM thanks the Academy of Finland 2016–2019, Grant 250444, for support. The study was also supported by University of KwaZulu-Natal funding to RS. The content is solely the responsibility of the authors and does not necessarily represent the official views of the South African Medical Research Council or the National Institutes of Health. Our study utilised waves 1–3 data from the National Income Dynamics Study of the Southern Africa Labour and Development Research Unit, Cape Town (data producer; 2015) and DataFirst, Cape Town (data distributor, 2015). We thank Lynn Woolfrey at DataFirst at the University of Cape Town.
Footnotes
For the sample adult questionnaire (2008) see http://www.nids.uct.ac.za/images/documents/wave1/W1_Adult_Questionnaire_12May2016.pdf
For the MODIS satellite data see https://reverb.echo.nasa.gov
Contributors
AT, FT, RS, and JKB were responsible for the conception and design of the study, analysis and interpretation of the data, and drafting of the manuscript. AMV, DC, EDM, and VH participated in conception and design of the study, analysis and interpretation of the data, and drafting the manuscript. All authors read and approved the final manuscript.
Declaration of interests
We declare no competing interests.
References
- 1.Butchart SH, Walpole M, Collen B, et al. Global biodiversity: indicators of recent declines. Science. 2010;328:1164–68. doi: 10.1126/science.1187512. [DOI] [PubMed] [Google Scholar]
- 2.Seto KC, Fragkias M, Güneralp B, Reilly MK. A meta-analysis of global urban land expansion. PLoS One. 2011;6:e23777. doi: 10.1371/journal.pone.0023777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rees WE. Economic development and environmental protection: an ecological economics perspective. Environ Monit Assess. 2003;86:29–45. doi: 10.1023/a:1024098417023. [DOI] [PubMed] [Google Scholar]
- 4.Maze K, Barnett M, Botts EA, et al. Making the case for biodiversity in South Africa: re-framing biodiversity communications. Bothalia. 2016;46:1–8. [Google Scholar]
- 5.Seto KC, Güneralp B, Hutyra LR. Global forecasts of urban expansion to 2030 and direct impacts on biodiversity and carbon pools. Proc Natl Acad Sci. 2012;109:16083–88. doi: 10.1073/pnas.1211658109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gascon M, Triguero-Mas M, Martínez D, et al. Residential green spaces and mortality: a systematic review. Environ Int. 2016;86:60–67. doi: 10.1016/j.envint.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Pereira G, Christian H, Foster S, et al. The association between neighborhood greenness and weight status: an observational study in Perth Western Australia. Environ Health. 2013;12:49. doi: 10.1186/1476-069X-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown SC, Lombard J, Wang K, et al. Neighborhood greenness and chronic health conditions in Medicare beneficiaries. Am J Prev Med. 2016;51:78–89. doi: 10.1016/j.amepre.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Ebisu K, Holford TR, Bell ML. Association between greenness, urbanicity, and birth weight. Sci Total Environ. 2016;542:750–56. doi: 10.1016/j.scitotenv.2015.10.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124:1344–52. doi: 10.1289/ehp.1510363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanahan DF, Bush R, Gaston KJ, et al. Health benefits from nature experiences depend on dose. Sci Rep. 2016;6:28551. doi: 10.1038/srep28551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gascon M, Triguero-Mas M, Martínez D, et al. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health. 2015;12:4354–79. doi: 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. 2015;2:131–42. doi: 10.1007/s40471-015-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hausmann A, Slotow R, Burns JK, Di Minin E. The ecosystem service of sense of place: benefits for human well-being and biodiversity conservation. Environ Conserv. 2016;43:117–27. [Google Scholar]
- 15.Sugiyama T, Leslie E, Giles-Corti B, Owen N. Associations of neighbourhood greenness with physical and mental health: do walking, social coherence and local social interaction explain the relationships? J Epidemiol Community Health. 2008;62:e9. doi: 10.1136/jech.2007.064287. [DOI] [PubMed] [Google Scholar]
- 16.Triguero-Mas M, Dadvand P, Cirach M, et al. Natural outdoor environments and mental and physical health: relationships and mechanisms. Environ Int. 2015;77:35–41. doi: 10.1016/j.envint.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Roe JJ, Thompson CW, Aspinall PA, et al. Green space and stress: evidence from cortisol measures in deprived urban communities. Int J Environ Res Public Health. 2013;10:4086–4103. doi: 10.3390/ijerph10094086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson CW, Roe J, Aspinall P, et al. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc Urban Plan. 2012;105:221–29. [Google Scholar]
- 19.Annerstedt M, Ostergren PO, Björk J, Grahn P, Skärbäck E, Währborg P. Green qualities in the neighbourhood and mental health—results from a longitudinal cohort study in Southern Sweden. BMC Public Health. 2012;12:337. doi: 10.1186/1471-2458-12-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White MP, Alcock I, Wheeler BW, Depledge MH. Would you be happier living in a greener urban area? A fixed-effects analysis of panel data. Psychol Sci. 2013;24:920–28. doi: 10.1177/0956797612464659. [DOI] [PubMed] [Google Scholar]
- 21.Astell-Burt T, Mitchell R, Hartig T. The association between green space and mental health varies across the lifecourse. A longitudinal study. J Epidemiol Community Health. 2014;68:578–83. doi: 10.1136/jech-2013-203767. [DOI] [PubMed] [Google Scholar]
- 22.Iritié BGJJ. Economic growth and biodiversity: an overview conservation policies in Africa. J Sustain Dev. 2015;8:196–208. [Google Scholar]
- 23.WHO. Mental health included in the UN Sustainable Development Goals. [accessed April 1, 2017]; http://www.who.int/mental_health/SDGs/en/
- 24.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrari AJ, Charlson FJ, Norman R, et al. Burden of depressive disorders by country, sex, age, and year: findings from the Global Burden of Disease Study 2010. PLoS Med. 2013;10:e1001547. doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76:155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- 27.Sobocki P, Jönsson B, Angst J, Rehnberg C. Cost of depression in Europe. J Ment Health Policy Econ. 2006;9:87–98. [PubMed] [Google Scholar]
- 28.Hall R. A political economy of land reform in South Africa. Rev Afr Polit Econ. 2004;31:213–27. [Google Scholar]
- 29.O’Laughlin B, Bernstein H, Cousins B, Peters PE. Introduction: agrarian change, rural poverty and land reform in South Africa since 1994. J Agrarian Change. 2013;13:1–5. [Google Scholar]
- 30.The World Bank. Overview: South Africa. [accessed May 3, 2017]; http://www.worldbank.org/en/country/southafrica/overview.
- 31.Luiz JM. Economic governance, markets and public accountability: a freedom constraint? In: Plaatjies D, editor. Protecting the inheritance: governance & public accountability in democratic South Africa. Auckland Park: Jacana; 2013. pp. 106–22. [Google Scholar]
- 32.Turok I. Urbanisation and development in South Africa: economic imperatives, spatial distortions and strategic responses. London: International Institute for Environment and Development; 2012. [Google Scholar]
- 33.Southall R. The new black middle class in South Africa. Woodbridge: Boydell & Brewer; 2016. p. 42. [Google Scholar]
- 34.Bor J, Herbst AJ, Newell M, Bärnighausen T. Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science. 2013;339:961–65. doi: 10.1126/science.1230413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shisana O, Labadarios D, Rehle T, et al. South African national health and nutrition examination survey (SANHANES-1): 2014 edition. Cape Town: HSRC Press; 2014. [Google Scholar]
- 36.Herman AA, Stein DJ, Seedat S, et al. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. SAMJ. 2009;99:339–44. [PMC free article] [PubMed] [Google Scholar]
- 37.Evans-Lacko S, Knapp M. Global patterns of workplace productivity for people with depression: absenteeism and presenteeism costs across eight diverse countries. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1525–37. doi: 10.1007/s00127-016-1278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Di Minin E, Macmillan DC, Goodman PS, Escott B, Slotow R, Moilanen A. Conservation businesses and conservation planning in a biological diversity hotspot. Conserv Biol. 2013;27:808–20. doi: 10.1111/cobi.12048. [DOI] [PubMed] [Google Scholar]
- 39.Billé R, Lapeyre R, Pirard R. Biodiversity conservation and poverty alleviation: a way out of the deadlock? S.A.P.I.EN.S. 2012;5:1–15. [Google Scholar]
- 40.Koziell I, Saunders J. Living off biodiversity: exploring livelihoods and biodiversity issues in natural resources management. London: International Institute for Environment and Development; 2001. [Google Scholar]
- 41.Millennium Ecosystem Assessment. Ecosystems and human well-being: biodiversity synthesis. Washington, DC: World Resources Institute; 2005. [Google Scholar]
- 42.Netherlands Environmental Assessment Agency. Poverty, climate and biodiversity. Second sustainability outlook. Bilthoven: Netherlands Environmental Assessment Agency; 2008. The Netherlands in a sustainable world. [Google Scholar]
- 43.Tekelenburg T, Ten Brink B, Witmer M. How do biodiversity and poverty relate? An explorative study. Bilthoven: Netherlands Environmental Assessment Agency; 2009. [Google Scholar]
- 44.Raudsepp-Hearne C, Peterson GD, Tengö M, et al. Untangling the environmentalist’s paradox: why is human well-being increasing as ecosystem services degrade? Bioscience. 2010;60:576–89. [Google Scholar]
- 45.Southern Africa Labour and Development Research Unit. FAQ: general. [accessed April 1, 2017]; http://www.nids.uct.ac.za/documentation/faqs/general.
- 46.Leibbrandt M, Woolard I, de Villiers L. Methodology: report on NIDS Wave 1. Cape Town: University of Cape Town; 2009. [Google Scholar]
- 47.Radloff LS. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 48.Hamad R, Fernald LCH, Karlan DS, Zinman J. Social and economic correlates of depressive symptoms and perceived stress in South African adults. J Epidemiol Community Health. 2008;62:538–44. doi: 10.1136/jech.2007.066191. [DOI] [PubMed] [Google Scholar]
- 49.Myer L, Smit J, Roux LL, Parker S, Stein DJ, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDS. 2008;22:147–58. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 50.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 51.Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20:429–36. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 52.Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D Short Form. Psychol Assess. 2004;16:360–372. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- 53.Burgan RE, Hartford RA. General technical report INT-GTR-297. Ogden: US Department of Agriculture; 1993. Monitoring vegetation greenness with satellite data. [Google Scholar]
- 54.Pettorelli N. The normalized difference vegetation index. Oxford: Oxford University Press; 2013. [Google Scholar]
- 55.Rouse JW, Haas RH, Schell JA, Deering DW. Monitoring vegetation systems in the Great Plains with ERTS. In: Freden SC, Mercanti EP, Becker M, editors. Third Earth Resources Technology Satellite-1 Symposium. Washington, DC: National Aeronautics and Space Administration; 1974. pp. 309–17. [Google Scholar]
- 56.Tucker CJ, Townshend JR, Goff TE. African land-cover classification using satellite data. Science. 1985;227:369–75. doi: 10.1126/science.227.4685.369. [DOI] [PubMed] [Google Scholar]
- 57.Pettorelli N, Vik JO, Mysterud A, Gaillard JM, Tucker CJ, Stenseth NC. Using the satellite-derived NDVI to assess ecological responses to environmental change. Trends Ecol Evol. 2005;20:503–10. doi: 10.1016/j.tree.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 58.Weier J, Herring D. Measuring vegetation. [accessed June 8, 2015];2000 http://earthobservatory.nasa.gov/Features/MeasuringVegetation/
- 59.Lillesand TM, Kiefer RW. Remote sensing and image interpretation. 2. Hoboken: Wiley; 1987. p. 705. [Google Scholar]
- 60.NASA. MOD13A3 MODIS/Terra vegetation Indices Monthly L3 Global 1km SIN Grid V005. [accessed June 8, 2015];NASA EOSDIS Land Processes DAAC. 2015 https://doi.org/10.5067/MODIS/MOD13A1.006.
- 61.NASA. MODIS land team. [accessed June 8, 2015];Validation. 2017 https://landval.gsfc.nasa.gov.
- 62.NASA. Vegetation Indices Monthly L3 Global 1km. [accessed June 8, 2015];2014 https://lpdaac.usgs.gov/dataset_discovery/modis/modis_products_table/mod13a3.
- 63.OECD. OECD economic surveys: South Africa. Paris: OECD Publishing; 2013. 2013. [Google Scholar]
- 64.Visagie J. Growth of the middle class: two perspectives that matter for policy. Dev South Afr. 2015;32:3–24. [Google Scholar]
- 65.Wittenberg M. Weights: report on NIDS Wave 1. Cape Town: University of Cape Town; 2009. [Google Scholar]
- 66.Brown M, Daniels RC, de Villiers L, Leibbrandt M, Woolard I. National Income Dynamics Study Wave 2 user manual. Cape Town: University of Cape Town; 2013. [Google Scholar]
- 67.Statistics South Africa. Census 2001: investigation into appropriate definitions of urban and rural areas for South Africa. Pretoria: Statistics South Africa; 2003. [Google Scholar]
- 68.Statistics South Africa. Concept and definitions. Pretoria: Statistics South Africa; 2004. [Google Scholar]
- 69.Brown K. Coloured and black relations in South Africa: the burden of racialized hierarchy. Macalester International. 2000;9:198–203. [Google Scholar]
- 70.Makiwane M, Kwizera S. An investigation of quality of life of the elderly in South Africa, with specific reference to Mpumalanga province. Appl Res Qual Life. 2006;1:297–313. [Google Scholar]
- 71.Alcock I, White MP, Wheeler BW, Fleming LE, Depledge MH. Longitudinal effects on mental health of moving to greener and less green urban areas. Environ Sci Technol. 2014;48:1247–55. doi: 10.1021/es403688w. [DOI] [PubMed] [Google Scholar]
- 72.Alcock I, White MP, Lovell R, et al. What accounts for ‘England’s green and pleasant land’? A panel data analysis of mental health and land cover types in rural England. Landsc Urban Plan. 2015;142:38–46. [Google Scholar]
- 73.Lopizzo N, Bocchio Chiavetto L, Cattane N, et al. Gene-environment interaction in major depression: focus on experience-dependent biological systems. Front Psychiatry. 2015;6:68. doi: 10.3389/fpsyt.2015.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McEachan RR, Prady SL, Smith G, et al. The association between green space and depressive symptoms in pregnant women: moderating roles of socioeconomic status and physical activity. J Epidemiol Community Health. 2016;70:253–59. doi: 10.1136/jech-2015-205954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weimann H, Rylander L, Albin M, et al. Effects of changing exposure to neighbourhood greenness on general and mental health: a longitudinal study. Health Place. 2015;33:48–56. doi: 10.1016/j.healthplace.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 76.Dadvand P, Wright J, Martinez D, et al. Inequality, green spaces, and pregnant women: Roles of ethnicity and individual and neighbourhood socioeconomic status. Environ Int. 2014;71:101–08. doi: 10.1016/j.envint.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 77.Mowafi M, Khadr Z, Bennett G, Hill A, Kawachi I, Subramanian SV. Is access to neighborhood green space associated with BMI among Egyptians? A multilevel study of Cairo neighborhoods. Health Place. 2012;18:385–90. doi: 10.1016/j.healthplace.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 78.Butler G, Richardson S. Barriers to visiting South Africa’s national parks in the post-apartheid era: black South African perspectives from Soweto. J Sustain Tour. 2015;23:146–66. [Google Scholar]
- 79.Macleod C. South African psychology and ‘relevance’: continuing challenges. S Afr J Psychol. 2004;34:613–29. [Google Scholar]
- 80.Union of South Africa. Natives (Urban Areas) Act, Act No 21 of 1923. [accessed April 1, 2017]; http://disa.ukzn.ac.za/leg19230614028020021.
- 81.Union of South Africa. Group Areas Act, Act No 41 of 1950. [accessed April 1, 2017]; http://disa.ukzn.ac.za/leg19500707028020041.
- 82.Meadows ME, Hoffman MT. The nature, extent and causes of land degradation in South Africa: legacy of the past, lessons for the future? Area. 2002;34:428–37. [Google Scholar]
- 83.Mattes R. South Africa’s emerging black middle class: a harbinger of political change? J Int Dev. 2015;27:665–92. [Google Scholar]
- 84.Stedman RC. Toward a social psychology of place predicting behavior from place-based cognitions, attitude, and identity. Environ Behav. 2002;34:561–81. [Google Scholar]
- 85.Ardington C. Case A Interactions between mental health and socioeconomic status in the South African national income dynamics study. Tydskr Stud Ekon Ekon. 2010;34:69–85. [PMC free article] [PubMed] [Google Scholar]
- 86.Statistics South Africa. Poverty trends in South Africa: an examination of absolute poverty between 2006 and 2011. Pretoria: Statistics South Africa; 2014. [Google Scholar]
- 87.van den Berg AE, Maas J, Verheij RA, Groenewegen PP. Green space as a buffer between stressful life events and health. Soc Sci Med. 2010;70:1203–10. doi: 10.1016/j.socscimed.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 88.Wessels K, Prince S, Zambatis N, MacFadyen S, Frost P, Van Zyl D. Relationship between herbaceous biomass and 1-km2 advanced very high resolution radiometer (AVHRR) NDVI in Kruger National Park, South Africa. Int J Remote Sens. 2016;27:951–73. [Google Scholar]
- 89.Ziervogel G, New M, Archer van Garderen E, et al. Climate change impacts and adaptation in South Africa. Wiley Interdiscip Rev Clim Change. 2014;5:605–20. [Google Scholar]
- 90.Perotti R. Growth, income distribution, and democracy: what the data say. J Econ Growth. 1996;1:149–87. [Google Scholar]
- 91.Easterly W. The middle class consensus and economic development. J Econ Growth. 2001;6:317–35. [Google Scholar]
- 92.Aşıcı AA. Economic growth and its impact on environment: a panel data analysis. Ecol Indic. 2013;24:324–33. [Google Scholar]
- 93.Government of South Africa. Act No. 16 of 2013: Spatial Planning and Land Use Management Act, 2013. Pretoria: Government of South Africa; 2013. Government Gazette No. 36730. [Google Scholar]
- 94.Mutanga O, Dube T, Ahmed F. Progress in remote sensing: vegetation monitoring in South Africa. S Afr Geogr J. 2016;98:461–71. [Google Scholar]